Back to Journals » OncoTargets and Therapy » Volume 11
Predictive value of LDH kinetics in bevacizumab treatment and survival of patients with advanced NSCLC
Authors Li B, Li C, Guo M, Shang S, Li X , Xie P , Sun X, Yu J , Wang L
Received 19 April 2018
Accepted for publication 19 August 2018
Published 27 September 2018 Volume 2018:11 Pages 6287—6294
DOI https://doi.org/10.2147/OTT.S171566
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jianmin Xu
Butuo Li,1,2,* Cheng Li,3,* Meiying Guo,2,4 Shuheng Shang,2,4 Xiaogang Li,5 Peng Xie,2 Xindong Sun,2 Jinming Yu,1,2 Linlin Wang2
1Department of Radiation Oncology and Key Laboratory of Cancer Prevention and Therapy, Tianjin Medical University, Tianjin, People’s Republic of China; 2Department of Radiation Oncology, Shandong Cancer Hospital Affiliated to Shandong University, Shandong Academy of Medical Science, Jinan, People’s Republic of China; 3Department of Dean’s Office, Shandong Cancer Hospital Affiliated to Shandong University, Shandong Academy of Medical Science, Jinan, People’s Republic of China; 4Department of Radiation Oncology, School of Medicine, Shandong University, Jinan, People’s Republic of China; 5Department of Radiation Oncology, School of Medicine and Life Sciences, University of Jinan-Shandong Academy of Medical Sciences, Jinan, People’s Republic of China
*These authors contributed equally to this work
Background: The combination of bevacizumab and chemotherapy is still one of the standard treatments for advanced non-small-cell lung cancer (NSCLC) patients in the new era of targeted therapy. Although a high level of baseline lactate dehydrogenase (LDH) was found to predict survival benefit from bevacizumab in patients with metastatic colorectal cancer, the predictive value of serum level of LDH in NSCLC patients treated with bevacizumab has not been investigated yet. Moreover, dynamic evaluation of serum level of LDH changes may be more informative and promising in predicting patients’ prognosis. We thus sought to analyze LDH kinetics and evaluate its predictive role in the response and survival of advanced NSCLC patients treated with bevacizumab.
Method: We retrospectively collected and analyzed a total of 161 advanced NSCLC patients who had undergone treatment with bevacizumab. Univariate and multivariate logistic regression analyses of serum level of LDH were used for response analyses, and Cox models for both overall survival (OS) and progression-free survival analyses (PFS). Longitudinal analysis of LDH was performed using a mixed-effect regression model.
Results: On multivariate Cox models, increase of serum level of LDH after 4 cycles with bevacizumab (INC4) treatment was shown to be the independent risk factor for OS (hazard ratio =2.17, 95% CI: 1.21–3.90, P=0.009), and the serum level of LDH after 2 cycles (LDH2) and the increase of LDH after 6 cycles with bevacizumab (INC6) treatment were the predictive factors for PFS (hazard ratio =2.33, 95% CI: 1.38–3.93, P=0.001; hazard ratio =1.96, 95% CI: 1.27–3.03, P=0.002, respectively). Patients with increase of serum level of LDH after 2 cycles of treatment with bevacizumab (INC2) (odds ratio =3.75, 95% CI: 1.83–7.68, P<0.001) were more likely to attain stable disease/progressive disease on multivariate logistic regression analyses, while patients with complete response (CR)/partial response (PR) experienced a reduction of serum level of LDH every 2 cycles (Coef =-0.076, std error =0.017, P<0.001) over time.
Conclusion: Dynamic changes of LDH were superior to baseline LDH in predicting prognosis of NSCLC patients treated with bevacizumab. Serum level of LDH reducing over time was a potential biomarker for patients to achieve good clinical response (CR/PR) to bevacizumab.
Keywords: lactate dehydrogenase, bevacizumab, non-small-cell lung cancer, mixed-effect model, predictive factor
Introduction
Non-small-cell lung cancer (NSCLC) accounts for almost 85% of all newly diagnosed cancers every year.1 Although the efficacy has been improved by the clinical use of EGFR-TKIs,2,3 ALK-TKIs,4 checkpoint inhibitors,5–7 and other drugs in the new era of targeted therapy, bevacizumab combined with chemotherapy is still the recommended option for nonsquamous NSCLC patients without driver genes.8–10 Moreover, bevacizumab was also combined with other target agents such as erlotinib, alectinib, osimertinib, and pembrolizumab for improving outcomes of NSCLC patients.11,12 Unfortunately, it remains difficult to identify suitable patients who can obtain benefits from using bevacizumab, and the prognosis of advanced NSCLC patients treated with bevacizumab is still extremely poor, with the median overall survival (OS) ranging from 12.3 to 24.3 months. Thus, sensitive and specific factors for predicting the response and prognosis of NSCLC patients treated with bevacizumab are urgently needed.
It is widely recognized that the growth and proliferation of tumor cells rely on anaerobic respiration, converting glucose to lactate, even under aerobic conditions. Lactate dehydrogenase (LDH) plays a pivotal role in glycolysis by catalyzing the interconversion between pyruvate and lactate, and it is considered to be a poor prognosis marker in several cancers, including NSCLC.13,14 Interestingly, the enrichment of LDH in tumor tissue has been demonstrated to be significantly associated with angiogenic factors including VEGF, bFGF, and TP,15 demonstrating the close relationship between LDH and tumor angiogenesis. Besides, a high baseline level of LDH was found to be promising in predicting the survival benefit from bevacizumab, a VEGF-signaling inhibitor, in patients with metastatic colorectal cancer.16–18 Nevertheless, the predictive value of serum level of LDH in NSCLC patients treated with bevacizumab has not been investigated yet.
Emerging evidence has shown that the microenvironment of cancer undergoes dynamic changes during treatment.19 The hypoxic nature of the tumor microenvironment, commonly induced by insufficient tumor angiogenesis, could be shifted during treatment, especially when including agents targeting tumor vasculature.20,21 However, information regarding baseline LDH level is extremely limited. Dynamic evaluation of serum level of LDH changes might be more accurate and informative for predicting the response and survival of patients with NSCLC after administration of bevacizumab, and it would be valuable information for therapeutic decision-making in clinical practice.
Therefore, the aim of our study was to evaluate the prognostic value of dynamic changes of serum level of LDH in advanced nonsquamous NSCLC patients treated with bevacizumab, and for the first time to explore the role of LDH longitudinal kinetics in predicting the early response of bevacizumab in these patients.
Materials and methods
Patient population
This study was approved by the Institutional Review Board of Shandong Cancer Hospital Affiliated to Shandong University (no SDTHEC20171206). All procedures were in accordance with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. For this retrospective study, formal written informed consent from all patients was not required, and all data were kept confidential. A total of 161 patients with advanced or recurrent NSCLC treated with bevacizumab plus standard chemotherapy between June 2011 and February 2018 were included in this study. Patient inclusion criteria comprised a diagnosis of stage IIIB or IV or recurrent nonsquamous NSCLC with no prior anti-VEGF therapy. Eligible patients were ≥18 years old, with an Eastern Cooperative Oncology Group performance status of 0 or 1, and histologically confirmed nonsquamous NSCLC, with adequate hepatic, renal, and bone marrow functions. Main exclusion criteria included gross hemoptysis, therapeutic anticoagulation, history of documented hemorrhagic or coagulated disease, the use of drugs inhibiting platelet function, clinically significant cardiovascular disease, and uncontrolled hypertension.
Detailed data on the serum levels of biological markers and other clinical factors, including gender, age, smoking status, EGFR status, and the presence of liver metastases, brain metastases, bone metastases, were collected retrospectively for all patients using uniform database templates to ensure consistent data collection. The response, defined as disease status after 6 cycles of bevacizumab, was assessed according to Response Evaluation Criteria in Solid Tumors version 1.1.
Statistical analysis
High level of baseline LDH was defined as baseline LDH exceeding 245 U/L, which was the upper limit of normal of LDH. Changes of LDH (CHG) during bevacizumab treatment were defined as decrease or increase compared with baseline LDH after 2, 4, or 6 cycles of bevacizumab treatment, respectively.
Associations of baseline LDH status with patient characteristic were analyzed by χ2 test as appropriate. Univariate and multivariate logistic regression analyses were used to describe the association between variables and response including LDH levels and CHG during bevacizumab treatment. Kaplan–Meier plots were used to assess and present the OS and progression-free survival (PFS) based on baseline LDH status. The proportional hazards assumption for Cox models was checked and validated first; then univariate and multivariate proportional hazards Cox models were used in both OS and PFS analyses to assess the independent prognostic values. If the proportional hazards assumption did not hold, time × covariates interaction Cox model was used. Variables with P<0.1 in univariate analyses were included in multivariate Cox models.22,23 Results were presented as hazard ratios (HR) with 95% confidence intervals (95% CIs). Survival and logistic analyses were conducted using SPSS 24 (IBM Corporation, Armonk, NY, USA).
A mixed-effect regression model with per-patient random intercept and slope were performed for the longitudinal analyses for LDH using R v3.4.4 (The R Foundation, Vienna, Austria). The value of LDH was transformed to be normally distributed to better perform regression analysis. Transformed LDH was defined as ln (LDH-105.8) using a zero-skewness log transformation in Stata v12.0 (StataCorp LLC, College Station, TX, USA).
Results
Patient characteristics
After a median follow-up of 17.1 months (2.3–86.3 months), a total of 161 advanced nonsquamous NSCLC patients treated with bevacizumab were enrolled in our study, and 87 patients were still alive at the end of follow-up. Baseline characteristics were well balanced in groups divided by high and low baseline serum level of LDH (Table 1).
  | Table 1 Baseline characteristics |
Survival analysis
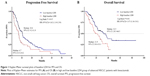
The median PFS and OS for all patients was 8.7 months (95% CI: 6.5–10.9) and 27.9 months (95% CI: 21.2–34.5), respectively. In low baseline LDH group, the PFS of patients was much better than that in high LDH group (10.6 vs 6.7 months, 95% CI: 5.2–8.2 vs 9.2–11.9, P=0.014, Figure 1A), and OS benefit was also found in the low LDH group with statistical significance (32.5 vs 21.9 months, 95% CI: 20.5–44.5 vs 10.6–33.1, P=0.01, Figure 1B).
Univariate Cox models were then performed for analyzing the variables related with OS and PFS in all patients (Tables 2 and 3). Smoking history, central tumor, bone metastasis, and liver metastasis were found to be associated with inferior OS and PFS. In terms of the serum level of LDH, high level of LDH at baseline and cycle 2, 4, 6 and increase of CHG2, CHG4, CHG6 (INC2, INC4, and INC6, respectively) were significantly correlated with worse PFS and OS.
On multivariate analyses, central tumor remained the independent risk factor for both progression and death, and liver metastasis and bone metastasis were the independent risk factors for PFS and OS, respectively. High LDH level at cycle 2 (LDH2) and increase of CHG6 (INC6) were associated with inferior PFS (HR =2.33, 95% CI: 1.38–3.93, P=0.001; HR =1.96, 95% CI: 1.27–3.03, P=0.002), while CHG4 of increased serum level of LDH (INC4) was shown to be an independent risk factor for OS (HR =2.17, 95% CI: 1.21–3.90, P=0.009) (Tables 2 and 3).
Response analysis
Overall, 68/161 patients achieved complete response (CR)/partial response (PR) after 6 cycles of bevacizumab treatment. As shown in Table 4, central tumor, bone metastasis, high LDH level at cycle 2 and 4, and increase of CHG2, CHG4, and CHG6 (INC2, INC4, and INC6, respectively) were associated with lower odds of CR/PR by univariate logistic regression analysis. On multivariate analyses, increase of CHG2 (INC2, odds ratio=3.75, 95% CI: 1.83–7.68, P<0.001) was shown to be independent in predicting worse response to bevacizumab (Table 4).
Mixed-effects regression analysis of LDH during treatment
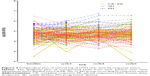
We subsequently analyzed LDH over time. A mixed-effect regression analysis with per-patient random intercept was used to analyze changes in LDH during 6 cycles of treatment. A spaghetti plot of transformed LDH is shown in Figure 2. Patients with CR/PR and stable disease (SD) had a lower log-transformed baseline LDH compared with patients with progressive disease (PD) (Coef =−0.28, std error =0.11, P=0.009 and Coef =−0.39, std error =0.11, P=0.001, respectively). Besides, patients with a response of CR/PR had a −0.076 change in transformed LDH every 2 cycles of bevacizumab treatment (std error =0.017, P<0.001) compared with patients with PD, while there was no statistical significance when compared patients with SD (Coef =−0.023, std error =0.017, P=0.18). When combining patients with SD and PD, patients with CR/PR experienced a −0.062 changes in transformed LDH every 2 cycles (std error =0.013, P<0.001).
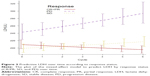
We further applied the mixed-effects regression model to predict LDH by response category (Figure 3), which showed that patients with CR/PR on bevacizumab experienced a reduction in LDH over time compared with SD and PD patients.
Discussion
LDH has been demonstrated to be an indirect marker of tumor hypoxia, neoangiogenesis, and metastasis and is associated with poor prognosis in several cancers,13,14 including NSCLC.15,24–28 Besides, high level of baseline LDH was found to predict a worse outcome in metastatic colorectal cancer patients with bevacizumab or receiving beyond-progression administration of bevacizumab in combination with chemotherapy.16–18 However, the potential role of serum level of LDH in advanced nonsquamous NSCLC treated with bevacizumab was still unknown. Here, we studied for the first time the kinetics of serum level of LDH during bevacizumab treatment and evaluated its predictive role in the response and survival of NSCLC patients.
Bevacizumab, a humanized anti-VEGF antibody, is widely used in NSCLC and metastatic colorectal cancers and could induce transient “normalization” of vasculature and thus improve oxygen distribution in tumors.29,30 Since serum level of LDH was shown to be an indirect factor indicative for hypoxia in tumor tissues with large tumor burden,13,14 it seems plausible that the improvement of hypoxia in the tumor microenvironment by bevacizumab could be reflected by the decrease of serum level of LDH. Therefore, dynamic changes of serum level of LDH may more exactly and in a more sensitive manner reveal the real hypoxia status during treatment. In our present study, baseline LDH was found to be associated with worse PFS and OS in advanced nonsquamous NSCLC patients treated with bevacizumab, which is in agreement with previous results seen in NSCLC patients without bevacizumab.15,28 However, the baseline level of LDH loses its significance in multivariate Cox models, and only CHG during bevacizumab treatment are shown to be independently predictive in progression and death, demonstrating that the dynamic changes in serum level of LDH are superior to baseline evaluation in predicting the prognosis of NSCLC patients treated with bevacizumab.
Moreover, we found that the level of baseline LDH was not correlated with response to bevacizumab in NSCLC patients. Instead, increase of serum level of LDH after 2 cycles of bevacizumab was an independent factor for poor response to bevacizumab in multivariate regression analysis. Mixed-effects regression analysis also indicated that serum level of LDH in patients with CR/PR showed a consistent decrease over time, with an increase seen in patients with PD and SD. Thus, dynamically monitoring serum level of LDH before and during bevacizumab treatment for advanced NSCLC patients might be helpful for identifying patients who can obtain clinical benefit from bevacizumab. And the obvious increase of LDH level during treatment may be an early marker of the resistance to bevacizumab before imaging detection. Although our findings still need to be validated in prospective trials, the estimation of serum level of LDH might provide additive value for early evaluation of the response to bevacizumab.
In the new era of targeted therapy, checkpoint inhibitors, including nivolumab and pembrolizumab, have shown encouraging results with regard to overall response rates, OS, and PFS in advanced NSCLC.5–7 Interestingly, VEGF not only promotes angiogenesis but also acts as a key mediator in inhibiting T-cell infiltration and helping tumor cells escape from immune surveillance.31 Blockage of VEGF was also found to increase T-cell numbers beyond lessened vascularity and then inhibit the tumor growth.32 Thus, combination of antiangiogenic therapy and immunotherapy is considered promising, and several trials are ongoing to evaluate the clinical benefits from bevacizumab combined with checkpoint inhibitors in several cancers, such as colorectal cancer (NCT02876224), NSCLC (NCT02681549), renal cell carcinoma (NCT03066427), and recurrent solid tumors (NCT02857920). Consequently, the observation of LDH changes during bevacizumab treatment might highlight the importance of exploring the time point at which the immunotherapies could be administrated.
Our study also has some limitations. First, this was a retrospective study carried out in a single center with limited patients, and so we cannot fully exclude information collection bias, because of it not being planned ahead of time. Second, we cannot totally control for all possible risk factors for cancer patients. Also, the level of LDH can be influenced by several factors, even with the balance of other factors. The exact mechanism underlying the correlation between LDH and angiogenesis must also be solved through further investigations.
Conclusion
Our results indicated that dynamic CHG were superior to baseline LDH in predicting outcomes for NSCLC patients treated with bevacizumab. Patients experiencing reduction of serum LDH level during treatment might achieve more clinical benefits from bevacizumab. Nevertheless, further prospective studies are required to validate the role of LDH kinetics in predicting the response and survival of NSCLC patients treated with bevacizumab.
Acknowledgment
This work was supported by the following grants: Natural Science Foundation of Shandong Province (Grant no ZR2016HM41 and ZR2015HZ004), the Project of Postdoctoral Innovation of Shandong Province (Grant no 201501010 and 201601006), the Project of Postdoctoral Science Foundation of China (Grant no 2016M590640), and National Natural Science Foundation of China (Grant no 81472812).
Disclosure
The authors report no conflicts of interest in this work.
References
Torre LA, Siegel RL, Ward EM, Jemal A. Global Cancer Incidence and Mortality Rates and Trends – An Update. Cancer Epidemiol Biomarkers Prev. 2016;25(1):16–27. | ||
Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. The Lancet Oncology. 2012;13(3):239–246. | ||
Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. The Lancet Oncology. 2010;11(2):121–128. | ||
Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. The New England Journal of Medicine. 2014;371(23):2167–2177. | ||
Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N Engl J Med. 2015;373(2):123–135. | ||
Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med. 2015;373(17):1627–1639. | ||
Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387(10027):1540–1550. | ||
Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355(24):2542–2550. | ||
Reck M, von Pawel J, Zatloukal P, et al. Overall survival with cisplatin-gemcitabine and bevacizumab or placebo as first-line therapy for nonsquamous non-small-cell lung cancer: results from a randomised phase III trial (AVAiL). Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2010;21(9):1804–1809. | ||
Zhou C, Wu YL, Chen G, et al. BEYOND: A Randomized, Double-Blind, Placebo-Controlled, Multicenter, Phase III Study of First-Line Carboplatin/Paclitaxel Plus Bevacizumab or Placebo in Chinese Patients With Advanced or Recurrent Nonsquamous Non-Small-Cell Lung Cancer. J Clin Oncol. 2015;33(19):2197–2204. | ||
Manegold C, Dingemans AC, Gray JE, et al. The Potential of Combined Immunotherapy and Antiangiogenesis for the Synergistic Treatment of Advanced NSCLC. J Thorac Oncol. 2017;12(2):194–207. | ||
Wang J, Chen J, Guo Y, Wang B, Chu H. Strategies targeting angiogenesis in advanced non-small cell lung cancer. Oncotarget. 2017;8(32):53854–53872. | ||
Granchi C, Bertini S, Macchia M, Minutolo F. Inhibitors of lactate dehydrogenase isoforms and their therapeutic potentials. Curr Med Chem. 2010;17(7):672–697. | ||
Langhammer S, Najjar M, Hess-Stumpp H, Thierauch KH. LDH-A influences hypoxia-inducible factor 1α (HIF1 α) and is critical for growth of HT29 colon carcinoma cells in vivo. Target Oncol. 2011;6(3):155–162. | ||
Koukourakis MI, Giatromanolaki A, Sivridis E, et al. Lactate dehydrogenase-5 (LDH-5) overexpression in non-small-cell lung cancer tissues is linked to tumour hypoxia, angiogenic factor production and poor prognosis. British Journal of Cancer. 2003;89(5):877–885. | ||
Marmorino F, Salvatore L, Barbara C, et al. Serum LDH predicts benefit from bevacizumab beyond progression in metastatic colorectal cancer. Br J Cancer. 2017;116(3):318–323. | ||
Passardi A, Scarpi E, Tamberi S, et al. Impact of Pre-Treatment Lactate Dehydrogenase Levels on Prognosis and Bevacizumab Efficacy in Patients with Metastatic Colorectal Cancer. PLoS One. 2015;10(8):e0134732. | ||
Yin C, Jiang C, Liao F, et al. Initial LDH level can predict the survival benefit from bevacizumab in the first-line setting in Chinese patients with metastatic colorectal cancer. Onco Targets Ther. 2014;7:1415–1422. | ||
Junttila MR, de Sauvage FJ. Influence of tumour micro-environment heterogeneity on therapeutic response. Nature. 2013;501(7467):346–354. | ||
Koh WJ, Bergman KS, Rasey JS. Evaluation of oxygenation status during fractionated radiotherapy in human nonsmall cell lung cancers using [F-18]fluoromisonidazole positron emission tomography. International Journal of Radiation Oncology, Biology, Physics. 1995;33(2):391–398. | ||
Orlowski K, Rohrer Bley C, Zimmermann M, et al. Dynamics of tumor hypoxia in response to patupilone and ionizing radiation. PLoS One. 2012;7(12):e51476. | ||
Lu S, Tan KS, Kadota K, et al. Spread through Air Spaces (STAS) Is an Independent Predictor of Recurrence and Lung Cancer-Specific Death in Squamous Cell Carcinoma. J Thorac Oncol. 2017;12(2):223–234. | ||
Carluccio E, Biagioli P, Ambrosio G. Prognostic Value of Right Ventricular Dysfunction on Clinical Outcomes After Transcatheter Aortic Valve Replacement. JACC Cardiovasc Imaging. 2018;11(6):932. | ||
Albain KS, Crowley JJ, Leblanc M, Livingston RB. Survival determinants in extensive-stage non-small-cell lung cancer: the Southwest Oncology Group experience. J Clin Oncol. 1991;9(9):1618–1626. | ||
Espinosa E, Feliu J, Zamora P, et al. Serum albumin and other prognostic factors related to response and survival in patients with advanced non-small cell lung cancer. Lung Cancer. 1995;12(1–2):67–76. | ||
Hespanhol V, Queiroga H, Magalhães A, Santos AR, Coelho M, Marques A. Survival predictors in advanced non-small cell lung cancer. Lung Cancer. 1995;13(3):253–267. | ||
Jeremic B, Milicic B, Dagovic A, Aleksandrovic J, Nikolic N. Pretreatment clinical prognostic factors in patients with stage IV non-small cell lung cancer (NSCLC) treated with chemotherapy. J Cancer Res Clin Oncol. 2003;129(2):114–122. | ||
Tas F, Aydiner A, Demir C, Topuz E. Serum lactate dehydrogenase levels at presentation predict outcome of patients with limited-stage small-cell lung cancer. Am J Clin Oncol. 2001;24(4):376–378. | ||
Mountzios G, Pentheroudakis G, Carmeliet P. Bevacizumab and micrometastases: revisiting the preclinical and clinical rollercoaster. Pharmacol Ther. 2014;141(2):117–124. | ||
Goel S, Duda DG, Xu L, et al. Normalization of the vasculature for treatment of cancer and other diseases. Physiol Rev. 2011;91(3):1071–1121. | ||
Voron T, Colussi O, Marcheteau E, et al. VEGF-A modulates expression of inhibitory checkpoints on CD8+ T cells in tumors. J Exp Med. 2015;212(2):139–148. | ||
Shrimali RK, Yu Z, Theoret MR, Chinnasamy D, Restifo NP, Rosenberg SA. Antiangiogenic agents can increase lymphocyte infiltration into tumor and enhance the effectiveness of adoptive immunotherapy of cancer. Cancer Res. 2010;70(15):6171–6180. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.