Back to Journals » Journal of Pain Research » Volume 14
Predictability of Fused 3D-T2-SPACE and 3D-TOF-MRA Images in Identifying Conflict in Trigeminal Neuralgia
Authors Pham HD, Dang TH , Duong TK, Dinh TT , Bui VG, Nguyen TV, Huynh QH
Received 25 July 2021
Accepted for publication 22 October 2021
Published 1 November 2021 Volume 2021:14 Pages 3421—3428
DOI https://doi.org/10.2147/JPR.S331054
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor E Alfonso Romero-Sandoval
Hong Duc Pham,1,2 Thu Ha Dang,1,2 Trung Kien Duong,3 Trung Thanh Dinh,1 Van Giang Bui,2,4 Tuan Vu Nguyen,5 Quang Huy Huynh6,7
1Radiology Department, Saint Paul Hospital of Hanoi, Hanoi City, Vietnam; 2Radiology Department, Hanoi Medical University, Hanoi City, Vietnam; 3Neurosurgery Department, Saint Paul Hospital of Hanoi, Hanoi City, Vietnam; 4Radiology Centre, National Cancer Hospital, Hanoi City, Vietnam; 5Cardiology Department, Pham Ngoc Thach University of Medicine, Ho Chi Minh City, Vietnam; 6Radiology Department, Pham Ngoc Thach University of Medicine, Ho Chi Minh City, Vietnam; 7Radiology Department, Trưng Vương Hospital, Ho Chi Minh City, Vietnam
Correspondence: Tuan Vu Nguyen
Cardiology Department, Pham Ngoc Thach University of Medicine, 2 Duong Quang Trung Street, Ho Chi Minh City, Vietnam
Tel +84903627477
Email [email protected]
Purpose: To evaluate the efficacy of fused three-dimensional T2 sampling perfection with application-optimized contrasts using different flip-angle evolutions (3D-SPACE) and three-dimensional time-of-flight magnetic resonance angiography (3D-TOF-MRA) sequences for detecting neurovascular compression (NVC) in patients presenting with trigeminal neuralgia (TN).
Methods: A prospective study was carried in 33 consecutive patients (m/f: 17/16; mean age, 56.3 ± 10.4 years) with unilateral TN confirmed NVC and consensus by two experienced radiologists on fused 3D-SPACE and 3D-TOF-MRA sequences of 3-tesla (3-T) MRI. All patients underwent microvascular decompression (MVD), using photos and video in surgery as documents compared with MRI. Both the MRI and MVD were reported for three grades (contact, compression, distortion), vessel types (artery or vein), identification of offending vessel, site (juxtapontine, cisternal, and juxtapetrous), and location (cranial, caudal, medial, lateral). Agreement between preoperative MRI visualization and surgical findings was assessed using the kappa (K) statistic.
Results: The k-values for the agreement were excellent for the grade of NVC (k=0.82), vessel types (k=0.78), and location of conflict (k=0.74), and good for identification of the offending vessel (0.65) and the site-affected vessel (k=0.69).
Conclusion: The fused D3-SPACE and 3D-TOF-MRA images are highly effective tools for the evaluation and treatment planning of NVC in TN patients.
Keywords: trigeminal neuralgia, neurovascular conflict, magnetic resonance imaging, microvascular decompression
Introduction
Trigeminal neuralgia (TN) is caused by compression of the trigeminal nerve root by an aberrant loop of an artery or vein in 80% to 90% of the cases.1 The most basic and effective treatment, in this case, is microvascular decompression (MVD), which can relieve symptoms in most cases completely. Patients with typical symptoms of TN, positive magnetic resonance findings, or the evident presence of neurovascular compression or conflict (NVC) are likely to benefit from MVD. They might have an excellent long-term prognostic factor.2–5 Therefore, preoperative image findings are significant for achieving superior clinical outcomes. Nowadays, the development of magnetic resonance (MR) imaging with high-resolution with thin-slice sequences through the pontocerebellar angle (MR cisternography) combined or fused with 3D time-of-flight spoiled gradient-recalled sequence (TOF-MR angiography), which allows effective diagnosis and assessment of NVC.6–9 Among MR cisternography sequences, 3D sampling perfection with application-optimized contrasts using different flip-angle evolutions (3D-SPACE) sequence produces a very high-resolution T2-weighted image with excellent contrast between structures applied to visualize the complex posterior fossa anatomy.10 We carried out this study to evaluate the usefulness of the fused 3D-T2-SPACE and 3D-TOF-MRA sequences in detecting NVC in patients presenting with typical TN.
Materials and Methods
Patients
At the Saint Paul Hospital of Hanoi, between March 2017 and May 2020, a prospective study was performed upon 33 consecutive patients presenting with trigeminal neuralgia. Their pain was assessed based on a visual analog score of severe or higher (between 7 and 10) and unresponsive to medical treatment. All patients underwent an MRI of the cerebellopontine angle for treatment planning of MVD surgery. Table 1 shows the characteristics of patients. Approval of this work was obtained from the institutional review board of Saint Paul Hospital, and written informed consent was obtained from the patients.
 |
Table 1 Characteristics of Patient Population |
MRI Procedures
All MRI procedures were performed on a 3-T MRI scanner (Skyra, Siemens Medical Solutions, Erlangen, Germany) with a 20-channel head-array coil and parallel imaging techniques. Conventional MR imaging (T1-WI, T2-WI, FLAIR, DIFFUSION, and GRE sequences) was used to rule out secondary trigeminal pain such as multiple sclerosis or cerebellopontine angle tumors.
The parameters of the 3D-T2-SPACE sequence were as follows: TR, 1400 ms; TE, 155 ms; flip angle mode, 120°; matrix, 320 × 320; FOV, 160 × 160mm; section thickness, 0.5 mm; acquisition time, 5 minutes 9 seconds; transverse sections; 56 slices. The imaging parameters of the 3D-TOF-MRA sequence were: TR, 21 ms; TE, 3.43 ms; flip angle, 18°; matrix, 331 × 384; FOV, 199 × 220; section thickness, 0.65 mm; acquisition time, 5 minutes 33 seconds; transverse sections; 84 slices. We note that the study did not use gadolinium-enhanced MR angiography.
MRI Post-Processing
Volumetric data obtained from T2-SPACE and TOF-MRA sequences were transferred to a dedicated workstation of the MR imaging unit (Syngo. via VB30, Siemens). The perspective views of these two sequences were independently reconstructed and then fused in a single 3D image. Thin-section reformatted on coronal, sagittal, and two planes parallel and perpendicular to the trigeminal nerve were achieved using an MPR algorithm.
MRI Analysis
All fused T2-SPACE and TOF-MRA images were evaluated in a single workstation with two different short times by two experienced radiologists (P.H.D and D.T.T) blinded to any knowledge of which side the spasm was located on, and discrepancies were resolved with consensus.
The presence of criteria NVC has recorded five features: 1) trigeminal nerve–vessel relationships were classified into four levels: 0, proximity (vessel close to the trigeminal nerve but without contact); I, (simple contact between the vessel and the trigeminal nerve); II, compression (vessel moderately compressing the trigeminal nerve); III, distortion (severe compression causing the trigeminal nerve to deform)7,11; 2) vessel types include arteries and veins, as well as single and multiple offending vessels; 3) the identification of the offending vessel was classified as an artery and a vein. The superior cerebellar artery (SCA), posterior inferior cerebellar artery (AICA), vertebral basilar artery (VBA), and anterior inferior cerebellar artery (PICA) were among these arteries; 4) the location of the conflicts along the nerve is divided into three sections: juxtapontine, at the trigeminal root entry zone (TREZ); cisternal, in the nerve’s mid-third; and juxtapetrous, at the exit of Meckel’s cave12; 5) aspects of conflicts around the circumference of the root were divided into one of the four following: cranial, caudal, lateral, or medial.13
Surgical Technique
All patients underwent MVD by one experienced surgeon (D.T.K) in a standard microdissection technique.12 In brief, full view of the cisternal trigeminal nerve from the root to the foramen of the Meckel cavity by fashioning a burr hole at the inferomedial angle of the transverse-sigmoid junction a retromastoid craniotomy approach. Under the microscope Carl Zeiss S88, the surgeon identifies compressive vessels after removing all the arachnoid surrounding the nerve. Next, the affected artery or vein is meticulously separated from the trigeminal nerve, and a shredded Teflon pad is placed between them. In each patient, the criteria for neurovascular conflict were similar to those in preoperative MRI findings recorded by the neurosurgeon performing the MVD.
Statistical Analysis
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. Quantitative data were described using mean and standard deviation. The significance of the obtained results was judged at the 5% level. The coincidence between preoperative MRI visualization and surgical findings was assessed using the kappa (K) statistic method. The k-values for agreement were categorized as follows: poor, <0.40; fair, 0.40–0.59; good, 0.60–0.74; and excellent, 0.75–1.
Results
The mean age at the time of MVD was 56.3 ± 10.4 years (age range 26–72 years), 17 (51.5%) males and 16 (48.5%) females. Nineteen (57.6%) patients reported left neuralgia and 14 (42.4%) right neuralgia. The clinical data are shown in Table 1.
The fused 3D-T2-SPACE and 3D-TOF-MRA sequences were good-quality images in all 33 instances. Surgical results showed that all patients had NVC. In these, two cases (6%) did not show NVC on MRI, but because these patients presented the worst pain (visual analog score 9–10 points) and agreed to be operated on and on MVD, they recorded both minor vein conflicts at grade I. Grade I conflict accounted for the highest rate of both MRI and MVD, with 52.8% and 55.6%, respectively. The kappa consensus coefficient on the degree of NVC between MRI and MVD is in excellent agreement (k=0.82, as shown in Table 2).
 |
Table 2 Grade of NVC on MRI Findings and MVD Results |
In Table 3, the most compression of vessel types was an arterial vascular and single artery, accounting for 29 (87.9%) patients who had two vessels in different locations, including two arteries in 2 (9.1%) patients, and a combination of one artery and one vein in 1 (3.0%) patient. Therefore, when describing conflicts, the present study will describe 36 conflict vessels, not 33 patients. There were no cases of misdiagnosis between artery and vein. The consensus on vessel types on MRI and MVD is presented at an excellent agreement (k=0.78).
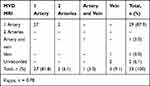 |
Table 3 Vessel Types of NVC on MRI Findings and MVD Results |
The identification of the most conflicting vessels was the superior cerebellar artery (SCA), accounting for 16 (44,4%) vessels and 12 (33,3%) vessels on MRI and MVD, respectively. Of these, two SCAs could not be identified surgically. This is followed by the anterior inferior cerebellar artery (PICA), posterior inferior cerebellar artery (AICA), the vertebral basilar artery (VBA), and the vein. The correlation coefficient between MRI and MVD in vascular identification was in good agreement (k=0.65, as shown in Table 4).
 |
Table 4 Identification of Conflicting Vessels on MRI Findings and MVD Results |
About the site of the conflicts along the root, MRI describes the most frequently occurring as the juxtapontine segment (root enter zone: REZ) in 20 (55.6%) vessels. However, on the surgical report, this segment is 15 (41.7%) vessels, the rest are four midcisternal and one juxtapetrous segment. The consensus coefficient between MRI and MVD is at a good level (k=0.69, as shown in Table 5). Finally, the consensus coefficient of the offending vessel concerning the nerve circumference was at a good level (k=0.74, as shown in Table 6).
 |
Table 5 Site of NVC on MRI Findings and MVD Results |
 |
Table 6 Aspects of NVC on MRI Findings and MVD Results |
Discussion
3D-T2-SPACE sequence is a high-resolution volumetric sequence that increases the contrast between CSF and tissues, providing accurate visualization of the cerebellopontine cistern and allowing a fine anatomical analysis of the vasculo-nervous structures of the involved TN. The CSF appears hyperintense, the blood vessels hypointense, and the cranial nerves isointense relative to the brain stem. With this sequence alone, it allows visualization of the nerves and vessels in the brain cisterns with great anatomical details, and a trained neuroradiologist can detect NVC. Ors et al reported that the SPACE sequence had fewer artifacts and was significantly more helpful than the CISS sequence for visualizing the posterior fossa cranial nerves.10
3D-TOF-MRA is based on the phenomenon of flow-related enhancement, which provides the high signal intensity of the arteries reflecting the high velocity of moving protons in the circulating blood. At the same time, stationary structures and nerves remain low in signal intensity. Compared with TOF-MRA, Yoshino found that high-resolution volumetric sequence (3D-CISS) is more useful in the detection of NVC in patients with TN.13
Traditionally, MR cisternography and MR angiography could be placed side by side for comparison, but there could be errors in memorizing complex data in the human mind. By a combination of these two sequences producing fused images, each can make up for the limitations of the other, allowing better tracking of the vessels and nerves and allowing a better depiction of their relationship, and it can be determined the differentiation of arterial and venous vasculature in the cerebellopontine angle cistern (Figure 1).8,14,15
In addition to these two sequences, some previous studies have added a 3D T1-weighted gadolinium-enhanced sequence that proved a useful adjunct reliable in detecting and predicting the degree of NVC and surgical planning in patients with TN.6 According to author Zhou et al, when comparing the results between MR cisternography (3D FIESTA sequence) and gadolinium-enhanced MR angiography, the 3D FIESTA sequence provides more useful information in the visualization of NVC in patients with TN.16 Moreover, several recent studies have shown that although no enhanced sequence is available, simple combining or fusion of these two sequences is a reliable, quick, efficient, safe, and non-invasive method for evaluation of the relationship between the trigeminal nerve and the neighboring vascular structures, and sufficient for the decision-making of MVD of the affected nerve,8,9 as well as in our present study.
Regarding the comparison between 1.5-T and 3-T MRI using the same imaging protocol, Leal et al reported that there were no statistically significant differences in the type of offending vessel, in location and severity of compression, except that visualization of the type of venous compression and determination of the exact site of compression around the root were more difficult using 1.5-T MRI.6
The degree of compression was classified into three grades depending on whether the trigeminal nerve is simply abused or indented or compressed by surrounding vessels. In the current study, there was an excellent agreement in the diagnosis of compression grade between MRI and MVD (k=0.82). This is very important because it is possible to predict the outcome after surgery. If there is only a simple contact grade of NVC, the long-term pain relief rate is only about 58%. If there are compression or distortion grades, the pain relief rate is up to 88%.2 The apparent presence and the degree of NVC are of paramount importance in predicting the probability of long-term pain relief, and therefore in the decision to propose MVD as the first choice of surgical treatment.2,4,5 So the question is which patients will benefit from MVD, which is the role of preoperative MRI. Additionally, the positive predictive value of seeing a grade III conflict on the MRI reached 100% (Figure 2). The most significant errors were undergrading conflicts of grade I or II. Overgrading of NVC represented by MRI simple closeness or contact at surgery was rarer than undergrading of high-grade conflicts.17 Moreover, multidimensional reconstruction of the nerve might be helpful, especially in identifying indentations or deformations of the nerve and, in that sense differentiating between grade I and grade II.7
The exact nature and origin of the arteries (ie, SCA, AICA, PICA or VBA) or venous of the conflicting vessels were for the most part of excellent quality, with concordance coefficients (kappa values) of 0.78. The most common arterial offenders were SCA and AICA. The SCAs are classically the most frequently encountered source of NVC and exert compression at the juxtapontine and/or cisternal sites (Figure 3).18 Brînzeu et al note that the site of AICA-related compression was frequently at the juxtapontine, where it was less evident to the examiner. This is a factor to be remembered when examining patients’ MR images.17
In the current study, the location of compressing offending vessels concerning the nerve circumference can be detected by both fusion image and MVD with excellent agreement. Zhou et al16 used MR angiography (3D FIESTA) to identify the responsible vessel’s position relative to the trigeminal nerve. They found excellent agreement between the position (medial, lateral, superior, and inferior) of the compressing vessel close to the trigeminal nerve identified by MR imaging and by surgery (k=0.81). The most common sites of compression are medial and cranial aspects relative to the position of the SCA. Leal et al6 and Gamaleldin et al9 found that nerve compression was the high percentage of superomedial sites to the high number of NVC syndromes due to SCA approaching the nerve. These results suggested the value of preoperative MRI in displaying the local anatomical relationship between vessels and nerves, providing valuable information for surgeons to precisely identify which nerve root fibers should be decompressed during surgery. Using diffusion tensor MRI with tractography remains a promising trend to clearly show the specific anatomy of the trigeminal nerve to help more insight into the etiology – pathogenesis and improve MVD outcomes in patients with TN.11,19
Our study has two (6%) cases of unidentified NVC on MRI but were still operated on because of typical symptoms. All patients in this study had previously failed medical therapy and were subsequently treated with MVD, which may favor the high incidence of NVC on the symptomatic side. The presence of NVC by high-resolution MRI gives the surgeon peace of mind to look for the offending vessel. However, the absence of vascular compression on MRI in a patient with classic TN still does not rule out surgery.20
The limitation of this study is the relatively small number of patients. Therefore, further investigations involving larger patient cohorts are required to extend these results. Also, another limitation of the current work is the absence of a control group of another MR cisternography and angiography sequences in evaluating NVC of patients with and without the symptomatic side of TN.
Conclusions
The fusion imaging techniques of 3D-T2-SPACE and 3D-TOF-MRA sequences with multiplanar reconstructions are beneficial for radiologists in adequately evaluating the grade of NVC. Although this technique does not use gadolinium-enhanced MR sequences, it still allows the detection of purely arterial or venous compressions, as well as the differentiation of their fairly exact anatomical origin. These imaging results may be helpful for neurosurgeons searching for conflicting vessels in patients with severe TN.
Ethical Approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the Saint Paul Hospital of Hanoi’s Ethical Committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for Publication
Written informed consent for publication of the clinical details was obtained from each patient.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Basic Kes V, Zadro Matovina L. Accommodation to diagnosis of trigeminal neuralgia. Acta Clin Croat. 2017;56(1):157–161. doi:10.20471/acc.2017.56.01.21
2. Sindou M, Leston J, Decullier E, Chapuis F. Microvascular decompression for primary trigeminal neuralgia: long-term effectiveness and prognostic factors in a series of 362 consecutive patients with clear-cut neurovascular conflicts who underwent pure decompression. J Neurosurg. 2007;107(6):1144–1153. doi:10.3171/JNS-07/12/1144
3. Oesman C, Mooij JJ. Long-term follow-up of microvascular decompression for trigeminal neuralgia. Skull Base. 2011;21(5):313–322. doi:10.1055/s-0031-1284213
4. Zhang H, Lei D, You C, Mao BY, Wu B, Fang Y. The long-term outcome predictors of pure microvascular decompression for primary trigeminal neuralgia. World Neurosurg. 2013;79(5–6):756–762.
5. Miller JP, Acar F, Hamilton BE, Burchiel KJ. Radiographic evaluation of trigeminal neurovascular compression in patients with and without trigeminal neuralgia. J Neurosurg. 2009;110(4):627–632. doi:10.3171/2008.6.17620
6. Leal PR, Hermier M, Souza MA, Cristino-Filho G, Froment JC, Sindou M. Visualization of vascular compression of the trigeminal nerve with high-resolution 3T MRI: a prospective study comparing preoperative imaging analysis to surgical findings in 40 consecutive patients who underwent microvascular decompression for trigeminal neuralgia. Neurosurgery. 2011;69(1):
7. Satoh T, Omi M, Nabeshima M, Onoda K, Date I. Severity analysis of neurovascular contact in patients with trigeminal neuralgia: assessment with the inner view of the 3D MR cisternogram and angiogram fusion imaging. Am J Neuroradiol. 2009;30(3):603–607. doi:10.3174/ajnr.A1409
8. Docampo J, Gonzalez N, Munoz A, Bravo F, Sarroca D, Morales C. Neurovascular study of the trigeminal nerve at 3 t MRI. Neuroradiol J. 2015;28(1):28–35. doi:10.15274/nrj-2014-10116
9. Gamaleldin OA, Donia MM, Elsebaie NA, Abdelkhalek Abdelrazek A, Rayan T, Khalifa MH. Role of fused three-dimensional time-of-flight magnetic resonance angiography and 3-dimensional T2-weighted imaging sequences in neurovascular compression. World Neurosurg. 2020;133:e180–e186. doi:10.1016/j.wneu.2019.08.190
10. Ors S, Inci E, Turkay R, Kokurcan A, Hocaoglu E. Retrospective comparison of three-dimensional imaging sequences in the visualization of posterior fossa cranial nerves. Eur J Radiol. 2017;97:65–70. doi:10.1016/j.ejrad.2017.10.012
11. DeSouza DD, Hodaie M, Davis KD. Structural magnetic resonance imaging can identify trigeminal system abnormalities in classical trigeminal neuralgia. Front Neuroanat. 2016;10:95. doi:10.3389/fnana.2016.00095
12. Sindou M, Acevedo G. Microvascular decompression of the trigeminal nerve. Oper Tech Neurosurg. 2001;4(3):110–126. doi:10.1053/onts.2001.26617
13. Yoshino N, Akimoto H, Yamada I, et al. Trigeminal neuralgia: evaluation of neuralgic manifestation and site of neurovascular compression with 3D CISS MR imaging and MR angiography. Radiology. 2003;228(2):539–545. doi:10.1148/radiol.2282020439
14. Jia JM, Guo H, Huo WJ, et al. Preoperative evaluation of patients with hemifacial spasm by Three-dimensional Time-of-Flight (3D-TOF) and Three-dimensional Constructive Interference in Steady State (3D-CISS) sequence. Clin Neuroradiol. 2016;26(4):431–438. doi:10.1007/s00062-015-0382-2
15. Muller S, Khadhraoui E, Khanafer A, Psychogios M, Rohde V, Tanrikulu L. Differentiation of arterial and venous neurovascular conflicts estimates the clinical outcome after microvascular decompression in trigeminal neuralgia. BMC Neurol. 2020;20(1):279. doi:10.1186/s12883-020-01860-8
16. Zhou Q, Liu ZL, Qu CC, Ni SL, Xue F, Zeng QS. Preoperative demonstration of neurovascular relationship in trigeminal neuralgia by using 3D FIESTA sequence. Magn Reson Imaging. 2012;30(5):666–671. doi:10.1016/j.mri.2011.12.022
17. Brînzeu A, Drogba L, Sindou M. Reliability of MRI for predicting characteristics of neurovascular conflicts in trigeminal neuralgia: implications for surgical decision making. J Neurosurg. 2018;130:611–621.
18. Mistry AM, Niesner KJ, Lake WB, et al. Neurovascular compression at the root entry zone correlates with trigeminal neuralgia and early microvascular decompression outcome. World Neurosurg. 2016;95:208–213. doi:10.1016/j.wneu.2016.08.040
19. Xie G, Zhang F, Leung L, et al. Anatomical assessment of trigeminal nerve tractography using diffusion MRI: a comparison of acquisition b-values and single- and multi-fiber tracking strategies. Neuroimage Clin. 2020;25:102160. doi:10.1016/j.nicl.2019.102160
20. Hitchon PW, Bathla G, Moritani T, Holland MT, Noeller J, Nourski KV. Predictability of vascular conflict by MRI in trigeminal neuralgia. Clin Neurol Neurosurg. 2019;182:171–176. doi:10.1016/j.clineuro.2019.05.005
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



