Back to Journals » International Journal of General Medicine » Volume 14
Premature Mortality Due to Tobacco-Related Malignancies in Poland
Authors Moryson W , Stawinska-Witoszynska B
Received 19 March 2021
Accepted for publication 10 May 2021
Published 31 May 2021 Volume 2021:14 Pages 2171—2182
DOI https://doi.org/10.2147/IJGM.S310416
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Waclaw Moryson, Barbara Stawinska-Witoszynska
Department of Epidemiology and Hygiene, Chair of Social Medicine, Poznan University of Medical Sciences, Poznan, 60-806, Wielkopolska, Poland
Correspondence: Waclaw Moryson Email [email protected]
Introduction: Although in Poland at the turn of the 20th and 21st centuries, tobacco consumption per capita was one of the highest in the world as a result of specific political and social conditions, nicotinism was the most common preventable cause of death that reduced life expectancy by 10 years on average. The aim of this study is to determine the level of premature mortality and its trends by age and sex for tobacco-related malignancies in Poland in the years 2008– 2017.
Methods: The standardised premature mortality rates as well as mortality rates for five-year age ranges according to the patients’ sex were used. The Joinpoint model was used to determine the time trends.
Results: Premature mortality due to all tobacco-dependent cancers analysed decreased in Poland throughout the analysed period in both male (2.5% per year) and female (1% per year) populations. A detailed analysis of individual diseases showed that a decrease in premature mortality was observed for almost all malignancies with the exception of malignant liver cancer among males, malignant oesophageal cancer among females and malignant lip, oral cavity and oropharyngeal cancer in both sexes. The reduction in mortality from all tobacco-related cancers in the male population was greatest between 40 and 44 years of age, reaching 5.6% year on year. Similarly, in the case of females, the decline in mortality was greater in the younger age cohorts and decreased in those aged over 50.
Conclusion: The favourable phenomenon of decreasing the level of premature mortality caused by tobacco-related malignancies may be associated, among others, with the policy of primary prevention of these diseases in the form of a widespread ban on smoking in public places, intensive information campaigns on the harmfulness of tobacco smoking and increasing taxation on tobacco products.
Keywords: premature mortality, cancer, smoking, epidemiology
Introduction
Nicotinism is the most common preventable cause of death worldwide. According to the World Health Organization, diseases caused by smoking kill more than 8 million people worldwide each year. More than 7 million die because of active smoking, and about 1.2 million die due to passive exposure to tobacco smoke.1 Smoking and the diseases it causes are estimated to reduce life expectancy by an average of 10 years, contributing significantly to premature mortality, ie, an increase in the number of deaths in a population before reaching the conventionally defined threshold of old age.2 Tobacco-related diseases, which are responsible for the increased mortality in the population exposed to tobacco smoke, include cancer, cardiovascular diseases and respiratory diseases.3
Since the early 20th century, the rapid increase in smoking prevalence, in addition to increased life expectancy and declining mortality from other causes, has made mortality from malignant cancers an increasingly common phenomenon.4 According to World Health Organization reports, malignancies, including tobacco-related cancers, are now the most common cause of death before the age of 70 in the Polish population.5
While there is a general awareness of the issue of premature mortality resulting from the most common smoking-related cancers, such as lung cancer, less attention has been paid to the less common tobacco-related cancers.
This study’s main objective was to determine the level of premature mortality and its trends by sex and age for cancers of the lip, oral cavity and pharynx, oesophagus, liver, larynx, and acute myeloid leukaemia in Poland in 2008–2017. All deaths of people before 65 years of age were classified as premature deaths. The authors also assessed the incidence of deaths and determined premature mortality trends in men and women due to all tobacco-related malignancies according to sex and age in the same period. This publication presents some of the findings on changes in premature mortality due to tobacco-related diseases in Poland.6
Materials and Methods
This study analysed all deaths of people under 65 years of age registered in Poland between 2008 and 2017. The data on the number of deaths and the population’s size in the analysed age ranges were obtained from the Central Statistical Office. The analysis of time trends takes into account a summary of all deaths where tobacco-related cancer was identified as the underlying cause of death: malignant neoplasms of the lip, mouth and throat (C00-C14), oesophagus (C15), stomach (C16), large intestine (C18-C21), liver (C22), pancreas (C25), larynx (C32), trachea, bronchus and lung (C33-C34), cervix (C53), urinary tract (C64-C67) and acute myeloid leukaemia (C92. 0).4 Subsequently, a separate analysis was conducted on premature mortality caused by selected malignant neoplasms - the lip, oropharynx, oesophagus, liver, pancreas, larynx, and acute myeloid leukaemia, taking into account gender and age. The diagnoses were classified according to the International Statistical Classification of Diseases and Health Problems (ICD-10).7
To analyse the mortality of male and female populations under 65, the authors used the mortality rates standardised based on the 2013 European standard population and crude death rates for age groups.8 The mortality trends were determined for the five-year age ranges (20–24, 25–29, 30–34, 35–39,40–44, 45–49, 50–54, 55–59, 60–64 years of age), taking into account the division by the gender.
The Joinpoint model was used to determine time trends in mortality. The model constitutes a particular version of linear regression, presenting time trends through a segmented curve consisting of the sections that join at points where a change in the time trend is significant. The Joinpoint method has proven its value only in descriptive analyses, such as the ones carried out in our study; it cannot be used for multivariate analyses. The Joinpoint model was used to calculate the average annual percentage change in premature mortality due to the analysed cancers and to determine whether the trend dynamics of mortality changed in the analysed period of time. If a year was identified when a change in the trend dynamics was observed, then information on the annual percentage change in mortality before and after that year was provided. The analysis was conducted with the minimum number of zero joinpoints (straight line), followed by tests for the model fitted with a maximum of one joinpoint. The Monte Carlo Permutation method for tests of significance was used. The homoscedasticity model was selected (errors are assumed to have constant variance). Using the Monte Carlo Permutation technique with 4499 randomly selected data sets, the numbers and locations of the joinpoints, with the best-fitted models for mortality trend, were estimated. Based on the calculated models, annual percentage change (APC) between points and average annual percentage change over the whole analysed period were determined for mortality rates.9 The Joinpoint results are not shown for some subgroups because at least in one year from the analysed range, the number of deaths due to analysed disease was zero. A statistical software, Joinpoint Regression 4.7.0.0 (US National Cancer Institute, Bethesda, United States of America), served to determine the regression models. For the annual percentage change (APC) as well as for the average annual percentage change (AAPC), a 95% confidence interval (95% CI) was determined, and a value of p<0.05 was assumed as the level of relevance.
Results
In Poland, all tobacco-related malignancies caused 7014 premature deaths in women and 14,988 in men, accounting for 21% of all premature deaths in women and 18.1% in men in 2008. In the same year, cancers analyzed in this study were responsible for 1384 (4.1%) premature deaths in women and 4024 (4.9%) in men (Table 1). The total number of premature deaths due to cancers of the lip, oropharynx, oesophagus, liver, larynx and acute myeloid leukaemia accounted for just over half the number of premature deaths from malignant lung cancers alone (Table 1).
 |
Table 1 Premature Deaths Due to Tobacco-Related Malignancies in Poland in 2008 (The First Year of the Study) by Gender (Absolute Numbers, %) |
For most of the cancers analysed, as with other tobacco-related cancers, around 90% of premature deaths occur between the ages of 50 and 65 (Table 2). It is notable that for all cancers and all age groups (in which mortality was not incidental) mortality rates are higher for men (Table 2).
 |
Table 2 Premature Mortality Due to the Analysed Cancers by Gender and Age in Poland in 2008 (Standardised Rates According to ESP2013) |
Due to tobacco-related cancers, the total premature mortality declined in Poland over the entire period analysed for both the male and female populations. Among males, the decline in the standardised mortality ratio amounted to 2.5% per year, and in the female population, the ratio remained stable between 2008 and 2014 and then began to decline by 2.7% per year (Table 3).
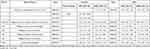 |
Table 3 Time Trends of Premature Mortality Rates Due to the Analysed Malignancies and All Tobacco-Related Malignancies in Total in Poland, 2008–2017 |
The level of premature mortality due to selected malignant neoplasms or a group of malignant neoplasms, as in the case of malignant cancers of the lip, oral cavity and pharynx among men, showed a decrease except for the latter group of malignant cancers as well as malignant liver cancer. The most rapid decrease was observed in premature mortality caused by malignant laryngeal tumours (3% per year) and acute myeloid leukaemia (2.7% per year). Premature mortality due to malignant cancers of the lip, oral cavity and pharynx increased by 0.9% per year, while for malignant cancers of the liver by 1.2% per year. Time trends in mortality due to all the analysed malignancies in the male population did not change throughout the entire analysed period(Table 3).
In the female population, a decrease in premature mortality was observed in the case of all analysed diseases with the exception of malignant tumours of the lip, oral cavity and pharynx and oesophagus. The most rapid decrease in premature mortality was observed due to cancers of the larynx (2% per year) and the liver (1.9% per year). Premature mortality due to cancers of the lip, oral cavity and pharynx increased by 3% per year, and for malignant cancers of the oesophagus, the increase was 0.7% per year. Similarly to the male population, the time trends in mortality due to all analysed malignant cancers did not change throughout the entire analysed period (Table 3).
The reduction in premature mortality due to all tobacco-related cancers in the male population was most significant between 40 and 44, reaching 5.6% annually. In the following older age groups, a decrease in mortality was also observed, but the dynamics were smaller, amounting to 1.3% per year in the oldest male group analysed. Similarly, in the case of women, the decrease in mortality was more significant in the younger age groups and decreased in the groups above 50 years of age. In two groups of females (55–59 and 60–64), the mortality rates increased in the first half of the decade analysed, by 0.3% per year and 2.7% per year, respectively. Since 2013, for women aged 55–59, and since 2014 for those aged 60–64, an annual decrease in mortality rates of 3.1% and 1.7%, respectively, was observed (Table 4).
 |
 |
 |
Table 4 Time Trends in Premature Mortality in the Population of Poland Due to Total Tobacco-Related Cancers and the Other Cancers Analysed According to the Five-Year Age Groups, 2008–2017 |
The results of the analysis of mortality trends due to individual tobacco-related malignancies by age group are presented below.
Malignant Cancers of the Lip, Oropharynx and Pharynx
The highest decrease of mortality (c.a. 4% per year) due to malignant cancers of the lip, oropharynx and pharynx was observed among men between 30 and 39 years of age. With age, the dynamics of the mortality decrease declined, and in the oldest age groups, ie 55–59 and 60–64 years, an increase in mortality was observed. Most age groups in the female population showed an increase in mortality, reaching as much as 5.8% per year among 40–44-year-old women and 4.9% in the 60–64 age group. Only the 30–34 and 45–49 age groups showed a decreasing trend, with mortality rates declining by 3.7% and 1.6% per year, respectively. (Table 4).
Malignant Tumours of the Oesophagus
The decrease mortality in males under 59 years of age, depending on the age group, ranged between 3.2% and 1% per year, while in those aged 60–64, the decrease was not significant. In the female population, mortality increased in all age groups except 50–54 years. The small increase in mortality among women between 60 and 64 years of age, of 0.1% per year, is noteworthy (Table 4).
Malignant Cancers of the Liver
Due to these malignancies, among men over 50 years of age there was an increasing premature mortality trend of approximately 2% per year for 50–59-year-olds and 0.9% for 60–64-year-olds, respectively. Among women between 45 and 54, there was a shift to an increasing mortality trend since 2013. In the older age groups, 55–59 and 60–64, the trend was downward, by 4% and 0.7% per year, respectively (Table 4).
Malignant Cancers of the Pancreas
In the female and male populations under 60, a significant decrease in premature mortality was observed, reaching up to 7% per year. Among the male population between 60 and 64 years of age, the mortality remained stable, while in the female population, it increased by 0.7% per year (Table 4).
Malignant Cancers of the Larynx
A decreasing trend in mortality was observed in both sexes under 60 (5% per year). In the 60–64 age group, the reduction in mortality among men was 0.3% per year, while in the group of women, an increase in mortality of 2% per year was observed (Table 4).
Acute Myeloid Leukaemia
Among males, the highest decrease in mortality occurred in the group between 20 and 24 years of age and between 35 and 39. It amounted to respectively 9.5% and 7.1% per year. The only age group among the males in which an increase in mortality was observed was the group between 25 and 29 years of age (0.9% per year). In the male population between 40 and 50 years of age, the decrease in mortality was 5% per year and it decreased in the older age groups, reaching 1.2% per year in the 60–64 group. Among females between 45 and 55, the mortality rate decreased by about 2% per year. In the older age groups, an increase in mortality was observed. It amounted to 0.6% per year among 55 to 59-year-old women, and to 1.2% per year in the oldest of the analysed age groups (Table 4).
Discussion
Poland belongs to the European countries, with one of the highest mortality rates due to cancer. While in Western European countries, a decline in mortality due to malignant tumours was observed as early as the 1980s, in Poland, it began to decline only at the turn of the 20th and 21st centuries.10,11 One of the factors responsible for this phenomenon was the different course of Poland’s nicotinism epidemic compared to that of Western European countries.12,13 In those countries, as well as in many other highly developed ones, ie, the USA, Canada or Japan, the highest prevalence of smoking took place in the 1950s and 1960s,14–17 however, due to early medical reports on the harmfulness of smoking tobacco,18–21 the 1960s saw a decline in the number of smokers.14,16,22 In Poland, however, as in other Central and Eastern European countries, the spread of nicotinism continued into the 1980s. Over the following years, cigarette consumption remained high, with a decline only beginning in the second half of the 1990s.10
In order to reduce mortality caused by tobacco-related diseases, including tobacco-related malignancies, in 2008, Poland ratified the World Health Organization’s MPOWER tobacco control strategy. It introduced several anti-tobacco measures, including a ban on smoking in public places, active tobacco counselling, warning about the harmful effects of tobacco, a ban on tobacco advertising, and increased tobacco taxes.23 Successive implementation of the solutions proposed by WHO resulted in a decrease in the prevalence of nicotinism in Poland between 2009 and 2017 among men from 32% to 29%, and in the case of women from 24% to 20%, according to the Chief Sanitary Inspectorate. Moreover, there was a decrease in passive exposure to tobacco smoke.24 However, it should be noted that despite the decline of smoking in Poland, it remains at a relatively high level, still ranking Poland among the countries with one of the highest smoking rates in Europe.25
Nonetheless, between 2008 and 2017, mortality caused by tobacco-related cancers declined faster in Poland among those aged under 65 than the mortality due to cancer in most European countries. That was more than two decades since smoking prevalence began to decline. Premature mortality due to tobacco-related cancers in males declined by 2.6% per year in Poland, while mortality in Europe among the 35–64 year-olds declined by an average of 1.7% per year between 1993 and 2009. In the female population, the decline in premature mortality in Poland (AAPC 1%) was at the same level as the European average between 1993 and 2009.11
A detailed analysis of individual diseases showed that a reduction in premature mortality was recorded for almost all malignant neoplasms. The exceptions were malignant cancers of the liver among men, malignant cancers of the oesophagus among women and malignant cancers of the lip, oral cavity and throat in both sexes.
Premature mortality due to malignant neoplasms of the lip, mouth and oropharynx was increasing in both sexes, despite a decrease in the prevalence of smoking and the stable levels of alcohol consumption which are the factors attributed to be responsible for 75% of all cases of these cancers at the end of the 20th century.26,27 An increase in mortality from malignant tumours of the lip, mouth and throat also occurred in other central and western European countries and parts of southern Europe.28 This trend is now being linked to risk factors other than alcohol and tobacco. It is estimated that 38% of oral and pharyngeal malignancies in Central Europe are due to HPV infection.29
In the case of mortality due to oesophageal cancers in the male population, an upward trend was observed in Poland until the end of the 20th century, which was reversed during the analysed period. A similar decline in male mortality in the pre-65 population was observed earlier in Western European countries, eg in France since the 1980s.30 Premature mortality of females due to oesophageal cancer in Poland, as in other European countries, remains stable and at a low level.30
In Poland, over the period in question, a clear decrease in premature mortality due to malignant liver tumours was observed in the female population. In contrast, premature mortality in males remained stable The analysis of premature mortality for 34 European countries in total shows a plateau between 1995 and 2010 in both sexes.11 However, the situation was different in different parts of Europe. Despite a lack of data on premature mortality in individual countries, mortality results showed an increase in Western and Northern European countries, where mortality from liver cancer remained low. Simultaneously, it declined in Central and Eastern European countries, where mortality from liver cancer was higher. The increase in mortality in Western and Northern Europe was attributed to the increase in HCV infections and the prevalence of obesity and diabetes.31,32 The reduction in mortality in Eastern European countries, on the other hand, was explained by a lower number of HBV infections.33
It is estimated that 30% of pancreatic malignancies could be avoided by giving up smoking.34 In Poland, as in other European countries, mortality due to pancreatic cancer is significantly higher than the world average. During the analysed decade, premature mortality in Poland decreased in both male and female populations. The observed trend was consistent with mortality trends from 2005–2015 in countries where the decline in smoking prevalence occurred much earlier, eg, the United Kingdom. However, in some European countries, eg Greece, despite the observed decrease in tobacco consumption, mortality from pancreatic cancer is increasing. This phenomenon is attributed to other factors like obesity, diabetes and lack of physical activity.35
Mortality from laryngeal cancer in Western European countries, after years of increase, reached a plateau in the late 1980s and early 1990s and then began to decline. In Eastern and Central European countries, such as Poland, the mortality level declined only at the beginning of the 21st century. In the analysed period of 2008–2017, the decline in premature mortality due to laryngeal malignancies had similar dynamics to the decline in mortality in the group between 35 and 64 years of age in other European countries over the period 2006–2012.36
The present analysis shows a reduction in premature mortality due to acute myeloid leukaemia, which is consistent with earlier reports on the decrease in mortality rates due to that cause in both sexes in Poland between 1990 and 2010. At that time, it was pointed out that this decrease in mortality was mainly due to lower mortality in children and young adults.37 In other European countries, similar declining mortality trends were observed since the 1980s.11
The analysis of time trends for the malignancies under consideration in particular age groups showed a greater decrease in premature mortality before the age of 55. With age, in male and female patients, the dynamics of mortality decrease declined, especially as regards laryngeal and pancreatic cancer. The observed phenomenon may be partly explained by gradual changes in lifestyle, which have been observed since the beginning of the political transformation in Poland. Enriching the diet with vegetable products, changing drinking patterns, taking actions limiting the exposure to carcinogens at work and, above all, decreasing tobacco consumption by men and women, have all been described in Poland since the 1990s, and the scale of these changes has been increasing.24,38–41 It therefore seems clear that younger people are the main beneficiaries of the changes described.
In addition, it should be noted that the results of the present analysis conducted for neoplastic diseases are consistent with the results of previous studies of premature mortality in Poland conducted for COPD.6
Strengths and Limitations of the Study
Nationwide coverage of the data and the size of the study population were among the advantages of the data analysis. A limitation, on the other hand, is the use of secondary sources of information, ie data on deaths from death certificates. These data may be affected by error. For example, according to the Central Statistical Office and the National Institute of Public Health and Hygiene, almost half of all cardiovascular deaths in Poland (46.7%) were related to the use of the so-called “garbage codes” defined by the WHO.42,43 Nevertheless, it should be emphasised that in the case of data on cancer deaths in Poland, the data have been assessed by the WHO as high quality records.44
Additionally, it is noteworthy that this work is designed as a descriptive epidemiological study. It aims to describe the trends in premature mortality due to malignancies in Poland. The methodology used does not make it possible to show a cause-and-effect correlation between any risk factors and reduced premature mortality. However, the results of the above analysis indicate that subsequent preventive health care decisions in Poland have ensured the continuation of the downward trend in premature mortality due to cancers observed since the early 1990s. Cigarette smoking is one of the important risk factors for analysed cancers whose changes have been observed in Poland over the past 25 years.22
Scope for Future Study
Along with the reduction in exposure to tobacco smoke, more attention is being paid to other risk factors that play an increasing role in the development of the so-called tobacco-related diseases. A reduction in mortality due to malignant neoplasms of the lip, oral cavity and pharynx seems possible with the continuation of smoke-free policies and the implementation of other preventive actions, such as universal vaccination against oncogenic HPV types. A decrease in mortality due to oesophageal cancer may be brought about by a reduction in obesity in the population, while mortality due to malignant liver cancer may be brought about primarily by prophylaxis of HBV infection in the form of vaccination of those not yet vaccinated and by early effective treatment of hepatitis C.
Conclusions
- The study showed a decreasing trend of premature mortality due to all tobacco-related malignancies in Poland between 2008 and 2017 for both sexes and for the younger age groups who were already affected by political changes that had the potential to change people’s lifestyles.
- In the case of selected cancers, no reduction in premature mortality was found only for malignant liver cancer in males, malignant oesophageal cancer in females and malignant cancers of the lip, mouth and throat in both sexes.
- The advantageous phenomenon of decreasing premature mortality caused by tobacco-dependent malignancies may be associated, among other things, with the ongoing primary prevention of these diseases in the form of a widespread ban on smoking in public places, intensive information campaigns on the harmful effects of smoking and the increased taxation of tobacco products.
- The range of preventive measures should target all cancer risk factors (including obesity, poor diet, viral infections and environmental pollution).
Data Sharing Statement
Data available in a publicly accessible repository that does not issue. DOIs Publicly available datasets were analysed in this study. This data can be found here: http://demografia.stat.gov.pl/bazademografia/Tables.aspx.
Ethics Statement
The study has been exempted from requiring ethical approval by Ethics Committee of the Poznan University of Medical Sciences.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors reported no conflicts of interest for this work and declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. World Health Organization, Bloomberg Philanthropies. WHO Report on the Global Tobacco Epidemic, 2017: Monitoring Tobacco Use and Prevention Policies; 2017.
2. Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341–350. doi:10.1056/NEJMsa1211128
3. Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368(4):351–364. doi:10.1056/NEJMsa1211127
4. National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking—50 years of progress: a report of the surgeon general. Centers for Disease Control and Prevention (US); 2014. Available from: http://www.ncbi.nlm.nih.gov/books/NBK179276/.
5. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
6. Moryson W, Stawinska-Witoszynska B. Premature mortality due to Chronic Obstructive Pulmonary Disease (COPD) in Poland. Medicina. 2021;57(2):126. doi:10.3390/medicina57020126
7. World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems. World Health Organization; 2011.
8. Pace M, Cayotte E, Agafitei L, et al. Revision of the European Standard Population: Report of Eurostat’s Task Force.
9. Yu B, Huang L, Tiwari RC, Feuer EJ, Johnson KA. Modelling population-based cancer survival trends by using join point models for grouped survival data. J R Stat Soc Ser a Stat Soc. 2009;172(2):405–425. doi:10.1111/j.1467-985X.2009.00580.x
10. World Health Organization. The Current Status of the Tobacco Epidemic in Poland; 2009.
11. Bosetti C, Bertuccio P, Malvezzi M, et al. Cancer mortality in Europe, 2005–2009, and an overview of trends since 1980. Ann Oncol. 2013;24(10):2657–2671. doi:10.1093/annonc/mdt301
12. Postawy-Polaków-do-palenia-tytoniu-Raport-2017.pdf. Available from: https://gis.gov.pl/wp-content/uploads/2018/04/Postawy-Polak%C3%B3w-do-palenia-tytoniu-Raport-2017.pdf.
13. Lopez AD, Collishaw NE, Piha T. A descriptive model of the cigarette epidemic in developed countries. Tob Control. 1994;3(3):242–247. doi:10.1136/tc.3.3.242
14. Giovino GA, Shelton DM, Schooley MW. Trends in cigarette smoking cessation in the United States. Tob Control. 1993;2(Suppl1):
15. Reid J, Hammond D, Tariq U. Tobacco Use in Canada: Patterns and Trends.
16. Wald NJ, Nicolaides-Bouman A; St. Bartholomew’s Hospital (London, England), eds. UK Smoking Statistics.
17. Funatogawa I, Funatogawa T, Yano E. Trends in smoking and lung cancer mortality in Japan, by birth cohort, 1949–2010. Bull World Health Organ. 2013;91(5):332–340. doi:10.2471/BLT.12.108092
18. Calle EE, Rodriguez C, Jacobs EJ, et al. The American Cancer Society Cancer Prevention Study II nutrition cohort: rationale, study design, and baseline characteristics. Cancer. 2002;94(2):500–511. doi:10.1002/cncr.10197
19. Kannel WB. Factors of risk in the development of coronary heart disease—six-year follow-up experience: the Framingham Study. Ann Intern Med. 1961;55(1):33. doi:10.7326/0003-4819-55-1-33
20. Doll R, Hill AB. The mortality of doctors in relation to their smoking habits. BMJ. 1954;1(4877):1451–1455. doi:10.1136/bmj.1.4877.1451
21. Hammond EC. Smoking and death rates—report on forty-four months of follow-up of 187,783 men. JAMA. 1958;166(11):1294. doi:10.1001/jama.1958.02990110030007
22. Organisation for Economic Co-operation and Development. Daily Smokers; 2018. doi:10.1787/1ff488c2-en
23. World Health Organization. WHO Report on the Global Tobacco Epidemic, 2019: Offer Help to Quit Tobacco Use. World Health Organization; 2019.
24. Anna Trząsalska SM. Raport z ogólnopolskiegobadaniaankietowegonatematpostawwobecpaleniatytoniu. 2017.
25. Organisationmondiale de la santé. WHO Report on the Global Tobacco Epidemic, 2017: Monitoring Tobacco Use and Prevention Policies; 2017.
26. Blot WJ, McLaughlin JK, Winn DM, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988;48(11):3282.
27. Negri E, La Vecchia C, Franceschi S, Tavani A. Attributable risk for oral cancer in northern Italy. Cancer Epidemiol Biomarkers Prev. 1993;2(3):189.
28. Diz P, Meleti M, Diniz-Freitas M, et al. Oral and pharyngeal cancer in Europe: incidence, mortality and trends as presented to the global oral cancer forum. Transl Res Oral Oncol. 2017;2:2057178X1770151. doi:10.1177/2057178X17701517
29. de Martel C, Ferlay J, Franceschi S, et al. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol. 2012;13(6):607–615. doi:10.1016/S1470-2045(12)70137-7
30. Castro C, Bosetti C, Malvezzi M, et al. Patterns and trends in esophageal cancer mortality and incidence in Europe (1980–2011) and predictions to 2015. Ann Oncol. 2014;25(1):283–290. doi:10.1093/annonc/mdt486
31. Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends–an update. Cancer Epidemiol Biomarkers Prev. 2016;25(1):16–27. doi:10.1158/1055-9965.EPI-15-0578
32. Mittal S, El-Serag HB. Epidemiology of hepatocellular carcinoma: consider the population. J Clin Gastroenterol. 2013;47(Supplement 1):S2–S6. doi:10.1097/MCG.0b013e3182872f29
33. McGlynn KA, Petrick JL, London WT. Global epidemiology of hepatocellular carcinoma. Clin Liver Dis. 2015;19(2):223–238. doi:10.1016/j.cld.2015.01.001
34. Parkin DM, Boyd L, Walker LC. 16. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010: summary and conclusions. Br J Cancer. 2011;105(S2):S77–S81. doi:10.1038/bjc.2011.489
35. Ilic M, Ilic I. Epidemiology of pancreatic cancer. WJG. 2016;22(44):9694. doi:10.3748/wjg.v22.i44.9694
36. Chatenoud L, Garavello W, Pagan E, et al. Laryngeal cancer mortality trends in European countries: laryngeal cancer mortality in Europe. Int J Cancer. 2016;138(4):833–842. doi:10.1002/ijc.29833
37. Didkowska J, Wojciechowska U, Czaderny K, Olasek P, Ciuba A. Cancer in Poland in 2017. The Maria Skłodowska-Curie Memorial Cancer Center and Institute of Oncology; 2019.
38. Manczuk M, Sulkowska U, Zatonski WA. Closing the Health Gap in European Union. Warsaw, Poland: Cancer Epidemiology and Prevention Division, the Maria Skłodowska-Curie Memorial Cancer Center and Institute of Oncology; 2008.
39. Zatoński WA, Zatoński M. Health in the polish people’s republic. JHI. 2016;1:7–16. doi:10.5114/jhi.2016.61413
40. Cherrie JW. Reducing occupational exposure to chemical carcinogens. Occup Med (Chic Ill). 2009;59(2):96–100. doi:10.1093/occmed/kqn172
41. Driscoll T; World Health Organization; Protection of the Human Environment. Occupational Carcinogens: Assessing the Environmental Burden of Disease at National and Local Levels. World Health Organization, Protection of the Human Environment; 2004.
42. GUS. Zgonywedługprzyczynokreślanychjako “garbage codes.” stat.gov.pl. Available from: https://stat.gov.pl/obszary-tematyczne/ludnosc/statystyka-przyczyn-zgonow/zgony-wedlug-przyczyn-okreslanych-jako-garbage-codes,3,3.html.
43. Department of Health Statistics and Information Systems. WHO Methods and Data Sources for Global Causes of Death 2000–2011; 2013.
44. World Health Organization. WHO Report on Cancer: Setting Priorities, Investing Wisely and Providing Care for All; 2020.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
