Back to Journals » Clinical Interventions in Aging » Volume 18
Preoperative Vitamin D Deficiency is Associated with Increased One-Year Mortality in Chinese Geriatric Hip Fracture Patients – A Propensity Score Matching Study
Authors Fu G , Wu R, Zhang R, Chen D, Li H , Zheng Q, Ma Y
Received 28 October 2022
Accepted for publication 10 February 2023
Published 18 February 2023 Volume 2023:18 Pages 263—272
DOI https://doi.org/10.2147/CIA.S395228
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Guangtao Fu,1,* Rongjie Wu,1,2,* Ruiying Zhang,1,* Duanyong Chen,1 Haotao Li,1 Qiujian Zheng,1,3 Yuanchen Ma1
1Department of Orthopedics, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, People’s Republic of China; 2Shantou University Medical College, Shantou, People’s Republic of China; 3The Second School of Clinical Medicine, Southern Medical University, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yuanchen Ma, Tel +86-18688889132, Email [email protected]; Qiujian Zheng, Tel +86-13802740561, Email [email protected]
Background: Vitamin D deficiency is a common comorbidity in geriatric hip fracture patients. However, there is still an ongoing debate regarding the influence of preoperative Vitamin D status on postoperative mortality in hip fracture patients.
Methods: Elderly patients (≥ 60 years) who underwent surgical interventions for unilateral hip fracture from 2015 to 2020 in our center were included. We retrospectively retrieved the demographic data from the electronic medical database. Preoperative serum total 25-hydroxy-Vitamin D was set as the independent variable and patients were classified as the Vitamin D deficiency (< 20ng/mL) and the control groups consequently. Clinical outcomes include all-cause mortality, walking ability, and major postoperative complications in the first postoperative year. Propensity score matching (PSM) was performed in a ratio of 1:1 in the two groups for further comparison.
Results: A total of 210 patients were included and 121 patients (57.6%) were diagnosed with Vitamin D deficiency. Patients in the Vitamin D deficiency group were much older and therefore preferred peripheral nerve block, and had significantly higher proportions of females, preoperative dementia, higher ASA grade, and lower baseline serum albumin level. Overall, 79 patients were identified in the Vitamin D deficiency and control groups after PSM, respectively. Patients diagnosed with Vitamin D deficiency showed a significantly higher one-year mortality (21.5% vs 6.3%, P=0.011) and a much lower one-year independent walking rate (67.1% vs.84.8%, P=0.016) after the matching. Regarding the dataset before PSM and after PSM, the AUC for serum Vitamin D for predicting one-year mortality was 0.656 (P=0.006) and 0.695 (P=0.002), respectively.
Conclusion: Our retrospective PSM-design study provides new evidence that Vitamin D deficiency was associated with a significantly higher mortality and poor walking ability in the first year after surgical intervention based on southern Chinese populations.
Keywords: vitamin D deficiency, mortality, hip fracture, propensity score match, Chinese population
Introduction
Geriatric hip fracture is a global public health problem, which affects approximately 4.5 million people per year worldwide.1 Due to the well-proven efficiency of surgical interventions, hip fracture patients typically require urgent operative treatment unless contraindicated by severe medical instability.2 Although several significant advances in anesthesia and surgical procedures were reported recently, hip fracture patients are still at substantial risk for a worse prognosis.3 It was reported that 7%4 and 16.6%5 of the hip fracture patients died within 30 days and the first year after surgery, respectively. As poor prognosis is related to a high risk of medical dispute,6 identifying patient-specific risk factors of death and walking disability is conducive to more reasonable and cost-effective preoperative clinical decision-making.
Vitamin D deficiency is a common comorbidity in geriatric hip fracture patients, with the incidence varying from 46% to 77.8%.7–9 Vitamin D deficiency is associated with many clinical outcomes including type of hip fracture, risk of falls, and cognitive status in hip fracture patients.10,11 However, there is still an ongoing debate when concerning the influence of preoperative Vitamin D status on postoperative mortality in hip fracture patients. Although there have been nearly a dozen retrospective studies investigating this issue,7–9,12–18 it is difficult to reach a consensus due to the conflicting results caused by the heterogenization of study design and statistical method, variable methods of Vitamin D measurement, as well as different follow-up time. Additionally, the quality of evidence in most of the previously-mentioned studies is largely limited by the selection bias due to the retrospective design. We previously reported that there were some major risk factors (ie, age, gender, serum albumin (ALB), anesthesia procedure, etc.) of increased postoperative mortality in hip fracture patients,19,20 which might be a potential cause of the conflicting results in previously-mentioned studies.
Consequently, the present study aimed to further investigate the influence of preoperative Vitamin D deficiency on one-year mortality in Chinese geriatric hip fracture patients via a retrospective propensity score matching (PSM) design, with the inclusion of almost all the currently known confounding factors.
Methods and Materials
Study Design
The present study was approved by the institutional review board of Guangdong Provincial People’s Hospital (KY2020-621-01) and was conducted following the ethical principles of the Helsinki declaration. The institutional review board of our hospital waived the informed consent procedure for our study due to the retrospective nature of the review. All the authors confirmed that the data used in our study was maintained with confidentiality. The electronic medical records of our hospital were reviewed and patients who met the following criteria were included in the present study: 1) aged ≥60 years, 2) diagnosed with a low-energy mechanism femoral neck or intertrochanteric fracture at our center between January 1, 2015, and December 31, 2020, 3) underwent surgical intervention. The exclusion criteria included those: 1) without intact data of Vitamin D, 2) with a previous history of trauma or surgery in the involved hip, 3) diagnosed with a peri-prosthetic, pathological or open fracture, and 4) diagnosed with severe multiple injuries that required non-orthopedic-related emergency surgeries.
Data Collection
Demographic data including age, gender, marital status, medical insurance, history of fragility fracture, preoperative dementia, as well as smoking and alcohol abuse history of selected patients were retrospectively retrieved from the medical data center. Clinical-related variables such as time from admission to surgery, diagnosis, Charlson comorbidity index (CCI), American Society of Anesthesiologist (ASA) grade, vital signs, serum total Vitamin D level, hemoglobin (HGB), and albumin (ALB) at the admission date, type of anesthesia and surgery, and results of electrocardiograph and chest radiography were also collected.
CCI was calculated to obtain an overall assessment of preoperative comorbid conditions.21 As we previously reported,19 CCI was transformed into a binary variable with the median of CCI (4) set as the cutoff. An abnormal vital sign was defined according to the criteria of Zanker’s study.22 Results of electrocardiogram and chest radiograph were classified as “Abnormality” only when they were considered to be clinically significant by the correspondent authors.
The independent variable in our study was the preoperative total serum Vitamin D level. Serum total 25-hydroxy-VD (t-25OHD) is currently the most widely used indicator of Vitamin D status,14 and Vitamin D deficiency was defined as <20ng/mL.9 Serum t-25OHD level was quantified by an electrochemiluminescence kit (Vitamin D total, Roche Diagnostics GmbH, Mannheim, Germany). The coefficient of variation percent (CV%) of intra- and inter-assay were 8.0% and 5.2%, respectively. The primary outcome was all-cause mortality in the first postoperative year, and the causes of death were also recorded. Secondary outcomes included walking ability, major postoperative complications within the first year, length of stay (LOS), and cost of hospitalization.
All-cause mortality, walking ability, and major postoperative complications in the first postoperative year were obtained from telephone follow-up by a well-trained staff with uniformed questionnaire. Patients were classified as “independent walking” when they scored ≥5 points in the locomotion section according to the functional independence measure scoring system.23 As we previously described,20 patients who died within the first year after surgery were defined as “walking ability impairment.” Major complications included pulmonary infection, deep venous thrombosis in the lower limbs, pulmonary embolism, craniocerebral events, prosthetic joint infection, periprosthetic fracture, and dislocation.
Statistical Analysis
Continuous data were expressed as mean ± standard deviation or median with an interquartile range. Categorical data were presented as percent (count). Baseline characteristics between the Vitamin D deficiency group and the control group were summarized and compared using bivariate tests (Mann–Whitney U, χ2, or Fisher’s exact tests). Patient demographics and baseline clinical data that possibly affect postoperative morbidity and mortality were included, followed by a PSM analysis with a ratio of 1:1. The detailed protocols of PSM for retrospective studies have been well described in Malhas et al’s study.24 Briefly, the propensity score was calculated by logistic regression analysis using patient demographics and baseline clinical data to examine the association of baseline Vitamin D level with one-year postoperative mortality. We used calipers of width equal to 0.2 of the standard deviation of the logit of the propensity score during PSM as recommended.25 The predictive abilities of preoperative serum Vitamin D level for one-year mortality in the entire data set (before PSM) and PSM set were further tested via area under the curve (AUC) analysis. Receiver operating characteristic (ROC) curves were performed to establish the cut-off values. Two-tailed tests were used, and differences were considered significant if P<0.05. SPSS 20.0 statistical software (Chicago, IL, USA) was used for the analysis.
Results
Demographic Data
A total of 820 patients who underwent surgical treatment due to femoral neck fracture or intertrochanteric fracture from January 1st, 2015, to December 31, 2020 in our center were identified. Only 245 of them (29.9%) had intact data of serum total Vitamin D level, and 210 patients were enrolled after exclusion (Figure 1). One hundred and twenty-one patients (57.6%) were diagnosed with Vitamin D deficiency, while there were 89 patients (42.4%) in the control group, with the mean serum Vitamin D level being 13.55 (10.86, 17.12) ng/mL and 26.02 (22.91, 30.73) ng/mL, respectively. The details of baseline demographic and clinical data of the entire data set, control group, and Vitamin D deficiency group are shown in Table 1.
 |
Table 1 Baseline Demographic and Clinical Data |
 |
Figure 1 Flowchart of the present study. |
Before matching, patients diagnosed with Vitamin D deficiency were older (80 yrs. vs 75yrs. P<0.001) and therefore preferred peripheral nerve block (53.7% vs 34.8%, P=0.013),20 and had higher proportion of female (80.2% vs 64.0%, P=0.014), preoperative dementia (16.5% vs 3.4%, P=0.005), higher ASA grade (43.8% vs 28.1%, P=0.029), lower baseline serum ALB level (33.62 ± 4.21 g/L vs 35.01 ± 4.51 g/L, P=0.024). Seventy-nine patients were identified in Vitamin D deficiency group and control group after PSM, respectively. No significant difference was found in the baseline demographic and clinical data between the two groups after matching. Notably, the rate of anti-osteoporotic treatment during stay of the entire data set was relatively low (25.7%), which did not differ in the two groups both before and after matching. Nevertheless, all enrolled patients were recommended daily supplements of vitamin D (0.5ug, Calcitriol) and calcium (600mg, Caltrate D) after discharge, and their compliance was confirmed by telephone follow-up.
Clinical and Health Economics Outcomes
The all-cause one-year mortality of the entire data set was 14.8% (Table 2). The detailed causes of all the 31 deaths are shown in Table 3. Patients diagnosed with Vitamin D deficiency showed significantly higher one-year mortality both before (20.7% vs 6.7%, P<0.001) and after the matching (21.5% vs 6.3%, P=0.011).
 |
Table 2 Clinical and Health economics Outcomes |
 |
Table 3 Causes of Death in the First Postoperative Year of the Entire Data Set |
As shown in Figure 2, the AUC for serum Vitamin D for predicting one-year mortality in the entire data set (before PSM) was 0.656 (P=0.006, 95% CI: 0.555–0.757). The best cut-off value of serum Vitamin D was 16.21 ng/mL, with the specificity and the sensitivity being 64.2% and 67.7%, respectively. Before PSM, there were 85 patients with a serum Vitamin D lower than 16.21 ng/mL, who showed 3.77 times the risk of one-year mortality when compared with the others (P=0.002, 95% CI: 1.67–8.51).
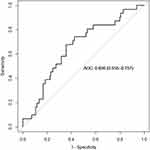 |
Figure 2 Results of AUC for serum Vitamin D for predicting one-year mortality in the entire data set (before PSM). |
As for the data set after PSM, the AUC for serum Vitamin D for predicting one-year mortality was 0.695 (P=0.002, 95% CI: 0.578–0.811, Figure 3). The best cut-off value of serum Vitamin D was 17.80 ng/mL, with the specificity and the sensitivity being 64.0% and 72.7%, respectively. After PSM, those with a serum Vitamin D lower than 17.80 ng/mL showed 3.82 times the risk of one-year mortality when compared with the others (P=0.001, 95% CI: 1.58–9.23).
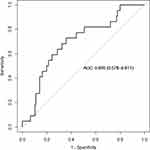 |
Figure 3 Results of AUC for serum Vitamin D for predicting one-year mortality in the data set after PSM. |
There was a significantly lower one-year independent walking rate in the Vitamin D deficiency group both before (65.3% vs 85.4%, P<0.001) and after the matching (67.1% vs.84.8%, P=0.016), which is shown in Table 2. Although a higher risk of major complications was still found in the Vitamin D deficiency group after PSM, it did not reach a significant level (10.1% vs 3.8%, P=0.177). Sixteen major complications within the first postoperative year were reported in surviving patients of the entire data set. Details of the major complications are listed in Table 4 and pulmonary infection was the most common complication (43.8%) in the present study. The hospitalization costs and LOS did not differ between the two groups.
 |
Table 4 Details of the One-Year Major Complications in Survival Patients of the Entire Data Set |
Discussion
Vitamin D deficiency is a common and important condition in geriatric hip fracture patients but is often underestimated by orthopedic surgeons. In the Mediterranean region, the prescription of vitamin D supplements is only 30–35% in patients before and after a hip fracture.26 Only 15% of hip fracture patients had a vitamin D concentration measurement in the perioperative period according to an earlier published study.27 Similarly, there was a comparable low Vitamin D measurement rate in our study (29.9%). In our study, the one-year mortality rate of geriatric hip fracture patients before and after PSM was 14.8% and 13.9%, respectively. Our data of one-year mortality in hip fracture patients after surgery was comparable to the results of a recently published study involving patients with similar age and treatment strategies.5 Of note, the large-scale study involving 269,535 patients in Asian population reported that 14.5% of hip fracture patients who had surgery died within 1 year, which was also consistent with the one-year mortality we found in our center.28 Thus, we suggest that our involved patients were representative and the potential selection bias was limited.
In the current study, patients in the Vitamin D deficiency group had a significantly higher one-year mortality both before and after the matching, which indicated that preoperative Vitamin D deficiency is one of the risk factors for one-year mortality in geriatric hip fracture patients. As far as we know, there were five studies regarding the one-year mortality rate in geriatric hip fracture patients. Being consistent with our study, previous reports using multivariate Cox regression or univariate analysis showed that vitamin D deficiency (<20 ng/mL) was associated with greater one-year mortality after hip fractures.17,18 Survival analysis indicated that the t-25OHD showed a tendency to predict survival, as the one-year mortality rate increased from 8% to 14% when comparing the t-25OHD deficiency group (≤16 ng/mL) and the control group.14 In addition, a retrospective, total cohort study including 30,552 patients found that Vitamin D supplementation showed a moderate but significant influence on postoperative mortality in hip fracture patients,29 which is in favor of our findings. However, the opposite side claimed that the four groups classified by quartiles of serum 25(OH)D did not differ in the one-year mortality of geriatric hip fracture patients.12 A recent study also reported no statistically significant relationship between vitamin D deficiency and one-year mortality, although there is a slightly higher incidence of one-year mortality in the vitamin D deficiency group (25% vs 21%).9 Of note, we found that different vitamin D measurement methods were performed among the studies. For instance, liquid chromatography-tandem mass spectrometry was performed in Ingstad’s study, while an electrochemiluminescence kit was performed in our study.9 Given the different accuracy and precision of different techniques, we speculated the variation in vitamin D measurement methods could be one of the potential biases that led to this conflicted conclusion. In addition, the heterogenization of study design, sample size, and statistical method of the previously-mentioned studies could also contribute to the conflicted conclusion. Collectively, the majority of studies support that preoperative vitamin D deficiency is closely associated with increased one-year mortality in hip fracture patients, which is consistent with our finding.
As far as we know, we are the first to use PSM to minimize selection bias when investigating the potential relationship between Vitamin D and postoperative mortality in hip fracture patients. Our PSM model included almost all the well-known preoperative indicators for postoperative mortality that were described in previous studies,22 such as gender, age, CCI, residence, ALB, anesthesia procedure, anti-osteoporotic treatment, and preoperative ECG results. As it was reported that data after PSM presumably approximates what a prospective randomized data set would have shown,30 we suggest that our study likely has a higher standard of evidence than other retrospective studies.
It is widely accepted that Asian countries will contribute more to the pool of hip fractures in the coming years.1,31 However, all the five studies we mentioned before were conducted at medical centers in Europe and our study represented the first time to investigate this issue in south Chinese populations. As significant differences in hip fracture prevalence, bone mineral density, and bone geometry were found between the Asian and Caucasian populations,32,33 we propose that our study could provide additional evidence of the influence of Vitamin D on long-term prognosis in hip fracture patients from southern China.
Currently, there is no consensus on the optimal cut-off values of t-25OHD for predicting clinical outcomes and the definition of adequate vitamin D status due to the different racial background.14,34 Based on the results of an observational, cross-sectional analysis, which was conducted in healthy South Asian populations who were aged from 40 to 69 years, 92% of the patients (5918 in 6433) were classified as Vitamin D deficiency (<20 ng/mL) according to the criteria, which were primarily set based on Caucasian populations.35 Consistently, we also found that the best cut-off values (16.21 ng/mL before PSM and 17.80 ng/mL after PSM) for predicting one-year mortality in south Chinese geriatric hip fracture patients were slightly lower than the commonly used cut-off thresholds of Vitamin D deficiency. Thus, we propose that the optimal cut-off value of Vitamin D for predicting clinical outcomes should be lower in Chinese populations, but more evidence is strongly needed.
Vitamin D status is one of the predictors of postoperative walking ability recovery in geriatric hip fracture patients.36 In the current study, significantly lower long-term (1 year) independent walking rates were found in Vitamin D deficiency patients both before and after the matching. Similarly, it was reported that there was a worse short-term (30 and 60 days) mobility in patients with Vitamin D <12 ng/mL.7 Vitamin D is crucial in maintaining and improving muscle strength as well as physical performance.37 It was also reported that older people with vitamin D deficiency might be at risk of sarcopenia, a geriatric syndrome characterized by the progressive loss of skeletal muscle mass and strength, which is often complicated by adverse events, such as falls and even death.38 Furthermore, Vitamin D was identified as an independent risk factor for in-hospital postoperative medical complications (pneumonia, thromboembolic events, and poorer cognitive status).39 Thus, we suggest that Vitamin D deficiency-related muscle strength decrease might be one of the major causes of reduced postoperative mobility, higher mortality, and increased risk of prolonged bed rest related-complications.
Our study has a few limitations. Firstly, it is a single-center, retrospective study with a relatively small sample size. Large-scale prospective studies are needed to further validate our conclusion, although PSM was performed to minimize the potential influence of selection bias in the current study. Nevertheless, the serum Vitamin D levels were measured in the same way by the same laboratory throughout the period in our study due to the single-center design. Secondly, the outpatient follow-up was largely limited by the COVID-19 issue. Only a very small proportion of patients have the results of vitamin D at the third month after surgery, details of which we have provided in Supplementary Figure 1. However, the long-term Vitamin D status was unavailable in the present study, which might cause potential bias for the one-year clinical outcomes.
Conclusion
The present study provides new evidence that Vitamin D deficiency was associated with a significantly higher mortality and poor walking ability in the first year after surgical intervention based on southern Chinese populations.
Data Sharing Statement
The database is available on request from the last author Yuanchen Ma ([email protected]).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval for the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
This work was supported by Guangdong Basic and Applied Basic Research Foundation (2022A1515011103) and (2021A1515110458), NSFC Incubation Program of GDPH (KY012021163), as well as the Program of Science and Technology of Guangzhou (201904010424).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. 2017;377(21):2053–2062. doi:10.1056/NEJMcp1611090
2. Bhandari M, Einhorn TA, Guyatt G, et al. Total hip arthroplasty or hemiarthroplasty for hip fracture. N Engl J Med. 2019;381(23):2199–2208.
3. Le Manach Y, Collins G, Bhandari M, et al. Outcomes after hip fracture surgery compared with elective total hip replacement. JAMA. 2015;314(11):1159–1166. doi:10.1001/jama.2015.10842
4. Pincus D, Ravi B, Wasserstein D, et al. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318(20):1994–2003. doi:10.1001/jama.2017.17606
5. Morri M, Ambrosi E, Chiari P, et al. One-year mortality after Hip fracture surgery and prognostic factors: a prospective cohort study. Sci Rep. 2019;9(1):18718. doi:10.1038/s41598-019-55196-6
6. Yin T, Liu Z, Xu Y. Analysis of crisis management of medical disputes in China and Australia: a narrative review article. Iran J Public Health. 2019;48(12):2116–2123.
7. Hao L, Carson JL, Schlussel Y, Noveck H, Shapses SA. Vitamin D deficiency is associated with reduced mobility after Hip fracture surgery: a prospective study. Am J Clin Nutr. 2020;112(3):613–618. doi:10.1093/ajcn/nqaa029
8. Nurmi-Lüthje I, Lüthje P, Kaukonen JP, Kataja M. Positive effects of a sufficient pre-fracture serum vitamin D level on the long-term survival of hip fracture patients in Finland: a minimum 11-year follow-up. Drugs Aging. 2015;32(6):477–486. doi:10.1007/s40266-015-0267-8
9. Ingstad F, Solberg LB, Nordsletten L, Thorsby PM, Hestnes I, Frihagen F. Vitamin D status and complications, readmissions, and mortality after Hip fracture. Osteoporosis Int. 2021;32(5):873–881. doi:10.1007/s00198-020-05739-9
10. Dretakis K, Igoumenou VG. The role of parathyroid hormone (PTH) and vitamin D in falls and Hip fracture type. Aging Clin Exp Res. 2019;31(10):1501–1507. doi:10.1007/s40520-019-01132-7
11. Carrillo González I, Martínez-Ramírez MJ, Tenorio Jiménez C, et al. 25-hydroxyvitamin D levels in the early healing of osteoporotic Hip fracture and their relationship with clinical outcome. Nutr Hosp. 2020;37(2):327–334. doi:10.20960/nh.02427
12. Madsen CM, Jørgensen HL, Lind B, et al. Secondary hyperparathyroidism and mortality in Hip fracture patients compared to a control group from general practice. Injury. 2012;43(7):1052–1057. doi:10.1016/j.injury.2011.12.025
13. Fisher A, Goh S, Srikusalanukul W, Davis M. Elevated serum PTH is independently associated with poor outcomes in older patients with Hip fracture and vitamin D inadequacy. Calcif Tissue Int. 2009;85(4):301–309. doi:10.1007/s00223-009-9283-1
14. Toldy E, Salamon A, Kálmán B, Ágota K, Horváth D, Lőcsei Z. Prognostic relevance of circulating 25OHD fractions for early recovery and survival in patients with hip fracture (†). J Clin Med. 2018;7:8. doi:10.3390/jcm7080193
15. Salamon A, Hepp B, Mátrai A, et al. A csípőtáji csonttörést szenvedett betegek D-vitamin-ellátottsága [Vitamin D supply of patients with hip fracture]. Orv Hetil. 2014;155(17):659–668. Dutch. doi:10.1556/OH.2014.29878
16. Fisher A, Fisher L, Srikusalanukul W, Smith PN. Usefulness of simple biomarkers at admission as independent indicators and predictors of in-hospital mortality in older Hip fracture patients. Injury. 2018;49(4):829–840. doi:10.1016/j.injury.2018.03.005
17. Menéndez-Colino R, Alarcon T, Gotor P, et al. Baseline and pre-operative 1-year mortality risk factors in a cohort of 509 Hip fracture patients consecutively admitted to a co-managed orthogeriatric unit (FONDA Cohort). Injury. 2018;49(3):656–661. doi:10.1016/j.injury.2018.01.003
18. Schaller F, Sidelnikov E, Theiler R, et al. Mild to moderate cognitive impairment is a major risk factor for mortality and nursing home admission in the first year after Hip fracture. Bone. 2012;51(3):347–352. doi:10.1016/j.bone.2012.06.004
19. Fu G, Li M, Xue Y, et al. Rapid preoperative predicting tools for 1-year mortality and walking ability of Asian elderly femoral neck fracture patients who planned for Hip arthroplasty. J Orthop Surg Res. 2021;16(1):455. doi:10.1186/s13018-021-02605-0
20. Fu G, Li H, Wang H, et al. Comparison of peripheral nerve block and spinal anesthesia in terms of postoperative mortality and walking ability in elderly hip fracture patients - a retrospective, propensity-score matched study. Clin Interv Aging. 2021;16:833–841. doi:10.2147/CIA.S311188
21. Haugan K, Klaksvik J, Foss OA. 30-day mortality in patients after Hip fracture surgery: a comparison of the Charlson Comorbidity Index score and ASA score used in two prediction models. Injury. 2021;52(8):2379–2383. doi:10.1016/j.injury.2021.02.004
22. Zanker J, Duque G. Rapid geriatric assessment of hip fracture. Clin Geriatr Med. 2017;33(3):369–382. doi:10.1016/j.cger.2017.03.003
23. D’Andrea A, Le Peillet D, Fassier T, et al. Functional Independence Measure score is associated with mortality in critically ill elderly patients admitted to an intermediate care unit. BMC Geriatr. 2020;20(1):334. doi:10.1186/s12877-020-01729-y
24. Malhas L, Perlas A, Tierney S, Chan VWS, Beattie S. The effect of anesthetic technique on mortality and major morbidity after Hip fracture surgery: a retrospective, propensity-score matched-pairs cohort study. Reg Anesth Pain Med. 2019;44(9):847–853. doi:10.1136/rapm-2019-100417
25. Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10(2):150–161. doi:10.1002/pst.433
26. Cianferotti L, Parri S, Gronchi G, Civinini R, Brandi ML. The use of cholecalciferol in patients with Hip fracture. Clin Cases Miner Bone Metab. 2017;14(1):48–53. doi:10.11138/ccmbm/2017.14.1.048
27. Davidson CW, Merrilees MJ, Wilkinson TJ, McKie JS, Gilchrist NL. Hip fracture mortality and morbidity--can we do better? N Z Med J. 2001;114(1136):329–332.
28. Yoo S, Jang EJ, Jo J, et al. The association between hospital case volume and in-hospital and one-year mortality after Hip fracture surgery. Bone Joint J. 2020;102(10):1384–1391. doi:10.1302/0301-620X.102B10.BJJ-2019-1728.R3
29. Cancio JM, Vela E, Santaeugènia S, Clèries M, Inzitari M, Ruiz D. Influence of demographic and clinical characteristics of elderly patients with a Hip fracture on mortality: a retrospective, total cohort study in North-East Spain. Bone. 2018;117:123–129. doi:10.1016/j.bone.2018.09.002
30. Reiffel JA. Propensity score matching: the ‘devil is in the details’ where more may be hidden than you know. Am J Med. 2020;133(2):178–181. doi:10.1016/j.amjmed.2019.08.055
31. Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of Hip fracture: worldwide geographic variation. Indian J Orthop. 2011;45(1):15–22. doi:10.4103/0019-5413.73656
32. Danielson ME, Beck TJ, Lian Y, et al. Ethnic variability in bone geometry as assessed by Hip structure analysis: findings from the Hip strength across the menopausal transition study. J Bone Miner Res. 2013;28(4):771–779. doi:10.1002/jbmr.1781
33. Morin SN, Berger C, Liu W, et al. Differences in fracture prevalence and in bone mineral density between Chinese and White Canadians: the Canadian Multicentre Osteoporosis Study (CaMos). Arch Osteoporos. 2020;15(1):147. doi:10.1007/s11657-020-00822-4
34. Carlsson M, Wanby P, Brudin L, et al. Older Swedish adults with high self-perceived health show optimal 25-hydroxyvitamin D levels whereas vitamin D status is low in patients with high disease burden. Nutrients. 2016;8:11. doi:10.3390/nu8110717
35. Darling AL, Blackbourn DJ, Ahmadi KR, Lanham-New SA. Very high prevalence of 25-hydroxyvitamin D deficiency in 6433 UK South Asian adults: analysis of the UK Biobank Cohort. Br J Nutr. 2021;125(4):448–459. doi:10.1017/S0007114520002779
36. Pioli G, Lauretani F, Pellicciotti F, et al. Modifiable and non-modifiable risk factors affecting walking recovery after Hip fracture. Osteoporos Int. 2016;27(6):2009–2016. doi:10.1007/s00198-016-3485-y
37. Knechtle B, Nikolaidis PT. Vitamin D and Sport Performance. Nutrients. 2020;12(3):841. doi:10.3390/nu12030841
38. Remelli F, Vitali A, Zurlo A, Volpato S. Vitamin D deficiency and sarcopenia in older persons. Nutrients. 2019;11:12. doi:10.3390/nu11122861
39. Fakler JK, Grafe A, Dinger J, Josten C, Aust G. Perioperative risk factors in patients with a femoral neck fracture - influence of 25-hydroxyvitamin D and C-reactive protein on postoperative medical complications and 1-year mortality. BMC Musculoskelet Disord. 2016;17:51. doi:10.1186/s12891-016-0906-1
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
