Back to Journals » International Journal of General Medicine » Volume 17
Predicting Endothelium-Dependent Diastolic Function (FMD) and Its Correlation with the Degree of Coronary Artery Disease (CAD) and Plaque Vulnerability for Cardiovascular Events
Authors Zhang G, Yang J, Xing H, Yin H, Gu G
Received 27 August 2023
Accepted for publication 21 February 2024
Published 22 March 2024 Volume 2024:17 Pages 1117—1125
DOI https://doi.org/10.2147/IJGM.S435417
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Yuriy Sirenko
Guangming Zhang,1 Jing Yang,1 Hanghang Xing,1 Hongning Yin,2 Guoqing Gu1
1Department of Cardiology, The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei, 050004, People’s Republic of China; 2Department of Heart ultrasound, The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei, 050004, People’s Republic of China
Correspondence: Guangming Zhang, Department of Cardiology, The Second Hospital of Hebei Medical University, 215, Heping West Road, Shijiazhuang, Hebei, 050004, People’s Republic of China, Tel +86 311-66002999, Email [email protected]
Objective: This study aims to investigate the correlation between vascular endothelium-dependent diastolic function (FMD) and the degree of coronary artery disease (CAD), plaque vulnerability, and its predictive value for cardiovascular events.
Methods: Initially, patients (n=100) who were admitted from January 2020 to January 2021 and intended to undergo percutaneous coronary intervention (PCI) were selected. Further, FMD in all patients was determined before the procedure and divided into a high-FMD group (≥ 4.2%) and a low-FMD group (< 4.2%). Further, the data of two groups, including general information, coronary artery lesions, and plaque fibrous cap, were compared. Finally, the relationship between FMD and the degree of coronary artery lesions and plaque vulnerability was analyzed.
Results: No significant differences were observed concerning general information, number of coronary arteries-associated branches, lesion type, involvement of the left main stem (LM), the proportion of chronic occluded lesions (CTO), and lipid pool angle between the low-FMD group and the high-FMD group (P > 0.05). Nevertheless, the degree of stenosis of the lesions in the low-FMD group was significantly higher than in the high-FMD group (P < 0.05). In addition, the thickness of the fibrous cap was considerably lower than that in the high-FMD group (P < 0.05). Moreover, the incidence rate of TCFA was significantly higher than the high-FMD group (P < 0.05). The correlation analysis showed that FMD was significantly negatively correlated with the degree of coronary artery lesion stenosis and TCFA (P < 0.05) and positively correlated with the fibrous cap thickness (P < 0.05).
Conclusion: Overall, a negative correlation between FMD and the degree of coronary stenosis, plaque vulnerability, and a high predictive value for post-PCI cardiovascular events suggested that FMD could be a critical diagnostic marker for CAD.
Keywords: coronary heart disease, endothelium-dependent diastolic function, lesion extent, plaque vulnerability, predictive value
Background
Cardiovascular-related diseases (CVDs) are the most common ailments globally, accounting for numerous mortalities globally. Among CVDs, coronary artery disease (CAD) has emerged as the leading cause of heart disease and cardiovascular events.1,2 To treat and prevent CVDs, it is required to understand the pathogenesis and mechanisms of the associated factors comprehensively. Vascular endothelial cells are important components of the vascular wall, which can regulate the physiological functions of blood vessels, including vasodilation and constriction.3 In this vein, several reports indicated that vascular endothelial dysfunction was the earliest pathophysiological change in the atherosclerotic process, thus acting as an important marker of atherosclerosis. Typically, endothelial dysfunction often results in immediate variations in the vascular tone and functional attributes. The brachial artery-mediated vascular endothelium-dependent diastolic function (FMD) signifies impaired coronary microcirculation, enhanced vascular resistance, and compromised diastolic relaxation.4–6 These acute consequences may manifest as angina pectoris, myocardial ischemia, and an increased susceptibility to arrhythmias, thereby elevating the risk of acute cardiovascular events. The dysfunctional endothelium promotes the recruitment of inflammatory cells, oxidative stress, and the formation of atherosclerotic plaques. Subsequently, these plaques may undergo changes that render them vulnerable to rupture, leading to thrombus formation and acute cardiovascular events, such as myocardial infarction and stroke.6 A recent study employed intravascular ultrasound, reporting a strong correlation between lower FMD values and larger necrotic nuclei in the coronary plaques.7 Therefore, FMD assessment may become an effective, non-invasive method to determine the degree of disease severity and plaque vulnerability in CAD patients.
To this end, percutaneous coronary intervention (PCI) has emerged as an effective and widespread treatment for patients with CAD, which, however, results in in-stent restenosis and cardiovascular events. A previous study8 indicated that impaired endothelial function in PCI patients exhibited a relationship with prognosis. In addition, FMD could be used as a predictor of cardiovascular events after PCI. Considering these aspects, this study investigated the correlation between endothelium-dependent diastolic function and the extent of CAD, as well as plaque vulnerability. Moreover, herein, we intend to assess its predictive value for cardiovascular events towards reducing cardiovascular events by improving vascular endothelial function, enlightening patients’ quality of life, and reducing the global burden of various CVDs.
Subjects and Methods
Patients’ Information
Patients (n = 100) anticipated to undertake PCI treatment from January 2020 to January 2021 were recruited for the study. The inclusion criteria for the recruitment of the patients were included, such as (1) age of 35~80 years old, (2) meeting the clinical diagnostic criteria of CAD and taking PCI treatment, and (3) complete clinical data. Contrarily, the exclusion criteria were set as follows: (1) patients with severe insufficiency of heart, liver, and kidney functions; (2) patients with combined acute and chronic infections; (3) patients with cerebrovascular disease and CHD; (4) patients with contraindication to coronary angiography; (5) patients with malignant tumors; and (6) patients who lost their visits during the follow-up period.
Collection of General Information
The general information, including various demographic factors and pathological data of the patients, were collected, such as age, sex, body mass index (BMI), past medical history (hypertension, diabetes mellitus, hyperlipidemia, chronic renal insufficiency, history of PCI, and history of myocardial infarction), the history of smoking, post-admission lipids, glycosylated hemoglobin, creatinine clearance, left ventricular ejection fraction, and intake of basal medications (aspirin, clopidogrel, statins, among others.
FMD Measurements
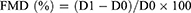
Notably, the high-frequency ultrasound was applied to measure the FMD of the femoral artery before and after 3d of PCI following the procedure. Initially, the vascular drugs were discontinued 24 hours before the preliminary examination of the subject. Further, FMD was recorded using a vascular endothelial function detector in the early morning on an empty stomach in a calm state. Then, the mean value of the brachial artery basal internal diameter at the end of diastole was measured and referred to as D0. Further, the forearm pressure was increased to 280~300 mmHg, deflated for 5 min, and stayed for 60~90s. Then, the brachial artery internal diameter was recorded and stated as D1. Finally, the resultant FMD value was calculated according to the below formula (Eq. 1)
Collection of Diseased Vessels
To enumerate the diseased vessels, the cumulative number of branches of the diseased vessel was recorded, along with the type of lesion, the involved left main stem (LM), and a chronic total occlusive (CTO) lesion during PCI. Further, the vascular lesions were measured by applying a quantitative coronary angiography analysis system, in which the normal reference vessel diameter of the diseased vessel, the vessel diameter at the lesion, the degree of stenosis of the lesion, and the length of the lesion were measured.
Optical Coherence Tomography (OCT) Examination
Further, OCT examination was applied to determine the plaque fibrous cap thickness, in which the cap thickness was measured thrice at the thinnest site, and the mean value was calculated. The thin cap fibrous plaques (TCFA) were defined as lipid plaques >90° and fibrous cap thickness <65 μm. The bright spots within the fibrous cap and their subsequent shadows were considered a macrophage accumulation.
Statistical Analysis
The statistical analysis of the recorded data was performed using the SPSS 27.0 software. The measured data conformed to the normal distribution and were expressed as mean ± standard deviation (x±s) from three replicates. Further, the comparison between the two groups was tested by the independent sample t-value, and the counted data were expressed as n (%). The correlation coefficients were calculated using Pearson’s and Spearman’s methods. The predictive value of FMD for post-PCI cardiovascular events was analyzed by the subject’s work characteristics, ie, the Receiver Operating Characteristic (ROC) curve. Notably, the difference was considered statistically significant at a defined level of P < 0.05. The predictive value of FMD for cardiovascular events after PCI was analyzed, considering P < 0.05 statistically significant.
Results
Comparison of General Information Between the Two Groups
From January 1, 2020, to January 1, 2021, patients with CAD (n=100 cases) received the PCI treatment. After PCI treatment, the FMD values were collected. According to the median value of FMD (4.2), the 100 cases were grouped into high-FMD (n=58) and low-FMD groups (n=42). Initially, the general information between the groups of high-FMD and low-FMD groups was compared. Various characteristics of general information of the two notified groups, including demographic and pathophysiological information, were observed and tabulated in Table 1. It was observed that these features of gender, age, BMI, smoking history, underlying diseases, lipids, creatinine, left ventricular ejection fraction, and basal medication between the high-FMD and the low-FMD groups showed no statistically significant difference (P > 0.05).
 |
Table 1 A Summary Shows the Comparison of General Information of the Two Groups |
Comparison of Coronary Artery Lesions in the FMD Groups
Further, a comparison of coronary artery lesions between the two groups indicated no significant difference in the number of involved branches, lesion type, involved LM, and CTO ratio in the high-FMD group compared with that in the low-FMD group (P > 0.05, Table 2). Moreover, the degree of lesion stenosis in the low-FMD group was significantly greater than that of the high-FMD group (P < 0.05, Table 2).
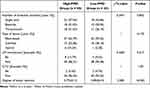 |
Table 2 A Summary Indicates the Comparison of Coronary Artery Lesions |
Comparison of OCT Findings Between the Two Groups
The comparison of OCT examination results between the two groups indicated that the thickness of the fiber cap in the low-FMD group was significantly lower than that in the high-FMD group (P < 0.05). Moreover, the proportion of TCFA was considerably higher in the low-FMD group than in the high-FMD group (P < 0.05). To this end, the difference in the angle of the lipid pool was not statistically significant over the high-FMD group (P > 0.05, Table 3).
 |
Table 3 A Summary Shows the Comparison of OTC Findings Between the Two Groups |
Relationship Between FMD and Degree of Stenosis and Plaque Vulnerability in Coronary Artery Lesions
Further, Pearson correlation analysis was applied to explore the relationship between the FMD and degree of stenosis and plaque vulnerability in CAD. It was observed from the results, as stated in Table 4, that a significant negative correlation between FMD and the degree of stenosis of the diseased arteries (P < 0.05) and a significant positive correlation with the thickness of the fibrous cap (P < 0.05) was established. Moreover, the Spearman correlation analysis indicated a significant negative correlation between FMD and TCFA formation (P < 0.05, Table 4).
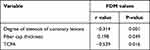 |
Table 4 The Data Shows the Relationship Between FMD and the Degree of Stenosis and Plaque Vulnerability in Coronary Artery Lesions |
Cardiovascular Events After PCI
Further, the cardiovascular events were observed by following up on the patients’ condition after PCI. The 18-month follow-up after PCI resulted in 22 cardiovascular events in 100 patients, including 13 myocardial infarctions, 5 sudden cardiac deaths, and 4 coronary revascularizations. Nevertheless, the study yielded an impressive cardiovascular good event rate of 22% (22/100).
Comparison of FMD in Different Prognostic Groups
Further, the FMD values in different prognostic groups were compared. It was observed that the FMD values in the cardiovascular event group were significantly lower than those in the no cardiovascular group. Notably, the difference was statistically significant (P < 0.05, Table 5). The survival analysis showed that the low-FMD group showed worse clinical outcomes compared to the high-FMD group (Figure 1).
 |
Table 5 A Summary Shows the Comparison of FMD in Different Prognostic Groups |
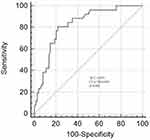 |
Figure 1 The Kaplan-Meier curves analyze the difference between the events in the groups with high- and low-FMD. |
Clinical Value of FMD in Predicting Cardiovascular Events After PCI
Finally, the clinical value of FMD in predicting cardiovascular events after PCI was determined using the ROC curve analysis. The ROC curve analysis indicated that the best cut-off value of FMD for predicting cardiovascular events after PCI was ≤5.24% (Figure 2). In addition, the resultant area under the curve (AUC) was 0.825, with a 95% CI of 0.736–0.893, P=0.006. To this end, Youden’s index was 0.592, giving a sensitivity of 80.77% and a specificity of 78.38%. The positive and negative predictive values were 60% and 91.89%, respectively.
 |
Figure 2 The image shows the ROC curve of FMD for predicting cardiovascular events after PCI. |
Discussion
CAD has emerged as one of the major forms of CVDs, in which various factors often influence the development of CAD. Among such influential factors, abnormal vascular endothelial function plays a key role in developing coronary artery lesions. The vascular endothelium, an inner layer of the vascular wall, is often essential for maintaining vascular tone, anti-inflammatory, anti-thrombotic, and other physiological functions.9 In the case of endothelial function impairment, the vessel wall is often prone to thickening, thrombosis, and increased plaque vulnerability, promoting the development of coronary lesions.10,11 Subsequently, the increased plaque vulnerability critically reflects the stability and susceptibility to rupture the formed plaque.12 These vulnerable plaques prone to thrombosis can lead to serious cardiovascular events, such as myocardial infarction or ischemic stroke. Together, vascular endothelial dysfunction is an early change in the atherosclerotic process and an important marker of atherosclerosis, independently predicting cardiovascular events and leading to mortality.
Typically, the vascular endothelial function in clinical practice can be reflected by measuring brachial artery flow-mediated FMD. Previous reports demonstrated13 that brachial artery-mediated FMD predicted adverse cardiovascular events, possibly reflecting coronary endothelial dysfunction. There is no uniformity regarding the most appropriate FMD cut-off value in diagnosing CAD. In several reports, the FMD value of <4.5% showed higher sensitivity and specificity in diagnosing CAD. Moreover, several researchers believed the FMD value of <5.64% was the optimal cut-off value for predicting CAD-associated lesions.14,15 Accordingly, in the current study, we divided the high-FMD group and low-FMD group with a cut-off value of 4.2%. The degree of lesion stenosis in the low-FMD group was significantly higher than that in the high-FMD group. Thus, FMD could be related to the degree of lesion stenosis. Previous studies confirmed that brachial artery FMD was significantly impaired in patients with CAD, indicating that the impairment could correlate with the degree of coronary artery lesion.16 In another instance, it was demonstrated17 that the more extensive the coronary artery lesion, the poorer the endothelial function of the patient and the lower the FMD value. Indeed, the severity of CAD involves several aspects, including the number of diseased vessel branches, the type of diseased vessel, plaque vulnerability, and the status of the necrotic core. In this study, no significant difference was observed in comparing the number of involved branches, lesion type, involved LM, and CTO ratio between the high-FMD and low-FMD groups. These findings were in discrepancy with the study by Guo et al,18 indicating that the FMD of the multi-branch lesion group was significantly lower than that of the double-branch lesion group and the single-branch lesion group.
Moreover, the FMD value of the double-branch lesion group was considerably lower than that of the single-branch lesion group, meaning the number of branches of the diseased vessel and FMD. Overall, FMD is also correlated with the number of diseased vessel branches. This discrepancy between the findings of this study and the reported literature might be due to the use of different variability in patient populations. Specifically, Guo et al enrolled 130 patients with suspected CAD, while our study recruited 100 patients with CAD. Notably, the pathogenesis of CAD often involves the presence of unstable plaques in the coronary arteries, in which the stability of plaques is closely related to their morphological characteristics. Usually, the unstable plaques appear as eccentric plaques, characterized by many inflammatory cell infiltrates, low collagen content, thin fibrous caps, and a large extent of lipid core necrotic areas.19,20 Such eccentric plaques are prone to rupture and thrombus formation, which in turn leads to the occurrence of adverse cardiovascular events.21,22 To this end, OTC is an endovascular imaging technique developed recently that distinguishes red and white thrombus, reveals the plaque’s nature, identifies vulnerable plaques, and directly measures the fibrous cap thickness.23,24 In the current study, the experimental results showed a significant difference in fiber cap thickness and TCFA between the high-FMD group and the low-FMD group, indicating that FMD could effectively assess the stability of lipid plaques. Furthermore, a correlation analysis was taken to show that FMD possessed a significant negative correlation with the degree of coronary lesion stenosis and TCFA formation and a positive correlation with fibrous cap thickness.
Although an incidence of in-stent restenosis existed after PCI, drug-eluting stents (DES) significantly reduced the risk of restenosis.25 Moreover, balancing the anti-restenosis effects of the drug with the preservation of endothelial function remains a critical consideration in the design of DES. Several efforts have been dedicated to optimizing stent formulations towards minimizing the impact on endothelial cells while effectively preventing restenosis. In one case, impaired FMD predicted in-stent restenosis and cardiovascular events in PCI patients.26 However, the use of DES altered the association between endothelial function and in-stent restenosis as the released drugs from the stent strongly inhibited the endothelial cell regrowth in the stent. These consequences necessitated a reassessment of the relationship between impaired endothelial function and prognosis in patients undergoing PCI.27,28 In this study, FMD was tested in the early post-PCI period, and significant differences in FMD values were found in different prognostic groups, suggesting that FMD could be used as a potential predictor of cardiovascular events after PCI. Finally, the ROC analysis curve showed an AUC value of 0.825 in terms of FMD for predicting post-PCI cardiovascular events, a sensitivity of 80.77%, and a specificity of 78.38%, confirming that monitoring FMD in the early post-PCI period could possess a high predictive value for cardiovascular events.
Conclusion
In summary, vascular endothelial damage has emerged as one of the mechanisms of CHDs. In this article, we observed a significant correlation between FMD and the degree of stenosis of coronary artery lesions and plaque vulnerability. These events indicated that early monitoring of FMD after PCI showed a high predictive value for cardiovascular events. Despite the exploration of predicting the correlation between FMD and the degree of CAD, the current study suffers from some key limitations. First, as it was a retrospective analysis, some cases had to be thus excluded. Second, the sample size was small, requiring a greater sample size to validate the findings. Third, the follow-up period was too short, imposing the extended support for establishing the conclusion. Fourth, the imaging properties of nodules were not considered during the study. Our group will study the imaging properties of nodules in future investigations. Fifth, a specific limitation was the absence of follow-up in the medical records following the patient’s discharge from the hospital. The reasons could be that most cases were either placed low emphasis or did not document the need for follow-ups. In the following relevant study, we will ensure to address these limitations in the future.
Data Sharing Statement
All data can be obtained upon request.
Ethical Approval and Consent to Participate
This study was approved by the Research Ethics Committee at The Second Hospital of Hebei Medical University. All procedures involving human participants were approved by the institutional and national research committee and conformed to the ethical guidelines of the Declaration of Helsinki. All patients gave written informed consent.
Funding
The study was funded by the 2020 Hebei Provincial Department of Finance Elderly Disease Prevention and Control Funding Project: The Relationship between Endothelial Dysfunction and Plaque Severity and Vulnerability in Elderly Coronary Heart Disease Patients and Its Prognostic Significance. (No.303163320).
Disclosure
All authors have declared no competing interests for this work.
References
1. Katta N, Loethen T, Lavie CJ, et al. Obesity and coronary heart disease: epidemiology, pathology, and coronary artery imaging. Curr Prob Cardiol. 2021;46(3):100655. doi:10.1016/j.cpcardiol.2020.100655
2. Dong Y, Chen H, Gao J, et al. Molecular machinery and interplay of apoptosis and autophagy in coronary heart disease. J Mol Cell Cardiol. 2019;136:27–41. doi:10.1016/j.yjmcc.2019.09.001
3. Cheng H, Zhong W, Wang L, et al. Effects of shear stress on vascular endothelial functions in atherosclerosis and potential therapeutic approaches. Biomed Pharmacother. 2023;158:114198. doi:10.1016/j.biopha.2022.114198
4. Ruggiero D, Paolillo S, Rattag D. 1. Endothelial function as a marker of pre-clinical atherosclerosis: assessment techniques and clinical implications. Monaldi Arch Chest Dis. 2013;80(3):106–110. doi:10.4081/monaldi.2013.71
5. Duan H, Zhang Q, Liu J, et al. Suppression of apoptosis in vascular endothelial cell, the promising way for natural medicines to treat atherosclerosis. Pharmacol Res. 2021;168:105599. doi:10.1016/j.phrs.2021.105599
6. Liang S, Zhang J, Ning R, et al. The critical role of endothelial function in fine particulate matter-induced atherosclerosis. Particle Fiber Toxicol. 2020;17:1–24.
7. Sawada T, Emoto T, Motoji Y, et al. Possible association between non-invasive parameter of flow-mediated dilatation in brachial artery and whole coronary plaque vulnerability in patients with coronary artery disease. Int J Cardiol. 2013;166(3):613–620. doi:10.1016/j.ijcard.2011.11.101
8. Munk PS, Butt N, Larsen AI. Endothelial dysfunction predicts clinical restenosis after percutaneous coronary intervention. Scand Cardiovasc J. 2011;45(3):139–145. doi:10.3109/14017431.2011.564646
9. Wang X, Gao M, Zhou S, et al. Trend in young coronary artery disease in China from 2010 to 2014: a retrospective study of young patients≤45. BMC Cardiovasc Disord. 2017;17(1):18. doi:10.1186/s12872-016-0458-1
10. Barak OF, Mladinov S, Hoiland RL, et al. Disturbed blood flow worsens endothelial dysfunction in moderate-severe chronic obstructive pulmonary disease. Sci Rep. 2017;7(1):16929. doi:10.1038/s41598-017-17249-6
11. Pretorius D, Richter RP, Anand T, et al. Alterations in heparan sulfate proteoglycan synthesis and sulfation and the impact on vascular endothelial function. Matrix Biol Plus. 2022;16:100121. doi:10.1016/j.mbplus.2022.100121
12. Craighead DH, Freeberg KA, Seals DR. Vascular endothelial function in midlife/older adults classified according to 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines. J Am Heart Assoc. 2020;9(17):e016625. doi:10.1161/JAHA.120.016625
13. Deng YQ, Zhang ZJ, Li HX, et al. Value of Vascular Endothelial Function and Homocysteine in Prediction of Coronary Heart Disease. Chin General Pract. 2013;16(11):3672–3675.
14. Kuvin JT, Patel AR, Sliney KA, et al. Peripheral vascular endothelial function testing as a noninvasive indicator of coronary artery disease. J Am Coll Cardiol. 2001;38(7):1843–1849. doi:10.1016/S0735-1097(01)01657-6
15. Simova I, Katova T, Denchev S. Diagnostic accuracy of flow-mediated dilatation and intima-media thickness for the presence of significant coronary artery disease. J Am Soc Hypertens. 2009;3(6):388–394. doi:10.1016/j.jash.2009.09.003
16. Spanos K, Tzorbatzoglou I, Lazari P, et al. Carotid artery plaque echomorphology and its association with histopathologic characteristics. I Masc Surg. 2018;68(6):1772–1 780.
17. Li S, Sun L, Qi L, et al. Effect of high homocysteine level on the severity of coronary heart disease and prognosis after stent implantation. J Cardiovasc Pharmacol. 2020;76(1):101–105. doi:10.1097/FJC.0000000000000829
18. Guo CC, Peng YM, Zhang YQ, et al. Predictive value of flow mediated dilatation for coronary artery lesions. Chin J Arteriosc. 2018;26(7):715–719.
19. Hu DQ, Huang ZX, Chan TM, Dong W, Lu X, Duan H. Acute coronary syndrome risk prediction based on GRACE Risk Score. Stud Health Technol Inform. 2017;245:398–402.
20. Kakkos SK, Griffin MB, Nicolaides AN, et al. Size of juxtaluminal hypoechoic area in ultrasound images of asymptomatic carotid plaques predicts the occurrence of stroke. Vasc Surg. 2012;57(3):609–6181. doi:10.1016/j.jvs.2012.09.045
21. Puri R, Nissen SE, Shao M, et al. Coronary atheroma volume and cardiovascular events during maximally intensive statin therapy. Eur Heart J. 2017;38(12):960–968.
22. Otsuka F, Sakakura K, Yahagi K, et al. Is necrotic core a marker of adverse plaque morphology? A multimodality intravascular imaging study. J Am Coll Cardiol. 2020;75(10):1171–1182.
23. Zhang L, Li X, Lyu Q, et al. Imaging diagnosis and research progress of carotid plaque vulnerability. Clin Ultrasound. 2022;50(7):905–912. doi:10.1002/jcu.23266
24. Fuji K, Kawasaki D, Masutani M. OCT assessment of thin-cap fibroatheroma distribution in native coronary arteries. JACC Cardiovasc Imaging. 2010;3(2):168–175. doi:10.1016/j.jcmg.2009.11.004
25. Serruys PW, Degertekin M, Tanabe K, et al. Intravascular ultrasound findings in the multicenter, randomized, double-blind RAVEL (RAndomized study with the sirolimus-eluting VElocity balloon expandable stent in the treatment of patients with de novo native coronary artery Lesions) trial. Circulation. 2002;106(7):798–803. doi:10.1161/01.CIR.0000025585.63486.59
26. Matsuzawa Y, Kwon TG, Lennon RJ, et al. Prognostic value of flow-mediated vasodilation in brachial artery and fingertip artery for cardiovascular events: a systematic review and meta-analysis. J Am Heart Assoc. 2018;7(6):e008870. doi:10.1161/JAHA.118.008870
27. Dai Y, Xu M, Wang Y, et al. Impaired brachial artery flow-mediated dilation predicts restenosis risk in patients with coronary artery disease treated with drug-eluting stents. Coronary Artery Dis. 2019;30(2):112–119.
28. Dhillon R, Gosling RC, Dashwood AM, et al. Assessment of endothelial function predicts long-term cardiovascular events after percutaneous coronary intervention. J Am Heart Assoc. 2020;9(4):e014675.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.