Back to Journals » Neuropsychiatric Disease and Treatment » Volume 20
Predicting Communication Skills Outcomes for Preschool Children with Autism Spectrum Disorder Following Early Intervention
Authors Kauley N, John JR , Barr KR, Wu WT , Grove R, Masi A, Eapen V
Received 16 August 2023
Accepted for publication 25 December 2023
Published 8 January 2024 Volume 2024:20 Pages 35—48
DOI https://doi.org/10.2147/NDT.S435740
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Nadine Kauley,1,* James Rufus John,1,2,* Karlen R Barr,3 Weng Tong Wu,1 Rachel Grove,4 Anne Masi,1 Valsamma Eapen1– 3
1School of Clinical Medicine, University of New South Wales, Sydney, NSW, Australia; 2Ingham Institute of Applied Medical Research, Liverpool, NSW, Australia; 3South Western Sydney Local Health District, Liverpool, NSW, Australia; 4School of Public Health, University of Technology Sydney, Sydney, NSW, Australia
*These authors contributed equally to this work
Correspondence: Valsamma Eapen, ICAMHS, L1 MHC, Liverpool Hospital, Elizabeth Street, Liverpool, NSW, 2170, Australia, Tel +61 2 96164205, Email [email protected]
Purpose: This study aims to assess changes in the receptive and expressive language skills and to determine if the baseline characteristics such as communication, cognitive and motor skills, predict outcomes in preschool children with Autism Spectrum Disorder (ASD) following early intervention.
Methods: We recruited 64 children participating in the Early Start Denver Model (ESDM) early intervention program at an Autism Specific Early Learning and Care Center (ASELCC) in Australia. Baseline characteristics across various developmental domains was measured using the Mullen Scales of Early Learning (MSEL), Vineland Adaptive Behaviour Scales, 2nd Edition (VABS-II), and the ESDM Curriculum Checklist. Linear mixed-effects models were used to examine the effects of the intervention on outcomes. Fixed-effects such as time, groups (verbal and minimally verbal), and time-by-group interactions were assessed whilst adjusting for covariates. Further, multiple linear regression models were used to determine if the baseline characteristics were significant predictors of the outcomes following the early intervention.
Results: Among the 64 children who participated in this study, 38 children were verbal, whereas 26 were deemed to have minimal verbal skills. The mean age of the sample was 4.1 years with a significant male predilection (83%) and from a culturally and linguistically diverse (CALD) background (64%). Findings of the linear mixed effects model showed significant within and between group differences in the ESDM subscales, indicating higher magnitude of changes in the verbal group compared to the minimally verbal group. Finally, the multiple linear regression models suggested that baseline MSEL visual reception and expressive language scores were predictive of changes in the ESDM receptive and expressive communication scores.
Conclusion: Understanding a child’s baseline skill levels may provide valuable clues regarding what interventions would work best, or which interventions may be less suitable for individual preschool-aged children with ASD.
Keywords: autism, early intervention, learning skills, early childhood
Introduction
Autism Spectrum Disorder (ASD) is a complex and heterogeneous condition that influences how people interact with and experience the world.1 ASD can sometimes be accompanied by language delay,2,3 resulting in some children with ASD using a more effortful, explicit problem-solving approach in learning when compared to their typically developing peers.4 Significant progress has been made in ensuring earlier diagnosis and improving case identification of ASD over the last few decades.5–7 The rising prevalence of ASD detected in children is occurring at increasingly younger ages, which may be attributed to increased reporting, advocacy, and the growing knowledge base of both verbal and non-verbal manifestations of the condition.5,8,9 Recent research has also been motivated by the importance of starting interventions early enough to capitalize on the ample neural plasticity of infants and preschool-aged children.10,11 There has been substantial evidence to indicate the value of early intervention in improving outcomes for children with ASD.12–15 Early intervention may lay the foundation for development, leading to positive outcomes, allowing improved engagement and relationships with others, as well as increasing chances of realizing the full educational and employment potential.16
Intensive early intervention is of particular importance in children with ASD who are identified as being non- or minimally verbal. Difficulties with language development in children with ASD early in development have been shown to extend into the school-aged years.17,18 Recent literature describes minimally verbal children as having less than 30 functional words or unable to use speech alone to communicate.18 For children between the ages of 20 and 48 months, the criteria is reduced to 20 words.19 Minimally verbal children with ASD may also use echolalia, or word repetitions in speech, possibly leading to communication breakdowns, such as being misunderstood and not supported during social interactions.20,21 The majority of studies of early intervention in ASD focus on children with functional expressive language skills and higher intelligence quotient (IQ).22 As such, little is known about children with limited language skills. Classification is also challenging, as all children with ASD are different, and do not exhibit a single set of definitive characteristics, specific skills or challenges.16
Behavioural interventions, developmental interventions, technology-based interventions, cognitive-behavioral therapy, and naturalistic developmental behavioural interventions have shown positive effects for children with ASD, although no intervention is best for all children with ASD.23 The optimal amount of an intervention for children with ASD is dependent on various factors, including practicalities of a family’s situation, and the amount of time parents are able to implement therapeutic strategies at home.24 Several communication interventions exist for children with ASD, although more evidence is required regarding the ability of these interventions to improve verbal and nonverbal language.18 A recent meta-analysis showed that early behavioural interventions are effective for children with ASD across domains of adaptive behaviour, socialization, cognition, and communication.25 A child’s baseline developmental characteristics, such as cognitive and communication abilities, may predict whether they respond well to an intervention.7,26 The Early Start Denver Model (ESDM) is a comprehensive behavioural intervention using specific techniques to encourage joint attention and engagement between the facilitator and children during normal play.27,28 ESDM is generally delivered for up to 25 hours per week.29 Childcare workers and parents can also employ the techniques in their interactions with children with ASD as, once learned, these techniques can be adapted, translated, and generalized to suit environments familiar to the child, including childcare centers and the home. Evidence suggests that the ESDM can be efficacious in enhancing child outcomes such as cognitive skills and adaptive functioning30–33 while also improving maladaptive behaviours.34 Studies have also shown that these gains are maintained two years post-intervention, particularly in core ASD traits such as social and communication difficulties and restricted and repetitive behaviour that improved during this period.12 Children with ASD with lower symptom severity, higher adaptive functioning, and receptive language abilities prior to intervention have shown greater improvement in previous studies.35,36 However, there is limited research on the effectiveness of ESDM among minimally verbal preschool aged children.37
Further understanding is required regarding whether baseline characteristics in certain developmental areas are predictive of intervention effectiveness. To address this knowledge gap, this study has two main aims. First, the study will determine whether preschool aged children with ASD show improvement in receptive and expressive language, following ESDM intervention. Second, the study will determine if baseline characteristics across developmental domains will predict outcomes following ESDM intervention. The hypothesis is that children who have a higher level of language skills, both expressive and receptive prior to intervention, will have improved outcomes in these and other developmental domains after receiving the ESDM compared to children with a lower level of language skills. We also hypothesize that the characteristics that children exhibit at baseline will be predictive of the progress achieved when exiting the early intervention program. Findings of this study will determine if key characteristics in minimally verbal children with ASD predict greater language, and global developmental gains to ensure optimal outcomes from intensive early intervention programs.
Methods
Participants
Participants in this study were preschool aged children with a confirmed diagnosis of ASD, attending an Autism-Specific Early Learning and Care Center (ASELCC) in Australia. The center is one of the six ASELCCs established by the Australian Government within the setting of a long day child care center for children aged 2–6 years. Children having a DSM-IV-TR diagnosis of Autistic Disorder, made by a community-based physician, who enrolled in the ESDM early intervention program any time from its inception at the ASELCC in 2010 until 2016 were included. These children would all have met criteria for a DSM-5 diagnosis of ASD. Exclusion criteria included neurological (eg, uncontrolled epilepsy) disorders, and significant vision, hearing, motor, or physical impairment that prevented full participation in the intervention program.
A diagnosis of ASD was confirmed using Modules 1 or 2 of the Autism Diagnostic Observation Schedule – Second Edition (ADOS-2),38 conducted by researchers trained in administration of the assessment. Module 1 is used for assessing preverbal children who are yet to develop any spoken language, and Module 2 is for those who have a few spoken words. Children were separated into two groups, “Verbal” and “Minimally Verbal” based on their score in Question A1 (overall level of non-echoed spoken language) of the ADOS-2.39 Those scoring 0, 1 or 2 on Module 1 of the ADOS, or 0 or 1 on Module 2 were classed as “Verbal”, while those who scored 3 or 4 on Module 1, or 2 or 3 on Module 2 were classified as “Minimally Verbal”.
The total sample of 64 children consisted of 38 children in the “verbal” group and 26 children in the “minimally verbal” group. The sociodemographic characteristics of the participants are shown in Table 1. The mean (±SD) age of the sample at entry to the intervention was 4.1 (±0.6) years with a significant male predilection with 53 males (83%) and 11 females (17%). More than half of the children (64%) came from a culturally and linguistically diverse (CALD) background based on language spoken at home. The remaining primary characteristics were mostly proportionate between the verbal and minimally verbal groups, except for gender and a diagnosis of developmental delay. The verbal group were 92% male and 9% female, while the minimally verbal were 69% male and 31% female. In the verbal group, only 7 (18%) children were diagnosed with a global developmental delay as well as autism whereas the minimally verbal group had 11 children (42%) with a global developmental delay (Table 1).
 |
Table 1 Sociodemographic Characteristics of the Participants (Overall and by Groups) |
Procedure
This study was a retrospective analysis of pre- and post-intervention data. Data were collected at two time points: at participant entry into the ESDM program and again when participants exited from the program.
The average time in the intervention was similar across the two groups, with the total mean (±SD) duration of 15.1 (±6.3) months. The shortest and longest times spent in the intervention were 4 and 29 months, respectively. The proportion of children in either group who were participating in other interventions while also participating in the ESDM program was also similar (Table 2). Forty-seven children in total were participating in or receiving other interventions.
 |
Table 2 Details of the Intervention Across Groups |
Data Collection
Several measures were used to assess the children in this study, including the ESDM Curriculum Checklist for Young Children with Autism, Mullen Scales of Early Learning (MSEL) and the Vineland Adaptive Behaviour Scales (VABS). Parents were also asked to complete the ASELCC History Taking form that asked for demographic information.
ESDM Curriculum Checklist for Young Children with Autism
The ESDM Curriculum Checklist is a set of specific objectives categorized under various developmental domains such as expressive and receptive language, joint attention, imitation, cognition, play and social skills, and fine and gross motor skills, that allow the assessment of young children with ASD participating in the ESDM program.28 It also facilitates the development of individualized learning goals for each child to achieve which is continually updated as per progress being made. In this study, childcare workers trained in the delivery of the ESDM provided the intervention to the children while at the Autism Specific Early Learning and Care Center (ASELCC). The program was intensive, with both one-on-one and group teaching occurring over periods ranging from 2 to 24 months in duration. The checklist was administered every 12 weeks by the ASELCC staff delivering the intervention to the children. For the purposes of this study, change scores of the ESDM subscales of Receptive Communication, Expressive Communication, and Social Skills were used as the outcome variables of interest.
Mullen Scales of Early Learning
The Mullen Scales of Early Learning (MSEL) are a standardized assessment evaluating childhood development at any time from birth to 68 months.40 The measure is separated into four subscales, each assessing a child’s skill level in different developmental domains, including visual reception, receptive and expressive language, and fine motor abilities. The measure allows raw totals from each subscale to be converted to age equivalent scores that indicate at what stage of development a child is compared to a typically developing child. For the purposes of this study, the first three subscales such as visual reception, receptive language, and expressive language were used in the analysis. High reliability of the MSEL is shown through a test–retest reliability of 0.80 after two weeks. The MSEL also demonstrates good convergent validity with the Differential Ability Scales in the verbal and nonverbal domains.41
Vineland Adaptive Behaviour Scales
The Vineland Adaptive Behaviour Scales second edition (VABS-II) is a semi-structured interview used to measure adaptive behaviour, which also includes a parent and teacher rating form.42 In this study, the parent-completed questionnaire was used, assessing their child’s ability in multiple developmental areas, such as communication, daily living skills, social skills and relationships, and motor function. A higher score on these subscales indicates a higher level of endorsed ability in this domain. The questionnaire also asks how often their child exhibits problem (maladaptive) behaviours, where the higher the score, the more frequent the occurrence of maladaptive behaviours in the child. For the purposes of this study, the maladaptive behaviour scores were used in the analysis as a key predictor. In a sample of preschool children, excellent internal consistency of the VABS-II was found with Cronbach’s alpha ranging from 0.82 to 0.95 across the scales.43 Excellent concurrent validity is shown with high correlations with the Adaptive Behaviour Scale- School Edition ranging from 0.77 to 0.85.44
ASELCC History Taking Form
Parents or carers of all children attending the ASELCC were required to complete this form as part of the service. Information regarding their child or children, their diagnosis of ASD, and the ASD traits and behaviours they display were recorded. The form also collected key sociodemographic information of the child and parents. Child’s characteristics included age, gender of the child, culturally and linguistically diverse (CALD) background status, birth order, and diagnosis of developmental disorder whereas parents’ characteristics included age, primary carer education, and family annual income.
Data Analysis
Data used for analysis was extracted from the MSEL, VABS-II, and ESDM Curriculum Checklist assessments performed at baseline (just prior to intervention entry) and at exit.
Firstly, to identify significant differences in the sociodemographic characteristics, intervention details, and assessment scores of the MSEL and VABS subscales between the verbal and minimally verbal groups at baseline, we used independent samples t-tests and Pearson’s chi-squared tests or Fisher’s exact tests for continuous and categorical variables, respectively. Secondly, an intention-to-treat (ITT) linear mixed effects model with Bonferroni correction for multiple corrections was used to examine the effects of the intervention on ESDM subscales. Linear mixed-effect models can effectively account for within-subject correlations and handle unbalanced data, making them well-suited for analysing data with missing values. Fixed effects such as time, group, and time by group interaction were also assessed separately for each outcome variable whilst adjusting for sociodemographic covariates. Significant effects were followed up with pairwise contrasts comparing group differences in pre-to-post and pre-to-follow-up total scores. Finally, we used a multiple linear regression analysis to determine if the baseline characteristics such as communication, cognitive and motor skills, predict changes in the ESDM subscale scores following intervention. Adjusted R2 values were checked for the performance of the models as an equivalent measure of ROC. The significance level was set as 0.05, and all statistical tests were two sided. All analyses were undertaken in Statistical Package for the Social Sciences (SPSS) version 28 (IBM SPSS, IBM Corp., Armonk, NY, USA) and R studio version 4.1.2.
Results
Effectiveness of the Intervention
Changes in the ESDM, MSEL, and VABS Subscales
A comparison of mean scores of the clinical assessments between the verbal and minimally verbal groups at baseline and exit is shown in Table 3. Findings of the analysis showed significant within group (between entry and exit) and between group differences in mean scores for ESDM subscales of receptive communication, expressive communication, and social skills. The between group differences suggest a higher magnitude of improvement in all the ESDM subscales in the verbal group compared to the minimally verbal group (Table 3 and Figure 1).
 |
Table 3 Comparison of Mean Scores of Clinical Assessments Between the Verbal and Minimally Verbal Groups at Baseline and Exit |
There was also a significant within group and between group differences in the MSEL visual reception, receptive language, and expressive language scores. Similar to the ESDM subscales, a higher magnitude of improvement is seen in all the MSEL subscales in the verbal group compared to the minimally verbal group. However, no significant changes were noted in the VABS maladaptive behavioural scores. Further, changes in the MSEL subdomains and VABS maladaptive behavioural scores are graphically presented as Figure 2.
Findings of the Linear Mixed Effects Model
The results of the linear mixed-effects models for the ESDM subscales are presented in Table 4. The mixed-effects model showed significant within group differences in the ESDM receptive communication (t=8.74, p<0.001), expressive communication (t=8.99, p<0.001), and social skills scores (t=7.57, p<0.001) as indicated by the significant effect of time. Further, the models also showed significant effect of group differences for expressive communication (t=−0.57, p=0.038) and social skills scores (t=−0.151, p=0.050) but not for receptive communication scores. There were also significant interactions between time and group for all three subscales. Consistently, posthoc pairwise comparisons also showed significant differences in group and time for ESDM expressive communication and social skills scores but only significant differences over time for receptive communication scores (Supplementary Table 1).
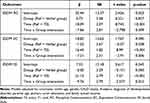 |
Table 4 Linear Mixed-Effects Models |
Predicting Outcomes Post-Intervention
The ESDM Curriculum Checklist subscale scores at Time 2 were subtracted from scores at Time 1 to determine overall change in each developmental area (change scores). These figures were applied in a multiple linear regression model to determine whether change scores could be predicted from baseline characteristics whilst adjusting for key sociodemographic covariates (Table 5). The results of the regression analyses indicated that MSEL visual reception scores on entry was a significant predictor and was negatively associated with the ESDM receptive communication change scores (B −0.50, 95% CI −0.85, −0.15), meaning lower MSEL visual reception scores at entry was associated with higher magnitude of improvement in the receptive communication following the intervention. Further, baseline MSEL receptive language scores was also a significant predictor and was positively associated with the ESDM receptive communication and expressive communication change scores meaning higher MSEL receptive language scores at entry was associated with higher magnitude of improvement in the ESDM receptive communication and expressive communication following the intervention. No significant associations were found between the social skills change score and MSEL variables. In terms of key sociodemographic variables, age at enrolment was a key predictor where younger children showed higher magnitude of improvement in ESDM receptive communication and expressive communication following the intervention.
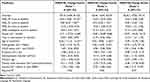 |
Table 5 Multiple Linear Regression Analysis |
Discussion
The primary aim of this study was to determine whether preschool aged children with ASD improved their skills in receptive and expressive language after attending an ASD-specific learning center and participating in an ESDM intervention program. The verbal and minimally verbal groups showed significant improvements across the three developmental domains in the MSEL of visual reception, receptive communication, and expressive communication, and in the ESDM subscales of receptive communication, expressive communication, and social skills over time. Moreover, significantly greater magnitude of improvement in these domains was seen in the verbal group compared with the minimally verbal group. In addition, findings of the regression analyses showed baseline MSEL visual reception scores were associated with greater improvement in ESDM receptive communication following the intervention. Additionally, baseline MSEL receptive language scores as well as sociodemographic factor such as younger age at enrolment were related to greater improvement in ESDM receptive and expressive communication after the intervention.
Findings of this study are consistent with previous research showing improvements in children with ASD’s social communication and expressive language skills following ESDM intervention.15,31,35,45 Previous research shows that verbal children may have better language and communication skills, including receptive language, compared with minimally verbal children.46 Therefore, it is perhaps unsurprising that verbal children in this study improved on social skills and receptive and expressive communication skills to a greater degree than minimally verbal children. Minimally verbal children on the other hand may encounter more barriers to improving their communication compared with verbal children, such as difficulties with visual processing and atypical auditory behaviours that impact their linguistic abilities.47,48 In this regard, it is interesting to note that those with lower visual reception score at baseline were able to gain maximum benefit from the intervention as there was possibly more room for improvement. This coupled with the finding that better baseline language skills of receptive and expressive communication and younger age at entry predicted better intervention outcome seems to suggest that early intensive interventions focused on strengthening skills in the visual reception area can help children reach their maximum potential.
More recent developments in interventions for ASD have looked at the possibility of baseline characteristics, including cognitive and language abilities, being used to determine how they will perform on a specific intervention.7,26,35,36,49,50 Further, it has been shown that specific baseline characteristics such as social affect and play skills predict better outcomes following intervention such as ESDM as these children are much more likely to engage in sensory social routines and related relational elements that are characteristic of the ESDM program.51 This can guide practitioners in directing parents and guardians towards interventions that their children are most likely to benefit from, or conversely, that are unlikely to result in any positive outcome.52 Treatment guidelines for children with ASD could incorporate pre-treatment characteristics to help practitioners provide timely strengths-based, person-centered interventions.53,54 Providing intervention options based on a child’s current level of functioning could help to ensure that the right support is provided, resulting in a potential reduction of wasted emotional and financial resources.55,56 In this study, the ESDM Curriculum Checklist proved useful in investigating baseline characteristics, as its objectives specifically assess abilities that a child should ideally have after participating in the ESDM program. This allowed us to determine the difference between the ESDM Curriculum Checklist scores of each child from exit to entry, and thus the overall change seen across developmental domains, including visual reception, and receptive and expressive language.
According to our results, level of skills in visual reception and receptive language at entry, along with age at enrolment can successfully be used to predict the improvements that children will make in receptive communication by the end of their time in the ESDM program. Age and capacity for receptive language at baseline may also predict the improvements children will make in expressive language skills. This aligns with previous research on the ESDM program that shows a child’s baseline verbal developmental quotient at 18 to 48 months significantly predicts school-age verbal cognition.57 Research investigating the active ingredients in the ESDM intervention relating to language skills may help in understanding how they interact with the characteristics of the child to produce positive outcomes.55 Further, improving valid measurement of communication skills in children with ASD may improve identification and early intervention regarding language skills, including use of naturalistic approaches.58 For minimally verbal children, incorporating parental education may be an important way to improve uptake of interventions, including training parents to work on these skills in the home.59 As previously identified in the literature, children with ASD may benefit more from interventions if they begin at a younger age, although more needs to be understood regarding the interactions between predictor variables.60–62 The finding of younger age predicting greater improvements following intervention also highlights the importance of continuing research on expressive and receptive communication in ASD in preschool children. Other factors including cognition, prelinguistic communication skills, and comorbidities may also predict spoken language outcomes for preschool aged children with minimally verbal language.63 Asta and Persico (2022) proposed that a child with ASD’s social communication characteristics could be used to determine outcomes on the ESDM.36 We did not reach the same conclusion, with MSEL expressive language scores on entry showing no significant predictive values for receptive or expressive communication, or social skills change scores on the ESDM Curriculum Checklist. A possible explanation for this is that there were no exclusion criteria for children involved in the study, such as medical conditions, compared with previous intervention studies which may not replicate real-world clinical services.55
Limitations
The ADOS-2 was used to divide the children into the two groups, verbal and minimally verbal. This assessment was administered by an independent assessor who is trained to research reliability.39 However, different staff, including psychologists, research fellows, and research assistants performed the pre and post assessment of children while at the ASELCC over the study period. As the assessment was not carried out by the same individuals for each child, the degree of inter-rater reliability is unknown. Furthermore, as an unfamiliar person assessed the children, they may not have as readily showcased their verbal abilities, as they may have around family or ASELCC staff they are more familiar with.
An additional consideration that question the validity of studies involving preschool-aged autistic children is that the verbal skills as assessed using standardized measures may not necessarily capture their “pre-verbal” skills. The term refers to children who will eventually learn to use spoken language though do not yet exhibit it.19,64,65 Consequently, the question remains as to whether, due to their age, these children are rated as non-verbal or preverbal on assessment. A systematic review further reported that assessing the improvement in language over time by raw scores may not be possible.66 Being mindful of age being a confounder and aiming to reduce this effect, this study only used age equivalent data from the MSEL in our analysis.
Further, the lack of a control group consisting of typically developing preschool children who had also undergone the intervention may have provided more information in terms of the degree to which the autistic children improved. Future research could reproduce this study with a larger, more diverse sample that is more representative of the young autistic population, and a control group of typically developing children to allow for comparisons to be investigated.
About 73% of children were also participating in other interventions during the period of ESDM delivery, so we cannot be certain whether the improvements noted are due to the effects of the ESDM alone. One other factor that could not be corrected for was the large loss of results at entry, especially in the VABS-II assessment. We believe that this was largely due to it being a parent-completed questionnaire, with parents having many other stressors in their lives preventing them from completing it. As the VABS-II is a questionnaire filled out by parents, it is possible that there is the impact of parental perception introducing an element of bias and that scores in the language subscales would not be entirely representative of a child’s actual skill level. For example, parents may misinterpret echolalia as functional expressive language. For these reasons, we did not include it as a measure for the entire sample. However, we did see the merit of having parental perspectives in our study, so some analysis was still completed on the children who had entry and exit data for the VABS-II test.
Conclusion
The current study found that baseline skills in visual reception, receptive language, and expressive language are predictive of receptive communication gains following ESDM intervention. Understanding a child’s baseline characteristics may provide valuable clues regarding what interventions would work best, or which interventions may be less suitable for individual preschool aged children with ASD. However, there is limited research evidence available on minimally verbal children with a significant unmet need to guide clinicians on choosing the right intervention. A better understanding of “what would work for whom and why” and what baseline characteristics are critical in predicting outcomes should form important considerations for practice and policy makers and this should ideally include not only the verbal skills but preverbal skills and prelinguistic vocal behaviours.
Abbreviations
ADOS-2, Autism Diagnostic Observation Schedule – Second Edition; ASD, Autism Spectrum Disorder; ASELCC, Autism Specific Early Learning and Care Center; CALD, culturally and linguistically diverse; ESDM, Early Start Denver Model; IQ, intelligence quotient; MANOVA, multivariate analysis of variance; MSEL, Mullen Scales of Early Learning; and VABS-II - Vineland Adaptive Behaviour Scales, 2nd Edition.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available due to their sensitive nature. However, aggregate data may be available from the corresponding author upon reasonable request.
Ethical Approval and Informed Consent
The study was granted ethical approval by the University of New South Wales Human Research Ethics Committee (HREC) HC14267 and was conducted in accordance with the principles outlined in the Helsinki Declaration. All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from the legal guardian(s) of all participants that enrolled in early intensive intervention programs at the Autism Specific Early Learning and Care Center (ASELCC).
Acknowledgments
The authors would like to acknowledge the contributions of the families and staff in the KU Marcia Burgess Autism Specific Early Learning and Care Center (KU Children’s Services), South West Sydney, and Ms Elizabeth Aylward in NSW who have contributed to the research program. The authors also acknowledge the financial support of the Cooperative Research Center for Living with Autism (Autism CRC), established and supported under the Australian Government’s Cooperative Research Centers Program. Additionally, they acknowledge access to the Child and Family Outcome Study data collected from children and families attending the ASELCC established through funding from the Australian Government’s Department of Social Services and Autism Co-operative Research Center.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors acknowledge the financial support of the Cooperative Research Center for Living with Autism (Autism CRC), established and supported under the Australian Government’s Cooperative Research Centers Program.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Masi A, DeMayo MM, Glozier N, Guastella AJ. An overview of autism spectrum disorder, heterogeneity and treatment options. Neurosci Bull. 2017;33(2):183–193. doi:10.1007/s12264-017-0100-y
2. Wilson RB. Improving awareness, identification, and treatment of motor impairments in Autism. Pediatrics. 2022;149(Supplement 4). doi:10.1542/peds.2020-049437K
3. Demopoulos C, Hopkins J, Lewine JD. Relations between nonverbal and verbal social cognitive skills and complex social behavior in children and adolescents with autism. J Abnormal Child Psychol. 2016;44(5):913–921. doi:10.1007/s10802-015-0082-z
4. Bo J, Lee C-M, Colbert A, Shen B. Do children with autism spectrum disorders have motor learning difficulties? Res Autism Spectrum Disord. 2016;23:50–62. doi:10.1016/j.rasd.2015.12.001
5. Hansen SN, Schendel DE, Parner ET. Explaining the increase in the prevalence of Autism spectrum disorders: the proportion attributable to changes in reporting practices. JAMA Pediatrics. 2015;169(1):56–62. doi:10.1001/jamapediatrics.2014.1893
6. Russell G, Collishaw S, Golding J, Kelly SE, Ford T. Changes in diagnosis rates and behavioural traits of autism spectrum disorder over time. BJPsych Open. 2015;1(2):110–115. doi:10.1192/bjpo.bp.115.000976
7. Albahri A, Hamid RA, Zaidan A, Albahri O. Early automated prediction model for the diagnosis and detection of children with autism spectrum disorders based on effective sociodemographic and family characteristic features. Neural Comput Appl. 2023;35(1):921–947. doi:10.1007/s00521-022-07822-0
8. Brian JA, Bryson SE, Zwaigenbaum L. Autism spectrum disorder in infancy: developmental considerations in treatment targets. Curr Opinion Neurol. 2015;28(2):117–123. doi:10.1097/WCO.0000000000000182
9. Russell G, Stapley S, Newlove-Delgado T, et al. Time trends in autism diagnosis over 20 years: a UK population-based cohort study. J Child Psychol Psychiatry. 2022;63(6):674–682. doi:10.1111/jcpp.13505
10. Cioni G, Inguaggiato E, Sgandurra G. Early intervention in neurodevelopmental disorders: underlying neural mechanisms. Dev Med Child Neurol. 2016;58(S4):61–66. doi:10.1111/dmcn.13050
11. French L, Kennedy EM. Annual research review: early intervention for infants and young children with, or at‐risk of, autism spectrum disorder: a systematic review. J Child Psychol Psychiatry. 2018;59(4):444–456. doi:10.1111/jcpp.12828
12. Estes A, Munson J, Rogers SJ, Greenson J, Winter J, Dawson G. Long-term outcomes of early intervention in 6-year-old children with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2015;54(7):580–587. doi:10.1016/j.jaac.2015.04.005
13. Eisenhower A, Martinez Pedraza F, Sheldrick RC, et al. Multi-stage screening in early intervention: a critical strategy for improving ASD identification and addressing disparities. J Autism Develop Disorder. 2021;51(3):868–883. doi:10.1007/s10803-020-04429-z
14. Bieleninik Ł, Posserud M-B, Geretsegger M, Thompson G, Elefant C, Gold C. Tracing the temporal stability of autism spectrum diagnosis and severity as measured by the Autism diagnostic observation schedule: a systematic review and meta-analysis. PLoS One. 2017;12(9):e0183160. doi:10.1371/journal.pone.0183160
15. Vivanti G, Dissanayake C, Team VA. Outcome for children receiving the Early Start Denver Model before and after 48 months. J Autism Develop Disorder. 2016;46(7):2441–2449. doi:10.1007/s10803-016-2777-6
16. Elder JH, Kreider CM, Brasher SN, Ansell M. Clinical impact of early diagnosis of autism on the prognosis and parent-child relationships. Psychol Res Behav Manage. 2017;10:283–292. doi:10.2147/PRBM.S117499
17. Haebig E, Saffran JR, Ellis Weismer S. Statistical word learning in children with autism spectrum disorder and specific language impairment. J Child Psychol Psychiatry. 2017;58(11):1251–1263. doi:10.1111/jcpp.12734
18. Brignell A, Chenausky KV, Song H, Zhu J, Suo C, Morgan AT. Communication interventions for autism spectrum disorder in minimally verbal children. Cochrane Database Syst Rev. 2018;2018(11). doi:10.1002/14651858.CD012324.pub2
19. Haebig E, Jiménez E, Cox CR, Hills TT. Characterizing the early vocabulary profiles of preverbal and minimally verbal children with autism spectrum disorder. Autism. 2021;25(4):958–970. doi:10.1177/1362361320973799
20. Neely L, Gerow S, Rispoli M, Lang R, Pullen N. Treatment of echolalia in individuals with autism spectrum disorder: a systematic review. Rev J Autism Develop Disorder. 2016;3(1):82–91. doi:10.1007/s40489-015-0067-4
21. Trembath D, Westerveld MF, Teppala S, et al. Profiles of vocalization change in children with autism receiving early intervention. Autism Res. 2019;12(5):830–842. doi:10.1002/aur.2075
22. Soorya LV, Siper PM, Beck T, et al. Randomized comparative trial of a social cognitive skills group for children with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2015;54(3):208–216. e201. doi:10.1016/j.jaac.2014.12.005
23. Trembath D, Varcin K, Waddington H, et al. Non-pharmacological interventions for autistic children: an umbrella review. Autism. 2022;27(2):275–295. doi:10.1177/13623613221119368
24. Trembath D, Waddington H, Sulek R, et al. An evidence-based framework for determining the optimal amount of intervention for autistic children. Lancet Child Adolesc Health. 2021;5(12):896–904. doi:10.1016/S2352-4642(21)00285-6
25. Wergeland GJH, Posserud M-B, Fjermestad K, Njardvik U, Öst L-G. Early behavioral interventions for children and adolescents with autism spectrum disorder in routine clinical care: a systematic review and meta-analysis. Clin Psychol. 2022;29(4):400–414.
26. Fossum KL, Williams L, Garon N, Bryson SE, Smith IM. Pivotal response treatment for preschoolers with autism spectrum disorder: defining a predictor profile. Autism Res. 2018;11(1):153–165. doi:10.1002/aur.1859
27. Rogers SJ, Dawson G. Early Start Denver Model for Young Children with Autism: Promoting Language, Learning, and Engagement. Guilford Publications; 2010.
28. Rogers SJ, Dawson G. Early Start Denver Model Curriculum Checklist for Young Children with Autism. Guilford Press; 2009.
29. Tupou J, Waddington H, van der Meer L, Sigafoos J. Effects of a low-intensity Early Start Denver Model-based intervention delivered in an inclusive preschool setting. Int J Develop Disabil. 2022;68(2):107–121. doi:10.1080/20473869.2019.1707434
30. Zitter A, Rinn H, Szapuova Z, et al. Does treatment fidelity of the early start Denver model impact skill acquisition in young children with autism? J Autism Develop Disorder. 2021;1:1–11.
31. Baril EM, Humphreys BP. An evaluation of the research evidence on the Early Start Denver Model. Journal of Early Intervention. 2017;39(4):321–338. doi:10.1177/1053815117722618
32. Shi B, Wu W, Dai M, et al. Cognitive, language, and behavioral outcomes in children with autism spectrum disorders exposed to early comprehensive treatment models: a meta-analysis and meta-regression. Frontiers in Psychiatry. 2021;12:691148. doi:10.3389/fpsyt.2021.691148
33. Eapen V, Crncec R, Walter A. Clinical outcomes of an early intervention program for preschool children with Autism spectrum disorder in a group setting. BMC Paediatr. 2013;13(1):1–9. doi:10.1186/1471-2431-13-3
34. Fulton E, Eapen V, Crnčec R, Walter A, Rogers S. Reducing maladaptive behaviors in preschool-aged children with autism spectrum disorder using the early start Denver model. Front Pediatr. 2014;2:40. doi:10.3389/fped.2014.00040
35. Sinai-Gavrilov Y, Gev T, Mor-Snir I, Vivanti G, Golan O. Integrating the Early Start Denver Model into Israeli community autism spectrum disorder preschools: effectiveness and treatment response predictors. Autism. 2020;24(8):2081–2093. doi:10.1177/1362361320934221
36. Asta L, Persico AM. Differential predictors of response to early start Denver model vs. early intensive behavioral intervention in young children with Autism spectrum disorder: a systematic review and meta-analysis. Brain Sci. 2022;12(11):1499. doi:10.3390/brainsci12111499
37. Koegel LK, Bryan KM, Su PL, Vaidya M, Camarata S. Definitions of nonverbal and minimally verbal in research for autism: a systematic review of the literature. J Autism Develop Disorder. 2020;50(8):2957–2972. doi:10.1007/s10803-020-04402-w
38. Hus V, Lord C. (ADOS®-2) Autism Diagnostic Observation Schedule™.
39. Lord C, Rutter M, DiLavore P, Risi S, Gotham K, Bishop S. Autism Diagnostic Observation Schedule: ADOS-2 west Western Psychological Services. Los Angeles, CA: Western Psychological Services; 2002.
40. Mullen EM. Mullen Scales of Early Learning. Minneapolis: Pearson; 1995.
41. Bishop SL, Guthrie W, Coffing M, Lord C. Convergent validity of the Mullen Scales of Early Learning and the differential ability scales in children with autism spectrum disorders. Am J Intellect Dev Disabil. 2011;116(5):331–343. doi:10.1352/1944-7558-116.5.331
42. Sparrow S, Cicchetti D, Balla D. Vineland adaptive behavior scales II. Circle Pines. MN: American Guidance Service; 2005.
43. Goldberg MR, Dill CA, Shin JY, Nhan NV. Reliability and validity of the Vietnamese Vineland Adaptive Behavior Scales with preschool-age children. Res Dev Disabil. 2009;30(3):592–602. doi:10.1016/j.ridd.2008.09.001
44. Perry A, Factor DC. Psychometric validity and clinical usefulness of the vineland adaptive behavior scales and the AAMD adaptive behavior scale for an autistic sample. J Autism Dev Disord. 1989;19(1):41–55. doi:10.1007/BF02212717
45. Holzinger D, Laister D, Vivanti G, Barbaresi WJ, Fellinger J. Feasibility and outcomes of the Early Start Denver Model implemented with low intensity in a community setting in Austria. J Dev Behav Pediatr. 2019;40(5):354–363. doi:10.1097/DBP.0000000000000675
46. Plesa Skwerer D, Brukilacchio B, Chu A, Eggleston B, Meyer S, Tager-Flusberg H. Do minimally verbal and verbally fluent individuals with autism spectrum disorder differ in their viewing patterns of dynamic social scenes? Autism. 2019;23(8):2131–2144. doi:10.1177/1362361319845563
47. Ortiz-Mantilla S, Cantiani C, Shafer VL, Benasich AA. Minimally-verbal children with autism show deficits in theta and gamma oscillations during processing of semantically-related visual information. Sci Rep. 2019;9(1):5072. doi:10.1038/s41598-019-41511-8
48. Schwartz S, Wang L, Shinn-Cunningham BG, Tager-Flusberg H. Atypical perception of sounds in minimally and low verbal children and adolescents with autism as revealed by behavioral and neural measures. Autism Res. 2020;13(10):1718–1729. doi:10.1002/aur.2363
49. Solish A, Klemencic N, Ritzema A, et al. Effectiveness of a modified group cognitive behavioral therapy program for anxiety in children with ASD delivered in a community context. Molecular Autism. 2020;11(1):1–11. doi:10.1186/s13229-020-00341-6
50. Smith IM, Flanagan HE, Garon N, Bryson SE. Effectiveness of community-based early intervention based on pivotal response treatment. J Autism Develop Disorder. 2015;45(6):1858–1872. doi:10.1007/s10803-014-2345-x
51. Eapen V, Crncec R, Walker A. There are gains, but can we tell for whom and why? Predictors of treatment response following group early start Denver model Intervention in preschool - aged children with autism spectrum disorder. Autism Open Access. 2016;6:1.
52. Stahmer AC, Schreibman L, Cunningham AB. Toward a technology of treatment individualization for young children with autism spectrum disorders. Brain Res. 2011;1380:229–239. doi:10.1016/j.brainres.2010.09.043
53. Trembath D, Varcin K, Waddington H, et al. National Guideline for Supporting the Learning, Participation, and Wellbeing of Autistic Children and Their Families in Australia. Brisbane: Autism CRC; 2022.
54. Fuentes J, Hervás A, Howlin P. ESCAP practice guidance for autism: a summary of evidence-based recommendations for diagnosis and treatment. Eur Child Adolesc Psychiatry. 2021;30(6):961–984. doi:10.1007/s00787-020-01587-4
55. Vivanti G, Prior M, Williams K, Dissanayake C. Predictors of outcomes in autism early intervention: why don’t we know more? Front Pediatr. 2014;2:2. doi:10.3389/fped.2014.00002
56. Bremer E, Lloyd M. Baseline behaviour moderates movement skill intervention outcomes among young children with autism spectrum disorder. Autism. 2021;25(7):2025–2033. doi:10.1177/13623613211009347
57. Clark M, Vinen Z, Vivanti G, Dissanayake C. Prediction of school-age outcomes for autistic children following receipt of group-early start Denver model. Res Autism Spectr Disord. 2023;104:102164. doi:10.1016/j.rasd.2023.102164
58. Trembath D, Paynter J, Sutherland R, Tager-Flusberg H. Assessing communication in children with autism spectrum disorder who are minimally verbal. Curr Dev Disord Rep. 2019;6(3):103–110. doi:10.1007/s40474-019-00171-z
59. Koegel LK, Bryan KM, Su PL, Vaidya M, Camarata S. Parent education in studies with nonverbal and minimally verbal participants with autism spectrum disorder: a systematic review. Am J Speech Lang Pathol. 2020;29(2):890–902. doi:10.1044/2019_AJSLP-19-00007
60. Towle PO, Patrick PA, Ridgard T, Pham S, Marrus J. Is Earlier Better? The relationship between age when starting early intervention and outcomes for children with Autism spectrum disorder: a selective review. Autism Res Treat. 2020;2020:7605876. doi:10.1155/2020/7605876
61. Maksimović S, Marisavljević M, Stanojević N, et al. Importance of early intervention in reducing autistic symptoms and speech-language deficits in children with autism spectrum disorder. Children. 2023;10(1):1. doi:10.3390/children10010122
62. Trembath D, Stainer M, Caithness T, et al. Spoken language change in children on the autism spectrum receiving community-based interventions. J Autism Dev Disord. 2023;53(6):2232–2245. doi:10.1007/s10803-022-05511-4
63. Trembath D, Sutherland R, Caithness T, et al. Clinician proposed predictors of spoken language outcomes for minimally verbal children with autism spectrum disorder. J Autism Dev Disord. 2021;51(2):564–575. doi:10.1007/s10803-020-04550-z
64. Oosting DR, Howard MS, Carter AS. Reciprocal associations between language ability and social functioning development in pre-verbal autistic children. J Autism Develop Disorder. 2023;1:1–13.
65. McDaniel J, Yoder P, Woynaroski T, Watson LR. Predicting receptive-expressive vocabulary discrepancies in preschool children with autism spectrum disorder. J Speech Lang Hear Res. 2018;61(6):1426–1439. doi:10.1044/2018_JSLHR-L-17-0101
66. Brignell A, Morgan AT, Woolfenden S, et al. A systematic review and meta-analysis of the prognosis of language outcomes for individuals with autism spectrum disorder. Autism Develop Lang Impair. 2018;3:2396941518767610. doi:10.1177/2396941518767610
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


