Back to Journals » Vascular Health and Risk Management » Volume 12
Predictive value of NT-proBNP for 30-day mortality in patients with non-ST-elevation acute coronary syndromes: a comparison with the GRACE and TIMI risk scores
Authors Schellings DAAM, Adiyaman A, Dambrink JH, Gosselink ATM, Kedhi E, Roolvink V, Ottervanger JP, van't Hof AWJ
Received 14 July 2016
Accepted for publication 24 August 2016
Published 21 November 2016 Volume 2016:12 Pages 471—476
DOI https://doi.org/10.2147/VHRM.S117204
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Daniel Duprez
Dirk AAM Schellings,1,2 Ahmet Adiyaman,1 Jan-Henk E Dambrink,1 AT Marcel Gosselink,1 Elvin Kedhi,1 Vincent Roolvink,1 Jan Paul Ottervanger,1 Arnoud WJ van’t Hof,1
1Department of Cardiology, Isala Heart Centre, Zwolle, 2Department of Cardiology, Slingeland Hospital, Doetinchem, the Netherlands
Background: The biomarker N-terminal pro-brain natriuretic peptide (NT-proBNP) predicts outcome in patients with non-ST-elevation acute coronary syndromes (NSTE-ACS). Whether NT-proBNP has incremental prognostic value beyond established risk strategies is still questionable.
Purpose: To evaluate the predictive value of NT-proBNP for 30-day mortality over and beyond the Global Registry of Acute Coronary Events (GRACE) and Thrombolysis In Myocardial Infarction (TIMI) risk scores in patients with NSTE-ACS.
Methods: Patients included in our ACS registry were candidates. NT-proBNP levels on admission were measured and the GRACE and TIMI risk scores were assessed. We compared the predictive value of NT-proBNP to both risk scores and evaluated whether NT-proBNP improves prognostication by using receiver operator curves and measures of discrimination improvement.
Results: A total of 1324 patients were included and 50 patients died during follow-up. On logistic regression analysis NT-proBNP and the GRACE risk score (but not the TIMI risk score) both independently predicted mortality at 30 days. The predictive value of NT-proBNP did not differ significantly compared to the GRACE risk score (area under the curve [AUC]) 0.85 vs 0.87 p=0.67) but was considerably higher in comparison to the TIMI risk score (AUC 0.60 p<0.001). Adjustment of the GRACE risk score by adding NT-proBNP did not improve prognostication: AUC 0.86 (p=0.57), integrated discrimination improvement 0.04 (p=0.003), net reclassification improvement 0.12 (p=0.21).
Conclusion: In patients with NSTE-ACS, NT-proBNP and the GRACE risk score (but not the TIMI risk score) both have good and comparable predictive value for 30-day mortality. However, incremental prognostic value of NT-proBNP beyond the GRACE risk score could not be demonstrated.
Keywords: myocardial infarction, NSTE-ACS, NT-proBNP, GRACE risk score, TIMI risk score
Introduction
In patients presenting with non-ST-elevation acute coronary syndromes (NSTE-ACS) or non-ST-elevation myocardial infarction (NSTEMI), the Thrombolysis In Myocardial Infarction (TIMI) risk score as well as the Global Registry of Acute Coronary Events (GRACE) risk calculation have established predictive value.1–3 However, the GRACE score provides the most accurate stratification of ischemic risk, both on admission and at discharge and has become the recommended risk strategy for early patient decision making.4–6
Beside clinical markers of risk, key element of the GRACE score is the biomarker cardiac troponin (cTn) or high sensitivity (hs)-cTn at present. Beyond diagnostic utility, this biomarker has also important prognostic accuracy in a directly proportional way.4,7 In addition, the biomarker brain natriuretic peptide (BNP) and its N-terminal fragment (NT-proBNP) have shown to provide prognostic information in patients with NSTE-ACS as well, and subsequently improve risk stratification in combination with cTn.8 Whether BNP has really significant incremental value to established NSTE-ACS risk models is still debatable, however.4 In this report, we evaluated the predictive value of baseline NT-proBNP measurement for all cause mortality at 30-day follow-up over and beyond the established TIMI and GRACE risk scores in patients admitted with NSTE-ACS.
Methods
Population
Between 2006 and 2014, individual data from all patients with admission diagnosis of NSTE-ACS (or NSTEMI) admitted at the Isala Heart Centre (Zwolle, the Netherlands) was prospectively recorded. Patients were diagnosed with NSTE-ACS, when they met the definitions according to the European Society of Cardiology-guidelines based on clinical presentation (chest pain), electrocardiogram (EKG) abnormalities, or elevated cardiac enzymes (cTn or hs-cTn > upper limit of normal or doubling of hs-cTn within 3 hours), hence inclusion criteria involved the full clinical spectrum of NSTE-ACS presentation. A written informed consent for data registration and future analysis was obtained from each patient. To avoid double inclusion of patients, only the first recorded admission for NSTE-ACS during the study period was used. Although treatment of patients was to the discretion of the cardiologist and not by protocol, all patients were treated with optimized drug-therapy including angiotensin-converting enzyme inhibitors, β-blockers, aspirin, and lipid-lowering drugs, where appropriate. Study approval was obtained from the ethic committee of the Isala Heart Centre.
Measurements
To study the predictive value of NT-proBNP for 30-day mortality over and beyond the TIMI risk score and the GRACE risk calculator, patients were divided in percentiles according to the different scores and baseline NT-proBNP values. NT-proBNP and hs-cTn were measured in each patient on admission by protocol. Both risk scores were calculated afterward.
The GRACE risk score was calculated by the eight different baseline variables incorporated in the risk calculator: age, heart rate (beats per minute), systolic blood pressure, serum creatinine level, cardiac arrest at admission, ST-segment deviation on EKG, elevated cTn, and congestive heart failure (Killip class). According to the GRACE risk score, patients are classified into three risk groups. For in-hospital mortality, this implies: low (≤108), intermediate (109–140), and high (>140) risk (www.gracescore.org).
The TIMI risk score for NSTE-ACS estimates mortality based on: age ≥65, ≥3 coronary artery disease (CAD) risk factors, known CAD (stenosis ≥50%), aspirin use in the past 7 days, severe angina (≥2 episodes in 24 hours), ST-segment deviation ≥0.5 mm, and positive cardiac markers. This risk score ranges from 0 to 7 points reflecting 5%–41% risk at 14 days of all-cause mortality, new or recurrent myocardial infarction or severe recurrent ischemia requiring urgent revascularization.1
Endpoint
The primary endpoint in this study was death from any cause at 30 days after withdrawal of blood from which the NT-proBNP level was determined.
Statistical analysis
In each patient, the TIMI and GRACE risk scores were calculated. We assessed the predictive value of NT-proBNP, the GRACE risk score, and the TIMI risk score for NSTE-ACS for the primary endpoint by receiver operating characteristic (ROC) curve analysis. To assess the predictive value of the NT-proBNP adjusted risk models, the linear combination of NT-proBNP and each risk model was used. To perform an analysis using the risk model and NT-proBNP together, we calculated weighted scores for each as follows: (β1 * risk score) + (β2 * ln NT-proBNP), where β1 and β2 denote β-coefficients for the risk score and log NT-proBNP obtained from the logistic regression model. Because NT-proBNP was not normally distributed we used logarithmically transformed values. Logistic regression analysis was performed to estimate the influence of NT-proBNP and TIMI/GRACE risk scores on 30-day mortality by calculating the change in area under the curve (AUC).
Additionally, we used two complementary measures of discrimination improvement to evaluate the model performance when NT-proBNP was added to the GRACE or TIMI risk model: the net reclassification improvement (NRI) and the integrated discrimination improvement (IDI). The IDI combines the increase in mortality probability for those experiencing an event plus the decrease in mortality probability for those not experiencing an event. The NRI quantifies the net proportion of subjects getting correctly reclassified to low or high mortality probabilities when adding a predictor to the model using a cut-off point for the predicted probabilities of 10%. AUCs were compared in SAS using PROC Logistic. All statistical analyses were performed using SPSS (version 19) and SAS (version 9.2). A two-sided p-value of <0.05 was considered to be statistically significant.
Results
During the study period, a total of 1324 patients were included. Baseline characteristics are given in Table 1. Mean age was 73 years (standard deviation [SD] 11.6) and most patients had no history of cardiovascular disease, except for hypertension, which was present in 58% of patients. Baseline NT-proBNP levels ranged from 6.0 to 35,000 pg/mL (mean ± SD of 2036±4430), with a median of 519 pg/mL and were available in all patients. The GRACE score could be calculated in 900 patients and ranged from 42 to 281 points (mean ± SD of 139±42), with most patients at intermediate to high risk for in-hospital mortality (25th percentile score ≤ 108). The TIMI score was calculated in 911 patients and ranged from 0 to 7 points (mean ± SD of 3.1±1.4). Values within the 25 percentile ranged from 0 to 2 points. As a consequence, 75% of patients had values between 3 and 7 points.
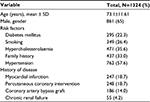  | Table 1 Baseline characteristics of the included NSTE-ACS patients Abbreviations: NSTE-ACS, non-ST-elevation acute coronary syndromes; SD, standard deviation. |
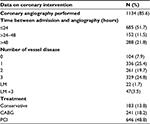
In 1134 (85.6%) patients, coronary angiography was performed during hospital admission. Outcome data are presented in Table 2. Most patients had obstructive CAD and 78% of these patients needed percutaneous coronary intervention or coronary artery bypass grafting.
Ejection fraction (EF) could be measured in 828 patients (63%). In 9.4% of these patients, a poor left ventricular function was present (EF <30%). Most patients had EF >40% (58%).
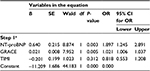
During the 30 days of follow-up, 50 patients died. On logistic regression analysis, NT-proBNP and the GRACE risk score were independent predictors of 30-day mortality (Table 3).
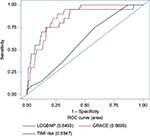
NT-proBNP values among the patients who died, widely ranged from 51 to 35,000 pg/mL (mean ± SD of 8516±9974, median 4505 pg/mL). The GRACE risk score in these patients ranged from 125 to 251 points (mean ± SD of 192±33.2, median 199 points), reflecting patients at higher in-hospital mortality risk. The TIMI score in the patients who died, ranged from 1 to 7 points (mean ± SD of 3.6±1.4, median 4.0 points). Both risk scores and NT-proBNP values were significantly higher in patients who died, compared to those who survived. NT-proBNP values correlated significantly with both risk models but correlation with the GRACE score was stronger than correlation with the TIMI score (Pearson correlation 0.62 and 0.33, respectively p<0.001). At ROC curve analysis, NT-proBNP depicted good predictive value for 30-day mortality (AUC 0.80, range 0.73–0.87). For the GRACE score, AUC was as high as 0.85 (0.79–0.90) but the difference was not significant (p=0.67).
The TIMI risk score, however, revealed a poor predictive value with AUC of 0.61 (0.50–0.71), which was significantly smaller in comparison to NT-proBNP and the GRACE risk score. Adding NT-proBNP to the GRACE risk score revealed no significant improvement of predictive value: AUC 0.86 versus 0.85 (p=0.57), NRI 0.12, (p=0.21), and IDI 0.04 (p=0.003).
However, the combination of NT-proBNP/GRACE, showed a slightly predictive improvement in comparison with NT-proBNP-only (AUC 0.86 vs 0.83, p=0.03). Adding NT-proBNP to the TIMI risk score, considerably improved prognostication of 30-day mortality: AUC 0.84 (p≤0.0001), NRI 0.41 (p=0.001), and IDI 0.1 (p<0.0001). Figure 1 depicts ROC curves of NT-proBNP, and the GRACE and TIMI risk scores. Because comparable analysis could not be performed in patients with missing data, these curves are based on endpoint measurement of 692 patients who had valid values for NT-proBNP and both risk scores, therefore AUC values slightly differ from those found in individual analysis.
Discussion
In this study, NT-proBNP at baseline and the GRACE risk calculator had good and comparable predictive value for 30-day mortality in NSTE-ACS patients and were much more accurate than the TIMI risk score. However, adding NT-proBNP could not enhance the GRACE risk prediction of 30-day mortality.
Previous findings
Natriuretic peptides have been extensively evaluated and showed to be predictors of mortality in patients with ACS, with comparable clinical utility for BNP and NT-proBNP.8 Studies evaluating whether NT-proBNP measurement would improve risk assessment in NSTE-ACS patients beyond the established GRACE or TIMI risk scores have been previously performed. Regarding the GRACE risk score, conflicting results were noticed. Depending on different outcome measures and time points of BNP withdrawal, some reports confirmed incremental value of BNP9–11 while other reports did not or revealed only a small improvement of prognostication.12,13 The TIMI risk score, however, has clearly less predictive accuracy in comparison with BNP and the GRACE score, so that incremental value of BNP to the TIMI risk score logically could be demonstrated.6,9,14–16
Timing of BNP
Although previous findings are consistent with our results, further explanation is required since BNP is predictive in ACS independently of age, EKG change, and cTn concentration; all elements of the GRACE score.17,18 As a consequence, it does make sense that BNP measurement should have additional value in clinical practice. Probably, time of BNP assessment and its relation with outcome measures (short vs longer time mortality) may be of influence. In patients with ACS, elevated baseline cTn concentrations or a rise of high sensitivity cTn within a few hours is often present since elevated cTn values are of diagnostic utility and are anchored in NSTE-ACS definition.8
Baseline NT-proBNP, however, could be within a normal range, even in patients at early mortality risk as demonstrated by our analysis, who would have been detected by the GRACE risk score. Data concerning optimal timing of BNP measurement in NSTE-ACS are limited. One of the aforementioned studies, which confirmed additional value of BNP to the GRACE risk score, was based on measurements at 24–96 hours.9 Furthermore, serial admission BNP measurement in NSTE-ACS has been performed. In one report, patients with chest pain were studied and NT-proBNP samples were collected five times within 24 hours of presentation and at discharge. Although baseline elevated BNP and NT-proBNP were predictive for 30-day adverse events including mortality, serial sampling showed no prognostic improvement.19 Unlike this, another study concerning a high risk subgroup of acute myocardial infarction patients, did reveal that only the highest follow-up BNP remained associated with in hospital death.20 Also in patients with ST-elevation myocardial infarction (STEMI), nonbaseline serial BNP appears to be of optimal predictive value.21,22 Based on this knowledge, we think that the optimum time point for BNP withdrawal and its potential incremental effect on prognostication in NSTE-ACS patients deserve further investigation.
Clinical implications
Beside mortality, nonfatal major adverse cardiac events and also major bleeding are important outcome measures that directly affect patient management and hospital admission duration. The GRACE risk score was developed to predict death, but this score can also predict the risk of bleeding and freedom from clinical events in NSTE-ACS patients for which the GRACE investigators constructed a modified risk model that identified up to 30% of patients at low risk of death or any adverse in-hospital event.23 Whether BNP could be useful in predicting a wide variety of adverse events or the benefit of early revascularization in NSTE-ACS patients has to be determined. However, in STEMI patients, we recently found that baseline NT-proBNP could identify patients eligible for early hospital discharge, with low occurrence of adverse events at 10-day follow-up.24
Limitations
Several limitations have to be noticed. Although all outcome measures were registered prospectively, scores of both the TIMI and GRACE risk models were calculated afterward, and not by protocol; so this may be considered retrospectively. As a consequence, in about one-third of patients, the GRACE and/or TIMI risk scores were unknown due to missing values, which may affect the results. Finally we confined outcome measures to all cause 30-day mortality. Despite this, our results certainly contribute to better understanding of risk assessment by NT-proBNP in clinical practice, since our study cohort consisted of a “real life”, unselected NSTE-ACS patient population.
Conclusion
In NSTE-ACS patients, NT-proBNP and the GRACE risk score (but not the TIMI risk score) both have good and comparable predictive value for 30-day mortality. However, in our study, incremental prognostic value of NT-proBNP beyond the GRACE risk score could not be demonstrated.
Acknowledgment
We would like to thank Mrs Vera Derks for her secretarial support and Dr Petra Koopmans for performing statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284(7):835–842. | ||
Granger CB, Goldberg RJ, Dabbous O, et al; Global Registry of Acute Coronary Events Investigators. Predictors of hospital mortality in the Global Registry of Acute Coronary Events. Arch Intern Med. 2003;163(19):2345–2353. | ||
Fox KA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ. 2006;333(7578):1091. | ||
Roffi M, Patrono C, Collet J-P, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2016;37:267–315. Available from: http://www.escardio.org/guidelines. Accessed September 11, 2015. | ||
Aragam KG, Tamhane UU, Kline-Rogers E, et al. Does simplicity compromise accuracy in ACS risk prediction? A retrospective analysis of the TIMI and GRACE risk scores. PLoS One. 2009;4(11):e7947. | ||
de Araújo Gonçalves P, Ferreira J, Aguiar C, Seabra-Gomes R. TIMI, PURSUIT, and GRACE risk scores: sustained prognostic value and interaction with revascularization in NSTE-ACS. Eur Heart J. 2005;26(9):865–872. | ||
Mueller C. Biomarkers and acute coronary syndromes: an update. Eur Heart J. 2014;35(9):552–556. | ||
Thygesen K, Mair J, Mueller C, et al. Recommendations for the use of natriuretic peptides in acute cardiac care: a position statement from the study group on biomarkers in cardiology of the ESC working group on acute cardiac care. Eur Heart J. 2012;33(16):2001–2006. | ||
Garcia-Alvarez A, Regueiro A, Hernández J, Kasa G, Sitges M, Bosch X, Heras M. Additional value of B-type natriuretic peptide on discrimination of patients at risk for mortality after a non-ST-segment elevation acute coronary syndrome. Eur Heart J Acute Cardiovasc Care. 2014;3(2):132–140. | ||
Guidez T, Marechaux S, Pincon C, et al. Addition of B-type natriuretic peptide to the GRACE score to predict outcome in acute coronary syndrome: a retrospective (development) and prospective (validation) cohort-based study. Emerg Med J. 2012;29(4):274–279. | ||
Widera C, Pencina MJ, Meisner A, et al. Adjustment of the GRACE score by growth differentiation factor 15 enables a more accurate appreciation of risk in non-ST-elevation acute coronary syndrome. Eur Heart J. 2012;33(9):1095–1104. | ||
Meune C, Drexler B, Haaf P, et al. The GRACE score’s performance in predicting in-hospital and 1-year outcome in the era of high-sensitivity cardiac troponin assays and B-type natriuretic peptide. Heart. 2011;97(18):1479–1483. | ||
Ang DS, Wei L, Kao MP, Lang CC, Struthers AD. A comparison between B-type natriuretic peptide, Global Registry of Acute Coronary Events (GRACE) score and their combination in ACS risk stratification. Heart. 2010;96(3):227–228 | ||
Reesukumal K, Pratumvinit B. B-type natriuretic peptide not TIMI risk score predicts death after acute coronary syndrome. Clin Lab. 2012;58(9–10):1017–1022. | ||
Kim JH, Jeong MH, Ahn Y, et al; Other Korea acute Myocardial Infarction Registry (KAMIR) Investigators. A novel risk stratification model for patients with non-ST elevation myocardial infarction in the Korea acute myocardial infarction registry (KAMIR): limitation of the TIMI risk scoring system. Chonnam Med J. 2011;47(1):20–26. | ||
Tello-Montoliu A, Marin F, Roldán V, et al. A multimarker risk stratification approach to non-ST elevation acute coronary syndrome: implications of troponin T, CRP, NT-proBNP and fibrin D-dimer. J Intern Med. 2007;262(6):651–658. | ||
de Lemos JA, Morrow DA, Bentley JH, et al. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Eng J Med. 2001;345(14):1014–1021. | ||
Jernberg T, Stridsberg M, Venge P, Linahl B. N-terminal pro brain natriuretic peptide on admission for early risk stratification of patients with chestpain and no ST-segment elevation. J Am Coll Cardiol. 2002;40(3):437–445. | ||
Kwan G, Isakson SR, Beede J, Clopton P, Maisal AS, Fitzgerald RL. Short-term serial sampling of natriuretic peptides in patients presenting with chest pain. J Am Coll Cardiol. 2007;49(11):1186–1192. | ||
Pesaro AEP, Katz M, Caixeta A, et al. Prognostic value of serial brain natriuretic peptide measurements in patients with acute myocardial infarction. Cardiology. 2015;131(2):116–121. | ||
Ezekowitz JA, Théroux P, Chang W, et al. N-terminal pro-brain natriuretic peptide and the timing, extent and mortality in ST elevation myocardial infarction. Can J Cardiol. 2006;22(5):393–397. | ||
Ezekowitz JA, Théroux P, Welsh R, Bata I, Webb J, Armstrong PW. Insights into the change in brain natriuretic peptide after ST-elevation myocardial infarction (STEMI): why should it be better than baseline? Can J Physiol Pharmacol. 2007;85(1):173–178. | ||
Brieger D, Fox KA, Fitzgerald G, et al; Global Registry of Acute Coronary Events investigators. Predicting freedom from clinical events in non-ST-elevation acute coronary syndromes: The Global Registry of Acute Coronary Events. Heart. 2009;95(11):888–894. | ||
Schellings DA, Adiyaman A, Giannitsis E, et al. Early discharge after primary percutaneous coronary intervention: the added value of N-terminal pro-brain natriuretic peptide to the Zwolle Risk Score. J Am Heart Assoc. 2014;3(6):e001089. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.