Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Predictive Value of Skeletal Muscle Function Test Combined with Climbing Test for Postoperative Cardiopulmonary Complications in Patients with COPD and Concurrent Lung Cancer
Authors He Z, Li H, Cao B, Zan Z, Feng H, Wei Q, Liu K
Received 29 September 2023
Accepted for publication 16 November 2023
Published 24 November 2023 Volume 2023:18 Pages 2699—2706
DOI https://doi.org/10.2147/COPD.S438336
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Zemin He,1 Hong Li,1 Boxiong Cao,1 Ziliang Zan,1 Hao Feng,1 Qiang Wei,1 Keting Liu2
1Department of Thoracic Surgery, The First People’s Hospital of Shuangliu District (West China Airport Hospital of Sichuan University), Chendu, Sichuan Province, People’s Republic of China; 2Department of Neurology, Chengdu Seventh People’s Hospital, Chendu, Sichuan Province, People’s Republic of China
Correspondence: Qiang Wei, Department of Thoracic Surgery, The First People’s Hospital of Shuangliu District (West China Airport Hospital of Sichuan University), 120 Chengbei Upper Street, Dongsheng Town, Shuangliu District, Chendu, Sichuan Province, People’s Republic of China, Tel +86 13778533702, Email [email protected]
Purpose: To explore the predictive value of skeletal muscle function measurement combined with stair climbing test for postoperative cardiopulmonary complications in patients with chronic obstructive pulmonary disease (COPD) and non-small cell lung cancer (NSCLC).
Patients and Methods: A prospective study was conducted from June 2022 to July 2023 at West China Hospital of Sichuan University, including 335 COPD patients with lung cancer who underwent surgery. The patients were divided into two groups based on the occurrence of postoperative cardiopulmonary complications: the complication group and the non-complication group. The demographic data, including gender, age, smoking history, quadriceps strength, body mass index (BMI), respiratory muscle strength, 6-minute walk test (6MWD), stair climbing test, and preoperative pulmonary function tests, were compared between the two groups. Logistic regression analysis was performed to evaluate the predictive power of each parameter for postoperative cardiopulmonary complications.
Results: Among the enrolled patients, 103 (30.7%) developed postoperative cardiopulmonary complications. Significant differences were observed between the two groups in terms of quadriceps strength, respiratory muscle strength, 6MWD, smoking history, stair climbing test, DLCO%, FEV1%, heart rate, oxygen saturation, surgical duration, surgical approach, resection range, and blood loss (P< 0.05). Logistic regression analysis revealed that respiratory muscle strength, quadriceps strength, stair climbing test, FEV1%, DLCO%, ΔHR, ΔSPO2, surgical approach were identified as risk factors for postoperative cardiopulmonary complications in patients with COPD and lung cancer.
Conclusion: Skeletal muscle function measurement, stair climbing test, FEV1, surgical approach, and DLCO% can serve as assessment tools for surgical risk in patients with COPD and lung cancer. They can predict the occurrence of postoperative cardiopulmonary complications to a certain extent, providing valuable predictive value for these complications in patients with COPD and NSCLC.
Keywords: respiratory muscle function, Cardiopulmonary complications, lung cancer surgery, Climbing test
Introduction
Lung cancer is a malignancy with high morbidity and mortality, and surgery is currently considered as the preferred treatment. Chronic obstructive pulmonary disease (COPD) is an independent risk factor for lung cancer, with 40% to 60% of lung cancer patients presenting with COPD disease.1
These patients have poor lung function and a higher risk of postoperative cardiorespiratory complications, which also leads to increased postoperative complications and mortality. Therefore, it is very important to predict the possible postoperative complications and to perform preoperative intervention. For lung cancer patients with COPD, preoperative assessment was similar to patients undergoing conventional lung cancer surgery. However, conventional static lung function tests are unable to assess exercise endurance and cardiac function reserve. Although the cardiopulmonary exercise test (CPET) is considered the gold standard,2 the clinical needs cannot be met due to objective conditions. Some studies have found that skeletal muscle function can partly reflect the degree of severity of COPD. The stair climbing test is often used as a supplementary test for patients with low lung function. It is unclear whether the combination of these two methods can predict postoperative cardiopulmonary complications in patients with non-small cell lung cancer with COPD. In this study, patients with NSCLC with COPD were selected to compare the skeletal muscle function and floor climbing test results between the two groups of patients with postoperative complications and without complications.
The purpose of this study was to investigate the value of the skeletal muscle function combined with stair climbing test as a prediction of postoperative cardiopulmonary complications in patients with non-small cell lung cancer with COPD. The specific study results are presented as follows.
Materials and Methods
Ethical Considerations
This study has been approved by the ethics committee of West China (Airport) Hospital Sichuan University (batch number: 2022-ks-06). Written informed consent was obtained from all patients.
Patients and Study Design
The clinical data of COPD patients with non-small cell lung cancer (NSCLC) treated in the Department of Thoracic Surgery of West China Airport Hospital, Sichuan University, were prospectively included. Inclusion criteria included: (1) age of 18 years; (2) diagnosis of COPD according to the GOLD diagnostic criteria;3 (3) complete medical records; (4) all patients underwent lung resection, and the pathological diagnosis was non-small cell lung cancer; (5) Patients with surgical indications after preoperative evaluation of clinical stage IA–IIIA. Exclusion criteria include: (1) other serious respiratory diseases, such as acute asthma, bronchiectasis, active tuberculosis, and pleural effusion; (2) contraindications; (3) history of chest surgery; (4) cognitive impairment, severe osteoarthropathy, and recent myocardial infarction, who are unable to complete skeletal muscle function tests and stair climbing tests. A total of 335 patients with COPD associated with lung cancer were included in an age range of 31 to 87 years with a mean of (57.9 ± 8.93) years. There were 238 male and 97 female cases.
This study records the age, gender, disease duration, height, weight, BMI, smoking history, and drinking history of the 335 COPD patients with NSCLC included in the study. We identified respondents with a history of cigarette smoking by an affirmative response to the tobacco use question, “Have you smoked at least 100 cigarettes in your entire life?” Patients who had smoked≥100 cigarettes were considered those with a smoking history.
To assess the patient with quadriceps muscle strength, 6-minute walking distance (6 MWD), stair climbing test and preoperative pulmonary function test (FEV 1% and DLCO%). Spirometry was performed using a MasterScreen PFT (Weian Medical Device Company) spirometer. All participants underwent spirometry based on the American Thoracic Society and European Respiratory Society (ATS/ERS) guidelines.4 None of the patients used bronchodilators before spirometry. The patients performed up to three forced expiratory maneuvers to obtain acceptable results. Well-trained respiratory technicians continuously monitored the spirometry procedure and reviewed the flow–volume curves to ensure adherence to the standards. The parameters taken during the test included FEV 1% and DLCO%.5
All determinations were performed by the same operator to reduce the error.
Quadriceps muscle strength: Quadriceps muscle strength was measured in all patients using a WDF-50 digital explicit extension dynamometer (Wenzhou Weidu Electronics Co., Ltd., WDF-50 digital display push-pull meter, Wenzhou, China). During the measurement, the subject sat in a high chair, the back close to the chair, the knee flexion 90°, the measuring plate was placed on the front of the calf, requiring the subject to push the plate to generate the maximum knee extension force and keep it for 5 seconds. Quadriceps muscle strength was measured three times, and the maximum value was taken as the final quadriceps muscle strength.
Respiratory muscle strength: Respiratory muscle strength was measured using a portable lung function detector (Wuhan Kangbeinuo Medical Equipment Co., Ltd., Lung Function Testing Instrument, Wuhan, China). The subject aspirated through the mouth to filled the air into the lungs to determine the strength of the respiratory muscles.
6 MWD test: According to the expert consensus of 6 min walking distance,6 the subjects walked back and forth for 6 minutes to measure the walking distance. If the discomfort symptoms appear, immediately stop the test and treat it accordingly.
Stair-Climbing Test: The patient climbed five floors at a usual speed (at a cumulative height of 16.5 meters), guided by the same doctor. Record whether the patient completed the stair climbing test, and determine the heart rate and fingertip oxygen saturation of the patient before and after the test, and calculate the change of heart rate (Δ HR) and fingertip oxygen saturation (Δ SpO 2).
Procedure-related information: recorded the method of lung resection (thoracotomy/minimally invasive surgery), resection range (lobe/sublobe), operation time (3 hours />3 hours), and intraoperative blood loss (100mL/> 100mL). Postoperative cardiopulmonary complications were recorded according to the STS / ESTS criteria (persistent lung air leakage, pulmonary infection, arrhythmia, acute myocardial infarction, pulmonary embolism, heart failure, breast augmentation, bronchopleural fistula, secondary endotracheal intubation, death, etc.).
Statistical Analyses
Statistical analysis was performed by SPSS23.0. Measurement data were normal distribution by Shapiro–Wilk test, expressed by mean ± standard deviation ( ); independent sample t-test; count data were represented by cases (%), compared by χ2 test; risk factors of COPD associated with lung cancer were analyzed by dichotomy logistic regression method. Differences were considered statistically significant at P <0.05.
); independent sample t-test; count data were represented by cases (%), compared by χ2 test; risk factors of COPD associated with lung cancer were analyzed by dichotomy logistic regression method. Differences were considered statistically significant at P <0.05.
Results
Comparison of General Characteristics Between Groups
A total of 335 subjects were included in the study, with 103 cases (30.7%) experiencing postoperative cardiopulmonary complications. Among them, Lobectomy was performed in 150 cases (44.8%), sublobar resection including segmentectomy and wedge resection in 185 cases (55.2%); Thoracotomy included 76 cases (22.7%) converted to thoracotomy and 259 cases (77.3%) underwent thoracoscopic surgery. A total of 132 cases of postoperative cardiopulmonary-related complications were recorded, occurring in 103 patients, accounting for 30.7% of enrolled cases, including 54 (16.1%) cases of persistent pulmonary air leakage, 48 (14.3%) lung infections, 33 (9.9%) cases of arrhythmia, 27 (8.1%) cases of atelectasis, 0 cases of acute myocardial infarction, and 3 (0.9%) cases of pulmonary embolism, respiratory failure led to re-tracheal intubation in 15 (4.5%) cases, 27 (8.1%) cases of atelectasis. One case died in the perioperative period, which was a large postoperative cerebral infarction, and died after thrombectomy.
The results of univariate analysis showed that there were statistical differences between the two groups including quadriceps muscle strength, respiratory muscle strength, 6 MWD, smoking history, stair climbing test, DLCO%, FEV 1%, heart rate, oxygen saturation, operation time, surgical method, resection range, bleeding loss, and the proportion of postoperative cardiopulmonary complications (P <0.05). Detailed results are shown in Table 1.
 |
Table 1 Baseline Characteristics of the Study Population |
Risk Factors for Complications After COPD Combined with Lung Cancer Surgery
For the indicators in Table 1 that met P <0.05 in univariate analysis, we further performed a multivariate logistic regression analysis to assess the relationship with the occurrence of complications. The value of the variable is as follows: the unfinished stair climbing test is 1; completed is 2; FEV 1% <60% is 1, ≥60% is 2; DLCO% <60% 1, ≥60% is 2; Δ HR ≥30 is 1, <30 is 2; ΔSPO2≥4% 1, less than 4% is 2; operation time ≥210min is 1, <210min is 2; thoracotomy is 1, thoracoscopy is 2; bleeding ≥100mL is 1, <100mL is 2; lobectomy is 1, sublobectomy is 2; with smoking history is 1, without smoking history is 2. Respiratory muscle strength, quadriceps muscle strength, and 6 MWD were included in the regression analysis with actual values. The results showed that respiratory muscle strength, quadriceps strength, stair climbing test, FEV 1%, DLCO%, Δ HR, Δ SPO 2, surgical methods were the risk factors for postoperative cardiopulmonary complications in patients with COPD and lung cancer. See Table 2.
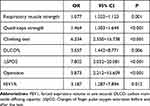 |
Table 2 Risk Factors for Postoperative Complications |
Predictors of Postoperative Cardiopulmonary Complications
Figure 1 shows the ROC curves for the individual indicators. The results show that the area under the ROC curve (AUC) of quadriceps muscle strength is 0.876 (95% CI: 0.840~0.913), and the AUC of ΔSPO2 is 0.722 (95% CI: 0.657~0.786), and the sensitivity and specificity of this model are 72.4% and 21.4%, respectively. The AUC of the surgical method was 0.710 (95% CI: 0.652~0.767), and the sensitivity and specificity of the model were 90.9% and 46.6%, respectively. The AUC of respiratory muscle strength is 0.710 (95% CI: 0.652~0.767), and the AUC of the floor climbing test is 0.704 (95% CI: 0.641~0.767). The sensitivity and specificity of this model are 76.7% and 35.9%, respectively. The AUC of FEV 1% is 0.699 (95% CI: 0.637 to 0.761), and the sensitivity and specificity of this model are 72.8% and 33.0%, respectively. The AUCof DLCO% is 0.608 (95% CI: 0.542~0.674). The sensitivity and specificity of the model are 63.4% and 41.7%, respectively. The results showed that the AUC values of skeletal muscle function and floor climbing test were numerically greater than FEV 1% and DLCO%.
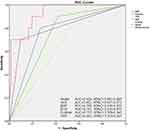 |
Figure 1 The accuracy of the model for predicting the probability of postoperative complications was evaluated by use of the ROC curve. |
Discussion
Assessment of cardiopulmonary function before lung resection surgery is very important for determining the surgical indications, the scope of resection, and the cardiopulmonary complications that may occur during the perioperative period. At present, there is expert consensus in China, mainly through lung function, including FEV 1, DLCO, prediction of forced expiratory volume in the first second after surgery (PPO-FEV 1), prediction of postoperative lung carbon monoxide diffusion (PPO-DLCO) and cardiopulmonary exercise test (CPET),2 etc., among which CPET is the gold standard for the assessment of surgical risk in NSCLC patients. Among surgical patients with COPD and non-small cell lung cancer, some studies reported that the probability of non-small cell lung cancer patients with COPD was 40.54% was significantly higher than that of NSCLC alone 22.35%, and the incidence of perioperative cardiopulmonary complications was higher.7 However, the current methods to evaluate cardiopulmonary complications after COPD with non-small cell lung cancer (NSCLC) are limited, and further research and exploration of more detection methods are needed to assess the risk associated with developing cardiopulmonary complications during the perioperative period. By analyzing the skeletal muscle function level of patients with COPD combined with NSCLC, our study clarified that these two indicators have important predictive ability to predict postoperative cardiopulmonary complications in patients with COPD combined with NSCLC.
Our results suggest that 132 cases of postoperative cardiopulmonary complications occurred. It occurred in 103 patients, accounting for 30.7% of the enrolled cases. There were 54 (16.1%) persistent lung leaks, 48 (14.3%) lung infections, respiratory failure led to re-tracheal intubation in 15 cases, 27 cases of atelectasis (8.1%). The complications in our study subjects were higher than those reported by Dong8 for pneumonia (1.8%), retention of CO 2 (2.4%), and atelectasis (3.5%), which may be related to our enrolled patients were combined with COPD. Their study also believes that the climbing test can be a means of assessing the complications of lung surgery. Some have also reported that pulmonary respiratory complications may be related to the size of lobectomy, and COPD patients are an independent risk factor for pulmonary surgery,9 which may also explain the higher incidence of cardiopulmonary complications in our study.
The results of this study showed that in the complication group, the indicators representing skeletal muscle function, including quadriceps muscle strength, respiratory muscle strength, and 6 MWD were lower than those in the noncomplicated group. The results of multivariate analysis suggest that quadriceps muscle strength and respiratory muscle strength could have a predictive value of postoperative cardiopulmonary complications in patients with COPD and NSCLC (P <0.05). Han-Yu Deng et al10 showed that patients with sarcopenia after surgical resection of non-small cell lung cancer had a significantly worse prognosis than those without sarcopenia, especially in early stage patients. Sarcopenia is an independent risk factor for postoperative complications in patients with NSCLC. This can be seen by the ROC curve results. Skeletal muscle function indicators including respiratory muscle strength and quadriceps muscle strength, and floor climbing tests have more predictive power of postoperative cardiopulmonary complications in patients with COPD and lung cancer than FEV 1% and DLCO% of lung function. The results showed that the AUC values of skeletal muscle function and floor climbing test were numerically greater than FEV 1% and DLCO%. Previous studies have shown that,11 chronic obstructive pulmonary disease (COPD) due to inflammation, hypercapnia, mitochondrial dysfunction, oxidative and nitrosative stress, hypoxia, and multiple other metabolic changes, and possible factors associated with genetic and epigenetic modification, lead to the imbalance between muscle cell anabolism and catabolism, resulting in skeletal muscle dysfunction. Studies have reported that,12 weakened skeletal muscle function is a risk factor for complications after lung cancer lung resection, and the incidence of postoperative complications (29.0%) is higher than that of patients with normal skeletal muscle function (4.2%). Therefore, weakened skeletal muscle function is related to the occurrence of postoperative cardiopulmonary complications in patients with COPD combined lung cancer.
The indicators such as lung function and CPET have long been used as the primary predictive indicators of cardiopulmonary complications after lung resection. In recent years, many studies have found that the stair climbing test has great significance in the preoperative evaluation of lung resection surgery and can replace CPET to some extent. In the 2013 American Association of Chest Physicians guidelines for preoperative evaluation of lung resection surgery,13 it is recommended to further improve the assessment of exercise capacity such as CPET for patients with low lung function. Our study showed that preoperative FEV 1%, DLCO%, completing the stair climbing test and Δ SPO 2 had predictive value for cardiopulmonary complications after COPD combined with NSCLC (P <0.05). A meta-analysis of 2038 lung cancer surgery patients by Boujibar et al14 also showed that climbing height, climbing time, and oxygen saturation change in the stair climbing test can be used as the first-line cardiopulmonary function screening indicators and are predictive of complications after lung resection. Dong et al8 conducted 171 NSCLC patients to evaluate the risk of surgical complications, and the results suggested that the change of blood oxygen saturation in the stair climbing test can effectively predict postoperative complications, which is a simple and effective method. These results are similar to our study results, but the height of climbing and the speed of climbing are not completely consistent, so there may be differences in the results. For patients with COPD and NSCLC, acute attack of COPD may be occured in the process of climbing test, so corresponding medical support should be provided in clinical test.
Conclusion
Skeletal muscle function measurement, stair climbing test, FEV 1, surgical method and DLCO% can be used as the evaluation method of surgical risk in COPD patients with lung cancer, which can predict the occurrence of postoperative cardiopulmonary complications to some extent, have predictive value for cardiopulmonary complications after COPD with NSCLC. However, due to the short duration, small number of cases, and as a single-center study, the results still have some deficiencies, which should be further verified by large sample size and multi-center studies in the later stage.
Data Sharing Statement
The data will be available upon reasonable request to the corresponding authors.
Ethics Approval and Informed Consent
Ethical approval was obtained from the human research ethics committee of West China (Airport) Hospital Sichuan University (2022-ks-06). We confirmed this study complied with the Declaration of Helsinki. All participants had signed the informed consent form.
Acknowledgments
We gratefully thank research assistant Hong LI and assistant XiaoMin Luo of West China (Airport) Hospital Sichuan University for their contribution to the data collection of patients.
Funding
This work was supported by grants from the Chengdu Medical Scientific Research Project (2022103).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kobayashi S, Tsuchiya K, Nishide M, Nishikiori T, Nakagawa T, Shimada N. Pironetin, a novel plant growth regulator produced by Streptomyces sp. NK10958. III. Biosynthesis. J Antibiot. 1995;48(8):893–895. doi:10.7164/antibiotics.48.893
2. Rowland AJ, Dixon PN, Holliger B, Wofinden RC. Evaluation of home nurse attachment in Bristol. Br Med J. 1970;4(5734):545–547. doi:10.1136/bmj.4.5734.545
3. Matzke AJ, Matzke MA. Position effects and epigenetic silencing of plant transgenes. Curr Opin Plant Biol. 1998;1(2):142–148. doi:10.1016/S1369-5266(98)80016-2
4. Graham BL, Steenbruggen I, Miller MR, et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019;200(8):e70–e88. doi:10.1164/rccm.201908-1590ST
5. Kaaks R, Christodoulou E, Motsch E, et al. Lung function impairment in the German Lung Cancer Screening Intervention Study (LUSI): prevalence, symptoms, and associations with lung cancer risk, tumor histology and all-cause mortality. Transl Lung Cancer Res. 2022;11(9):1896–1911. doi:10.21037/tlcr-22-63
6. Enright PL. The six-minute walk test. Respir Care. 2003 ;48(8):783–785. PMID:12890299.
7. Chapanis A, Scarpa LC. Readability of dials at different distances with constant visual angle. Hum Factors. 1967;9(5):419–426. doi:10.1177/001872086700900504
8. Dong J, Mao Y, Li J, He J. Stair-climbing test predicts postoperative cardiopulmonary complications and hospital stay in patients with non-small cell lung cancer. Med Sci Monit. 2017;23:1436–1441. doi:10.12659/MSM.900631
9. Pezzuto A, Trabalza Marinucci B, Ricci A, et al. Predictors of respiratory failure after thoracic surgery: a retrospective cohort study with comparison between lobar and sub-lobar resection. J Int Med Res. 2022;50(6):3000605221094531. doi:10.1177/03000605221094531
10. Deng HY, Hou L, Zha P, Huang KL, Peng L. Sarcopenia is an independent unfavorable prognostic factor of non-small cell lung cancer after surgical resection: a comprehensive systematic review and meta-analysis. Eur J Surg Oncol. 2019;45(5):728–735. doi:10.1016/j.ejso.2018.09.026
11. Henrot P, Dupin I, Schilfarth P, et al. Main pathogenic mechanisms and recent advances in COPD peripheral skeletal muscle wasting. Int J Mol Sci. 2023;24(7). doi:10.3390/ijms24076454
12. Shinohara S, Otsuki R, Kobayashi K, Sugaya M, Matsuo M, Nakagawa M. Impact of sarcopenia on surgical outcomes in non-small cell lung cancer. Ann Surg Oncol. 2020;27(7):2427–2435. doi:10.1245/s10434-020-08224-z
13. Brunelli A, Kim AW, Berger KI, Addrizzo-Harris DJ. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e166S–e190S. doi:10.1378/chest.12-2395
14. Boujibar F, Gillibert A, Gravier FE, et al. Performance at stair-climbing test is associated with postoperative complications after lung resection: a systematic review and meta-analysis. Thorax. 2020;75(9):791–797. doi:10.1136/thoraxjnl-2019-214019
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
