Back to Journals » Infection and Drug Resistance » Volume 11
Prediction of imipenem-resistant microorganisms among the nosocomial critically ill patients with Gram-negative bacilli septicemia: a simple risk score
Authors Chen IL, Lee CH , Ting SW, Wang LY
Received 16 November 2017
Accepted for publication 23 January 2018
Published 1 March 2018 Volume 2018:11 Pages 283—293
DOI https://doi.org/10.2147/IDR.S157200
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Joachim Wink
I-Ling Chen,1,2 Chen-Hsiang Lee,2–4 Shih-Wen Ting,2,3 Lily Yu-Chin Wang1
1Department of Pharmacy, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; 2Infection Control Team, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; 3Division of Infectious Diseases, Department of Internal Medicine, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; 4College of Medicine, Chang Gung University, Kaohsiung, Taiwan
Objectives: The increasing number of reports on infections due to carbapenem-resistant Gram-negative bacilli (GNB) has raised concerns, because they have complicated empiric or guided antibiotic therapy for critically ill patients. We aimed to develop a scoring system to predict nosocomial imipenem-resistant GNB (IR-GNB) septicemia among the critically ill patients.
Materials and methods: The study included critically ill adult patients with nosocomial GNB septicemia at Kaohsiung Chang Gung Memorial Hospital (CGMH) in 2013–2015, and the scoring system for predicting IR-GNB septicemia was developed, followed by prospective validation conducted among patients at Linkou CGMH and Kaohsiung CGMH between January and June, 2016.
Results: In the development of the scoring system, 748 patients were included. The independent factors associated with IR-GNB septicemia were prior exposure (days) to carbapenems (adjusted odds ratio [aOR] per 1-day increase, 1.1; 1–3 days: 2 points, 4–6 days: 5 points, 7–9 days: 8 points, and ≥10 days: 13 points), use of mechanical ventilation (aOR 3.7; 5 points), prior colonization with IR-GNB strains (aOR 3.5; 5 points) within 30 days before the onset of GNB septicemia, and comorbid condition with chronic kidney disease (aOR 2.1; 3 points). The internal validation showed an area under the receiver operating characteristic curve (ROC) of 0.75; and an external validation among 314 patients showed similarly good performance (ROC 0.77). Youden’s index indicated the score of ≥6 as the best cutoff value with sensitivity of 75% and specificity of 79%.
Conclusion: This scoring system might help clinicians stratify the risk for developing IR-GNB septicemia among critically ill patients and combined antibiotics may be used until antimicrobial de-escalation/adjustment is clearly indicated by the subsequently identified GNB and its susceptibility profile.
Keywords: antimicrobial resistance, carbapenem, bacteremia, nosocomial infection, scoring system, outcome
Introduction
Bloodstream infection is a major cause of morbidity and mortality worldwide,1 and Gram-negative bacilli (GNB) account for nearly one-half of the cases of bacteremia.2 When confronted with severely septic patients, it is often challenging for physicians to tailor the most suitable empiric regimen to patients before positive blood culture reports are available.3 Before the results of identification and susceptibility testing for GNB strains are available, carbapenems such as imipenem or meropenem have been considered as preferred agents for the treatment of patients with moderate-to-severe infections and risk factors for infection with multidrug-resistant GNB organisms, but are ineffective (when given alone) against carbapenem-resistant pathogens.3
As time to initiation of appropriate therapy is the strongest modifiable independent predictor for mortality in severe sepsis,4 physicians need to act fast in order to impact the patient outcomes. However, due to growing reports globally of infections due to carbapenem-resistant bacteria such as carbapenemase-producing KPC type,5 the empiric administration of an antibiotic combination with the addition of aminoglycosides has been recommended when bacterial resistance is suspected.6 To understand the risk factors for acquiring infections caused by carbapenem-resistant GNB could be useful in directing therapeutic resources in high-risk patients and planning intervention. Most previous studies dealt with patients with a specific pathogen, such as Acinetobacter baumannii or Klebsiella pneumoniae, to investigate the risk factors for bacteremia caused by multidrug-resistant pathogens,5,7 but not those with preliminary blood cultures yielding GNB. To our knowledge, studies are scarce that compare patients with septicemia caused by imipenem-resistant GNB (IR-GNB) to those with septicemia caused by imipenem-susceptible GNB (IS-GNB) at sepsis onset when the preliminary blood cultures yield GNB.
An easy-to-calculate scoring system, with high performance, based solely on parameters readily available at bedside to attending clinicians, is needed in order to direct health care providers in their management of severely septic patients in the hospital setting. Prior attempts to develop a scoring system for predicting septicemia due to IR-GNB had limitations, because it was based on only 16 cases of bacteremia due to carbapenem-resistant Enterobacteriaceae.7 In this study, we aimed to develop a bedside scoring model in order to help physicians quantify the likelihood for septicemia caused by IR-GNB as opposed to IS-GNB, and to prospectively validate the scoring system among a different cohort of patients.
Materials and methods
Patients and setting
This retrospective cohort study was performed in all patients with mono-bacteremia caused by GNB who were admitted to Kaohsiung Chang Gung Memorial Hospital (CGMH), a 2700-bed tertiary-care medical center in southern Taiwan, between January 1, 2013 and December 31, 2015. In this cohort, risk factors independently associated with IR-GNB were identified and were used to develop a clinical prediction score. The scores were further prospectively validated among all GNB mono-bacteremic patients admitted to Kaohsiung CGMH and Linkou CGMH, a 3700-bed tertiary-care medical center in northern Taiwan, between January 1 and June 30, 2016. In this current study (ethical approval and waiver of consent), the patients were made anonymous to maintain confidentiality of the data The Institutional Review Board of the CGMH approved the study (No. 201601503B0) and waived the need for patient consent because of the retrospective nature of the study.
The same inclusion and exclusion criteria were used for all cases in derivation and validation cohorts. The inclusion criteria were based on patients with GNB septicemia, which was defined as the presence of at least two of four possible systemic inflammatory response syndrome characteristics,8 age ≥18 years, and septicemia onset >48 hours after admission. For patients who had more than one episode of GNB septicemia during the study period, only the first episode was considered. These included patients were further divided into cases of GNB septicemia due to IS-GNB and those due to IR-GNB. A schematic flowchart is shown in Figure 1.
  | Figure 1 Flow chart of this study. Abbreviations: IR-GNB, imipenem-resistant Gram-negative bacilli; IS-GNB, imipenem-susceptible Gram-negative bacilli. |
Data collection
The candidate variables were retrieved and reviewed from the CGRDS (Chang Gung Research Database), which provided information about pharmacy dispensing, demographics, and clinical measures, including diagnosis, laboratory results, and health care utilizations. More detailed information, including history of indwelling devices, bloodstream infection source, surgical interventions, exposure history of antibiotics and other drugs (chemotherapeutic agents and steroids) within 30 days before the onset of GNB septicemia, and length of hospital stay before the first isolation of GNB in blood cultures, was also recorded. The initial severity of septicemia was estimated with Pitt bacteremia score9 and the illness severity was evaluated by Sequential Organ Failure Assessment (SOFA) scoring systems calculated during the first 24 hours of septicemia onset. Any of the clinical strains isolated within 30 days before the index GNB septicemia were reviewed to assess the colonization status with IR-GNB.
Microbiologic studies
There were no changes in microbiologic laboratory techniques during the study period. Blood cultures were performed using the BACTEC 9240 system (Becton-Dickinson Sparks, MD, USA). All isolated microorganisms were identified using standard biochemical tests and were verified by a Vitek System (bioMérieux, Marcy l’Etoile, France) using a GNI Card. Susceptibility testing was performed following the guidelines of the Clinical Laboratory Standards Institute (CLSI) for susceptibility testing and the results were interpreted according to the CLSI at the time of the tests.10 Isolates with intermediate susceptibility were considered resistant.
Definitions
Intensive care unit (ICU)-acquired GNB septicemia was defined as the isolation of GNB in at least one blood culture specimen obtained more than 48 hours after septic patients were admitted to the ICU. Bloodstream infection sources were determined clinically based on the presence of an active infection site coincident with bacteremia or the isolation of a microorganism from other clinical specimens before or on the same date of bloodstream infection onset. If the bloodstream infection source could not be assigned to a specific site, it was classified as primary bacteremia. The preexisting comorbidities were assessed using the modified Charlson comorbidity score.11 Corticosteroid therapy was defined by 16 mg prednisone or its equivalent per day at least for 15 consecutive days; neutropenia was defined as <500 neutrophils per microliter of blood; chemotherapy was defined as receipt of cytotoxic antineoplastic drugs within 30 days before the onset of the index GNB septicemia. Exposure history of antibiotics was analyzed by the class of antibiotics as systemic antibiotic use for >48 hours during the 30-day period before septicemia onset. The parenteral antimicrobials listed in the electronic database of the hospital’s pharmacy included carbapenems (ertapenem, doripenem, imipenem, and meropenem), non-extended-spectrum cephalosporins (cefazolin), extended-spectrum cephalosporins (cefuroxime, ceftriaxone, and flomoxef), antipseudomonal cephalosporins (ceftazidime and cefepime), natural penicillin (penicillin G), amino-penicillins (ampicillin and amoxicillin), antipseudomonal penicillins (piperacillin and piperacillin-tazobactam), aminopenicillins/β-lactamase inhibitor (amoxicillin/clavulanate and ampicillin/sulbactam), aminoglycosides (gentamicin and amikacin), fluoroquinolones (ciprofloxacin, levofloxacin, and moxifloxacin), and glycopeptides (vancomycin and teicoplanin). The IR-GNB bacteremia was defined if the GNB isolate was resistant or intermediately susceptible to imipenem.
Statistical analysis
Dichotomous variables were analyzed with the χ2-test or Fisher’s exact test, and continuous variables were analyzed with the Mann–Whitney U-test. Variables with a p ≤0.1 in univariate analysis were then included in the forward stepwise multivariable logistic regression analysis. Predictor reliability was assessed by using a bootstrap resampling technique with 1000 samples.12 Bootstrap consisted of generating 1000 simulated populations from the distribution of the original dataset. Each simulation results in a new sample of the same size as the original data set (748 patients), which is generated through a process of random selection (with replacement) of individuals from the original sample. At each step of the simulation, every individual from the original data set is again eligible to be selected, irrespective of whether he has already been selected, repeating the automated variable selection process by bootstrapping, that is, most frequently selected (at least 50% of the bootstrap samples) variables within bootstrap samples being included in the prediction model may identify true predictors. The discriminatory power of this derivation model was tested using receiver operating characteristic curve (ROC) analysis by assessing the area under the curve (AUC), and the calibration efficiency was tested using Hosmer–Lemeshow goodness-of-fit test for estimating goodness of fits to the data.
A score was then calculated by assigning points based on the regression coefficients obtained from the logistic regression analysis for the independent risk factors of IR-GNB septicemia by transforming the individual parameter estimates (log[OR]/β-values) of the model into weights (points) according to the method used in the Framingham Heart Study.13 Continuous variables will be converted to ordinal categorical variables based on clinically meaningful thresholds and the lowest adjusted OR/β-value will be used as reference for each ordinal variable. An increasing amount of points will then be assigned according to equivalently spaced adjusted OR/β-values. All of these variables were assigned a single point. The best cutoff point was determined when the point yielded the best specificity and sensitivity. The Youden index (sensitivity+specificity−1) was calculated, and the maximum value was used to identify the optimal cutoff.14 The sensitivity, specificity, positive and negative predictive values (PPV and NPV, respectively) for the prediction model at different cutoff values were obtained using a standard definition and methods.15 The scores were applied to a prospectively included cohort of adult patients admitted to Kaohsiung CGMH and Linkou CGMH from January 2016 to June 2016. All analyses were carried out using SAS 9.4 statistical software (SAS Institute, Cary, NC, USA).
Results
A total of 3320 patients with GNB mono-bacteremia was admitted to Kaohsiung CGMH during the retrospective study period; 209 patients were aged <18 years, 1527 patients had episodes of bacteremia before or within 48 hours after admission, and 836 patients did not meet the diagnosis of sepsis; as a result, 748 patients (including 89 with IR-GNB septicemia and 659 with IS-GNB septicemia) were included. The most common pathogens isolated from patients with IS-GNB septicemia were Enterobacteriaceae (445 isolates, 67.5%), and the most common pathogens isolated from patients with IR-GNB septicemia were non-glucose-fermenting GNB (81 isolates, 91.0%; Figure S1).
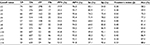
Comparisons of clinical characteristics between the IR-GNB and IS-GNB group are shown in Table 1. Demographics including sex, age, and Charlson comorbidity index were not significantly different among the groups. The risk factors of patients with IR-GNB septicemia in the univariate analysis were SOFA score, Pitt bacteremia score, comorbidity condition with chronic kidney disease and cancer, recent hospitalization within 3 months, septicemia acquired in the ICU, previous colonization with IR-GNB strains within 30 days before the onset of GNB septicemia, and receiving immunosuppressive therapy or invasive procedures and devices (including total parenteral nutrition, neutropenia, central venous catheter, urinary catheter, intubation, and mechanical ventilator support) within 30 days before onset of GNB septicemia. Patients with IR-GNB septicemia had longer lengths of hospital stay before the onset of septicemia, and also had longer exposure duration to almost all classes of antimicrobial agents, except aminopenicillins/β-lactamase inhibitors and extended-spectrum cephalosporins within 30 days before the onset of GNB septicemia (Table 1).
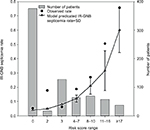
To develop the prediction scores for IR-GNB septicemia, a multivariate logistic regression model investigated all potential predictors identified in univariate analysis, which included duration of exposure to carbapenems, use of mechanical ventilation, previous colonization with IR-GNB strain within 30 days before the onset of GNB septicemia, and comorbid condition with chronic kidney disease (Table 2). The p-value of the Hosmer–Lemeshow test for the model was 0.39, and the area under the ROC curve was 0.79 (95% CI, 0.73–0.84). The risk scores were divided by significant coefficient predictors with the smallest coefficient (0.1116) and resulting quotient was multiplied by two to round to the nearest integer. Overall scores for each of the patients with GNB septicemia were calculated and evaluated for their performance in predicting IR-GNB septicemia. Based on the derivation model, model calibration looked satisfactory; the probability for IR-GNB septicemia in the validation cohort was used to divide subjects into deciles. In each of the deciles, the number of predicted IR-GNB septicemia cases (expected) was compared to the actual number of IR-GNB septicemia cases (observed). Figure 2 showed that the expected number of IR-GNB septicemia cases was less than the observed number of cases for some deciles of risk. The predictability of these collective scores was similar to that of individual predictor-weighted probabilities from the final multivariate logistic regression model (AUC, 0.75; 95% CI, 0.70–0.80). A summary of the diagnostic accuracy of the risk score for the various score cutoff values is shown in Table 3. Youden index indicates that the risk score performed best at a cutoff value of ≥6 points had a sensitivity of 72% and a specificity of 78% (a PPV of 31% and an NPV of 95%).
External validation was performed in a prospective cohort of 1583 patients admitted to both Kaohsiung CGMH and Linkou CGMH between January 2016 and June 2016. Of the 314 patients with GNB septicemia after admission within 48 hours during the study period, 61 patients were infected by IR-GNB isolates. The scoring system in predicting IR-GNB septicemia performed relatively well, with an AUC of 0.77 (95% CI, 0.71–0.83) and a sensitivity and specificity of 75% and 79%, respectively, at a cutoff point of ≥6.
Discussion
In agreement with other reports,16,17 carbapenem-resistant Gram-negative pathogens that caused nosocomial septicemia in our study were also mainly Enterobacteriaceae, and non-glucose-fermenters, that is, A. baumannii or Pseudomonas aeruginosa. In our setting, duration of exposure to carbapenems, use of mechanical ventilation, previous colonization with IR-GNB strain within 30 days before the onset of GNB septicemia, and comorbid condition with chronic kidney disease were associated with a higher risk of contracting IR-GNB septicemia during the hospitalization. In studies evaluating risk factors for carbapenem-resistant Enterobacteriaceae infection, exposure to health care and antimicrobials is among the most prominent risks. Patel et al found that invasive infections with carbapenemase-producing KPC type were independently associated with recent organ transplantation, receipt of mechanical ventilation, exposure to antimicrobials, and longer length of stay.18 We found that chronic kidney disease was more important than the overall Charlson comorbidity index in the multivariable analysis. This finding is in line with those of previous reports that the Charlson comorbidity index did not necessarily predict the risk of septicemia with multi-drug-resistant organisms after admission.19,20 Furthermore, increased severity of illness in our cohort and other study21 was not necessarily a predisposing factor of infection with antibiotic resistance organisms. A recent study conducted in ICU patients also confirmed that emergence of imipenem resistance did not obligatorily occur in the more severely ill patients.22
The increase in resistance among Gram-negative bacteria is frequently related to the high selective pressure of antimicrobials commonly used in hospitalized patients.23–25 In accordance, in the present study, prolonged duration of exposure to almost all classes of antimicrobial agents, except aminopenicillins/β-lactamase inhibitors and extended-spectrum cephalosporins, within 30 days before the onset of GNB septicemia seemed related to the emergence of imipenem resistance in the univariate analysis. However, after controlling for confounding factors and interaction, duration of exposure to carbapenems within 30 days before the onset of GNB septicemia was the independent risk factor for nosocomial IR-GNB infection. Carbapenems have been noted as a risk factor for infections with carbapenem-resistant Gram-negative isolates.25–27 None of these studies have focused on duration of exposure; therefore, data on duration of antibiotic exposure rather than only prior exposure to antibiotics as the risk factors for IR-GNB are still limited. Armand-Lefèvre et al described that the main risk factor for IR-GNB colonization in the intestine of ICU patients was prior imipenem exposure;28 the odds ratio for colonization was already as high as 5.9 after 1–3 days of exposure, which further increased to 7.8 thereafter.28 The findings indicated that imipenem use might be associated with the emergence of IR-GNB in commensal flora in a dose-dependent relationship.
Inadequate empiric antimicrobial therapy is consistently associated with increased mortality in critically ill patients mainly due to the presence of resistant organisms.29,30 Therefore, there is a critical, unmet medical need to identify, at the bedside, which patients are at the highest risk for nosocomial infection with multidrug-resistant pathogens so that initial empiric therapy can target these patients. Unfortunately, most previous studies dealing with patients with nosocomial drug-resistant GNB bacteremia were either limited by their retrospective cohort design or by focusing on specific bacteria, or some groups of patients.20,31,32 Furthermore, without aggregating these risk factors, the utility of this information at the bedside might be limited. Comprehensive decision analysis tools and scoring systems have been employed to overcome some of these issues.33 Although informative, none was able to generate a comprehensive validated scoring system for critically ill patients with preliminary blood cultures yielding GNB at sepsis onset. As application of clinical evidence varies tremendously among clinicians,34 use of our simple scoring system would help clinicians narrow the variability for decision making especially in the hospitalized patients who were critically ill. When applied to the prospective validation cohort of separate cohort of patients, our scoring system yielded AUC of 0.77 for IR-GNB septicemia. As a result, the current scoring system is able to clearly distinguish the low- from the high-risk patients for IR-GNB septicemia.
Strengths of this current study include the use of readily available bedside information to formulate the scoring system. Although this was a single-center study, further validation was done in other settings. The prospective validation of the scoring system using a separate cohort among different institutions indicated that scoring system was indeed robust in predicting a nosocomial IR-GNB septicemia. However, our study still has some limitations. First, we excluded patients who had bacteremia before or within 48 hours of admission to address our primary outcome of interest – patients who developed nosocomial infections. Second, our study is a retrospective study in derivation cohort and the relevant data have been collected from patients’ medical records. It is possible that some important confounding variables might be omitted. In addition to multivariate analysis, we used prospective external validation in other hospitals to minimize any potential confounding bias. Third, there was no routine screening performed for detection of IR-GNB during the study period. However, colonization with IR-GNB strains within 30 days before the onset of GNB septicemia was an independent risk factor for IR-GNB septicemia, probably resulting from the interplay between pathogens and the defenses of the hosts infected. Fourth, as the clonality of the isolates was not investigated, a possible cross-transmission event could not be distinguished from within-host resistance development. The genotypic or phenotypic analyses were not performed on these IR-GNB strains to understand the mechanisms of imipenem resistance due to porin loss or carbapenemases. Fifth, multiple bacteria with different virulence and susceptibility result in difficulties interpreting and possibly create methodologic flaws. However, the result might be a useful information for critically ill patients with suspected or documented GNB septicemia. Finally, we were also unable to obtain the comprehensive antibiotic history (if any) of those patients with previous stays at other hospitals.
In summary, duration of exposure to carbapenems, use of mechanical ventilation, previous colonization with IR-GNB strain within 30 days before the onset of GNB septicemia, and comorbid condition with chronic kidney disease were the factors independently related to carbapenem resistance, indicating the need for prudent and rational use of carbapenems. Our simple, prospectively validated risk stratification score for prediction of nosocomial IR-GNB septicemia may guide the clinicians to identify critically ill patients who are at risk of antibiotic-resistant GNB infections. In these circumstances, combined antibiotics may be used until antimicrobial de-escalation/adjustment is clearly indicated by the subsequently identified GNB and its susceptibility profile.
Acknowledgments
This work was supported by a grant from Chang Gung Memorial Hospital, Taiwan (CMRPG 8F1801). We would like to thank the Biostatistics Center, Kaohsiung Chang Gung Memorial Hospital for the statistics work. The authors also thanks Dr. Chien-Ching Hung at the Department of Internal Medicine, National Taiwan University Hospital, Taipei, for his critical review of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Goto M, Al-Hasan MN. Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect. 2013;19(6):501–509. | ||
Uslan DZ, Crane SJ, Steckelberg JM, et al. Age- and sex-associated trends in bloodstream infection: a population-based study in Olmsted County, Minnesota. Arch Intern Med. 2007;167(8):834–839. | ||
Peleg AY, Hooper DC. Hospital-acquired infections due to gram-negative bacteria. N Engl J Med. 2010;362(19):1804–1813. | ||
Paul M, Shani V, Muchtar E, Kariv G, Robenshtok E, Leibovici L. Systematic review and meta-analysis of the efficacy of appropriate empiric antibiotic therapy for sepsis. Antimicrob Agents Chemother. 2010;54(11):4851–4863. | ||
Munoz-Price LS, Poirel L, Bonomo RA, et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis. 2013;13(9):785–796. | ||
Averbuch D, Orasch C, Cordonnier C, et al. European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European Conference on Infections in Leukemia. Haematologica. 2013;98(12):1826–1835. | ||
Martin ET, Tansek R, Collins V, et al. The carbapenem-resistant Enterobacteriaceae score: a bedside score to rule out infection with carbapenem-resistant Enterobacteriaceae among hospitalized patients. Am J Infect Control. 2013;41(2):180–182. | ||
Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377. | ||
Chow JW, Yu VL. Combination antibiotic therapy versus monotherapy for gram-negative bacteraemia: a commentary. Int J Antimicrob Agents. 1999;11(1):7–12. | ||
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: 20th Informational Supplement, CLSI Document M100-S20. Wayne, PA: CLSI; 2010. | ||
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. | ||
Mannan HR. A practical application of a simple bootstrapping method for assessing predictors selected for epidemiologic risk models using automated variable selection. Int J Stat Appl. 2017;7(5):239–249. | ||
Sullivan LM, Massaro JM, D’Agostino RB Sr. Presentation of multivariate data for clinical use: the Framingham study risk score functions. Stat Med. 2004;23(10):1631–1660. | ||
Youden WJ. Index for rating diagnosis tests. Cancer. 1950;3(1):32–35. | ||
Lasko TA, Bhagwat JG, Zou KH, Ohno-Machado L. The use of receiver operating characteristic curves in biomedical informatics. J Biomed Inform. 2005;38(5):404–415. | ||
Clark NM, Patterson J, Lynch JP 3rd. Antimicrobial resistance among gram negative organisms in the intensive care unit. Curr Opin Crit Care. 2003;9(5):413–423. | ||
Paterson DL. Resistance in gram-negative bacteria: Enterobacteriaceae. Am J Infect Control. 2006,34(5 Suppl 1):S20–S28. | ||
Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol. 2008;29(12):1099–1106. | ||
Lye DC, Earnest A, Ling ML, et al. The impact of multidrug resistance in healthcare-associated and nosocomial Gram-negative bacteraemia on mortality and length of stay: cohort study. Clin Microbiol Infect. 2012;18(5):502–508. | ||
Korytny A, Riesenberg K, Saidel-Odes L, Schlaeffer F, Borer A. Bloodstream infections caused by multi-drug resistant Proteus mirabilis: epidemiology, risk factors and impact of multi-drug resistance. Infect Dis (Lond). 2016;48(6):428–431. | ||
Paterson DL. Looking for risk factors for the acquisition of antibiotic resistance: a 21st-century approach. Clin Infect Dis. 2002;34(12):1564–1567. | ||
Routsi C, Pratikaki M, Platsouka E, et al. Risk factors for carbapenem-resistant Gram-negative bacteremia in intensive care unit patients. Intensive Care Med. 2013;39(7):1253–1261. | ||
Friedrich LV, White RL, Bosso JA. Impact of use of multiple antimicrobials on changes in susceptibility of gram-negative aerobes. Clin Infect Dis. 1999;28(5):1017–1024. | ||
Hsueh PR, Chen WH, Luh KT. Relationships between antimicrobial use and antimicrobial resistance in Gram-negative bacteria causing nosocomial infections from 1991–2003 at a university hospital in Taiwan. Int J Antimicrob Agents. 2005;26(6):463–472. | ||
Chen IL, Lee CH, Su LH, Tang YF, Chang SJ, Liu JW. Antibiotic consumption and healthcare-associated infections caused by multidrug-resistant gram-negative bacilli at a large medical center in Taiwan from 2002 to 2009: implicating the importance of antibiotic stewardship. PLoS One. 2013;8(5):e65621. | ||
Akinci E, Colpan A, Bodur H, Balaban N, Erbay A. Risk factors for ICU-acquired imipenem-resistant Gram-negative bacterial infections. J Hosp Infect. 2005;59(4):317–323. | ||
Ong DS, Jongerden IP, Buiting AG, et al. Antibiotic exposure and resistance development in Pseudomonas aeruginosa and Enterobacter species in intensive care units. Crit Care Med. 2011;39(11):2458–2463. | ||
Armand-Lefèvre L, Angebault C, Barbier F, et al. Emergence of imipenem-resistant gram-negative bacilli in intestinal flora of intensive care patients. Antimicrob Agents Chemother. 2013;57(3):1488–1495. | ||
Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118(1):146–155. | ||
Retamar P, Portillo MM, López-Prieto MD, et al. Impact of inadequate empirical therapy on the mortality of patients with bloodstream infections: a propensity score-based analysis. Antimicrob Agents Chemother. 2012;56(1):472–478. | ||
Karaaslan A, Soysal A, Altinkanat Gelmez G, Kepenekli Kadayifci E, Söyletir G, Bakir M. Molecular characterization and risk factors for carbapenem-resistant Gram-negative bacilli colonization in children: emergence of NDM-producing Acinetobacter baumannii in a newborn intensive care unit in Turkey. J Hosp Infect. 2016;92(1):67–72. | ||
Lodise TP, Miller CD, Graves J, et al. Clinical prediction tool to identify patients with Pseudomonas aeruginosa respiratory tract infections at greatest risk for multidrug resistance. Antimicrob Agents Chemother. 2007;51(2):417–422. | ||
Vincent JL, Moreno R. Clinical review: scoring systems in the critically ill. Crit Care. 2010;14(2):207. | ||
McGinn T, Jervis R, Wisnivesky J, et al. Tips for teachers of evidence-based medicine: clinical prediction rules (CPRs) and estimating pretest probability. J Gen Intern Med. 2008;23(8):1261–1268. |
Supplementary material
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.