Back to Journals » Adolescent Health, Medicine and Therapeutics » Volume 8
Predicting the occurrence of headache and back pain in young adults by biopsychological characteristics assessed at childhood or adolescence
Authors Kröner-Herwig B, Gorbunova A , Maas J
Received 12 November 2016
Accepted for publication 14 February 2017
Published 28 March 2017 Volume 2017:8 Pages 31—39
DOI https://doi.org/10.2147/AHMT.S127501
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Alastair Sutcliffe
Birgit Kröner-Herwig, Anastasia Gorbunova, Jennifer Maas
Department of Clinical Psychology and Psychotherapy, Georg-Elias-Müller-Institute of Psychology, University of Göttingen, Göttingen, Germany
Abstract: The aim of the current study was to identify predictors of recurrent headache and back pain in young adults (aged 18–27 years) from data assessed in childhood or adolescence, i.e., 9 years before the final survey. Our interest was whether psychological characteristics contribute to the risk of pain prevalence in adult age when controlling for already empirically supported risk factors such as parental pain, pediatric pain and sex. The study was part of a five-wave epidemiological investigation of >5000 families with children aged between 7 and 14 years when addressed first. In a multiple hierarchical regression analysis, the abovementioned three variables (Block-I variables) were entered first followed by five psychological trait variables (Block-II variables: internalizing, anxiety sensitivity, somatosensory amplification, catastrophizing and dysfunctional stress coping) to find out the extent of model improvement. The multivariable hierarchical regression analysis confirmed the hypothesis that the Block-I variables significantly enhance the risk of future pain at young adult age. None of the psychological variables did so. Thus, the hypothesis of a significant surplus predictive effect was not confirmed. The amount of total explained variance differed strongly between headache and back pain. In particular, a valid prediction of back pain was not possible. When analyzed separately in simple regression analysis, psychological variables turned out to be significant predictors, however, of very low effect size. The inclusion of Block-I variables in the model clearly reduced the impact of the psychological variables. This risk profile is discussed in the context of the different trajectories of headache and back pain from childhood to adult age, which were proposed by various studies. We propose that a biopsychological characteristic denoted as emotional negativity, especially regarding self-reference, might be a common factor behind all selected variables. Risk research in recurrent pain is a field where much more multidisciplinary research is needed before progress can be expected.
Keywords: headache, back pain, prediction of adult pain, risk factors, biopsychological interaction
Introduction and objective
The current study aimed at a long-term prospective analysis regarding to what extent psychological factors in childhood and adolescence increase the predictability of headache and back pain at young adult age.
The prospective design based on data from an earlier large population study on pain in youths carried out by our research team focused on psychological factors associated with pediatric pain.1 Headache has been a target of research in children and adolescents for many years, whereas pediatric back pain had not been given too much attention.2–9 Many studies identified the association of headache with various psychosocial characteristics.10–14 In addition, our recent research on the population sample showed more or less close linkages with psychosocial factors such as quality of family interaction, school stress and certain psychological characteristics of children with headache of every type. These studies consisted of cross-sectional analyses or longitudinal designs with short intervals.1,15–17
The following constructs operationalized and mostly assessed by psychometric tests seemed to be promising regarding our main issue to examine the prospective potential of psychological factors regarding the occurrence of pain in adult age.
Of special interest was the role of internalizing, a trait defined by symptoms of depression and anxiety.14,18 It is already identifiable in early childhood and seems to be rather stable. The review of Balottin et al19 underlined its importance, as did our data from earlier studies. An association of internalizing with headache, in particular with migraine and also tension-type headache (TTH), was found to show a higher level of internalizing in headache-afflicted youngsters.16 This finding can be integrated into the Common-Path Model of Kato et al,20 assuming negative affectivity and hypersensitivity regarding the central processing of internal and external stimuli as common paths both to recurrent or chronic pain and to psychological disorders such as depression and anxiety.21
The heightened level of anxiety sensitivity and somatosensory amplification, found in headache-afflicted children and adolescents, can be interpreted as indicators of the second path (hypersensitivity) assumed in the model of Kato et al. So far, no study has examined whether these traits offer a contribution to the prediction of the occurrence of headache and back pain at adult age.20
Anxiety sensitivity defined as a disposition to feel threatened by physiological symptoms of arousal and anxiety seems to be heightened in children with headache and other recurrent pains.17,22–26 There is also evidence that it predicts anxiety disorders and other Axis I disorders classified by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) in later life.27
Although research on somatosensory amplification, a tendency to focus on and emphasize physical sensations, is still rare, a few studies, beside ours, found an association of this kind of processing of somatic stimuli with recurrent pain.28–30
The analysis of another psychological variable, i.e., dysfunctional stress coping, promised to offer further knowledge regarding the association of stress processing and pain.17,31,32 According to Lazarus and Folkman,33 the failure to adequately cope with problems either by cognitive reappraisal or by tackling the problem situation itself will maintain the state of stress in the individual and is assumed to contribute to pain and psychological dysfunctions.
A catastrophizing manner of pain processing, a well-researched strategy of evaluating and coping with pain, is long known to influence pain experience.17,24,31,34
Studies by Tsao et al,26 Vervoort et al35 and Kröner-Herwig and Maas36 showed that catastrophizing, i.e., magnifying negative sensory stimulation, ruminating about it and feeling helpless, goes along with higher intensity and frequency of pain and the associated disability. Thus, we expected the abovementioned variable to contribute to the prediction of pain, in particular headache, in young adults.
Less evidence on psychosocial associations exists concerning back pain in children and adolescents. Some findings, however, gave evidence of a linkage.17,31,37–39
The conduction of the current survey enabled us to examine whether the psychological variables introduced earlier, assessed in children and adolescents 9 years before the follow-up study, contribute to the prediction of headache and back pain at young adult age. Furthermore, we wanted to examine potential differences between these types of pain in this respect.
It was our intention to compare the predictive value of psychological variables in relation to variables with a proposed closer involvement of biological mechanisms. These variables were early pain vulnerability indicated by pain symptoms in childhood or adolescence (baseline period of this study) and the occurrence of parental pain with genetic and possibly also social modeling influence.40 In addition, sex was included as a control variable, since it is one of the most stable differential factors in pain with a stronger disposition to pain in females.41
The psychological variables taken together were assumed to contribute to the prediction of headache and back pain and increase the amount of explained variance. Hence, a hierarchical logistic regression procedure was planned, where the predictive power of the above delineated control variables in the model was assessed first (Block-I variables). In the second step, the psychological variables (Block-II variables) were included to determine their surplus prognostic effect. Based on simple logistic regression models, we assumed significant associations with pain regarding each control variable and also each psychological factor. Furthermore, we expected the total amount of variance explained to be higher in headache than back pain, especially regarding the psychological variables.
Methods
Design and sample
Beginning in the year 2003, four annual postal surveys (S1–S4) on pediatric pain were carried out in southern Lower Saxony (Germany).1 The fifth survey (S5) was accomplished in 2015, i.e., 9 years later. The first survey (S1) was carried out comprising 8800 families with at least one child in the age of 7–14 years, who were randomly drawn from community registries. Hence, participants of S5 were in the age of 19–27 years.
A number of 5542 families, who constituted the responder sample in S1 (2003), were contacted in S4 (2006) and then in S5 (2015). The former postal addresses of the families were used. A large dropout rate was expected in S5 9 years after the last contact with the families as the probability of the families having moved to another place, the young adults having left their family home while going to college/university, having started a traineeship at another place and having set up a household of their own was rather high. All nonresponding families were then informed about the possibility to engage in an online survey, asking them to inform their child who had participated in the earlier surveys.
Only 215 former participants chose this mode of enrollment. A high dropout rate of 66% was observed in S5. The total number of cases was further reduced by participants with missing data (>50%) regarding the complete questionnaire with ~18 pages. In addition, contradicting information on the identity of the responder led to a reduction of cases prone for statistical analysis to n=1522. The sample had an age range of 19–27 years with an average M=22.4 years (standard deviation [SD]=2.36 years). Only 43.5% of the participants were males. The dominance of female participants was caused by a larger dropout rate of males, particularly in S5.
The question posed regarding the occurrence of headache was answered by 1506 subjects (Ss) and 1488 responded regarding back pain. The participants were asked whether they had ever experienced headache in the last 6 months. If the answer was yes, they were questioned further whether their headache was always associated with an illness or also evolved at other times. All participants who agreed to the first response alternative were excluded from the data pool for analysis. This coding was chosen in order to exclude cases of the so-called secondary pain caused by medical conditions (such as a cold), especially regarding headache.
The above mentioned questions asking for the frequency of headache presented the following possible responses: at least once a week/at least once a month but less than once a week/less than once a month. The response “headache at least once per month” during the period of the last 6 months was coded as “headache”. Hence, the answers “never” or “less than once per month” were coded as “no headache”.
The same procedure was used when classifying back pain: the answers to the question asking for the presence of back pain in the last 6 months “never” or “rarely” led to a coding of “no back pain”. The responses “several times” and “all the time” led to the coding of the presence of back pain. The different response term was chosen because of the different time characteristics: headache usually is an episodic event of several hours, whereas back pain is a more continuing form of pain mostly over several days and usually being modified by posture.
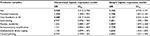
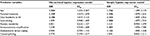
In S5, headache was found in 51% (n=768) of the participants and back pain in 43.3% (n=644) of the participants (Tables 1 and 2). An evaluation of disability due to the different pains was also examined, but was not part of the definition of the presence of pain in S5.
  | Table 1 Descriptive statistics for headache classes Abbreviations: M, mean; SD, standard deviation; S4, fourth survey. |
  | Table 2 Descriptive statistics for back pain classes Abbreviations: M, mean; SD, standard deviation; S4, fourth survey. |
Ethics
The German Association of Psychology approved the study, including surveys 1–4, and the Ethic Committee of the Institute of Psychology of the University of Göttingen did so for survey 5. Informed consent was provided by all participants. The parents or guardians of the children in the earlier surveys provided informed consent on their behalf.
Control and predictor variables
The procedural definition of the dichotomous criterion headache (yes/no) and back pain (yes/no) in S5 was just given. The pain variables in S4 used as control and parental pain (self-report) were assessed in the same way. In 88.5% of the cases, the biological mother gave response. Sex of the participant was the third control variable. Further, in the text, these variables are denoted as Block-I predictors.
The Block-II predictors, i.e., the psychological variables, included internalizing, anxiety sensitivity, somatosensory amplification, dysfunctional stress coping and catastrophizing. The complete psychometrically validated test instruments could not be applied in S4 in most cases because of the multitude of variables assessed in the questionnaire. To safeguard the participants against excessive strains and to maintain their motivation, a limited number of items were selected from the instrument. The selection was based on high item-scale correlations or high factor loadings of the chosen items. A minimum of 50% of these items had to be responded to; otherwise, the scale score was rated as missing. All items were coded in the same way (1–5): the total score of all scale items was devided by the number of items. The highest value corresponds to the highest frequency or intensity of the symptom (see examples in the following and Tables 1 and 2, descriptive data).
Internalizing was measured by selected items from the Youth Self-Report originally validated for youths between 11 and 18 years.42 The internalizing scale comprised eight items (e.g., “I felt guilty”). Contrary to the original form of a 3-point rating scale, responses were scaled on a 5-point scale (never–always) to ensure comparability with other scales and higher grade of differentiation.
Anxiety sensitivity was assessed using five items of the Anxiety Sensitivity Inventory (ASI) by Blais et al.43 Items (e.g., “I am frightened when my heart beats fast”) were rated on a 5-point scale (never–very much).
Somatosensory amplification comprised five items (e.g., “I am very sensitive to pain”) and was also assessed with a 5-point scale (never–very much).
Dysfunctional coping was assessed with five items of the Stress Coping Questionnaire for Children and Adolescents by Hampel et al44), which were rated on a 5-point scale (never–always; e.g., “When I am put under pressure by my mates or at school, I pretend that I am ill”). Catastrophizing was assessed with the German Pain Catastrophizing Scale for Children (PCS-C).36 The scale consists of 13 items (e.g., “When I am in pain … It is awful and I feel it overwhelms me”). Responses to the statements denote the degree of agreement on a 5-point scale (never [1]–very much [5]).
All psychological scales had moderate to high internal consistency with Cronbach’s alpha between 0.71 (somatosensory amplification) and 0.89 (catastrophizing). Items with an item-scale correlation >0.4 were included to calculate the mean scale score for each psychological scale.45
Statistics
A hierarchical logistic regression analysis was performed on headache and back pain entering the three control or Block-I variables first in one block; all five psychological variables were entered in the second step, also as a block.
The “no headache” and “no back pain” categories served as reference. This procedure allowed us to test the main hypothesis on the surplus effect of the Block-II variables on the explanation of variance in pain.
To evaluate the goodness-of-fit R2 respectively changes in R2 of the total model compared to baseline was used, as well the change in correctly predicted cases.
To test for multicollinearity among predictors, the variance inflation factor (VIF) and tolerance were determined. As suggested by Bowerman and O’Connell,46 R2 average VIF substantially >1 is an indicator for potential bias in the regression estimation. According to Menard,47 tolerance <0.20 indicates potential bias estimation as well. The predictors in the model for headache had an average VIF of 1.61, and all tolerances were >0.40. Similar results were obtained for back pain model with an average VIF of 1.59 and lowest tolerance of 0.42. Linearity assumption of the logit was also met. All analyses were performed with SPSS 23.0.
Results
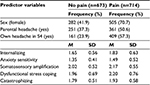
Headache
The hierarchical logistic regression analysis was carried out on 1387 complete cases. The regression model resulted in 23.5% variance in headache prevalence explained by the Block-I variables (Table 3). Headache presented in S4 was the strongest predictor of headache in S5 with an odds ratio (OR) of 3.61 followed by sex (OR=2.95) and parental headache (OR=1.52). Psychological predictors in Block-II variables added only 0.4% to the explained variance; none of these presented itself as a significant predictor of headache in S5. In total, 68.6% of the cases were correctly categorized in comparison to 51.5% in the baseline model. In all, 70.7% cases of headache were correctly predicted. The goodness-of-fit statistics showed an increase in correct classification by 17.1% (Table 4).
  | Table 4 Goodness-of-fit statistics for the regression models Note: aModel without predictors. |
Preliminary to the testing of the main hypothesis by hierarchical regression, every single psychological predictor was tested in a simple regression analysis with controlling for multiple testing. All psychological variables turned out to be significant though with a small effect size with ORs between 1.60 and 1.87 (Table 3).
The set of five psychological variables by itself explained only 5.1% of the variance in headache in S5. When controlling for a Block-I variable from S4 (e.g., childhood pain), each psychological predictor was reduced to a nonsignificant size with the exception of coping style, which remained significant (OR=1.22, p=0.017).
When controlling for a Block-I variable from S4 (e.g., childhood pain), each psychological predictor was reduced to a nonsignificant size with the exception of coping style, which remained significant (OR=1.22, p=0.017). Within the simple logistic regression model, all three Block-I variables achieved highly significant scores (Table 3).
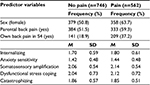
Back pain
Of the 1488 participants who responded to the back pain item, 43.3% gave an affirmative response (Table 2). Because of various missings, only 1308 cases were retained in regression analysis. Block-I variables explained 7.4% of variance in the criterion and Block-II variables an additional 0.9%. All Block-I variables were significantly associated with back pain in S5. Back pain in S4 was the strongest predictor with an OR of 2.40, followed by sex (OR=1.58) and parental back pain (OR=1.33; Table 5). The goodness-of-fit statistic shows an increase of 6% of correctly classified cases (Table 4).
When examining the psychological variables in simple regression analyses, three of five variables could significantly predict back pain in S5: internalizing, somatosensory amplification and dysfunctional coping with small ORs from 1.15 to 1.30. All turned to insignificance when Block-I variables were entered into the analysis. The percentage of correct predictions was 63.0% with “no back pain” being correctly predicted in 82.8% of the cases.
Discussion
Hierarchical regression model: headache and back pain
The results of regression analysis confirmed the hypothesis that all Block-I variables assessed in S4 are significant predictors of headache and back pain in S5, i.e., 9 years later, with the Ss being 19–27 years old. Our main hypothesis assumed that the selected psychological variables should lead to a distinct improvement in the prognosis of pain, in particular headache has to be rejected when the results of the hierarchical logistic regression with Block-I and Block-II variables are taken into account.
When entered block-wise in the model, psychological variables did not reach significance in either headache or back pain. In headache, a gain of only 0.4% of the explained variance above the control variables was achieved, and in back pain, 0.9% was achieved. The amount of explained variance by Block-I variables contrasts these results, with 23.5% explained variance in headache and 7.4% in back pain.
The expectation of a higher precision of the headache model compared to back pain was confirmed. However, it was not dependent on the psychological variables, but on Block-I predictors.
A total prediction rate of 68.4% regarding headache was achieved, with similar rates for the prediction of headache cases (70.7%) vs 66.3% of cases without headache. Back pain prediction rates were lower (total 61.8%), clearly favoring the accurate identification of no back pain (82.2%) by the model.
Thus, the Block-I variables assumedly linked to basic biopsychological mechanisms explain much more variance in headache than in back pain. When entering only the psychological variables into the regression analysis, 5.1% of variance is explained in headache and only 1.6% in back pain.
It has, however, to be underlined that also regarding headache, there remains a remarkably large explanatory gap in our total prediction model. It seems not pushed too hard to assert that information from childhood/adolescence, at least the one used here, cannot validly predict back pain in young adults. According to our knowledge, there are no further longitudinal studies focusing on the prognosis of pain in adult age, making use of multiple predictors from childhood/adolescence as we did.
Psychological variables: under a magnifying lens
At first sight, the results in particular regarding the psychological variables were somehow conflicting with the findings from earlier studies that often reported significant associations with psychological variables at least in cross-sectional analyses.19,21 We wanted therefore to dive deeper into the data that built the basis of the current findings, since the complexity of interrelations between variables and its consequences on the outcome when multiple regression analysis is performed is well known.
Therefore, simple regression models were calculated showing that each of the psychological variables significantly predicted headache in S5 (p<0.001) with ORs between 1.60 and 1.87. This was also the case in back pain with the exception of anxiety sensitivity and catastrophizing (range of significant ORs: 1.15–1.30). The significance of results cannot hide the fact that ORs are of low size and thus of limited relevance.
Further explorative analysis revealed that controlling for Block-I variables makes the influence of almost each psychological variable on outcome insignificant. We also found substantial correlations between psychological variables (0.38≤r≤0.71). A factor analysis revealed an appropriate one-factor solution with 59% of variance explained. These findings document that the psychological variables assess to a certain extent a common feature (e.g., represented as depressive mood and feelings of anxiousness in internalizing or helplessness and an extremely negative emotional response to bodily responses as in catastrophizing and somatosensory amplification), best described as a habitual emotional negativity in self-reference.
In summary, the discussed findings underline again that cross-sectional studies assessing bivariate correlations cannot substitute prospective research. Furthermore, they document that the accumulation of presumably independent potential risk factors in the regression model does not guaranty a better solution.
Block-I variables: under a magnifying lens
Pain in childhood/adolescence be it headache or back pain occurring monthly or weekly within the 6-month period before the assessment in S4 proved to be the strongest predictor of pain. People with pediatric headache are 3.6 times more likely to have headache in an early adult age as ones without pediatric headache. The same tendency was detected in back pain with a 2.4 times higher risk of having back pain in S5 by people with pediatric back pain. This confirms the findings of a number of studies showing that early pains indicate a dispositional pain vulnerability.48 The interpretation that this disposition is stronger in headache and may be earlier expressed is in concordance with data documenting that headache develops at a lower age in childhood than back pain and has a higher prevalence already during childhood/adolescence in contrary to low back pain.49 With some caution, the phenomenon that early biopsychological characteristics affected by genetic or gene/environment interactions play a smaller role in back pain or at least become effective later could be interpreted.
Although the occurrence of parental pain is a significant predictor for headache and back pain, the risk was not dramatically increased according to our results (headache: OR=1.53 and back pain: OR=1.33). This disagrees to a certain extent with a finding from another analysis on headache in our pediatric population where a more complex measure of parental headache was used differing between types of headache and assessing both parents.16 The highest OR of 6.53 was found for pediatric migraine when at least one of the parents had migraine and TTH.
In summary, results on parental influence on headache and back pain, including genetic and social modeling mechanisms, are not uniform and less consistent than originally proposed: the data of Messinger et al50 and Laurell et al51 mirror our results for headache in the current study. In addition, a significant but not really large OR (2.07) was seen by Szpalski et al37 regarding parental back pain and back pain in children. In contrast, Borge and Nordhagen52 as well as Jones et al53 did not report a higher risk of back pain when parental pain was present.
As expected, sex reliably differentiated the risk of pain in early adulthood. In headache, we found approximately threefold higher risk for women. The effect was less strong in back pain, indicating that there was less difference between males and females. Not knowing what factors mediate the sex effect, being biological or/and psychological, these factors seem to be less influential in back pain. Thus, the plausibility of the conclusion that the occurrence of back pain is determined by a multitude of different factors accumulating their effects over a longer period of time compared to headache is at least plausible. In summary, the important role of sex for pain was again confirmed by the current study.54
Limitations
Our main outcome variables headache and back pain were rather roughly defined, not including specifying features such as frequency, intensity or duration of pain. In addition, the important aspect of disability was not considered.
The psychological variables were not measured by validated complete psychometric instruments and allowed no estimation of standard scores based on a normative sample. However, the internal consistency of the scales used was at least satisfying and the correlation between the complete and the shortened formats of the questionnaires was high.15
In the regression analysis, a sample with an age range covering a maximum of 7 years was used, which could have “blurred” our results as the interaction of biopsychological factors could be different at different developmental periods.
Conclusion
The prognostic value of three variables, i.e., pain in childhood/adolescence, parental pain and sex, thought to involve to certain extent biological mechanisms was rather low and clearly lower in back pain than in headache. Notwithstanding statistical significance, predictions were correct in only 68.6% or 63.0% of cases when trying to differentiate pain-free Ss from the pain afflicted in young adulthood, respectively. Block-I variables had clearly more explanatory power on pain outcomes, resulting in statistical insignificance of psychological variables when used as controls. This leads us to the – rather speculative – assumption that our Block-I variables, in spite of their seemingly different character istics, contain components of the common constituent of the psychological variables, speculatively named emotional negativity in self-reference.
The difference in the prediction of headache and back pain could be a result of the differences in the trajectories: headache is the pain that sets in earlier childhood and reaches an early peak in adolescence and adulthood.55 Thus, biological and psychological dispositions could have an earlier and more lasting influence on headache, whereas back pain could be shaped by an individually diverse and variable multitude of factors over time.
The general conclusion is that in headache and especially in back pain, the examined models on the prediction of prevalence of pain in young adult age by biopsychological childhood parameters are far from being perfect. Literature search for potential risk factors in our study did not comprise, resulted in the factors smoking and especially body mass index. However, these risk factors were mainly found in adults and not in children and did not reveal a large effect size. Szpalski et al37 arrived at a similar evaluation in particular for back pain: “… out of the very extensive list of investigated variables only a limited number showed a relation with the persistence or occurrence of LBP in children”.
Hence, the research on the prognosis of recurrent pain in adult age from childhood and familial data is at best at a rather immature stage. More intensive and coordinated interdisciplinary cooperation is in need to achieve progress.
Acknowledgments
We thank Corinna Isensee, Carolin Fernandez-Castelao and Cynthia Bengs who have made significant contributions to the conception and design of wave 5 of the project. They supported us in the assessment of data and the management of documentation, which has made this article possible. Four assessment waves of the total project were supported by funds of the German Ministry of Education and Research as part of the German Headache Consortium.
Disclosure
The authors report no conflicts of interest in this work.
References
Kröner-Herwig B, Heinrich M, Morris L. Headache in German children and adolescents: a population-based epidemiological study. Cephalalgia. 2007;27(6):519–527. | ||
Rhee H. Prevalence and predictors of headaches in US adolescents. Headache J Head Face Pain. 2000;40(7):528–538. | ||
Fearon P, Hotopf M. Relation between headache in childhood and physical and psychiatric symptoms in adulthood: national birth cohort study. BMJ. 2001;322(7295):1145. | ||
Powers SW, Patton SR, Hommel KA, Hershey AD. Quality of life in childhood migraines: clinical impact and comparison to other chronic illnesses. Pediatrics. 2003;112(1 pt 1):e1–e5. | ||
Ghandour RM, Overpeck MD, Huang ZJ, Kogan MD, Scheidt PC. Headache, stomachache, backache, and morning fatigue among adolescent girls in the United States: associations with behavioral, sociodemographic, and environmental factors. Arch Pediatr Adolesc Med. 2004;158(8):797–803. | ||
Laurell K, Larsson B, Eeg-Olofsson O. Prevalence of headache in Swedish schoolchildren, with a focus on tension-type headache. Cephalalgia. 2004;24(5):380–388. | ||
Zwart JA, Dyb G, Holmen T, Stovner L, Sand T. The prevalence of migraine and tension-type headaches among adolescents in Norway. The Nord-Trøndelag Health Study (Head-HUNT-Youth), a large population-based epidemiological study. Cephalalgia. 2004;24(5):373–379. | ||
Balottin U, Termine C, Nicoli F, Quadrelli M, Ferrari-Ginevra O, Lanzi G. Idiopathic headache in children under six years of age: a follow-up study. Headache J Head Face Pain. 2005;45(6):705–715. | ||
Huguet A, Miró J. The severity of chronic pediatric pain: an epidemiological study. J Pain. 2008;9(3):226–236. | ||
Karwautz A, Wöber C, Lang T, et al. Psychosocial factors in children and adolescents with migraine and tension-type headache: a controlled study and review of the literature. Cephalalgia. 1999;19(1):32–43. | ||
Larsson B, Sund AM. Emotional/behavioural, social correlates and one-year predictors of frequent pains among early adolescents: influences of pain characteristics. Eur J Pain. 2007;11(1):57–57. | ||
Kaasbøll J, Lydersen S, Indredavik MS. Psychological symptoms in children of parents with chronic pain—the HUNT study. Pain. 2012;153(5):1054–1062. | ||
Wilner JG, Vranceanu A-M, Blashill AJ. Neuroticism prospectively predicts pain among adolescents: results from a nationally representative sample. J Psychosom Res. 2014;77(6):474–476. | ||
Blaauw BA, Dyb G, Hagen K, et al. The relationship of anxiety, depression and behavioral problems with recurrent headache in late adolescence – a Young-HUNT follow-up study. J Headache Pain. 2015;16(1):10. | ||
Kröner-Herwig B, Morris L, Heinrich M. Biopsychosocial correlates of headache: what predicts pediatric headache occurrence? Headache J Head Face Pain. 2008;48(4):529–544. | ||
Kröner-Herwig B, Gassmann J. Headache disorders in children and adolescents: their association with psychological, behavioral, and socio-environmental factors. Headache J Head Face Pain. 2012;52(9):1387–1401. | ||
Barke A, Gaßmann J, Kröner-Herwig B. Cognitive processing styles of children and adolescents with headache and back pain: a longitudinal epidemiological study. J Pain Res. 2014;7:405–414. | ||
Zwart JA, Dyb G, Hagen K, et al. Depression and anxiety disorders associated with headache frequency. The Nord-Trøndelag Health Study. Eur J Neurol. 2003;10(2):147–152. | ||
Balottin U, Poli PF, Termine C, Molteni S, Galli F. Psychopathological symptoms in child and adolescent migraine and tension-type headache: a meta-analysis. Cephalalgia. 2013;33(2):112–122. | ||
Kato S, Sullivan PF, Evengård B, Pedersen NL. A population based twin study of functional somatic syndromes. Psychol Med. 2009;39(3):497–505. | ||
Kröner-Herwig B. Pediatric headache: associated psychosocial factors and psychological treatment. Curr Pain Headache Rep. 2013;17(6):1–9. | ||
Asmundson GJG, Norton PJ, Veloso F. Anxiety sensitivity and fear of pain in patients with recurring headaches. Behav Res Therapy. 1999;37(8):703–713. | ||
Norton PJ, Asmundson GJ. Anxiety sensitivity, fear, and avoidance behavior in headache pain. Pain. 2004;111(1):218–223. | ||
Drahovzal DN, Stewart SH, Sullivan MJ. Tendency to catastrophize somatic sensations: pain catastrophizing and anxiety sensitivity in predicting headache. Cogn Behav Ther. 2006;35(4):226–235. | ||
Martin AL, McGrath PA, Brown SC, Katz J. Anxiety sensitivity, fear of pain and pain-related disability in children and adolescents with chronic pain. Pain Res Manage. 2007;12(4):267–272. | ||
Tsao JC, Allen LB, Evans S, Lu Q, Myers CD, Zeltzer LK. Anxiety sensitivity and catastrophizing associations with pain and somatization in non-clinical children. J Health Psychol. 2009;14(8):1085–1094. | ||
Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: prospective prediction of panic attacks and Axis I pathology. J Psychiatr Res. 2006;40(8):691–699. | ||
Raphael KG, Marbach JJ, Gallagher RM. Somatosensory amplification and affective inhibition are elevated in myofascial face pain. Pain Med. 2000;1(3):247–253. | ||
Ak I, Sayar K, Yontem T. Alexithymia, somatosensory amplification and counter-dependency in patients with chronic pain. Pain Clinic. 2004;16(1):43–51. | ||
Gregory RJ, Manring J, Wade MJ. Personality traits related to chronic pain location. Ann Clin Psychiatry. 2005;17(2):59–64. | ||
Weickgenant AL, Slater MA, Patterson TL, Atkinson JH, Grant I, Garfin SR. Coping activities in chronic low back pain: relationship with depression. Pain. 1993;53(1):95–103. | ||
Luka-Krausgrill U, Reinhold B. Kopfschmerzen bei Kindern: Auftretensrate und Zusammenhang mit Stress, Stressbewältigung, Depressivität und sozialer Unterstützung. Zeitschrift für Gesundheitspsychologie. 1996;4(2):137–151. | ||
Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer Publishing Company; 1984. | ||
Ruscheweyh R, Nees F, Marziniak M, Evers S, Flor H, Knecht S. Pain catastrophizing and pain-related emotions: influence of age and type of pain. Clin J Pain. 2011;27(7):578–586. | ||
Vervoort T, Eccleston C, Goubert L, Buysse A, Crombez G. Children‘s catastrophic thinking about their pain predicts pain and disability 6 months later. Eur J Pain. 2010;14(1):90–96. | ||
Kröner-Herwig B, Maas J. The German Pain Catastrophizing Scale for Children (PCS-C) – psychometric analysis and evaluation of the construct. GMS Psycho Soc Med. 2013;10:Doc07. | ||
Szpalski M, Gunzburg R, Balagué F, Nordin M, Melot C. A 2-year prospective longitudinal study on low back pain in primary school children. Eur Spine J. 2002;11(5):459–464. | ||
Lynch AM, Kashikar-Zuck S, Goldschneider KR, Jones BA. Psychosocial risks for disability in children with chronic back pain. J Pain. 2006;7(4):244–251. | ||
Reneman M, Poels B, Geertzen J, Dijkstra P. Back pain and backpacks in children: biomedical or biopsychosocial model? Disabil Rehabil. 2006;28(20):1293–1297. | ||
Hoftun GB, Romundstad PR, Rygg M. Association of parental chronic pain with chronic pain in the adolescent and young adult: family linkage data from the HUNT Study. JAMA Pediatr. 2013;167(1):61–69. | ||
Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesthesia. 2013;111(1):52–58. | ||
Achenbach TM. Manual for the Youth Self-Report and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. | ||
Blais MA, Otto MW, Zucker BG, et al. The anxiety sensitivity index: item analysis and suggestions for refinement. J Pers Assess. 2001;77(2):272–294. | ||
Hampel P, Petermann F, Dickow B. SVF-KJ; Stressverarbeitungsfragebogen von Janke und Erdmann angepasst für Kinder und Jugendliche. Psychologische Diagnostik moderierender Persönlichkeitsmerkmale bei Kindern und Jugendlichen. Göttingen: Hogrefe; 2001:138–146. | ||
WHOQOL Group. The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998;46(12):1569–1585. | ||
Bowerman BL, O‘Connell RT. Linear Statistical Models: An Applied Approach. Los Angeles: Brooks/Cole; 1990. | ||
Menard S. Applied Logistic Regression Analysis. Duxbury, MA: Sage; 1995. | ||
Feldman DE, Shrier I, Rossignol M, Abenhaim L. Risk factors for the development of low back pain in adolescence. Am J Epidemiol. 2001;154(1):30–36. | ||
van Gessel H, Gaßmann J, Kröner-Herwig B. Children in pain: recurrent back pain, abdominal pain, and headache in children and adolescents in a four-year-period. J Pediatr. 2011;158(6):977–983. | ||
Messinger HB, Spielings EL, Vincent AJ. Overlap of migraine and tension-type headache in the International Headache Society classification. Cephalalgia. 1991;11(5):233–237. | ||
Laurell K, Larsson B, Eeg-Olofsson O. Headache in schoolchildren: association with other pain, family history and psychosocial factors. Pain. 2005;119(1):150–158. | ||
Borge AIH, Nordhagen R. Recurrent pain symptoms in children and parents. Acta Paediatr. 2000;89(12):1479–1483. | ||
Jones M, Stratton G, Reilly T, Unnithan V. A school-based survey of recurrent non-specific low-back pain prevalence and consequences in children. Health Educ Res. 2004;19(3):284–289. | ||
Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009;10(5):447–485. | ||
Kröner-Herwig B, Zernikow B. Schmerz bei Kindern [Pain in children]. In: Kröner-Herwig B, Frettlöh J, Klinger R, Nilges P, editors. Schmerzpsychotherapie. Vol. 8. Berlin: Springer; 2017:645–668. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.