Back to Journals » International Journal of General Medicine » Volume 16
Predicting Factors for Mortality in Patients After the Modified Blalock-Taussig Shunt Procedure in Developing Countries: A Retrospective Study
Authors Amelia P, Advani N, Pulungan AB, Djer MM, Hegar B, Prawira Y, Sukardi R
Received 28 July 2023
Accepted for publication 14 October 2023
Published 15 November 2023 Volume 2023:16 Pages 5291—5300
DOI https://doi.org/10.2147/IJGM.S432855
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Yuriy Sirenko
Putri Amelia,1 Najib Advani,2 Aman B Pulungan,2 Mulyadi M Djer,2 Badriul Hegar,2 Yogi Prawira,2 Rubiana Sukardi3
1Department of Child Health, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia; 2Department of Child Health, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia; 3Center of Integrated Cardiac Service, Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Correspondence: Putri Amelia, Department of Child Health, H. Adam Malik Hospital/ Faculty of Medicine, Universitas Sumatera Utara, Jalan Dokter Mansyur No. 5, Padang Bulan, Medan, 20155, Indonesia, Email [email protected]
Background: Blalock-Taussig (BT) is a palliative procedure that preserves blood circulation to the lungs and alleviates cyanosis in patients with congenital heart diseases and reduced pulmonary blood flow. BT shunt remains a routinely performed procedure in developing countries before definitive surgery. However, evidence on predictor factors of mortality after this procedure is still scarce in Indonesia. This study evaluated the predictive factors of mortality after the BT shunt procedure.
Methods: This retrospective study evaluated the medical record data of all postoperative BT shunt patients at Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia, from 2016 to 2020. We performed univariate and multivariate analyses to identify the predictors of in-hospital mortality.
Results: The total subjects in this study were 197 children, 107 (54.3%) boys and 90 (45.7%) girls. The median values for age and body weight at the time of surgery were 20 months (11 days – 32 years) and 7.9 (2.7– 42) kg. The most prevalent diagnosis was the Tetralogy of Fallot, found in 80 (40.6%) patients. In-hospital postoperative mortality was 20.8% (41 patients). Based on multivariate analysis, predictors associated with mortality were weight < 4.25 kg (OR 20.9; 95% CI 7.4– 59.0; p < 0.0001) and emergency procedures (OR 3.5; 95% CI 1.3– 9.5; p = 0.016).
Conclusion: The mortality rate after BT shunt at PJT Rumah Sakit Cipto Mangunkusumo was 20.8%. Based on multivariate analysis, weight < 4.25 kg and emergency procedures are two predictors of mortality in BT shunt.
Keywords: Blalock-Taussig shunt, congenital heart disease, Indonesia, mortality
Introduction
Congenital heart disease (CHD) is the most common type of birth defects found in 8 per 1000 live births.1 In developing countries, most CHDs is not detected until postnatal or later in life, during childhood or some until adulthood. About 25% of babies born with heart abnormality have critical CHD. These babies need surgery or any other procedure in the first year of life.2
Blalock-Taussig (BT) shunt is one of the most common palliative procedures performed in CHD patients. BT shunt aims to improve blood flow to the pulmonary circulation, alleviate cyanosis, promote pulmonary artery growth, and preserve cardiac preload, afterload, and coronary artery perfusion.1 BT shunt is still commonly performed in developing countries before the definitive correction. However, it has been rarely performed in developed countries as the development of surgical techniques and adequate technologies, and the availability of experts have made it possible to perform the definitive surgery as early as possible.2,3
Mortality after BT shunt in Indonesia is still high, ranging from 12.5 to 14.6%4 Even though BT shunt has become an integral part of CHD treatment in Indonesia for years, research assessing its mortality is still scarce. Investigating BT shunt procedure outcomes and factors that affect them is crucial to measuring and improving the future quality of care . The main causes of mortality in BT shunt procedures can include postoperative bleeding, reoperation due to acute thrombosis of the shunt, low cardiac output syndrome due to over-shunting, sepsis, diaphragm paralysis, vagus nerve paralysis, surgical wound infection, pulmonary haemorrhage, atelectasis, and CICU care for more than 48 hours. In the last three years at the Integrated Cardiac Services (ICS) of Dr Cipto Mangunkusumo Hospital (RSCM) Jakarta, the postoperative mortality rate of BT shunt was reported to be around 14.6%, with the most common cause of death being low cardiac output syndrome (LCOS). Meanwhile, the mortality rate after BT shunt in Harapan Kita Hospital was reported to be around 12.5%. Several recent reports on the outcomes of BT shunt procedures have shown high morbidity and mortality rates in neonates. Mortality in patients with one ventricle physiology is reported to be around 15%, while in patients with two ventricle physiology, it is 3–5%.4–6 Accordingly, this study aims to assess the predictive factors of mortality after the BT shunt procedure in Jakarta, Indonesia.
Methods
Study Design and Population
This retrospective cohort study was conducted at Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia, from November 2020 to January 2021. All CHD pediatric patients with a previous history of BT shunt procedures were included in the study during this period. Data were primarily obtained from medical records from January 2016 to December 2020; thus, patients with incomplete records were excluded.
The Committee of Ethics of the Faculty of Medicine, University of Indonesia, has approved this study. The permission to assess the medical records was obtained from Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia. Informed consent was obtained from the patients before participating in the study.
Data Collection
We collected the baseline characteristics of patients’ age, sex, weight, nutritional status, and diagnosis. Meanwhile, additional predictors of mortality after the BT shunt procedure assessed in this study were the type of surgery (urgency/emergency), surgical approaches (sternotomy or thoracotomy), and the need for packed red cell (PRC) transfusion after the procedure. We diagnosed malnutrition in children based on the World Health Organization (WHO) growth chart 2006 (Z score <-2 SD for children below five years old and the Centers for Disease Control and Prevention (CDC) growth chart 2000 for children age 5–18 years old (weight/height <90%). This classification has been used by the Indonesian Pediatric Association (IDAI).
Outcome Measures
The primary outcome investigated was in-hospital mortality. In addition, we also found the predictor factors of mortality after the BT shunt procedure.
Data Analysis
Data analysis used IBM SPSS version 25.0. The Categorical data description was with their absolute (n) and relative frequencies (%). For normally distributed quantitative data, we presented it with mean and standard deviation. On the other hand, when it was not normally distributed data, we expressed them as median and range. The association between variables assessment initially was with bivariate analysis (chi-square or Fisher exact tests) . If the predictors had a p-value <0.25, they were deemed eligible for multivariate analysis, further determining the relationship between predictors and outcomes. Multivariate analysis was performed to determine the predictors associated with the occurrence of independent postoperative BT shunt mortality. For such analysis, all predictors with a p value <0.25 in the bivariate analysis were included in the multiple logistic regression analysis. The results of the multivariate analysis were reported as odds ratio (OR) with 95% confidence interval.
Ethics Approval and Consent to Participate
The Ethics Committee of the Faculty of Medicine, University of Indonesia – Cipto Mangunkusumo Hospital approved this study (KET-1301/UN2.F1/ETIK/PPM.00.02/2020).
Results
One hundred and ninety-seven patients met this study’s inclusion and exclusion criteria . The baseline characteristics are described in Table 1. Most of the subjects in this study have normal nutritional status. The most common diagnosis in this study was Tetralogy of Fallot (40.6%).
 |
Table 1 Baseline Characteristics of the Study Subjects |
Table 2 shows the characteristics of the BT shunt procedure performed at our center. Most of the surgeries performed were elective (81.2%) and without cardiopulmonary bypass (86.3%). The most frequent shunt size was 4 mm, and the median diameter and weight ratio were 0.4 mm/Kg. The majority of subjects did not get blood transfusion after the procedure (58.4%).
 |
Table 2 Characteristics of BT Shunt Procedures |
There were two numeric variables assessed separately from other categorical predictors. They are age and weight. We used the receiver operating characteristic curves to determine these variables’ cut-off in predicting the mortality after the BT shunt procedure (Figure 1). From the curve, we found that the area under curve (AUC) value of weight as a mortality predictor was 81% (95% CI, 74.1 to 89.7%; p < 0.0001). We determined the optimal weight cut-off from the line curve to predict the mortality after the BT shunt, which was 4.25 Kg (sensitivity: 51.2%; specificity: 94.2%) (Figure 2). Meanwhile, the AUC value for age was 75% (95% CI, 66.9 to 84.9%; p < 0.0001) (Figure 3). The age’s cut-off for predicting mortality was 270 days (sensitivity: 61%; specificity: 78.2%) (Figure 4).
 |
Figure 1 ROC curve of weight as a predictor for mortality after BT shunt. |
 |
Figure 2 Weight cut-off in predicting mortality. |
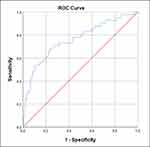 |
Figure 3 ROC curve of age as a predictor for mortality after BT shunt. |
 |
Figure 4 Age cut-off in predicting mortality. |
We evaluated six potential predictors of mortality after the BT shunt procedure among these subjects. Based on the bivariate analysis, four predictors showed a significant association with mortality. They are age, weight <4.25 Kg, type of surgery (elective/emergency), and surgical approach. Weight <4.25 Kg and emergency surgery significantly affected the mortality after the BT shunt procedure. Weight under <4.25 Kg increased the mortality risk by 20 times, while emergency procedures raised the risk by 3.5 times (Table 3).
 |
Table 3 Bivariate and Multivariate Analysis of Mortality |
The mortality trend after the BT shunt procedure between 2016 and 2020 can be seen in Table 4, which shows a downward trend over the years. The total mortality from 2016 to 2020 was 41 (20.8%) (Figure 5).
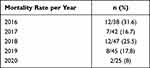 |
Table 4 Mortality of BT Shunt per Year |
 |
Figure 5 Kaplan–Meier 5 years survival post BT shunt operation. |
Discussion
The median of patients’ weight and age was 7.9 Kg and 20 months when the procedure was performed. In this study, many older children underwent surgery due to the complex anatomy of defects and sub-development of pulmonary artery branches. This finding contrasted with data from developing countries that mostly came from younger children. The previous BT shunt research at our center also had a wide range of ages, from 15 days to 17 years old.5 A study in Canada had a median age of 8 days, and the mean weight was 3.1 Kg.1 This apparent difference might be caused by the gap in healthcare access that remains a significant challenge in developing countries. Most patients (47.2%) had good nutritional status. However, 24.4% of patients had mild-moderate malnutrition, while the other 15.7% had severe malnutrition. Malnutrition is a common finding in CHD. The incidence of malnutrition-related CHD in Indonesia is 70.7%, and 22.4% is severe.6 Previous studies also reported that children with CHD tend to have height and weight under the 50th percentile; therefore, failure to thrive is expected in this cohort.7 Several factors are involved in this malnutrition tendency, such as inadequate intake, increased metabolic requirements, and the abnormality in absorption secondary to CHD.7,8 Early intervention in CHD is required to improve children’s nutritional status. A palliative procedure like a BT shunt can help patients to improve their condition before the definitive correction surgery. However, it is vital to notice that the outcomes of BT shunt are also poorer in children with severe malnutrition.7,8
One of the most important predictors of palliative procedure outcomes is age. Cardiac surgery is ideally performed at a younger age to lower morbidity and mortality. However, not every child is eligible for surgery due to anatomical complexity, hemodynamic status, and pulmonary vascular resistance. The palliative procedure at the optimal age is vital as it can significantly affect the outcomes.9 In this study, the patients’ median age was 20 months when the procedure was performed.
The thoracotomy approach was utilized more often than sternotomy for the BT shunt procedure at our center (54.3% vs 45.7%). This approach is considered more accessible, faster, and safer. However, a study in Boston reported that thoracotomy had a higher failure rate than sternotomy.10 One of the common complications is phrenic nerve paralysis, with an incidence of 23.8% in patients who underwent this procedure via thoracotomy.11,12
However, only two predictors, weight <4.25 Kg and type of surgery (elective/emergency), significantly affected the mortality after the BT shunt procedure. Weight under <4.25 increased the mortality 20.8 times, while the emergency type of surgery raised the mortality chance by 3.5 times. No study describes the association between the type of surgery (elective/emergency) and mortality risk.4,13 Why low body weight may predispose patients to death because of the unavailability of grafts with a size under 3 mm.
The mortality rate of patients in this study was 21% (41 people). This is higher than the previous data on postoperative BT shunt mortality at Cipto Mangunkusumo Hospital in the last three years, which was 14.6%. The mortality rate of patients in this study was the postoperative mortality rate of BT shunts from 2016 to 2020, which was 31.6%, 16.7%, 25.5%, 17.8% and 8%, respectively. This mortality rate has been decreasing each year because the development of surgical techniques, the improvement of the cardiac surgical team’s ability, and postoperative care have caused the mortality rate to be very low. The mortality rate after BT shunt surgery at Harapan Kita Hospital was reported to be around 12.5%.10
Finally, this study helps describe the outcomes after BT shunt in Indonesia, where the data were rarely available previously. The study’s population was also large enough to describe these outcomes. A multicenter approach might also be crucial for future adoption because of the high variability in experience and facilities between centers in Indonesia.
Conclusion
The mortality rate after BT shunt at PJT Rumah Sakit Cipto Mangunkusumo was 20.8%. Based on multivariate analysis, the predictor factors associated with mortality were weight <4.25 kg and emergency procedures.
Abbreviations
CHD, congenital heart disease; BT, Blalock-Taussig; PRC, packed red cell; OR, odds ratio; CI, confidence interval; PA-IVS, pulmonary atresia with intact ventricular septum; PA-VSD, pulmonary atresia with ventricle septal defect; CAVSD, complete atrioventricular septal defect, PS, pulmonary stenosis; DOLV, double outlet left ventricle; DORV, double outlet right ventricle; CPB, cardiopulmonary bypass; AUC, area under curve.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The Ethics Committee of the Faculty of Medicine, University of Indonesia – Cipto Mangunkusumo Hospital approved this study (KET-1301/UN2.F1/ETIK/PPM.00.02/2020). All patients provided informed consent, and all procedures were conducted according to the Declaration of Helsinki. Written informed parental consent was obtained from the parents of patient for publication of this study. We performed informed parental consent to the parents of patient.
Acknowledgments
The authors thank Universitas Indonesia, Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sasikumar N, Hermuzi A, Fan CPS, et al. Outcomes of Blalock-Taussig shunts in current era: a single center experience. Congenit Heart Dis. 2017;12(6):808–814. doi:10.1111/chd.12516
2. Jonas RA. Congenital Heart Surgery in Developing Countries. Pediatr Card Surg Annu. 2008;11(1):3–6. doi:10.1053/j.pcsu.2007.12.001
3. Rana JS, Ahmad KA, Shamim AS, Hassan SB, Ahmed MA. Blalock-Taussig shunt: experience from the developing world. Hear Lung Circ. 2002;11(3):152–156. doi:10.1046/j.1444-2892.2002.00145.x
4. Riyandi M, Lilyasari O, Juzar DA, Rahmat B. Age criteria as operative mortality predictor after modified Blalock-Taussig shunt. Indones J Cardiol. 2019;40(1):216–221. doi:10.30701/ijc.v40i1.763
5. Murni IK, Djer MM, Yanuarso PB, et al. Outcome of pediatric cardiac surgery and predictors of major complication in a developing country. Ann Pediatr Cardiol. 2019;12(1):38. doi:10.4103/apc.APC
6. Amelia P, Adriansyah R, Lubis B, Akil M. The association between cyanotic and acyanotic congenital heart disease with nutritional status. Open Access Maced J Med Sci. 2020;8(B):245–248. doi:10.3889/oamjms.2020.3978
7. Poskitt EME. Failure to thrive in congenital heart disease. Arch Dis Child. 1993;68(2):158–160. doi:10.1136/adc.68.2.158
8. Chen CW, Li CY, Wang JK. Growth and development of children with congenital heart disease. J Adv Nurs. 2004;47(3):260. doi:10.1111/j.1365-2648.2004.03090.x
9. Knirsch W, Zingg W, Bernet V, et al. Determinants of body weight gain and association with neurodevelopmental outcome in infants operated for congenital heart disease. Interact Cardiovasc Thorac Surg. 2010;10(3):377–382. doi:10.1510/icvts.2009.216135
10. Odim J, Portzky M, Zurakowski D, et al. Sternotomy approach for the modified Blalock-Taussig shunt. Circulation. 1995;92(9):256–261. doi:10.1161/01.CIR.92.9.256
11. Talwar S, Kumar MV, Muthukkumaran S, Airan B. Is sternotomy superior to thoracotomy for modified Blalock-Taussig shunt? Interact Cardiovasc Thorac Surg. 2014;18(3):371–375. doi:10.1093/icvts/ivt513
12. Akay TH, Ozkan S, Gultekin B, et al. Diaphragmatic paralysis after cardiac surgery in children: incidence, prognosis and surgical management. Pediatr Surg Int. 2006;22(4):341–346. doi:10.1007/s00383-006-1663-2
13. Küçük M, Özdemir R, Karaçelik M, et al. Risk factors for thrombosis, overshunting and death in infants after modified Blalock-Taussig shunt. Acta Cardiol Sin. 2016;32(3):337–342. doi:10.6515/ACS20150731A
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
