Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Preoperative Patient Education Practices and Predictors Among Nurses Working in East Amhara Comprehensive Specialized Hospitals, Ethiopia, 2022
Authors Tadesse B, Kumar P, Girma N, Anteneh S, Yimam W , Girma M
Received 29 November 2022
Accepted for publication 19 January 2023
Published 25 January 2023 Volume 2023:16 Pages 237—247
DOI https://doi.org/10.2147/JMDH.S398663
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Beza Tadesse,1 Prem Kumar,1 Natnaiel Girma,1 Samuel Anteneh,1 Wondwossen Yimam,2 Mitaw Girma2
1Department of Adult Health Nursing, College of Medicine & Health Sciences, Wollo University, Dessie, Ethiopia; 2Department of Comprehensive Health Nursing, College of Medicine & Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Prem Kumar, Department of Adult Health, College of Medicine & Health Sciences, Wollo University, Dessie, Ethiopia, Email [email protected]
Background: The time before surgery is a traumatic period for patients. Despite this fact, no research has been conducted on nurses’ preoperative patient education in Ethiopia. This study aimed to assess preoperative patient education practices and associated factors among nurses working in East Amhara comprehensive specialized hospitals, Ethiopia, 2022.
Methods: A hospital-based cross-sectional study was conducted with 416 nurses. Pretested, structured questionnaires were used to collect the data. Bivariable analysis was performed for each independent variable with a P-value < 0.25 on the data imported to multivariate logistic regression analysis. AOR with a 95% CI and a P-value < 0.05 at a 5% level of significance were considered.
Results: Only 38.5% of nurses were found to have good practices for preoperative patient education, with a response rate of 98%. Nurses with 6 years of work experience (AOR = 3.15, 95% CI: 1.692– 5.874), adequate time (AOR = 2.33, 95% CI: 1.119– 4.889), training (AOR = 4.27, 95% CI: 1.548– 11.796), age 25– 29 (AOR = 0.15, 95% CI: 0.070– 0.331), age 30– 34 (AOR = 0.25, 95% CI: 0.137– 0.479), and knowledge (AOR = 3.73, 95% CI: 2.222– 6.273) were significantly associated.
Conclusion: Preoperative patient education practices among nurses were poor. Work experience, knowledge, training, and adequate time were found to be significant. Organize preoperative patient education programs for nurses that share experiences and provide ongoing training.
Keywords: East Amhara region, nurses, practices, preoperative education
Introduction
Patient education, as part of professional nurses’ education responsibilities, ensures that healthy knowledge, attitudes, behaviors, and habits are acquired by both healthy and sick people. Today’s patient education has recently shifted its emphasis from a concentration on illness pathophysiology and treatment to one that includes disease prevention, patient development, and the care of the patient’s family, as well as their involvement in care management.1 Preoperative patient education is defined as “providing the patient with health information, psychosocial support, and the opportunity to acquire particular skills before surgery”.2
The primary goal of pre-surgical education is to reduce patient suffering by raising awareness of the procedure, pain management strategies, postoperative discomfort, and anticipated signs of sepsis. Preoperative education has also been shown to reduce surgical illness and deaths, as well as unnecessary cancellations.3–5 Preoperative education benefits the patient in the alleviation of surgery-related anxiety, better postoperative pain control, more realistic patient expectations of surgery, lower lengths of hospital stays, higher rates of home discharges, and fewer telephone calls to surgeons’ offices postoperatively. This can benefit the patient and their families by encouraging them to undertake positive health actions and supporting their auto-decision-making and healthcare providers; the hospitals can do this by providing patients with health-related information, teaching them skills aimed at reducing discomfort and complications, and offering psychological support.2
Pre-operative education can benefit from surgical intervention in coping with the surgical economic burden and giving the patient satisfaction.7,8 Previous investigations have shown that effective communication can enhance patient outcomes such as comprehension, emotional well-being, and psychological adjustment.9 Nurses’ involvement is crucial in ensuring that patients are informed and accept the key elements of their treatment regimen.10 Particularly for individuals undergoing surgical operations, this is required. Patients receive information from nurses so they are informed about their expectations both before and after the surgical operation.11 Patient education can be improved by in-service training, preparing standard guidelines, enhancing continuing nursing education, and regular supportive supervision which is always an indispensable role in improving the quality of inpatient care.12 This is particularly essential for patients undergoing surgery. Patients receive information from nurses regarding preoperative procedures and surgical interventions.13,14
Ethiopian surgical nursing guidelines outline what patients and those concerned about them should know before surgical procedures. The main topics included ensuring psychological preparation, confirming physical preparation, ensuring informed consent, and conducting patient education. The procedure includes catheterization (which may be performed in the operating room), keeping the patient on Nil Per Orally (NPO), and removing all removable prostheses and ornaments for post-operative care.15 Preoperative patient education has been provided using a range of techniques, including written materials, spoken instruction, and audio-visual presentations, as well as one-on-one counseling or in-group discussions, or by combining some or all of these techniques.16 Before major surgery, the patient must be examined and advised on how to prepare for it.17 One of the most vital components of nursing care is educating patients and their families.18 Patients who had undergone inpatient care experienced extreme levels of pain; in the study about the “effect of different pre-operative education programs on the anxiety and pain levels of patients”, those who were seeking pre-surgical education had lower levels of pain and anxiety, as well as fewer complications.19 Preoperative instruction educates the patient about surgery as well as what to expect after the procedure.20
Globally, over 312.9 million surgical procedures are performed every year.21 Major complications after inpatient surgery have been reported to occur up to 22% of the time, with a death rate as high as 0.8%. Additionally, approximately one million patients can die due to complications following the surgery due to inadequate preoperative education, and approximately seven million patients a year will face major issues as a consequence of post-surgical intervention;22 Every five surgical patients in Africa, according to earlier studies from 25 nations for all inpatient surgeries, experienced a preoperative problem, and one-tenth of them died postoperatively because of this insufficient preoperative instruction.23
The healthcare system in Ethiopia is undergoing substantial expansion. Preoperative education has been delivered using a variety of techniques, including written materials, spoken instruction, and audio-visual presentations, as well as one-on-one counseling or in-group discussions, or by combining some or all of these. Although there is a lack of data on surgical outcomes, published statistics show a 7% all-cause surgical mortality rate.24 Distress and apprehension are more frequent psychosomatic reactions in patients awaiting anesthesia and surgery because, at Jima University and Gondar Hospital, surgery is perceived as a life-threatening event that causes significant anxiety among surgical preoperative educators. Patients also recognize mortality after surgery as the most important and dangerous point in their lives. Approximately 59.6% of surgical patients have preoperative anxiety linked to the dread of surviving anesthesia; 53.9% experience fear of mortality; 51.7% experience fear related to postoperative pain; and 43.3% experience concerns for their families. According to reports, among inpatient patients awaiting surgery, 60% to 80% may experience anxiety, and 5% may decide against the procedure.25
However, recent studies have shown that in Ethiopia, patients undergoing surgery still experience anxiety, feel less confident in post-surgical self-care, are less satisfied overall with their healthcare experience, and have increased lengths of hospital stay due to poor surgical outcomes. This is despite the Ethiopian Minister of Health’s recommendation to provide every patient undergoing surgery with preoperative education based on current evidence-based best practice research.24 Although there is a gap in the literature since no earlier studies have been conducted to demonstrate preoperative patient education techniques and associated factors for patients undergoing surgery in this subject area, this may be due to the quality of preoperative patient education practices. Preoperative education practices by nurses is precious for patients with surgical interventions in underdeveloped countries like Ethiopia, especially in hospitals with poor resource settings. In addition to this, the majority of previously conducted studies focused on patients, and most of them were single institution-based studies. Similarly, previous researchers used small samples, did not use validated instruments, and few did not conduct in-depth inferential analysis, some of them could have skewed their data sets. Whereas, in this study, the researcher adopted a multicentre approach to draw a better conclusion, and also incorporated all the nurses at the hospital where patients were treated.
This study aimed to identify how to improve preoperative patient education practices among nurses and revise the surgical nursing care guidelines. The findings of this study can be used by policymakers to develop effective approaches, such as regular training. It also aims to reduce and prevent anxiety and postoperative complications related to poor practices in preoperative surgical patient education practices. Consequently, the study aimed to evaluate preoperative patient education practices and predictors among nurses working in East Amhara comprehensive specialized hospitals in Ethiopia, 2022.
Conceptual Framework
After reviewing different studies conducted in the practice of preoperative patient education practices among nurses and its associated factors, the conceptual framework was developed (Figure 1).
 |
Figure 1 Conceptual framework on preoperative patient education practices and associated factors from a literature review. |
Methods and Materials
Study Area Design and Period
The research was conducted at three comprehensive specialized hospitals in the East Amhara regional state. Dessie Comprehensive Specialized Hospital is found in Dessie town, 400 km from Addis Ababa. It is the only multi-specialty hospital in South Wollo, giving services to around 8 million people in its catchment areas. This health facility is equipped with 400 beds in four major departments and other specialty units, and it has 800 health professionals. Debre Birhan Hospital is situated has 130 km from Addis Ababa and works for 2.8 million people in the catchment area in North Shoa, Oromia, and Afar. Woldia hospital is located in the North Wollo zone of Amhara regional state, 520 km away from the capital city, and serves around 3 million individuals, including some parts of Afar and Tigray. The hospital has around 490 health professionals. The researcher chose these hospitals because they are the only specialized health amenities that can receive and manage a large number of patients with different types of surgical operations. A hospital-based cross-sectional study design was implemented from July 15 to August 15, 2022.
Population
A total of 416 nurses who worked in the specialized, comprehensive, and specialized hospitals in the East Amhara region were selected randomly. All nurses employed during the data collection period were included; students and nurses who had not prepared patients for surgery for a year were excluded.
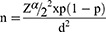
Sample Size Determination
The overall minimum sample size was determined by using single population proportion calculation formula with 50%.
By adding a 10% non-response rate = 39.
The final sample size is n=423 Where:
n = the required sample size
d = Margin of error between the sample and population=5% = 0.05
z = Standard normal distribution value at 95% confidence level zα/2=1.96 for 95% confidence interval
p = 50%.
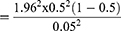
Sampling Technique and Procedure
The sample size for each hospital was computed by multiplying the total number of nurses for each hospital. Next, the total sample size was determined using a single mean formula, then divided by the total number of nurses in the three hospitals. n = Nf x nt/Nt. Then participants in each hospital used the proportional allocation formula. n=total sample size of each hospital. NF represents the total number of nurses in each hospital. Nt=total sample size calculated by using the single mean formula. Three N represents the total number of nurses (Figure 2).
 |
Figure 2 Schematic representation of the sampling procedure. |
Operational Definitions
Adequate Knowledge
Participants who scored knowledge-related questions with a score greater than or equal to the mean.26
Inadequate Knowledge
Respondents who scored above or equal to the mean score of knowledge questions.26
Good Practice
Participants who scored practice concerned questions with a score greater than or equal to the mean.27
Poor Practice
Respondents who scored below the mean score from the practice-related question.28
Training
There is formal and informal training regarding preoperative patient education practices.
Data Collection Tools and Procedure
A pretested, self-administered questionnaire was used to collect the data. The tool for the assessment of nurses’ sociodemographic characteristics was adapted by reviewing the literature, and it contains three open-ended and two multiple-choice questions. Tools for organizational factors, nurse-related factors, and practice were adapted by reviewing the literature of similar studies from previous years.28,29 The nurse-related factors and practice part of the questionnaire contained 39 Likert scale questions, to which responses were given on a 5-point Likert scale (strongly disagree, disagree, somewhat agree, agree, strongly agree). Finally, organizational factors contained five multiple-choice questions; the data were collected by three trained BSc nurses and supervised by two MScs.
Data Quality Control
The questionnaire was pretested on 5% of the nurses at Tibebe Ghion Specialized Hospital fifteen days before the final study. The validation of the tool was performed by experts in the field to assure the quality of the data. A tool for determining knowledge (nurse-related factors; (17 Likert scale questions), and practice (22 Likert scale questions) levels was determined by reviewing previous literature of similar studies. and the tool was validated by experts. Cronbach’s alpha tests for knowledge were 0.81 and 0.76, respectively, before and after the test. Cronbach’s alpha tests for practices were 0.72 and 0.87 for the pretest and posttest, respectively. The collected data were reviewed by the primary investigator and supervisors for consistency and completeness.
Data Processing and Analysis
Data were processed in Epi-data 4.6 before being exported to SPSS Version 26 for further analysis. Results were obtained by analyzing the association between the independent and dependent variables. Those variables with p-values less than 0.25 in the bivariable analysis were exported to the final model. A multivariable logistic regression analysis was carried out to see the relative effects of independent variables on the outcome variables. A p-value of less than 0.05 was taken as a cut-off point to declare a statistically significant association between independent and dependent variables. The Hosmer-Lemeshow test was used to evaluate whether the assumption for logistic regression is fulfilled or not and to evaluate model fitness. Multicollinearity diagnostics were to show that there was no value indicating the presence of multicollinearity between independent variables. And finally, the results were presented using texts, tables, and graphs.
Ethical Consideration
Ethical clearance was obtained from the Department of Adult Health Nursing and the College of Medicine and Health Sciences at Wollo University. Written informed consent was obtained from all the study participants. The code number was used to ensure the confidentiality of the participants. This study was carried out under the Helsinki Declaration’s ethical principles.
Results
Socio-Demographic Characteristics of the Study Participants
A total of 416 participants responded, with a response rate of 98%. Females made up 62% of the total. About 155(37.3%) of the participants’ ages fell within the range of 30–34 years. The participants’ average age was 31.84±5 SD. Among the study participants, 398(95.6%) held a bachelor’s degree or above. Half of the 228 participants (54.8%) had worked as nurses for less than or equal to five years, followed by 188 (45.2%) participants who had worked as nurses for ≥6 years, and finally, about 232(55.8%) participants had worked in the operation and surgical rooms for less than five years, followed by 184(44.2%) participants who had worked in the operation and surgical rooms for ≥6 years (Table 1).
 |
Table 1 Socio-Demographic Characteristics of the Study Participants in Study Settings from July 15 to August 15, 2022, Ethiopia (n=416) |
Nurse-Related Factors
Of the 416 study participants, 186 (44.7%) of the respondents had adequate knowledge regarding preoperative patient education practices (Figure 3).
 |
Figure 3 Knowledge level of nurses working in East Amhara region comprehensive specialized hospitals from July 15 To August 15, 2022, Ethiopia. |
Organizational Factors
Out of the 416 participants who responded, 209 (50.2%) had enough time to provide preoperative patient education practices, and 133 (32%) said they employed preoperative patient education practices checklists or guidelines. A translator is available for 110 (26.4) people who are experiencing a language barrier. Of the 145 individuals reported, 34.9% had pre-existing patient education practices training (Table 2).
 |
Table 2 Description of Organizational Factors Among Study Participants in Study Settings from July 15 to August 15, 2022, Ethiopia |
Preoperative Patient Education Practices
In this study, about 160 (38.5%) (95% CI: 32.7–43.3) of the participants had good practices regarding preoperative patient education practices (Figure 4).
 |
Figure 4 Preoperative patient education practices in East Amhara region comprehensive specialized hospitals from July 15 to August 15 in 2022, Ethiopia. |
With bivariable logistic regression analysis, the participant’s total working experience, working experience in the operation room and surgical room, following a preoperative guideline, having training, a language translator, having enough time for preoperative patient education practices, knowledge, and age were associated with preoperative patient education practices. Variables with p-values of less than 0.25 were exported to multivariable logistic regression. However, work experience, having enough time for preoperative patient education training, knowledge, and training, and ages 25–29 and 30–34 were significantly associated with the practice of nurses regarding preoperative patient education.
Nurses who had ≥ 6 years of working experience were 3.1 times more likely to teach good preoperative patient education practices than nurses who had less than 5 years of experience (AOR=3.15, 95% CI: 1.692–5.874). The odds of having enough time to provide preoperative patient education practices were 2.3 times greater than those who did not have enough time (AOR =2.33, 95% CI: 1.119–4.889). Respondents who had adequate knowledge were 3.7 times more likely to practice good preoperative education as compared to those with inadequate knowledge (AOR = 3.73, 95% CI: 2.222–6.273). Participants who had taken training were 4.2 times more likely to carry out good preoperative patient education practices than those who did not (AOR =4.27, 95% CI: 1.548–11.796). Respondents between the ages of 25–29 were 85% less likely to have a good preoperative education than those aged greater than or equal to 35 years (AOR=0.15,95% CI: 0.070–0.331). Participants who were in the age group of 30–34 were 75% less likely to have good preoperative patient education practices than those who were older or equal to 35 years (AOR = 0.25, 95% CI: 0.137–0.479) (Table 3).
Discussion
The study was intended to evaluate preoperative patient education practices and predictors among nurses. According to the study’s findings, 38.5% (32.7–43.3) of nurses used effective preoperative patient education practices. This implied that patients undergoing surgery were still at risk for anxiety and poor surgical results, and the majority (61.5%) of the nurses had poor preoperative patient education practices. This study’s proportion of effective preoperative patient education practice was higher than that of the Rwanda trial, which was 2.7%.8 The difference in this study was due to the variation in the study population because this research included all the nurses, whereas the study conducted in Rwanda included only perioperative nurses. Inconsistently, these results were lower than a study conducted in Nigeria.30 The possible discrepancies might be due to a lack of access to training, and this study included all nurses. Moreover, according to the mind-sponge theoretical view,31 the mindset of participants in preoperative patient education practices can also be influenced by individual perceptions, attitudes, and behaviors.
This study showed that those nurses who had adequate knowledge were significantly associated with good preoperative patient education practices as compared to nurses who had inadequate knowledge. These findings were consistent with studies conducted in Rwanda,32 Ibadan,33 Sudan,34 and Hong Kong.28,35 This effective explanation of the similarities between having adequate knowledge in both Rwanda and Ibadan is in line with the mind-sponge theory concepts.31
In this study, having training was significantly associated with good preoperative patient education practices. These findings were consistent with the research done in Turkey,6 China,38 and Hong Kong.35 This can be related to the increasing knowledge about the operation details and the specific perioperative care after attending the relevant surgical training courses; hence, they were much more eager and satisfied to use their newly equipped knowledge to teach and provide more preoperative information to patients. This implies that responsible bodies are prepared to provide service and in-service training programs for nurses on preoperative patient education practices, based on the latest evidence-based global and national guidelines. This study revealed that increasing the age of nurses was significantly associated with good preoperative patient education practice. This finding was in order with a study’s findings in Nigeria.29 As the age increased nurses had different exposure to procedures and they were known to have different and age direct relations with experience age increased experience also increasing.
This study found that those nurses who had enough time were significantly associated with good preoperative patient education practice as compared with those nurses who did not have enough time. This study was consistent with the studies done in Hong Kong35 and Saudi Arabia.36 The possible explanation could be a lack of time due to the high burden of surgical cases following at the current time, as nurses’ engagement in preoperative education and time constraints in clinical practice prevented nurses from performing any patient education activities. This possible explanation is supported by the World Bank report, “The Health Workforce in Ethiopia”, which shows Ethiopia is one of the countries with a very low health workforce, five times below the minimum threshold of 4.45 per 1000 population set by the World Health Organization to achieve the SDG Health.37
Preoperative patient education practices have significant health implications, most notably improving levels of surgical anxiety, emotional well-being, recovery time, prevention of post-surgical infections, treatment adherence, minimizing and adopting health-seeking behaviors, increasing patient satisfaction, lowering treatment costs,7,8 and improving patient education practices. In general, it helps to improve patients’ perioperative physical, physiological, and social derangements. Furthermore, it improves the overall quality of patients’ lives after surgical interventions. The findings of this study can be used by policymakers to develop effective approaches, such as regular training, developing guidelines, and continuing in-service education. Moreover, this is the first study from the Ethiopian perspective to date and is the benchmark proving this practice among nurses. The study’s findings advocate for additional research using a mixed method approach, multicentre studies at the zonal level, and a mind-sponge-based reasoning approach.
As a limitation, the study was conducted using only a cross-sectional quantitative study design, which might be insufficient to find all possible factors associated with preoperative patient education among nurses. In addition, the cause-and-effect relationship cannot be confirmed in this study since the research design was cross-sectional.
Conclusion
The nurses’ preoperative planning was inadequate. Preoperative education practices was significantly associated with work experience greater than or equals to 6 years, adequate knowledge, training, and adequate time for preoperative patient education practices. Organize experience-sharing and in-service training programs for nurses on topic, which are strongly recommended.
Funding
This research was sponsored and granted by Wollo University, whereas the institution does not provide a publication fee.
Disclosure
All the authors have declared no conflict of interest.
References
1. Niedzielski JK, Oszukowska E, Słowikowska-Hilczer J. Undescended testis - current trends and guidelines: a review of the literature. Arch Med Sci. 2016;12(3):667–677. doi:10.5114/aoms.2016.59940
2. Burgess LC, Arundel J, Wainwright TW. The effect of preoperative education on psychological, clinical and economic outcomes in elective spinal surgery: a systematic review. Healthcare. 2019;7:1. doi:10.3390/healthcare7010048
3. Elbashier IM, Shaaban KMA. Qualitative evaluation for cardiac surgical patients experience during psycho-educational sessions in Ahmaed Gassim cardiac center-2017. Nurs Primary Care. 2018;2(6):1–4. doi:10.33425/2639-9474.1087
4. Thorell A, MacCormick A, Awad S, et al. Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg. 2016;40(9):2065–2083. doi:10.1007/s00268-016-3492-3
5. Swartz JS, Amos KE, Brindas M, Girling LG, Ruth Graham M. Benefits of an individualized perioperative plan for children with autism spectrum disorder. Paediatr Anaesth. 2017;27(8):856–862. doi:10.1111/pan.13189
6. Pelkowski JN, Yoon SL, Adams S. Benefits of implementation of preoperative education classes for Hip and knee arthroplasty. Curr Orthop Pract. 2021;32:112–117. doi:10.1097/BCO.0000000000000959
7. Vuong QH. Be rich or don’t be sick: estimating Vietnamese patients’ risk of falling into destitution. SpringerPlus. 2015;4(1):529. doi:10.1186/s40064-015-1279-x
8. Vuong QH. Sociodemographic factors influencing Vietnamese patient satisfaction with healthcare services and some meaningful empirical thresholds. Iran J Public Health. 2018;47(1):119–126.
9. Almoajil H, Theologis T, Dawes H, et al. Patients’ and parents’ views about lower limb orthopaedic surgery for ambulant children and young people with cerebral palsy: a qualitative evidence synthesis. J Child Orthop. 2020;14(6):562–573. doi:10.1302/1863-2548.14.200139
10. Head BA, Song MK, Wiencek C, Nevidjon B, Fraser D, Mazanec P. Palliative nursing summit: nurses leading change and transforming care: the nurse’s role in communication and advance care planning. J Hosp Palliat Nurs. 2018;20(1):23–29. doi:10.1097/NJH.0000000000000406
11. Mitchell M. Day surgery nurses’ selection of patient preoperative information. J Clin Nurs. 2017;26(1–2):225–237. doi:10.1111/jocn.13375
12. Chaghari M, Saffari M, Ebadi A, Ameryoun A. Empowering education: a new model for in-service training of nursing staff. J Adv Med Educ. 2017;5(1):26–32.
13. Carli F, Silver JK, Feldman LS, et al. Surgical prehabilitation in patients with cancer: state-of-the-science and recommendations for future research from a panel of subject matter experts. Phys Med Rehabil Clin N Am. 2017;28(1):49–64. doi:10.1016/j.pmr.2016.09.002
14. Gröndahl W, Muurinen H, Katajisto J, Suhonen R, Leino-Kilpi H. Perceived quality of nursing care and patient education: a cross-sectional study of hospitalised surgical patients in Finland. BMJ Open. 2019;9(4):e023108. doi:10.1136/bmjopen-2018-023108
15. Evered L, Silbert B, Knopman DS, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Anesthesiology. 2018;129(5):872–879. doi:10.1097/ALN.0000000000002334
16. Aranha PR, Dsouza SN. Preoperative information needs of parents: a descriptive survey. J Res Nurs. 2019;24(5):305–314. doi:10.1177/1744987118821708
17. Bergsträsser E, Cignacco E, Luck P. Health care professionals’ experiences and needs when delivering end-of-life care to children: a qualitative study. Palliat Care. 2017;10:1178224217724770. doi:10.1177/1178224217724770
18. Yeola M, Jaipuriya P. Effect of pre-operative counselling on post-operative outcome in hernia surgery patients. Int J Sci Res. 2016;5(7):762–767.
19. Steenhagen E, van Vulpen JK, van Hillegersberg R, May AM, Siersema PD. Nutrition in peri-operative esophageal cancer management. Expert Rev Gastroenterol Hepatol. 2017;11(7):663–672. doi:10.1080/17474124.2017.1325320
20. Abd El GwadElkalashy R, Masry S. The effect of preoperative educational intervention on preoperative anxiety and postoperative outcomes in patients undergoing open cholecystectomy. BJU Int. 2018;117(1):62–71.
21. Dencker EE, Bonde A, Troelsen A, Varadarajan KM, Sillesen M. Postoperative complications: an observational study of trends in the United States from 2012 to 2018. BMC Surg. 2021;21(1):393. doi:10.1186/s12893-021-01392-z
22. Dmitri Nepogodiev AB, Glasbey JC, Elizabeth L, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38.
23. Melekie TB, Getahun GM. Compliance with surgical safety checklist completion in the operating room of University of Gondar Hospital, Northwest Ethiopia. BMC Res Notes. 2015;8(1):361. doi:10.1186/s13104-015-1338-y
24. Nigussie S, Belachew T, Wolancho W. Predictors of preoperative anxiety among surgical patients in Jimma University Specialized Teaching Hospital, South Western Ethiopia. BMC Surg. 2014;14(1):67. doi:10.1186/1471-2482-14-67
25. Woldegerima YB, Fitwi GL, Yimer HT, Hailekiros AG. Prevalence and factors associated with preoperative anxiety among elective surgical patients at University of Gondar Hospital. Gondar, Northwest Ethiopia, 2017. A cross-sectional study. Int J Surg Open. 2018;10:21–29.
26. Aliyu D, Adeleke IT, Omoniyi SO, et al. Knowledge, attitude and practice of preoperative visit: a survey of Nigerian perioperative nurses. Am J Health Res. 2014;3(1):54–60. doi:10.11648/j.ajhr.s.2015030101.18
27. Oyetunde MO, Akinmeye AJ. Factors influencing practice of patient education among nurses at the University College Hospital, Ibadan. Open J Nurs. 2015;5(05):500. doi:10.4236/ojn.2015.55053
28. Almashi AM, Almutary HH, Mersal NA. Essential elements of preoperative information as perceived by the nurses in surgical units: scoping review. Evid Based Nurs. 2020;2:3. doi:10.47104/ebnrojs3.v2i3.130
29. Aliyu D, Adeleke IT, Omoniyi SO, Kolo S, Odofin OM, EssienEkaete P. Knowledge, attitude and practice of preoperative visit: a survey of Nigerian perioperative nurses. Am J Health Res. 2015;3(1):54–60.
30. Akinsulore A, Owojuyigbe AM, Faponle AF, Fatoye FO. Assessment of preoperative and postoperative anxiety among elective major surgery patients in a tertiary hospital in Nigeria. Middle East J Anaesthesiol. 2015;23(2):235–240.
31. Vuong QH. Mindsponge Theory. Walter de Gruyter GmbH; 2023:214.
32. Mariza D. Knowledge, Practices and Barriers of Preoperative Patients Teaching Among Nurses Working in Operating Theatres at Referral Teaching Hospitals in Rwanda. University of Rwanda; 2019.
33. Sibhatu MK, Taye DB, Gebreegziabher SB, Mesfin E, Bashir HM, Varallo J. Compliance with the World Health Organization’s surgical safety checklist and related postoperative outcomes: a nationwide survey among 172 health facilities in Ethiopia. Patient Saf Surg. 2022;16(1):1–7. doi:10.1186/s13037-022-00329-6
34. Al Amine Ali ES, Ahmed Abdallah HM. Effect of preoperative preparation on patients outcome among patients undergoing surgical operations at Almik Nimir Hospital – Sudan. Int J Res. 2020;8(8):346–355. doi:10.29121/granthaalayah.v8.i8.2020.441
35. Lee CK, Lee IF. Preoperative patient teaching: the practice and perceptions among surgical ward nurses. J Clin Nurs. 2013;22(17–18):2551–2561. doi:10.1111/j.1365-2702.2012.04345.x
36. Ashwaq M. Essential elements of preoperative information as perceived by the nurses in surgical units. Afr J Online. 2020;2(3). doi:10.47104/ebnrojs3.v2i3.130
37. Owolabi EO, Mac Quene T, Louw J, Davies JI, Chu KM. Telemedicine in surgical care in low- and middle-income countries: a scoping review. World J Surg. 2022;46(8):1855–1869. doi:10.1007/s00268-022-06549-2
38. Yu J, Zhang Y, Yu T, et al. Preoperative anxiety in Chinese adult patients undergoing elective surgeries: a multicenter cross-sectional study. World J Surg. 2022;46(12):2927–2938. doi:10.1007/s00268-022-06720-9
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.