Back to Journals » Research and Reports in Tropical Medicine » Volume 8
Predictors of mortality within prison and after release among persons living with HIV in Indonesia
Authors Culbert GJ, Crawford FW, Murni A, Waluyo A, Bazazi AR , Sahar J, Altice FL
Received 30 October 2016
Accepted for publication 12 January 2017
Published 8 March 2017 Volume 2017:8 Pages 25—35
DOI https://doi.org/10.2147/RRTM.S126131
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Thomas Unnasch
Gabriel J Culbert,1,2 Forrest W Crawford,3–5 Astia Murni,6 Agung Waluyo,2 Alexander R Bazazi,7,8 Junaiti Sahar,2 Frederick L Altice7–9
1Department of Health Systems Science, College of Nursing, University of Illinois at Chicago, Chicago, IL, USA; 2Center for HIV/AIDS Nursing Research, Faculty of Nursing, Universitas Indonesia, Depok, Indonesia; 3Department of Biostatistics, Yale School of Public Health, 4Operations, Yale School of Management, 5Department of Ecology and Evolutionary Biology, Yale University, New Haven, CT, USA; 6Directorate General of Corrections, Indonesian Ministry of Law and Human Rights, Jakarta, Indonesia; 7Department of Epidemiology of Microbial Diseases, School of Public Health, 8Department of Medicine, Section of Infectious Diseases, AIDS Program, School of Medicine, Yale University, New Haven, CT, USA; 9Centre of Excellence for Research in AIDS (CERiA), University of Malaya, Kuala Lumpur, Malaysia
Objectives: HIV-related mortality is increasing in Indonesia, where prisons house many people living with HIV and addiction. We examined all-cause mortality in HIV-infected Indonesian prisoners within prison and up to 24 months postrelease.
Materials and methods: Randomly selected HIV-infected male prisoners (n=102) from two prisons in Jakarta, Indonesia, completed surveys in prison and were followed up for 2 years (until study completion) or until they died or were lost to follow-up. Death dates were determined from medical records and interviews with immediate family members. Kaplan–Meier and Cox proportional hazards regression models were analyzed to identify mortality predictors.
Results: During 103 person-years (PYs) of follow-up, 15 deaths occurred, including ten in prison. The crude mortality rate within prison (125.2 deaths per 1,000 PYs) was surpassed by the crude mortality rate (215.7 deaths per 1,000 PYs) in released prisoners. HIV-associated opportunistic infections were the most common probable cause of death. Predictors of within-prison and overall mortality were similar. Shorter survival overall was associated with being incarcerated within a specialized “narcotic” prison for drug offenders (hazard ratio [HR] 9.2, 95% confidence interval [CI] 1.1–76.5; P=0.03), longer incarceration (HR 1.06, 95% CI 1.01–1.1; P=0.01), and advanced HIV infection (CD4+ T-cell count <200/µL, HR 4.8, 95% CI 1.2–18.2; P=0.02). Addiction treatment was associated with longer survival (HR 0.1, 95% CI 0.01–0.9; P=0.03), although treatment with antiretroviral therapy (ART) or methadone was not.
Conclusion: Mortality in HIV-infected prisoners is extremely high in Indonesia, despite limited provision of ART in prisons. Interventions to restore immune function with ART and provide prophylaxis for opportunistic infections during incarceration and after release would likely reduce mortality. Narcotic prisons may be especially high-risk environments for mortality, emphasizing the need for universal access to evidence-based HIV treatments.
Keywords: antiretroviral therapy, HIV/AIDS, Indonesia, mortality, prisoners, substance use
Introduction
Indonesia is currently experiencing one of the world’s largest and most rapidly expanding HIV epidemics, closely intertwined with substance use and incarceration. Despite global reductions, HIV-related mortality in Indonesia, a populous and culturally diverse lower-middle-income country, increased 427% from 2005 to 2013, while the number of people living with HIV (PLH) receiving treatment with antiretroviral therapy (ART) in 2013 remained the lowest in the Asia-Pacific Region.1,2 In 2013, an estimated 29,000 (range: 17,000–46,000) AIDS-related deaths occurred in Indonesia,1 although very few of these (<1%) were officially recorded,3 making it difficult to evaluate the scope of the problem or monitor progress in HIV treatment.4
At the core of Indonesia’s expanding HIV epidemic are people who inject drugs (PWID) and prisoners for whom ART access and adherence are problematic,5 especially after release from prison.6 HIV prevalence in Indonesia has remained consistently high (>50%) among PWID,7,8 who experience significant drug-related comorbidities,9 and HIV-related mortality, even in settings where ART is provided at no cost to patients.10 In Jakarta, over half (56.4%) of PWID are HIV-infected,2 and a third (~29.7%) have been in prison.7 Incarceration of PWID has resulted in elevated HIV prevalence (6.5%) in prisons,11–13 where high-risk drug injection and needle sharing facilitate ongoing transmission.11,14 ART utilization in prisoners (30%–45% of PLH)15 is considerably higher than in the community (8% [5–13%]),1 yet falls substantially below international treatment guidelines.16 Methadone for the treatment of opioid addiction effectively reduces mortality in released prisoners,17 and is available in some Indonesian prisons. Unknown is whether ART and methadone are scaled to reach recommended coverage in prisoners or achieve expected health benefits, including reduced HIV transmission, upon release.18,19
Data from high-income countries reveal three main trends regarding intersecting mortality risks in prisoners. 1) HIV-related mortality within prisons has declined greatly with ART expansion,20 and mortality from liver disease, primarily hepatitis C-related,21 has surpassed HIV as a cause of death in prisoners,22–24 although these trends may not hold in low- and middle-income countries (LMICs) where the provision of ART in prisons is inadequate15 or absent.25 Prison overcrowding may be an especially important factor in mortality26 and related to tuberculosis exposure in PLH.27 2) Risk of death is markedly elevated in released prisoners,28,29 especially during the immediate postrelease period,30,31 due in part to drug relapse,32–34 gaps in HIV care,35–37 and ART nonadherence,38 but is mitigated by receiving opioid agonist therapy (OAT) with methadone or buprenorphine.17,39,40 3) Incarceration is an important social risk factor for shortened life span,41,42 ART nonadherence,43 and HIV risk behaviors,44 yet few interventions have been developed to address HIV and addiction in prison populations.45
Very little information is available about HIV-related mortality in prisoners in LMICs,28 where most (>60%) of the world’s prison population lives,46 and AIDS-related mortality in the community4 and HIV prevalence in prisoners47 are usually higher than in high-income countries. We conducted a prospective cohort study of randomly selected HIV-infected male prisoners in Indonesia to identify predictors of mortality and causes of death during incarceration and up to 2 years after prison release. Set in Indonesia, where HIV-related mortality has markedly increased, and prisons provide an entry point into HIV treatment services for many PWID,48 this study is among the first to examine HIV-related mortality among prisoners in an LMIC.
Materials and methods
Ethics statement
Permission for the study was provided by the Indonesian Ministry of Research and Technology and the Directorate General of Corrections, Ministry of Law and Human Rights. The study was conducted in accordance with international guidelines for research with prisoners.49 The Human Investigation Committee (HIC) at Yale University and Research Ethics Committee at the Faculty of Nursing, University of Indonesia approved the study. Participation was voluntary and subjects selected equitably, without prison staff involvement. All participants provided written informed consent in prison and were reconsented after release. Participants received a snack and toiletry kit at their enrollment visit within prison, and an additional 200,000 IDR (~$18 USD) at the postrelease interview.
Study design
We examined survival, measured from study enrollment until death or a maximum of 24 months (729 days), in a random sample of HIV-infected male prisoners. The study duration was 2 years. During that time, subjects were followed until they died or were lost to follow-up, whichever occurred first. For subjects who were alive and still incarcerated at the end of the study, censoring occurred on the date they were last know alive in prison. After enrollment, participants completed a baseline assessment that consisted of surveys administered by trained researchers in the Indonesian language. During the 2-year study period, researchers attempted to contact each participant who had been released from prison to interview them by telephone or in person. When researchers discovered that a released participant had died, they interviewed family members or caregivers to gather information about the date and cause of death.
Study setting
Indonesia has one of the largest prison populations globally, with over 161,000 prisoners nationwide and many more in pretrial detention.46 Approximately a quarter of Indonesia’s prison population (42,000 prisoners) is located in Jakarta, and prisons there are frequently overcrowded and understaffed.50 Prisoners convicted for drug-related offenses may be housed in one of 23 specialized “narcotic” prisons, first established in 2003 to provide additional services to the growing PWID prison population.51 HIV prevalence in narcotic prisons, officially estimated at 6.5%, varies considerably by region, with HIV prevalence exceeding 10% in prisons located in Jakarta and other large urban areas.12 A national policy expands access to HIV testing and treatment for prisoners,52 resulting in many PLH being diagnosed and initiating ART in prison.15 In Jakarta, 350–400 PLH receive HIV subspecialty care in jails and prisons each month,53 representing ~1% of all HIV cases citywide.54 Most prisoners with HIV had been diagnosed recently in prison.15
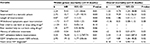
This study was conducted in two large all-male prisons in Jakarta, including one general and one narcotic prison. Table 1 shows characteristics of the two prisons, documenting high HIV prevalence and extreme overcrowding. During the study, 232 PLH were receiving health services through HIV subspecialty clinics located within each prison and comprised the sampling population for this study. Less than half (35%–44.1%) received ART, and very few (<2%) prisoners received methadone at the narcotic prison where it was available.
  | Table 1 Characteristics of male prisoners in Jakarta study sites |
Recruitment and retention
Participant recruitment and study measures have been described previously.15 Briefly, from November 2013 to April 2014, we recruited 102 HIV-infected prisoners already aware of their HIV status. Eligible participants were ≥18 years of age, HIV-infected, conversant in Indonesian, willing to participate in a voice-recorded interview, and provided informed consent. To generate a sample representative of the HIV-infected prisoner population with respect to ART utilization and CD4+ T-cell count, researchers randomly selected 60 subjects from each prison site using a list of all HIV-infected patients at each prison site. Stratification of the patient list by ART utilization (yes or no) and CD4+ T-cell (lymphocyte) count (<200 cells/µL, 200–350 cells/µL, 350–500 cells/µL, >500 cells/µL, and “undefined” as a quarter [25.5%] had not yet undergone CD4+ T-cell testing) yielded 10 blocks, from which we selected a proportional number of HIV-infected prisoners using a random number generator (www.random.org) to be screened for the study. To protect confidentiality, initial contact with prisoners selected for screening was through their physician, who introduced the study. All study procedures were conducted privately, away from other prisoners or prison staff members, in patient examination rooms within the clinic area of each prison. From 120 prisoners initially selected for screening, eleven could not be interviewed because they had been released (n=7), had died (n=2), were being held in solitary confinement (n=1), or had escaped prison (n=1). Two were ineligible, and five refused participation after initial screening, leaving 102 participants enrolled and completing the baseline assessment. To improve study retention, we collected detailed contact information from participants in prison, which we used to reach them by telephone and in person after they were released from prison.
Study measures
Survival time was defined as the interval between the date of enrollment and death. For participants who died in prison, date and cause of death were obtained from participant medical records. Deaths that occurred at outside hospitals while the participant remained in custody were treated as deaths in prison. The date of prison release was determined from prison administrative records. For participants who died after prison release, information about the date and cause of death was provided by immediate family members or caregivers using a standardized symptom questionnaire, with high sensitivity and specificity to identify probable HIV-related deaths.4
Participant social characteristics, drug use behaviors, and HIV treatment history were assessed at enrollment. Drug use was evaluated for the 3 months before incarceration, as well as a single question about whether participants had ever injected drugs in jail or prison.14 Addiction was assessed using the Texas Christian University Drug Screen,55 which has been adapted for prison settings.56 Specifically, participants were asked whether they had ever experienced withdrawal symptoms, attempted to cut back or stop using drugs, participated in addiction treatment, or were taking methadone in prison.
Participants provided the date of HIV diagnosis and were considered as “utilizing ART” if they reported having been prescribed ART during the current prison term. Chart review was used to determine participants’ most recent CD4+ T-cell count. ART adherence was assessed with a 5-point Likert-type question about the amount of ART that a participant had consumed in the last 7 days. We created a composite variable – high adherence – which was the product of participants’ ART utilization and adherence.
Statistical analysis
The R statistical computing environment57 and the survival package58,59 were used to conduct Cox proportional hazards regression analyses of factors associated with survival. The Cox model treats the instantaneous risk of death (hazard) for a given subject as the product of two terms: a time-dependent “baseline” hazard, which is assumed to be common to all subjects, and a function of the subject’s covariates. Covariates in the full model included sociodemographic characteristics (age, education, marital status, living with family before incarceration), institutional factors (length of incarceration and residence in a narcotic prison), addiction factors (addiction severity as previous attempts or needing help to cut back or stop using drugs, and addiction treatment as having participated in addiction treatment, or utilizing methadone in prison), and HIV factors (years since HIV diagnosis, utilizing ART before incarceration, adherence to ART, and AIDS-defining CD4+ T-cell count <200 cells/µL). To model the possibly different mortality risks experienced by participants inside and outside prison, we introduced a time-dependent indicator variable for current incarceration and examined its interaction with ART adherence and CD4+ T-cell count. Stepwise forward/backward variable selection using the Akaike information criterion, which penalizes model complexity,60 was used to find a more parsimonious set of predictors to account for observed variation in survival times.
We analyzed two survival periods – survival within prison and overall survival – up to 24 months postrelease. For both regression analyses, survival time was measured from the date of enrollment until death. Survival times for participants whose death was not observed were censored on the date last known alive. For participants who remained incarcerated at the end of the study, this was the date they were last known alive in prison. For released participants, censoring occurred on the day of prison release if they were lost to follow-up or on the date of the postrelease interview or last contact with research staff if they completed the study.
Results
Participant characteristics and bivariate associations with prison site
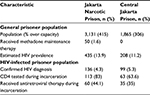
Most participants (64.4%) had injected drugs during the 3 months before incarceration, and over half (55.4%) had injected every day. Characteristics of study participants are shown in Table 2. Participants were 31.3 years of age on average (range 21–51 years), unmarried (68.3%), had not finished high school (54.4%), and were living with family before incarceration (71.3%). Most (78.2%) were diagnosed with HIV in prison, and very few (5.9%) had received ART before incarceration. Participants incarcerated in the narcotic prison (54.4%) had been incarcerated longer (mean 31.3 vs 23.2 months, P<0.001) and were more likely to have ever injected drugs within prison (69.8% vs 39.1%, P=0.002), although for many other measures of drug use and addiction severity, participants from the two prisons were similar. Twice as many participants from the narcotic prison had advanced HIV disease (CD4+ T-cell count <200 cells/µL, 34.5% vs 15.2%; P=0.02), and consequently a larger proportion was receiving ART (60% vs 37%, P=0.02). The difference in the proportion of ART recipients reporting high adherence (>95%) to ART was not significant.
  | Table 2 Participant characteristics by recruitment site Abbreviations: SD, standard deviation; ART, antiretroviral therapy. |
Survival rates and causes of death
Among 101 analyzable participants, 68 (67.3%) were released during the study period, of which 32 (47%) were immediately lost to follow-up and 36 (52.9%) had at least one contact with researchers after prison release (Figure 1). Half of the participants remained in the study (were still alive) for more than 428 days (range 13–729 days) after the baseline interview.
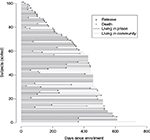  | Figure 1 Days from enrollment to prison release, follow-up, and death in HIV-infected prisoners (n=101). Note: Subjects were sorted by length of time (days) since enrollment. |
During 24 months (103 person-years) of follow-up, 15 deaths occurred, ten of which occurred in prison. The overall crude mortality rate (CMR) was 145.5 deaths per 1,000 person-years, taking into account both deaths that occurred within prison and after release. The CMR within prison (125.2 deaths per 1,000 person-years) was surpassed by the CMR after release (215.7 deaths per 1,000 person-years) by a factor of 1.7. Median time until death after prison release was 157 days, with death occurring as early as 15 days after prison release. The most common probable cause of death was infectious disease attributable to HIV infection (Table 3), which included deaths caused by opportunistic infections and those classifiable as HIV-related deaths based on symptoms. No deaths were attributed to accidental injuries, poisoning, suicide, or homicide. Drug overdose was ruled out as the cause of death for all but one participant.
Multivariate associations with mortality
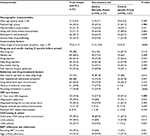
Figure 2 compares unadjusted survival (Kaplan–Meier) curves for participants recruited from the two prisons. The probability of surviving 12 months within prison was lower for participants in the narcotic prison, and though not significant in the unadjusted analysis (χ2=1.5, df=1; P=0.215), being incarcerated in a narcotic prison did emerge as a significant negative predictor of survival after adjusting for other measured covariates. Table 4 shows adjusted hazard ratios (HRs) for all-cause mortality both within prison and overall, which included an additional five deaths occurring in released participants. Selected variables for the two models were similar. In regression analyses for mortality within prison and overall, shorter survival was associated with being married (HR: 9.4, 95% confidence interval [CI]: 1.5–58.6 [P=0.01]; HR 4.7, 1.2–18 [P=0.02]), incarceration within a narcotic prison (HR: 15.7, 95% CI: 1.2–193.9 [P=0.03]; HR: 9.2, 95% CI: 1.1–76.5 [P=0.03]), longer duration of incarceration (HR: 1.07, 95% CI: 1–1.1 [P=0.03]; HR: 1.06, 95% CI: 1–1.1 [P=0.01]), and more advanced HIV disease (AIDS-defining), measured as CD4+ T-cell count <200 cells/µL (HR: 19.1, 95% CI: 1.7–206.6 [P=0.01]; HR: 4.8, 95% CI: 1.2–18.2 [P=0.02]), whereas a history of addiction treatment was significantly associated with longer survival (HR: 0.04, 95% CI: 0–0.9 [P=0.04]; HR: 0.13, 95% CI: 0.01–0.9 [P=0.03]), respectively. ART utilization before incarceration was associated with increased mortality within prison (HR: 76.81, 95% CI: 2.11–2787.74; P=0.01) but not overall. Although unadjusted MRs within prison (125.2 deaths per 1,000 person-years) and after release (215.7 deaths per 1,000 person-years) were different, when other covariates (demographic, institutional, and HIV- and addiction-related) were considered in time-dependent proportional hazards models (Table 4), the effect of prison release on survival was not significantly different from zero.
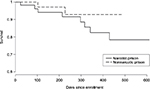  | Figure 2 Unadjusted Kaplan–Meier curves for participants recruited from one narcotic prison and one nonnarcotic prison in Indonesia. |
Discussion
Very few studies internationally have examined HIV-related mortality in prison populations in LMICs, despite high prevalence of HIV and other mortality risks in these settings.27 One systematic review with a meta-analysis of postrelease prison mortality in high-income countries documented a CMR of 8.5 deaths (range 7.2–10.3) per 1,000 person-years.28 Here, when limiting our analysis to prisoners with HIV, the CMR postrelease was over 25-fold higher or 215.7 deaths per 1,000 person-years. Even more concerning, however, is the CMR of 125.2 deaths per 1,000 person-years within prison, which contrasts with high-income countries like the US, where provision of simple well-tolerated ART regimens in the structured prison environment typically results in high rates of viral suppression61 and much lower AIDS mortality within prison (3.8 deaths per 1,000 person-years).20 Findings from our work in Indonesia and Malaysia62 suggest that both individual and structural factors contribute to extremely high mortality in HIV-infected prisoners, and that most of these deaths could be prevented through adherence to international guidelines recommending treatment for all PLH, including prisoners, regardless of CD4+ T-cell count.16
Advanced HIV infection, as measured by low CD4+ T-cell count, was among the most important individual risk factors for mortality in this sample of PLH, most of whom (64.4%) were PWID, with higher risk for HIV progression.63 Especially concerning was that longer survival was not associated with treatment with ART, which is fully subsidized by the Indonesian government and available to prisoners, but prioritized for prisoners with advanced HIV infection (World Health Organization clinical stages 3 and 4). Consequently, the mortality benefits of ART were not demonstrated in this study, and ART and CD4+ T-cell count were highly correlated. In contrast to high-income settings, where drug overdose is the most common preventable cause of death for prisoners,33,64 inadequately treated HIV infection, often resulting in opportunistic infection, appears to be the main risk factor for death in this sample of HIV-infected and mostly drug-dependent prisoners.
When dosed correctly, maintenance with OAT like methadone and buprenorphine can improve the likelihood of being prescribed ART65 and optimize adherence in people who use opioids.66 OAT also significantly reduces mortality after prison release,40 which may partly explain the apparently protective effect of addiction treatment in this study. Noteworthy from this study was that many HIV-infected prisoners with opioid-use disorders were incarcerated in the nonnarcotic prison, where interventions for addiction (eg, methadone) are not yet available. While interventions targeting opioid addiction have the potential to reduce mortality in prisoners in high-income settings,17 such interventions are unlikely to prevent deaths resulting from inadequate provision of ART in HIV-infected prisoners, which are clearly preventable through adherence to international treatment guidelines. Demonstration projects in Indonesia67 and Malaysia62 have shown reductions in HIV-related mortality in prisoners through multicomponent interventions addressing patient education and staff clinical training to expand ART closer to recommended levels.
Findings here suggest that structural factors, specifically those related to the prison environment contribute independently to mortality within prison and after release and help to contextualize the observed association between incarceration and shorter survival.41,42 Being in a prison for drug offenders and longer duration of incarceration were both associated with shorter survival, suggesting either that narcotic prisons may be especially high-risk environments for mortality or that characteristics of individuals housed in narcotic prisons place them at increased risk of death. These associations remained significant in the overall model, suggesting that prison-related factors may influence mortality even after prison release.
Although the pathways linking incarceration and mortality risk are not clear, our previous research at these sites suggests several possibilities. 1) Although many PLH are first diagnosed with HIV in prison, health care resources in prisons are often inadequate to ensure prompt ART initiation based on international guidelines.68,69 At the narcotic prison, for example, three physicians care for ~3,100 inmates, including 136 with HIV. Limited ART regimens and laboratory monitoring are also problematic, especially for patients starting ART with very low CD4+ T-cell counts, viral hepatitis, or tuberculosis, which are more common in prisoners.70 2) Prison overcrowding, poor ventilation, and inadequate sanitation facilitate transmission of opportunistic infections, including pulmonary tuberculosis, toxoplasmosis, and diarrheal diseases.27 3) Stigmatization of prisoners receiving ART71 and prisoners’ misperceptions about the risks and benefits of ART15 may contribute to some prisoners refusing ART. Even after adjusting for some of these variables (Table 5), however, there was still a 17-fold increase in the risk of death for PLH incarcerated in a narcotic prison, raising questions about unmeasured structural and individual factors that may influence survival in this population.
Of interest is the finding that being married was associated with increased mortality risk, and is not easily explained by the existing data. While it is purely speculation, one reason might be that these prisoners with HIV were in relationships where HIV was not disclosed to their spouse, and the prisoner did not want to engage in any activity (eg, going to HIV doctors, taking ART) that might have disclosed their status. HIV-related stigma in Indonesia remains extraordinarily high,72 as is stigmatization of drug use,73 and further exploration is needed to understand contextual issues better with regard to HIV disclosure and how such issues may be addressed under these circumstances.
Findings here should be considered in the context of certain limitations. 1) Although our final sample size was small (n=101), this is to our knowledge the largest study of HIV-related mortality among prisoners in an LMIC to date. 2) Findings were limited to two prisons with high HIV prevalence in Jakarta and did not include jails or mandatory drug rehabilitation centers, where individual and structural factors may differ. 3) Incomplete data following prison release may have biased mortality assessment if missing data were nonrandom. Concerning, for example, would be nonrandom missing data from participants with substance use disorders that were a factor in their survival. This concern is mitigated somewhat by high rates (73.5%) of self-reported substance use in participants who completed the postrelease interview. Loss to follow-up may have occurred because some participants relocated, were unable to provide valid contact information, or no longer wanted to participate. 4) Assumptions underlying the Cox proportional hazards model may not hold in settings where prison release depends on health-related variables. A compassionate release program, for example, would likely violate the independent censoring assumptions. Prisoners’ health, however, was not a factor in their release. Also assumed was that the baseline hazard of death was proportional for all subjects across time, which we are reasonably confident was the case, since prisoners received similar treatment within each prison. 5) Although family members provided information about cause of death in released participants, symptom-based “verbal autopsy” has high sensitivity and specificity for detecting HIV-related death in populations lacking civil registration or medical certification.4
Conclusion
Mortality in HIV-infected prisoners is extremely high, despite ART availability in prisons. Unlike high-income countries, where drug overdose is the most common preventable cause of death in released prisoners, most deaths among HIV-infected prisoners in Indonesia appear to be a direct consequence of HIV infection and mainly preventable through earlier ART initiation in all prisoners with HIV and prophylaxis for opportunistic infection. Narcotic prisons, where many PWID are concentrated, may be especially high-risk environments for mortality, potentially due to overcrowding and related environmental stressors, although further research is needed to elucidate the pathways through which structural factors influence HIV-related mortality in these settings.
Author contributions
GJC and FWC designed the study, analyzed and interpreted data, and wrote the paper. FWC conducted all statistical analyses. AM, AW, and JS contributed substantially to the acquisition, analysis, and interpretation of data and writing subsequent drafts. ARB and FLA contributed extensively to the interpretation of results and revising the final draft for intellectual content. All authors discussed the results and implications, and approved the final version to be published.
Acknowledgments
The authors thank study participants for sharing their time. They also thank Azalia P Muchransyah, Mariska Iriyanti, Ni Made Swasti Wulanyani, Budhi Mulyadi, and Herlia Yuliantini for research assistance. They gratefully acknowledge operational assistance from the Directorate General of Corrections, Republic of Indonesia, especially Akbar Hadi Prabowo and Hetty Widiastuti. They thank Nurlan Silitonga, Cindy Hidayati, Alia Hartanti, David Shenman, and Suzanne Blogg (HIV Cooperation Programme for Indonesia), Judith Levy (University of Illinois at Chicago), and Elly Nurachmah (Universitas Indonesia). GJC was supported through a Fulbright Senior Scholar Award in Global Health from the J William Fulbright Commission, US State Department and a Global Health Equity Fellowship (R25 TW009338) funded by NIAID and Fogarty International Center. FWC was supported by NIH/NCATS grant KL2 TR000140, NIMH grant P30MH062294, and NICHD/BD2K DP2HD091799. This work was also supported by NIH awards for research (NIDA R01 DA025943 and R01 DA041271), training (D43 TW001419 to AW, NIDA F30 DA039716 and T32 GM07205 to ARB), and career development (NIDA K24 DA017072 to FLA).
Disclosure
The authors report no conflicts of interest in this work.
References
Joint United Nations Programme on HIV/AIDS. The Gap Report. Geneva: UN; 2014. | ||
Joint United Nations Programme on HIV/AIDS. HIV in Asia and the Pacific. Bangkok: UN; 2013. | ||
Ministry of Health, Indonesia. Cases of HIV/AIDS in Indonesia reported through September 2014. Jakarta: Directorate General CDC and Environmental Health; 2014. | ||
World Health Organization. Guidelines for HIV Mortality Measurement. Geneva: WHO; 2014. | ||
Milloy MJ, Montaner J, Wood E. Barriers to HIV treatment among people who use injection drugs: implications for ‘treatment as prevention’. Curr Opin HIV AIDS. 2012;7(4):332–338. | ||
Iroh PA, Mayo H, Nijhawan AE. The HIV care cascade before, during, and after incarceration: a systematic review and data synthesis. Am J Public Health. 2015;105(7):e5–e16. | ||
Morineau G, Bollen LJ, Syafitri RI, Nurjannah N, Mustikawati DE, Magnani R. HIV prevalence and risk behaviours among injecting drug users in six Indonesian cities: implications for future HIV prevention programs. Harm Reduct J. 2012;9:37. | ||
Januraga PP, Wulandari LP, Muliawan P, et al. Sharply rising prevalence of HIV infection in Bali: a critical assessment of the surveillance data. Int J STD AIDS. 2013;24(8):633–637. | ||
Larney S, Randall D, Gibson A, Degenhardt L. The contributions of viral hepatitis and alcohol to liver-related deaths in opioid-dependent people. Drug Alcohol Depend. 2013;131(3):252–257. | ||
Lappalainen L, Hayashi K, Dong H, Milloy MJ, Kerr T, Wood E. Ongoing impact of HIV infection on mortality among people who inject drugs despite free antiretroviral therapy. Addiction. 2015;110(1):111–119. | ||
Blogg S, Utomo B, Silitonga N, Hidayati DA, Sattler G. Indonesian national inmate bio-behavioral survey for HIV and syphilis prevalence and risk behaviors in prisons and detention centers, 2010. SAGE Open. 2014;4:1–7. | ||
Directorate General of Corrections. HIV and HCV Prevalence and Risk Behavior Study in Indonesian Narcotics Prisons. Jakarta: Directorate of Corrections; 2012. | ||
Directorate General of Corrections. HIV and Syphilis Prevalence and Risk Behavior Study among Prisoners and Detention Centres in Indonesia. Jakarta: Directorate of Corrections; 2010. | ||
Culbert GJ, Waluyo A, Iriyanti M, Muchransyah AP, Kamarulzaman A, Altice FL. Within-prison drug injection among HIV-infected male prisoners in Indonesia: a highly constrained choice. Drug Alcohol Depend. 2015;149:71–79. | ||
Culbert GJ, Bazazi AR, Waluyo A, et al. The influence of medication attitudes on utilization of antiretroviral therapy (ART) in Indonesian prisons. AIDS Behav. 2016;20(5):1026–1038. | ||
World Health Organization. Guideline on When to Start Antiretroviral Therapy and on Pre-exposure Prophylaxis for HIV. Geneva: WHO; 2015. | ||
Degenhardt L, Larney S, Kimber J, et al. The impact of opioid substitution therapy on mortality post-release from prison: retrospective data linkage study. Addiction. 2014;109(8):1306–1317. | ||
Altice FL, Azbel L, Stone J, et al. The perfect storm: incarceration and the high-risk environment perpetuating transmission of HIV, hepatitis C virus, and tuberculosis in Eastern Europe and Central Asia. Lancet. 2016;388(10050):1228–1248. | ||
Dolan K, Wirtz AL, Moazen B, et al. Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet. 2016;388(10049):1089–1102. | ||
Maruschak LM. HIV in Prisons, 2001–2010. Washington: US Bureau of Justice Statistics; 2015. | ||
Larney S, Kopinski H, Beckwith CG, et al. Incidence and prevalence of hepatitis C in prisons and other closed settings: results of a systematic review and meta-analysis. Hepatology. 2013;58(4):1215–1224. | ||
Rosen DL, Wohl DA, Schoenbach VJ. All-cause and cause-specific mortality among black and white North Carolina state prisoners, 1995-2005. Ann Epidemiol. 2011;21(10):719–726. | ||
Spaulding AC, Sharma A, Messina LC, Zlotorzynska M, Miller L, Binswanger IA. A comparison of liver disease mortality with HIV and overdose mortality among Georgia prisoners and releasees: a 2-decade cohort study of prisoners incarcerated in 1991. Am J Public Health. 2015;105(5):e51–57. | ||
Spaulding AC, Seals RM, McCallum VA, Perez SD, Brzozowski AK, Steenland NK. Prisoner survival inside and outside of the institution: implications for health-care planning. Am J Epidemiol. 2011;173(5):479–487. | ||
Fu JJ, Bazazi AR, Altice FL, Mohamed MN, Kamarulzaman A. Absence of antiretroviral therapy and other risk factors for morbidity and mortality in Malaysian compulsory drug detention and rehabilitation centers. PLoS One. 2012;7(9):e44249. | ||
Rabe K. Prison structure, inmate mortality and suicide risk in Europe. Int J Law Psychiatry. 2012;35(3):222–230. | ||
Kamarulzaman A, Reid SE, Schwitters A, et al. Prevention of transmission of HIV, hepatitis B virus, hepatitis C virus, and tuberculosis in prisoners. Lancet. 2016;388(10049):1115–1126. | ||
Zlodre J, Fazel S. All-cause and external mortality in released prisoners: systematic review and meta-analysis. Am J Public Health. 2012;102(12):e67–e75. | ||
Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159(9):592–600. | ||
Huang YF, Kuo HS, Lew-Ting CY, et al. Mortality among a cohort of drug users after their release from prison: an evaluation of the effectiveness of a harm reduction program in Taiwan. Addiction. 2011;106(8):1437–1445. | ||
Forsyth SJ, Alati R, Ober C, Williams GM, Kinner SA. Striking subgroup differences in substance-related mortality after release from prison. Addiction. 2014;109(10):1676–1683. | ||
Binswanger IA, Nowels C, Corsi KF, et al. Return to drug use and overdose after release from prison: a qualitative study of risk and protective factors. Addict Sci Clin Pract. 2012;7:3. | ||
Møller LF, Matic S, van den Bergh BJ, Moloney K, Hayton P, Gatherer A. Acute drug-related mortality of people recently released from prisons. Public Health. 2010;124(11):637–639. | ||
Cepeda JA, Niccolai LM, Lyubimova A, Kershaw T, Levina O, Heimer R. High-risk behaviors after release from incarceration among people who inject drugs in St. Petersburg, Russia. Drug Alcohol Depend. 2015;147:196–202. | ||
Giordano TP, Gifford AL, White AC Jr, et al. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis. 2007;44(11):1493–1499. | ||
Springer SA, Pesanti E, Hodges J, Macura T, Doros G, Altice FL. Effectiveness of antiretroviral therapy among HIV-infected prisoners: reincarceration and the lack of sustained benefit after release to the community. Clin Infect Dis. 2004;38(12):1754–1760. | ||
Khawcharoenporn T, Zawitz C, Young JD, Kessler HA. Continuity of care in a cohort of HIV-infected former jail detainees. J Correct Health Care. 2013;19(1):36–42. | ||
Baillargeon J, Giordano TP, Rich JD, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301(8):848–857. | ||
Gisev N, Shanahan M, Weatherburn DJ, et al. A cost-effectiveness analysis of opioid substitution therapy upon prison release in reducing mortality among people with a history of opioid dependence. Addiction. 2015;110(12):1975–1984. | ||
Hedrich D, Alves P, Farrell M, Stöver H, Møller L, Mayet S. The effectiveness of opioid maintenance treatment in prison settings: a systematic review. Addiction. 2012;107(3):501–517. | ||
Lim S, Harris TG, Nash D, Lennon MC, Thorpe LE. All-cause, drug-related, and HIV-related mortality risk by trajectories of jail incarceration and homelessness among adults in New York City. Am J Epidemiol. 2015;181(4):261–270. | ||
Patterson EJ. The dose-response of time served in prison on mortality: New York State, 1989–2003. Am J Public Health. 2013;103(3):523–528. | ||
Milloy MJ, Kerr T, Buxton J, et al. Dose-response effect of incarceration events on nonadherence to HIV antiretroviral therapy among injection drug users. J Infect Dis. 2011;203(9):1215–1221. | ||
Milloy MJ, Kerr T, Salters K, et al. Incarceration is associated with used syringe lending among active injection drug users with detectable plasma HIV-1 RNA: a longitudinal analysis. BMC Infect Dis. 2013;13:565. | ||
Kouyoumdjian FG, McIsaac KE, Liauw J, et al. A systematic review of randomized controlled trials of interventions to improve the health of persons during imprisonment and in the year after release. Am J Public Health. 2015;105(4):e13–e33. | ||
Walmsley R. World Prison Population List. 11th ed. London: Institute for Criminal Policy Research; 2016. | ||
Dolan K, Moazen B, Noori A, Rahimzadeh S, Farzadfar F, Hariga F. People who inject drugs in prison: HIV prevalence, transmission and prevention. Int J Drug Policy. 2015;26 Suppl 1:S12–S15. | ||
Nelwan EJ, Van Crevel R, Alisjahbana B, et al. Human immunodeficiency virus, hepatitis B and hepatitis C in an Indonesian prison: prevalence, risk factors and implications of HIV screening. Trop Med Int Health. 2010;15(12):1491–1498. | ||
Lazzarini Z, Altice FL. A review of the legal and ethical issues for the conduct of HIV-related research in prisons. AIDS Public Policy J. 2000;15(3–4):105–135. | ||
Parlina I, Somba ND. Prisons still overcrowded, lack skilled staff. Jakarta Post. 2016 Mar 10 Available from: http://www.thejakartapost.com/news/2016/03/10/prisons-still-overcrowded-lack-skilled-staff.html. Accessed January 16, 2017. | ||
Indonesia National AIDS Commission. Republic of Indonesia Country Report on the Follow-up to the Declaration of Commitment on HIV/AIDS (United Nations General Assembly Special Session): Reporting Period 2010–2011. Jakarta: National AIDS Commission; 2012. | ||
Directorate of Corrections. National Action Plan for Control of HIV-AIDS and Drug Abuse in Correctional Units in Indonesia 2010–2014. Jakarta: Directorate of Corrections; 2010. | ||
Directorate of Corrections. Sistem database pemasyarakatan [correctional system database]. 2015. Available from: http://smslap.ditjenpas.go.id. Accessed 8 January 2015. Indonesian. | ||
Ministry of Health, Indonesia. Situasi dan Analysis HIV/AIDS. Jakarta: Ministry of Health; 2014. | ||
Texas Christian University. TCU Drug Screen II. Fort Worth (TX): TCU; 2007. | ||
Simpson DD, Joe GW, Knight K, Rowan-Szal GA, Gray JS. Texas Christian University (TCU) short forms for assessing client needs and functioning in addiction treatment. J Offender Rehabil. 2012;51(1–2):34–56. | ||
R Core Team. R: A Language Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing; 2015. | ||
Therneau TM. A package for survival analysis in S. version 2.38. 2015. Available from: https://cran.r-project.org/web/packages/survival/index.html. Accessed January 16, 2017. | ||
Therneau TM, Grambsch PM. Modelling Survival Data: Extending the Cox Model. New York: Springer; 2000. | ||
Bozdogan H. Model selection and Akaike’s information criterion (AIC): the general theory and its analytical extensions. Psychometrika. 1987;52(3):345–370. | ||
Meyer JP, Cepeda J, Wu J, Trestman RL, Altice FL, Springer SA. Optimization of human immunodeficiency virus treatment during incarceration: viral suppression at the prison gate. JAMA Intern Med. 2014;174(5):721–729. | ||
Culbert GJ, Pillai V, Bick J, et al. Confronting the HIV, tuberculosis, addiction, and incarceration syndemic in Southeast Asia: lessons learned from Malaysia. J Neuroimmune Pharmacol. 2016;11(3):446–455. | ||
Meijerink H, Wisaksana R, Iskandar S, et al. Injecting drug use is associated with a more rapid CD4 cell decline among treatment naïve HIV-positive patients in Indonesia. J Int AIDS Soc. 2014;17:18844. | ||
Merrall EL, Kariminia A, Binswanger IA, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105(9):1545–1554. | ||
Altice FL, Bruce RD, Lucas GM, et al. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: results from a multisite study. J Acquir Immune Defic Syndr. 2011;56 Suppl 1:S22–S32. | ||
Lappalainen L, Nolan S, Dobrer S, et al. Dose-response relationship between methadone dose and adherence to antiretroviral therapy among HIV-positive people who use illicit opioids. Addiction. 2015;110(8):1330–1339. | ||
Nelwan EJ, Indrati AK, Isa A, et al. Effect of HIV prevention and treatment program on HIV and HCV transmission and HIV mortality at an Indonesian narcotic prison. Southeast Asian J Trop Med Public Health. 2015;46(5):880–891. | ||
Bick J, Culbert G, Al-Darraji HA, et al. Healthcare resources are inadequate to address the burden of illness among HIV-infected male prisoners in Malaysia. Int J Prison Health. 2016;12(4):253–269. | ||
Gallant JE, Mehta SH, Sugarman J. Universal antiretroviral therapy for HIV infection: should US treatment guidelines be applied to resource-limited settings? Clin Infect Dis. 2013;57(6):884–887. | ||
Rich JD, Beckwith CG, Macmadu A, et al. Clinical care of incarcerated people with HIV, viral hepatitis, or tuberculosis. Lancet. 2016;388(10049):1103–1114. | ||
Culbert GJ, Earnshaw VA, Wulanyani NM, Wegman MP, Waluyo A, Altice FL. Correlates and experiences of HIV stigma in prisoners living with HIV in Indonesia: a mixed-method analysis. J Assoc Nurses AIDS Care. 2015;26(6):743–757. | ||
Brotosudirdjo S, Nurahmawati I. Empowerment the [sic] health providers by involving families in the prevention program of HIV-AIDS among housewives in Indonesia. Int J Evid Based Healthc. 2016;14:S5. | ||
Spooner C, Saktiawati AM, Lazuardi E, Worth H, Subronto YW, Padmawati RS. Impacts of stigma on HIV risk for women who inject drugs in Java: a qualitative study. Int J Drug Policy. 2015;26(12):1244–1250. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.