Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Prediction of Acute Kidney Injury in Intracerebral Hemorrhage Patients Using Machine Learning
Authors She S, Shen Y, Luo K, Zhang X, Luo C
Received 10 September 2023
Accepted for publication 30 November 2023
Published 11 December 2023 Volume 2023:19 Pages 2765—2773
DOI https://doi.org/10.2147/NDT.S439549
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Suhua She, Yulong Shen, Kun Luo, Xiaohai Zhang, Changjun Luo
The Second Department of Neurosurgery, Hunan University of Medical General Hospital, Huaihua, Hunan, People’s Republic of China
Correspondence: Changjun Luo, Email [email protected]
Background: Acute kidney injury (AKI) is prevalent in patients with intracerebral hemorrhage (ICH) and is associated with mortality. This study aimed to verify the predictive accuracy of different machine learning algorithms for AKI in patients with ICH using a large dataset.
Methods: A total of 1366 ICH patients received treatments between 2001 and 2012 from the Medical Information Mart for Intensive Care-III (MIMIC-III) database were identified based on the ICD-9 code: 431. The main outcome of AKI during hospitalizations was confirmed based on the KDIGO criteria. Overall, ICH patients were randomly divided into the training cohort and validation cohort with the ratio of 7:3. Six machine learning algorithms including extreme gradient boosting, logistic, light gradient boosting machine, random forest, adaptive boosting, support vector machine were trained in the training cohort with the 5-fold cross-validation method to predict the AKI. The predictive accuracy of those algorithms was compared by area under the receiver operating characteristics curve (AUC).
Results: A total of 1213 ICH patients were included with the incidence of AKI being 29.3%. The incidence of AKI was 29.3% among the 1213 patients with ICH. The AKI group had higher 30-day mortality (p< 0.001), longer ICU stay (p< 0.001), and longer hospital stay (p< 0.001). Among the six machine learning algorithms, the random forest performed the best in predicting AKI in both the training cohort (AUC=1.000) and the validation cohort (AUC=0.698). The top five features in the random forest algorithm-based model were platelets, serum creatinine, vancomycin, hemoglobin, and hematocrit.
Conclusion: The random forest algorithm-based predictive model we developed incorporating important features, including platelet count, serum creatinine level, vancomycin level, hemoglobin level, and hematocrit level, performed the best in predicting AKI among patients with ICH.
Keywords: Acute kidney injury, intracerebral hemorrhage, machine learning, random forest, predictive model
Introduction
As the second leading cause of death and disability worldwide, stroke is classified as ischemic and hemorrhagic type and is the leading cause of death and the second leading cause of long-term disability globally.1 Accounting for 20–30% of all stroke incidences, cerebral hemorrhage (ICH) has a 30-day mortality rate exceeding 50%.2 The high mortality associated with ICH is not solely ascribed to cerebral injury induced by intracranial hemorrhage but also to extracranial complications such as infection, stress ulcer, deep vein thrombosis, and acute kidney injury (AKI).1 Some studies have found that AKI is correlated with higher mortality and develops widely among patients with ICH, with an incidence ranging from 14.9% to 42.3%.2–6 It is necessary to assess the risk of AKI in patients with ICH as early as possible during hospitalization to avoid unnecessary nephrotoxic interventions and poor prognosis. The National Institutes of Health Stroke Scale (NIHSS) score, hypertension, baseline estimated glomerular filtration rate, serum cystatin C, and serum uric acid have been identified as risk factors for AKI among ICH patients using traditional logistic regression.2,3,6,7
The prospect of machine learning technology in medical research has gained attention and excitement because of its advantages in processing large and high-dimensional medical data. It can learn patterns that make it difficult for clinicians to accurately recognize and predict the probability of upcoming medical events, and it sometimes performs better than the traditional logistic regression in predicting clinical outcomes of various patients. While there is no study exploring the accuracy of machine learning algorithms for predicting the AKI among ICH patients. We hypothesize that machine learning algorithms-based model may perform better than the traditional logistic regression in predicting AKI among ICH patients. We design this study to evaluate the predictive value of machine learning algorithms for AKI among ICH patients using a large dataset.
Methods and Materials
Patients
This retrospective study used the Medical Information Mart for Intensive Care-III (MIMIC-III) database. As a freely public critical care database, this database contains anonymized clinical records of patients receiving treatments in the intensive care unit of the Beth Israel Deaconess Medical Center (BIDMC) (Boston, MA) between 2001 and 2012. The institutional review boards of Massachusetts Institute of Technology (MIT) and BIDMC provided ethical approval for the database. A total of 1366 ICH patients were included in this study according to the ICD-9 codes: 431 and 153 ICH patients were excluded according to the following criteria: (1) age <18 years (n=1), (2) no records of vital signs (n=71), (3) no records of laboratory test results (n=20), (4) no records of Glasgow Coma Scale (GCS) in patients (n=2), and (5) no records of continuous serum creatinine (n=59) (Figure 1). Finally, 1213 patients with ICH were included in the analysis.
 |
Figure 1 Screening flowchart of ICH patients from the MIMIC-III. Abbreviation: ICH, intracerebral hemorrhage. |
Study Variables
Data on age, sex, and comorbidities, including hypertension, diabetes mellitus, hyperlipidemia, coronary heart disease, atrial fibrillation, and chronic renal disease, were collected. Initial vital signs including systolic blood pressure, diastolic blood pressure, heart rate, body temperature, and pulse oxygen saturation (SpO2) were recorded. Disease severity was assessed by using the Glasgow Coma Scale (GCS). Laboratory tests of the first blood sample within the first day after admission were analyzed, including white blood cells, platelets, red blood cells, hemoglobin, red cell distribution width, hematocrit, glucose, serum creatinine, blood urea nitrogen, sodium, potassium, and chloride. Vancomycin and mannitol were also used in this study. The main outcome was the development of AKI during hospitalization, based on the Kidney Disease Improving KDIGO criteria. The length of ICU stay, length of hospital stay, and 30-day mortality rate were compared between the non-AKI and AKI groups.
Statistical Analysis
The Kolmogorov–Smirnov test was used to verify the normality of the variables. Non-normally distributed variables are shown as median and interquartile range and mean ± standard deviation for normally distributed variables. The Mann–Whitney U-test, Student’s t-test, and chi-square test were used to compare the differences in variables between the AKI and non-AKI groups. Statistical significance was defined as a two-sided p-value of <0.05.
Patients with ICH were randomly divided into training and validation cohorts at a ratio of 7:3. Six machine learning algorithms, including extreme gradient boosting (XGBoost), logistic, light gradient boosting machine (light GBM), random forest, adaptive boosting (AdaBoost), and support vector machine (SVM), were trained in the training cohort using the 5-fold cross-validation method to predict AKI. In the validation cohort, the predictive value of the models for AKI based on machine learning algorithms was validated by calculating seven indices: accuracy, area under the receiver operating characteristic curve (AUC), sensitivity, specificity, positive predicted value (PPV), negative predictive value (NPV), and F1 score. Feature importance in models based on machine learning algorithms was evaluated using the Shapley Additive explanation (SHAP) method. Python (Amsterdam, The Netherlands) was used for statistical analyses and graphical illustrations.
Results
Baseline Characteristics of Included ICH Patients
The incidence of AKI was 29.3% among the 1213 patients with ICH (Table 1). Compared with the non-AKI group, the AKI group had a higher percentage of male gender (p=0.021) and a higher incidence of complicated diabetes (p=0.002), atrial fibrillation (p=0.036), and chronic renal disease (p<0.001), but a lower incidence of hypertension (p=0.010). The GCS score of the AKI group was significantly lower than that of the non-AKI group (p=0.011). Regarding results of Laboratory examination showed that red cell distribution width (p<0.001), glucose (p=0.036), serum creatinine (p<0.001), and blood urea nitrogen (p<0.001) were significantly higher in the AKI group, whereas platelets (p=0.008), red blood cells (p<0.001), hemoglobin (p<0.001), and hematocrit (p<0.001) were significantly lower in the AKI group. The AKI group had higher usage incidence of vancomycin (p<0.001). Finally, the AKI group had higher 30-day mortality (p<0.001), longer ICU stay (p<0.001), and longer hospital stay (p<0.001). The comparison between ICH patients with or without CRD showed ICH patients with CRD had significantly higher level of serum creatinine and higher risk of AKI (Supplementary Table 1).
 |
Table 1 Baseline Information of ICH Patients Divided by the AKI |
Value of Machine Learning Algorithms on Predicting AKI Among ICH Patients
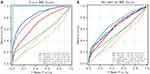
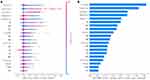
In the training cohort, the random forest performed better than the other machine learning algorithms in predicting AKI (AUC=1.000) (Table 2) (Figure 2A). In the training cohort, the XGBoost (AUC=0.846) and AdaBoost (AUC=0.810) ranked the second and the third regarding the AUC value. Furthermore, in the validation cohort, the random forest also performed the best than other machine learning algorithms on predicting AKI (AUC=0.698) (Figure 2B) and the XGBoost (AUC=0.663) and AdaBoost (AUC=0.644) still ranked the second and the third regarding the AUC value (Table 3). Regarding the feature importance evaluated using the SHAP method, platelets, serum creatinine, vancomycin, hemoglobin, and hematocrit ranked first among the random forest algorithm-based models (Figure 3A and B).
 |
Table 2 Value of Six Machine Learning Algorithms on Predicting the AKI in the Training Cohort of ICH Patients |
 |
Table 3 Value of Six Machine Learning Algorithms on Predicting the AKI in the Validation Cohort of ICH Patients |
Discussion
The incidence of AKI in patients with ICH was 29.3%, which was consistent with a previously reported incidence ranging from 14.9% to 42.3%.2–6 The difference in AKI incidence among ICH patients may be attributable to differences in comorbidities, hemorrhage volume, medical interventions, and medical level. Our analysis indicated that the random forest algorithm-based model performed best in predicting AKI in patients with ICH. Due to the high incidence and adverse outcomes of AKI among ICH patients, evaluating the risk of AKI as early as possible after admission may inform clinicians to avoid unnecessary nephrotoxic interventions and, therefore, improve the prognosis of ICH. Considering the feature importance in our developed random forest algorithm-based model, the top five features were platelets, serum creatinine, vancomycin, hemoglobin, and hematocrit. Platelet, hemoglobin, and hematocrit levels showed negative effects on AKI, whereas serum creatinine and vancomycin levels showed positive effects on AKI.
Some studies have found the nadir value of platelet during hospitalizations was positively associated with the risk of AKI.8,9 Platelets have attracted much attention because of their important role in ischemia and inflammatory injury of the end organs by stimulating endothelial responses and recruiting neutrophils.10–12 Aggregated platelets accompanied by activated leukocytes and fibrin promote microthrombus formation in renal microvessels.13 Consequently, platelet aggregation and microthrombi may obstruct renal vessels and glomeruli, causing renal ischemia and injury.
As a major component of red blood cells, hemoglobin is responsible for the transportation of oxygen from the lungs to tissues and organs. Previous studies have found that decreasing hemoglobin levels are associated with the development of AKI in various patients, including neonates and those undergoing cardiac surgery or percutaneous coronary intervention.14–16 Decreased hemoglobin levels in patients with ICH may be caused by intracranial bleeding, malnutrition, and pathophysiological consumption. Consequently, inadequate hemoglobin cannot provide sufficient oxygen to the renal tissue, leading to subsequent renal injury. Reflecting the ratio of red blood cells to plasma, hematocrit is the main factor affecting blood viscosity and is influenced by the volume of red blood cells and plasma. Decreased hematocrit can be caused by multiple factors, including bleeding, shock, burns, electrolyte disorders, liver cirrhosis, and malnutrition. The negative association between Hct and AKI after ICH may also reflect the harmful effect of insufficient oxygen release to the renal tissue caused by low levels of red blood cells.
Drug-induced nephrotoxicity plays a crucial role in the development of AKI. The vancomycin was widely used among included ICH patients with the incidence of 33.3%. The AKI group had higher incidence of vancomycin use than the non-AKI group (48.6% vs 27.0%). As a broad-spectrum antibiotic widely used to treat infections, particularly methicillin-resistant Staphylococcus aureus, vancomycin has raised concerns regarding its potential renal toxicity.17,18 The relationship between vancomycin use and AKI has been confirmed, particularly in patients receiving a higher dose or prolonged duration of vancomycin use.19
The comparison between ICH patients with or without chronic renal disease showed ICH patients with chronic renal disease had higher level of serum creatinine and risk of AKI than those without, which indicated that the importance of initial serum creatinine level on the risk of AKI might partially be mediated by the history of chronic renal disease. The previous chronic renal disease may predispose ICH patients to impaired renal function reflected by higher initial serum creatinine level. Certainly, the higher initial serum creatinine level may not only be attributable to the history of chronic renal disease but also other acute pathophysiological changes after ICH. Overall, the mechanism behind the AKI after ICH may be multiple including both intrinsic pathophysiological changes of extracranial systems after ICH, iatrogenic interventions, and previous history of impaired renal function. The platelet aggregation and microthrombus, insufficient oxygen release reflected by the low level of hemoglobin and hematocrit may reflect the intrinsic pathophysiological changes of extracranial systems after ICH and therefore cause the development of AKI. Monitoring these hematological indices and evaluating the risk of AKI using the random forest algorithm-based model could help clinicians to reduce the risk of AKI in ICH patients and therefore improve the prognosis of ICH. Meanwhile, the effect of rectifying these hematological indices on AKI development and prognosis of ICH should be further verified.
Our study had several limitations. First, this study was conducted using retrospective data from the MIMIC III database derived from a single medical center. Selection bias is inevitable. Therefore, the generalizability of our developed model should be externally verified in other medical centers. Second, some variables were not included in this study, including hematoma volume and hemorrhage location, owing to the limited medical records of MIMIC III. Future studies can improve the performance of our model by incorporating other important features. Third, although the SHAP method has been used to visually illustrate the relative importance of features, a web- or portable electronic equipment-based user-friendly program integrating our developed predictive model should be designed and produced to improve the chances of early detection of the risk of AKI in ICH patients.
Conclusion
The random forest algorithm-based predictive model we developed performs well in predicting AKI in patients with ICH.
Some important predictive features of AKI in ICH have been identified, including platelet count and serum creatinine, vancomycin, hemoglobin, and hematocrit levels. The predictive model incorporating these features is helpful for early detection of the risk of AKI in ICH patients. Future studies could be performed to improve the performance of our developed model by incorporating other important ICH related features.
Institutional Review Board Statement
Data for this study was collected from the MIMIC-III database designed and produced by the Beth Israel Deaconess Medical Center (BIDMC). This database was approved by the institutional review boards of Massachusetts Institute of Technology and BIDMC. All patients included in this public database were anonymized and de-identified for protecting individual privacy. This study was conducted accorded with the ethical standards of the Helsinki declaration.
Data Sharing Statement
The datasets used for the current study are available from the corresponding author on reasonable request.
Informed Consent Statement
Patient consent was waived because this is a retrospective study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol. 2009;8(4):345–354. doi:10.1016/S1474-4422(09)70023-7
2. Ansaritoroghi M, Nagaraju SP, Nair RP, et al. Study on acute kidney injury in patients with spontaneous intracerebral hemorrhage: an overview from a Tertiary Care Hospital in South India. World Neurosurg. 2019;123:e740–e6. doi:10.1016/j.wneu.2018.12.018
3. Jiang F, Su L, Xiang H, et al. Incidence, risk factors, and biomarkers predicting ischemic or hemorrhagic stroke associated acute kidney injury and outcome: a retrospective study in a general intensive care unit. Blood Purif. 2019;47(4):317–326. doi:10.1159/000499029
4. Qureshi AI, Huang W, Lobanova I, et al. Systolic blood pressure reduction and acute kidney injury in intracerebral hemorrhage. Stroke. 2020;51(10):3030–3038. doi:10.1161/STROKEAHA.120.030272
5. Khatri M, Himmelfarb J, Adams D, Becker K, Longstreth WT, Tirschwell DL. Acute kidney injury is associated with increased hospital mortality after stroke. J Stroke Cerebrovascul Dis. 2014;23(1):25–30. doi:10.1016/j.jstrokecerebrovasdis.2012.06.005
6. Wang Q, Li S, Sun M, Ma J, Sun J, Fan M. Systemic immune-inflammation index may predict the acute kidney injury and prognosis in patients with spontaneous cerebral hemorrhage undergoing craniotomy: a single-center retrospective study. BMC Nephrol. 2023;24(1):73. doi:10.1186/s12882-023-03124-2
7. Huang Y, Wan C, Wu G. Acute kidney injury after a stroke: a PRISMA-compliant meta-analysis. Brain Behav. 2020;10(9):e01722. doi:10.1002/brb3.1722
8. Wu M, Luan YY, Lu JF, et al. Platelet count as a new biomarker for acute kidney injury induced by hemorrhagic shock. Platelets. 2020;31(1):94–102. doi:10.1080/09537104.2019.1581921
9. Kertai MD, Zhou S, Karhausen JA, et al. Platelet counts, acute kidney injury, and mortality after coronary artery bypass grafting surgery. Anesthesiology. 2016;124(2):339–352. doi:10.1097/ALN.0000000000000959
10. Lapchak PH, Kannan L, Ioannou A, et al. Platelets orchestrate remote tissue damage after mesenteric ischemia-reperfusion. Am J Physiol Gastrointest Liver Physiol. 2012;302(8):G888–97. doi:10.1152/ajpgi.00499.2011
11. Kornerup KN, Salmon GP, Pitchford SC, Liu WL, Page CP. Circulating platelet-neutrophil complexes are important for subsequent neutrophil activation and migration. J Appl Physiol. 2010;109(3):758–767. doi:10.1152/japplphysiol.01086.2009
12. Li Z, Yang F, Dunn S, Gross AK, Smyth SS. Platelets as immune mediators: their role in host defense responses and sepsis. Thromb Res. 2011;127(3):184–188. doi:10.1016/j.thromres.2010.10.010
13. Devarajan P. Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol. 2006;17(6):1503–1520. doi:10.1681/ASN.2006010017
14. Balci C, Haftaci E, Kunt AT. Use of cerebral oxygen saturation and hemoglobin concentration to predict acute kidney injury after cardiac surgery. J Int Med Res. 2018;46(3):1130–1137. doi:10.1177/0300060517741064
15. Nada A, Askenazi D, Boohaker LJ, et al. Low hemoglobin levels are independently associated with neonatal acute kidney injury: a report from the AWAKEN Study Group. Pediatr Res. 2021;89(4):922–931. doi:10.1038/s41390-020-0963-x
16. Kuno T, Numasawa Y, Mikami T, et al. Association of decreasing hemoglobin levels with the incidence of acute kidney injury after percutaneous coronary intervention: a prospective multi-center study. Heart Vessels. 2021;36(3):330–336. doi:10.1007/s00380-020-01706-w
17. Altowayan WM, Mobark MA, Alduhami AA, Rabbani SI, Rabbani SI. The influence of vancomycin on renal functions, the predictors and associated factors for nephrotoxicity. PLoS One. 2023;18(4):e0284223. doi:10.1371/journal.pone.0284223
18. Yin X, Yang Q, Li H, Kang Y, Li Z. Vancomycin induced ferroptosis in renal injury through the inactivation of recombinant glutathione peroxidase 4 and the accumulation of peroxides. Drug Des Devel Ther. 2023;17:283–295. doi:10.2147/DDDT.S392813
19. Tsutsuura M, Moriyama H, Kojima N, et al. The monitoring of vancomycin: a systematic review and meta-analyses of area under the concentration-time curve-guided dosing and trough-guided dosing. BMC Infect Dis. 2021;21(1):153. doi:10.1186/s12879-021-05858-6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.