Back to Journals » Open Access Emergency Medicine » Volume 15
Predictive Factors of Oxygen Therapy Failure in Patients with COVID-19 in the Emergency Department
Authors Suttapanit K , Lerdpaisarn P, Sanguanwit P , Supatanakij P
Received 14 July 2023
Accepted for publication 18 September 2023
Published 4 October 2023 Volume 2023:15 Pages 355—365
DOI https://doi.org/10.2147/OAEM.S430600
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Karn Suttapanit, Peeraya Lerdpaisarn, Pitsucha Sanguanwit, Praphaphorn Supatanakij
Department of Emergency Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Praphaphorn Supatanakij, Department of Emergency Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, 270 Rama VI Road, Ratchathewi, Bangkok, 10400, Thailand, Email [email protected]
Background: Most patients with coronavirus disease 2019 (COVID-19) pneumonia require oxygen therapy, including standard oxygen therapy and a high-flow nasal cannula (HFNC), in the Emergency Department (ED), and some patients develop respiratory failure. In the COVID-19 pandemic, the intensive care unit (ICU) was overburdening. Therefore, prioritizing patients who require intensive care is important. This study aimed to find predictors and develop a model to predict patients at risk of requiring an invasive mechanical ventilator (IMV) in the ED.
Methods: We performed a retrospective, single-center, observational study. Patients aged ≥ 18 years who were diagnosed with COVID-19 and required oxygen therapy in the ED were enrolled. Cox regression and Harrell’s C-statistic were used to identifying predictors of requiring IMV. The predictive model was developed by calculated coefficients and the ventilator-free survival probability. The predictive model was internally validated using the bootstrapping method.
Results: We enrolled 333 patients, and 97 (29.1%) had required IMV. Most 66 (68.0%) failure cases were initial oxygen therapy with HFNC. Respiratory rate-oxygenation (ROX) index, interleukin-6 (IL-6) concentrations ≥ 20 pg/mL, the SOFA (Sequential Organ Failure Assessment) score without a respiratory score, and the patient’s age were independent risk factors of requiring IMV. These factors were used to develop the predictive model. ROX index and the predictive model at 2 hours showed a good performance to predict oxygen therapy failure; the c-statistic was 0.814 (95% confidence level [CI] 0.767– 0.861) and 0.901 (95% CI 0.873– 0.928), respectively. ROX index ≤ 5.1 and the predictive model score ≥ 8 indicated a high probability of requiring IMV.
Conclusion: The COVID-19 pandemic was limited resources, ROX index, IL-6 ≥ 20 pg/mL, the SOFA score without a respiratory score, and the patient’s age can be used to predict oxygen therapy failure. Moreover, the predictive model is good at discriminating patients at risk of requiring IMV and close monitoring.
Keywords: coronavirus disease 2019, COVID-19, oxygen therapy, respiratory rate-oxygenation index, ROX index, predictive model
Backgrounds
Coronavirus disease 2019 (COVID-19) affects mortality owing to viral pneumonia that progresses to acute respiratory distress syndrome and acute hypoxemic respiratory failure. Early strategies in this new emerging disease are intubation in patients with signs of respiratory distress and avoiding non-invasive ventilation or a high-flow nasal cannula (HFNC) that risks aerosol generation.1,2 In a study on COVID-19, HFNC therapy was associated with decreased intubation or mechanical ventilator use and mortality.3
A predictor for oxygen therapy is the respiratory rate-oxygenation (ROX) index at 2, 6, and 12 hours after applying HFNC. This index has been validated in treating hypoxemic respiratory failure without COVID-19.4 Many predictors of COVID-19 have been used to identify patients who require mechanical ventilation and those at risk of mortality, such as biomarkers and physiological parameters.5–9 However, the predictors of failure of intubation remain unclear. The optimal timing of intubation in COVID-19 patients who receive oxygen is controversial. Some studies have shown that early intubation reduces patients’ self-inflicted lung injury and adverse outcomes.1,10–12 In the COVID-19 pandemic, most patients were critical illnesses requiring invasive mechanical ventilation (IMV), leading to the intensive care unit (ICU)‘s overburdening. Therefore, prioritizing patients who require intensive care is important.
This study aimed to evaluate the predictors and develop a predictive model requiring IMV in COVID-19 patients treated with oxygen in the emergency department (ED).
Methods
Study Design and Setting
We performed a retrospective, single-center, at Ramathibodi Hospital, a tertiary care and university hospital in Bangkok. The Ethics Committee of Ramathibodi Hospital, Mahidol University, approved this study (COA. MURA2021/679). The ethics committee did not require consent for this research because the study is based on hospital registry data, and reviewing the medical record is the reason for the waiver and a statement covering patient data confidentiality and compliance according to the Declaration of Helsinki.
Selection of Participants
Patients aged ≥18 years who were diagnosed with COVID-19 and required oxygen therapy in the ED from March 20, 2020, to August 18, 2021, were included in the study. The exclusion criteria included the following: 1) patients who had intubation performed immediately after the ED visit; 2) patients who submitted a do-not attempt to intubation; and 3) missing data.
Definitions
COVID-19 was determined by laboratory-confirmed detection via qualitative reverse transcription-polymerase chain reaction; testing was performed on a nasopharyngeal swab or endotracheal aspirate. Additionally, oxygen therapy, including conventional oxygen therapy, was defined as the delivery of oxygen flow >6 L/min. The inspired oxygen fraction (FiO2) was approximated depending on the oxygen delivery device and oxygen flow delivery. For example, a nasal cannula with a flow of 6 L/min resulted in a FiO2 of approximately 0.44. A non-rebreathing mask with a reservoir bag flow of 10 L/min and 15 L/min resulted in a FiO2 of 0.8 and 1.0, respectively. An HFNC was defined as a device that delivered humidified and heated oxygen at a flow rate >30 L/min. The ROX index was defined as the ratio of oxygen saturation/FiO2 to the respiratory rate. Failure of oxygen therapy was defined as when patients required IMV. The decision to use IMV was dependent on the physician on duty.
Measurements and Clinical Outcomes
Patients included in this study were evaluated by emergency room staff, emergency physicians, and internal medicine residents. We recorded the patients’ demographic information (age, sex, comorbidity, and body mass index), vital signs at initiating oxygen therapy (systolic blood pressure, heart rate, respiratory rate, oxygen saturation, and temperature), and initial oxygen therapy (flow and FiO2). We also recorded the SOFA score without a respiratory score at initiating oxygen, the ROX index at 2, 6, 12 and 24 hours, and laboratory parameters (C-reactive protein (CRP), lactate dehydrogenase, absolute lymphocyte count, D-dimer, albumin, and blood glucose). Furthermore, PF ratio after intubation, time to intubation, and mortality were recorded. The data of participants were identified from Electrical Medical Records (EMR). All patient data were treated with confidentiality following the Declaration of Helsinki.
Our study aimed to assess the predictors and develop a predictive model of oxygen therapy failure within 7 days in patients with COVID-19 in the ED.
Data Analysis
We calculated the sample size required to analyze predictors for oxygen therapy failure. Our hospital data on COVID-19 showed that the intubation rate in patients treated with conventional oxygen therapy and HFNC was 24.9%, and 75.1% of patients were not intubated (N = 198 patients). Therefore, we calculate the sample size by the two-sample proportion test (Pearson’s chi-squared test) of oxygen therapy success and failure. Our calculation showed that 68 patients with COVID-19 who required oxygen therapy in the ED, 17 patients with intubation, and 51 patients with the success of oxygen therapy were needed to provide an adequate sample size for this study (95% power of sample size, 5% alpha error [two-sided test]).
Categorical variables are expressed as absolute values and percentages and continuous variables as mean (standard deviation (SD)) and medians (interquartile ranges (IQRs)). The Cox regression and Harrell’s C were used to assess predictive factors requiring IMV within 7 days in patients with COVID-19. Selected variables in Cox regression with a p-value less than 0.100 were used in multivariable Cox regression to assess the primary outcome. The predictive model was created using variables statistically significant in multivariable Cox regression. Nomogram predictive model was developed from coefficients calculated and survival probability of ventilator-free;13 model calibration was assessed using the proportional-hazards assumption. The predictive model was internally validated using bootstrapping, and 1000 bootstrap replications were drawn. Kaplan–Meier curves were used to determine the probability of being ventilator-free within 7 days in the predictive model and ROX index. Decision curve analysis was performed to assess the benefit of using the model. With the intensity of care in the COVID-19 pandemic, we restricted the probability threshold at 20% for requiring IMV within 48 hours.
Data were recorded and statistical analysis by STATA version 16.1 (StataCorp LLC, College Station, TX, USA).
Results
From March 20, 2020, to August 18, 2021, 407 patients were eligible for inclusion in the study. As a result, 74 patients were excluded according to the exclusion criteria, and 333 patients were finally analyzed (Figure 1).
 |
Figure 1 Study flow chart. |
Among these 333 patients (Table 1), 256 (76.9%) initially had oxygen therapy with an HFNC, and 77 (23.1%) had oxygen therapy with conventional oxygen. Ninety-seven (29.1%) patients had failed oxygen therapy and subsequently received IMV, and death at 28 days after the ED visit occurred in 31 (63.3%). Prediction performance in each variable was shown in Supplementary File 1.
 |
Table 1 The Baseline Characteristics and Univariable Cox Regression Analysis for Risk Factors Associated with Oxygen Therapy Failure in 7 Days in Patients with COVID-19 |
In the cohort, multivariable Cox regression showed patient’s age, the ROX index at 2 hours, IL-6 concentrations ≥20 pg/mL, and the SOFA score without a respiratory score were statistically significant independent factors in patients with oxygen therapy failure (Table 2).
 |
Table 2 Cox Proportion Hazard Model for Analyzing Risk Factors Associated with Oxygen Therapy Failure in 7 Days in Patients with COVID-19 |
The predictive nomogram model was developed with significant factors; the scores for each variable (Supplementary File 2) and ventilator-free survival probability are shown in Figure 2. The proportional-hazards assumption of the predictive model was 0.776. The predictive model was divided into three levels to predict requiring IMV: high risk (score >8; sensitivity 70.10% and specificity 95.76%), intermediate-risk (score 5–8, sensitivity 90.72% and specificity 73.31), low risk (score <5).
 |
Figure 2 The nomogram prediction model for predicting survival probability of ventilator-free within 24 hours, 48 hours and 7 days of COVID-19. |
Predicting the Performance of the Predictive Model for Requiring a Mechanical Ventilator in 7 Days in Patients with COVID-19
The predictive model had a better performance than the ROX index at 2 and 6 hours, as shown by Harrell’s C-statistic, p-value <0.001 and 0.334, respectively, Table 3. The internal validation of the predictive model for predicting oxygen therapy failure is shown in Table 3.
 |
Table 3 Prediction Performance of Predictive Model and ROX Index for Requiring IMV in 7 Days in Patients with COVID-19 in Training Cohort and Bootstrapping Internal Validating |
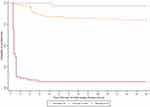
Survival Analysis of the Predictive Model and ROX Index and the Probability of Being Ventilator-Free
The high-risk group of the predictive model (Figure 3) and ROX index <5.1 (Figure 4) indicated a significantly lower probability of being ventilator-free in 7 days than the intermediate and low risk.
Of 97 patients who required IMV, delayed intubation for longer than 48 hours after oxygen therapy appeared to increase 28-day mortality, not significant [crude HR 1.13 (0.63, 2.03), p-value 0.684]. Decision curve analysis for requiring IMV within 48 hours, the predictive model was superior to the ROX index for predicting IMV associated with a threshold probability between 5% and 20%. (Figure 5).
 |
Figure 5 Decision curve analysis for assessing the net benefit between using risk strategy model of the predictive model and ROX index in requiring invasive mechanical ventilation within 48 hours. |
Discussion
In the COVID-19 pandemic, acute respiratory distress syndrome and respiratory failure have affected resources and mortality in the ICU.1–3 Many predictors have been used to predict worsening outcomes of COVID-19, but many studies only focused on the ICU setting.3,5,6
In this study on patients with COVID-19 in the ED, we found that elderly, a low ROX index, high IL-6 concentrations, and a high SOFA score without a respiratory score were associated with oxygen therapy failure within 7 days. Therefore, we developed the predictive model, which had a good performance to predict oxygen therapy failure. The cutoff for predicting the probability of requiring IMV was a ROX index of 5.10 and a predictive model score of more than 8.
In a previous study in the ICU, the ROX index <3.5 showed 89% specificity for HFNC failure.14 Additionally, Zucman et al showed that ROX index >5.37 at 4 hours was a low risk for intubation (66.0% sensitivity and 83.0% specificity).6 Outside of the ICU, a low ROX index indicates an increased risk of requiring IMV.15 Moreover, ROX index <5.9 at 12 hours after HFNC therapy was reported to show 90% specificity for HFNC failure.16 Therefore, our study supports previous evidence that the ROX index helped predict patients who require IMV. We classified patients with COVID-19 into three groups according to the ROX index. In the high-risk group, ROX index <5.1 at 2, 6, 12, and 24 hours showed 98.31%, 96.61%, 98.31%, and 99.15% specificity, respectively, and had a high probability of requiring IMV. In the moderate-risk group, ROX index of 5.11–9.99 at 2, 6, 12, and 24 hours showed 97.94%, 95.38%, 95.83%, and 100.00% sensitivity for requiring IMV, respectively, which suggested that oxygen therapy should be continued and closely monitored. In the low-risk group, ROX index >10 showed a low probability of oxygen therapy failure.
Many studies have identified potential biomarkers associated with COVID-19 pneumonia with a cytokine storm and worse outcomes.17,18 Arnold et al found that IL-6 had a good performance (AUROC: 0.770, 95% CI: 0.65–0.88, cutoff at 79 pg/mL) to predict adverse events and the requirement of respiratory support and ICU admission.7 In our study, IL-6 was a predictor for oxygen therapy failure and better performance than D-dimer, the absolute lymphocyte count albumin, CRP, and lactate dehydrogenase. A cutoff of IL-6 concentrations >20 pg/mL showed 71.13% sensitivity and 83.90% specificity for requiring IMV.
We developed the predictive model by using clinical parameters and biomarkers to identify patients who require IMV at an early stage. The predictive model had a better performance than the individual ROX index at 2 hours for predicting oxygen therapy failure. Additionally, in decision analysis, the predictive model had a better net benefit of predicting oxygen therapy failure within 48 hours than ROX index at 2 hours. The optimal time for intubation remains unclear in COVID-19 pneumonia. Gattinoni et al advocated avoiding delayed intubation to decrease lung injury if reducing respiratory effort was not possible after resolution of hypoxemia by applying oxygen therapy or a non-invasive ventilator.12 Bavishi et al found that delayed intubation led to a higher mortality rate (29%) than that (6%) with intubation within 4–24 hours after hospital admission.19 Our study appeared to show that delayed intubation had an increased risk of mortality, but this was not significant. Based on our results, we strongly support using clinical parameters with laboratory values in patients with COVID-19 pneumonia who require close monitoring and IMV for effective care to decrease adverse outcomes.
Limitations
Our study has several limitations. First, this was a single-center study, which limited the generalization of our results. However, this study had an adequate sample size to assess the outcome. Second, the management of initial oxygen therapy, switching conventional oxygen therapy to HFNC or non-invasive ventilation, and the decision of IMV used were based on physicians in the ED; this condition in medical decisions is a part of real-life practice. In addition, the physicians had been trained in resuscitation in patients with COVID-19 pneumonia. Third, our study excluded most of the patients’ delivery of oxygen flow less than 6 L/min because our setting was categorized as low risk and treated outside the hospital. Fourth, our study did not analyze treatment as the predictor because of varying times in initiated treatment with medication; especially tocilizumab was not the first line in our setting. However, this study was not statistically different from initial medication treatment as remdesivir and intravenous methylprednisolone. Finally, the predictive model only had internal validation performed, and further external validation is required.
Conclusions
This study shows that a low ROX index, high IL-6 concentrations, and a high SOFA score without a respiratory score and elderly are associated with requiring IMV within 7 days. The predictive model has a good performance in discriminating patients who require IMV. The COVID-19 pandemic, which has led to limited available resources, provides a challenge for appropriate allocation resource management of patients. The early identification of patients at risk could guide decision-making and allocation of resources for these patients.
Abbreviations
AUROC, Area under the receiver operating characteristic curve; CI, Confidence level; COVID-19, Coronavirus disease 2019; CRP, C-reactive protein; ED, Emergency Department; FiO2, The inspired oxygen fraction; HFNC, High-flow nasal cannula; ICU, intensive care unit; IL-6, Interleukin-6; IMV, invasive mechanical ventilation; IQR, interquartile range; IVMP, intravenous methylprednisolone; LDH, lactate dehydrogenase; PF ratio, Ratio of the partial pressure of arterial oxygen (PaO2 in mmHg) to inspired oxygen fraction (FiO2); ROX, Respiratory rate-oxygenation; SD, Standard deviation; SOFA, Sequential Organ Failure Assessment.
Data Sharing Statement
The datasets analyzed in this study are not publicly available owing to privacy issues but are available from the corresponding author upon reasonable request.
Ethical Approval
The study was approved by the Ethics Committee of Ramathibodi Hospital, Mahidol University. (COA. MURA2021/679). The ethics committee did not require consent because our study is based on hospital registry data, and reviewing the medical record is the reason for the waiver and a statement covering patient data confidentiality and compliance according to the Declaration of Helsinki. All patient data were treated with confidentiality by the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46(6):1099–1102. doi:10.1007/s00134-020-06033-2
2. de Simone G, Mancusi C. COVID-19: timing is important. Eur J Intern Med. 2020;77:134–135. doi:10.1016/j.ejim.2020.04.019
3. Wendel Garcia PD, Aguirre-Bermeo H, Buehler PK, et al. Implications of early respiratory support strategies on disease progression in critical COVID-19: a matched subanalysis of the prospective RISC-19-ICU cohort. Crit Care. 2021;25(1):175. doi:10.1186/s13054-021-03580-y
4. Roca O, Caralt B, Messika J, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy. Am J Respir Crit Care Med. 2019;199(11):1368–1376. doi:10.1164/rccm.201803-0589OC
5. COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47(1):60–73. doi:10.1007/s00134-020-06294-x
6. Zucman N, Mullaert J, Roux D, Roca O, Ricard JD, Contributors Dan Longrois Didier Dreyfuss. Prediction of outcome of nasal high flow use during COVID-19-related acute hypoxemic respiratory failure. Intensive Care Med. 2020;46(10):1924–1926. doi:10.1007/s00134-020-06177-1
7. Arnold DT, Attwood M, Barratt S, et al. Predicting outcomes of COVID-19 from admission biomarkers: a prospective UK cohort study. Emerg Med J. 2021;38(7):543–548. doi:10.1136/emermed-2020-210380
8. van Dam PMEL, Zelis N, van Kuijk SMJ, et al. Performance of prediction models for short-term outcome in COVID-19 patients in the emergency department: a retrospective study. Ann Med. 2021;53(1):402–409. doi:10.1080/07853890.2021.1891453
9. Mukhtar A, Rady A, Hasanin A, et al. Admission SpO2 and ROX index predict outcome in patients with COVID-19. Am J Emerg Med. 2021;50:106–110. doi:10.1016/j.ajem.2021.07.049
10. Meng L, Qiu H, Wan L, et al. Intubation and ventilation amid the COVID-19 outbreak: wuhan’s experience. Anesthesiology. 2020;132(6):1317–1332. doi:10.1097/ALN.0000000000003296
11. Gattinoni L, Marini JJ, Chiumello D, Busana M, Camporota L. COVID-19: scientific reasoning, pragmatism and emotional bias. Ann Intensive Care. 2020;10(1):134. doi:10.1186/s13613-020-00756-7
12. Gattinoni L, Marini JJ, Busana M, Chiumello D, Camporota L. Spontaneous breathing, transpulmonary pressure and mathematical trickery. Ann Intensive Care. 2020;10(1):88. doi:10.1186/s13613-020-00708-1
13. Zlotnik A, Abraira V. A general-purpose nomogram generator for predictive logistic regression models. Stata Journal. 2015;15(2):537–546. doi:10.1177/1536867X1501500212
14. Mellado-Artigas R, Mujica LE, Ruiz ML, et al. Predictors of failure with high-flow nasal oxygen therapy in COVID-19 patients with acute respiratory failure: a multicenter observational study. J Intensive Care. 2021;9(1):23. doi:10.1186/s40560-021-00538-8
15. Alberdi-Iglesias A, Martín-Rodríguez F, Ortega Rabbione G, et al. Role of SpO2/FiO2 ratio and ROX index in predicting early invasive mechanical ventilation in COVID-19. A pragmatic, retrospective, multi-center study. Biomedicines. 2021;9(8):1036. doi:10.3390/biomedicines9081036
16. Vega ML, Dongilli R, Olaizola G, et al. COVID-19 Pneumonia and ROX index: time to set a new threshold for patients admitted outside the ICU. Pulmonology. 2021;27(5):475–476. doi:10.1016/j.pulmoe.2021.07.001
17. Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G, de Oliveira MHS. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med. 2020;58(7):1021–1028. doi:10.1515/cclm-2020-0369
18. Kermali M, Khalsa RK, Pillai K, Ismail Z, Harky A. The role of biomarkers in diagnosis of COVID-19 - A systematic review. Life Sci. 2020;254:117788. doi:10.1016/j.lfs.2020.117788
19. Bavishi AA, Mylvaganam RJ, Agarwal R, Avery RJ, Cuttica MJ. Timing of intubation in coronavirus disease 2019: a study of ventilator mechanics, imaging, findings, and outcomes. Crit Care Explor. 2021;3(5):e0415. doi:10.1097/CCE.0000000000000415
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.