Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Prediabetes is Associated with Worse Long-Term Outcomes in Young Patients with Acute Coronary Syndrome
Authors Xu R, Wang C, Lang J, Wu J, Hu Y, Wang T, Zhang J, Cong H, Wang L
Received 24 August 2023
Accepted for publication 4 October 2023
Published 17 October 2023 Volume 2023:16 Pages 3213—3222
DOI https://doi.org/10.2147/DMSO.S433112
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Gian Paolo Fadini
Rongdi Xu,1,2 Cheng Wang,1,2 Jiachun Lang,1,2 Jikun Wu,1,2 Yuecheng Hu,2 Tong Wang,1,2 Jingxia Zhang,2 Hongliang Cong,1– 3 Le Wang2,3
1Clinical School of Thoracic, Tianjin Medical University, Tianjin, People’s Republic of China; 2Department of Cardiology, Tianjin Chest Hospital, Tianjin, People’s Republic of China; 3Tianjin Key Laboratory of Cardiovascular Emergency and Critical Care, Tianjin Municipal Science and Technology Bureau, Tianjin Chest Hospital, Tianjin, People’s Republic of China
Correspondence: Hongliang Cong; Le Wang, Department of Cardiology, Tianjin Chest Hospital, 261 Tai’erzhuang Road, Jinnan District, Tianjin, 300222, People’s Republic of China, Tel +86-22-88185003, Email [email protected]; [email protected]
Purpose: The incidence of prediabetes mellitus (pre-DM) is increasing among young individuals. Whether pre-DM can predict adverse cardiovascular events in acute coronary syndrome (ACS) patients remains controversial. This study aimed to investigate the impact of pre-DM on the long-term clinical outcomes of patients aged≤ 45 years with new-onset ACS.
Patients and methods: A total of 1113 patients with new-onset ACS (aged≤ 45 years) who underwent percutaneous coronary intervention (PCI) were enrolled in this study. Patients were divided into three groups according to their glycemic status or history: normal glucose metabolism (NGM), prediabetes (pre-DM), and diabetes mellitus (DM). The primary endpoint was defined as a composite of major adverse cardiovascular events (MACE) including all-cause death, myocardial infarction (MI), stroke, or unplanned repeat revascularization. Multivariate Cox regression analysis was performed to explore the association between abnormal glycemic status and MACE.
Results: The prevalence of NGM, pre-DM, and DM were 45.9% (n=511), 27.0% (n=301), and 27.0% (n=301), respectively. During a median follow-up of 65 months, MACE occurred in 23.5% (n=120) of NGM, 29.2% (n=88) of pre-DM, and 34.6% (n=104) of DM (P=0.003). After multivariate adjustment, both pre-DM and DM significantly increased the risk of MACE compared with the NGM group (pre-DM: HR1.38, CI95% 1.05– 1.83, P=0.023; DM: HR1.65, CI95% 1.27– 2.16, P< 0.001). Moreover, pre-DM had a similar impact on MACE as DM in young patients with ACS (P=0.162).
Conclusion: Pre-DM was common among patients aged≤ 45 years with new-onset ACS. Pre-DM was associated with an increased risk of future MACE compared to NGM.
Keywords: young patients, prediabetes, acute coronary syndrome
Introduction
The incidence of acute coronary syndrome (ACS) is gradually increasing among young Chinese individuals aged≤ 45 years, with changes in dietary habits, social stress, and exercise levels.1 Despite improved secondary prevention and treatment of coronary artery disease (CAD), the overall prevalence of poor cardiovascular events has shown little improvement among young patients.2 Globally, ACS remains a major cause of adverse outcomes in young adults.3 It is well established that modifiable risk factors such as smoking, obesity, and diabetes mellitus (DM) play a role in the development and prognosis of ACS. However, younger patients with ACS have more diverse risk profiles than older patients do. Therefore, it is crucial to explore risk factors in young patients with ACS to plan appropriate prevention strategies.
Prediabetes (pre-DM), an intermediate glycemic stage between normal glucose metabolism and DM,4 is becoming increasingly prevalent among young adults.5,6 According to recent diagnostic criteria, pre-DM can be defined according to fasting plasma glucose (FPG) and/or glycosylated hemoglobin (HbA1c).7 Irrespective of the defining criteria, pre-DM is highly related to increased exposure to DM, cardiovascular disease, and renal events compared with normoglycemia in the general population.8,9 Moreover, growing evidence suggests that pre-DM is associated with poor prognosis in established cardiovascular disease patients.10 Nevertheless, the relationship between pre-DM and recurrent cardiovascular events in individuals with ACS remains controversial. A recent study found that pre-DM increased the risk of all-cause death in young individuals undergoing coronary angiography (CAG).11 However, this association was not significant in those with CAD, acute myocardial infarction (AMI), or undergoing percutaneous coronary intervention (PCI) To date, there is a lack of insight into the relationship between pre-DM and long-term adverse prognosis in young ACS patients. Therefore, this study aimed to examine the impact of pre-DM assessed by FPG or HbA1c levels on the long-term prognosis of patients with new-onset ACS aged≤ 45 years.
Methods
Study Populations
This was a single-center, retrospective cohort study. We registered 2086 individuals aged ≤ 45 years who were admitted to Tianjin Chest Hospital between January 2014 and December 2020 for PCI for ACS. The inclusion criteria were as follows:1) age ≤ 45 years, 2) underwent PCI, and 3) first ACS in-a-lifetime. Moreover, 973 patients were excluded based on the following criteria: 1) severe cardiomyopathy, rheumatic heart disease, congenital heart disease, malignant tumors, or use of oral contraceptives or pregnancy; 2) incomplete clinical data; 3) lost to follow-up; 4) history of prior myocardial infarction; and 5) previous implantation of stents or coronary artery bypass grafting (CABG). Therefore, the final analysis included 1113 patients. Patients were divided into three groups according to their glucose metabolic status, patients were divided into 3 groups: NGM (n=511), pre-DM (n=301), and DM (n=301; Figure 1).
Clinical Definition
According to the recommendations of the American College of Cardiology, ACS includes ST-elevation myocardial infarction, non-ST-elevation myocardial infarction, or unstable angina. A family history of CAD was defined as proof of CAD in patients younger than 45 years (male) and 55 years (female). Current smoking was defined as an average of at least one cigarette per day (≥7 cigarettes per week) in the previous two weeks. Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg, diastolic blood pressure (DBP) ≥90 mmHg, or use of medications for treatment. The definition of glucose metabolic status is based on the American Diabetes Association (ADA).12 DM was defined as FPG >126 mg/dl and/or HbA1c >6.5%, and/or with a history of DM. Pre-DM was defined as FPG ≥100 and <126 mg/dl and/or HbA1c ≥5.7%. NGM was defined as FPG <100 mg/dl and HbA1c <5.7%. Dyslipidemia was defined as a total cholesterol (TC) exceeding 5.72 mmol/L and/or triglyceride (TG) levels exceeding 1.70 mmol/L in general adults. All patients underwent CAG for ACS using a radial or femoral approach. Angiographic stenosis was defined as a 50% reduction in the diameter of the major coronary artery or >50% reduction in the diameter of the left main coronary artery (LM).
Clinical and Laboratory Analysis
All data were obtained from the in-hospital clinical data. The risk factors analyzed included age, sex, smoking, family history of CAD, hypertension, dyslipidemia, and prior cerebral infarction. Laboratory data included levels of total cholesterol (TC), triglycerides (TG), low-density lipoprotein (LDL), high-density lipoprotein (HDL), serum creatinine, fasting plasma glucose (FPG), Hemoglobin A1c (HbA1c), and high-sensitivity C-reactive protein (hs-CRP). The left ventricular ejection fraction (LVEF) was evaluated by transthoracic echocardiography using the Teichholz method. All medical therapies during hospitalization were recorded, including aspirin, clopidogrel, ticagrelor, statins, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, β-blockers, mononitrate and antidiabetic drugs.
Follow Up
From October 2022 to January 2023, all individuals were followed up by telephone or through outpatient visits. The primary endpoint was defined as a composite of major adverse cardiovascular events (MACE). The secondary endpoints included all-cause death, myocardial infarction (MI), stroke, unplanned repeat revascularization, and the composite of death, MI and stroke. MACE included all-cause death, myocardial infarction (MI), stroke, and unplanned repeat revascularization. All-cause death was defined as death from any cause.
Statistical Analysis
The study population was divided into three groups based on fasting plasma glucose (FPG) or glycated hemoglobin (HbA1c) levels on admission. Baseline demographic characteristics, clinical features, treatment modalities, and long-term prognoses were compared among all study individuals. Normally distributed data are presented as mean ± standard deviation (X±S), while skewed distributed data are expressed as medians with interquartile ranges. Independent sample t-tests (for normally distributed data) and Kruskal–Wallis H-tests (for skewed distributed data) were conducted for continuous variables. The chi-squared test was used for categorical variables. The association between the glucose metabolism status and long-term clinical outcomes was assessed using a COX regression model. Univariate and multivariate COX proportional hazards regression models were used to analyze the independent predictors of adverse cardiovascular composite endpoints. Univariate Cox regression analysis was performed to determine possible predictive factors related to MACE. Then, variables with significant association (P<0.20) with MACE were included in multivariate Cox regression analysis. All variables found to be significant in the univariate analysis, including age, BMI, hypertension, hyperlipidemia, Gensini Score, TC, LDL-C, HDL-C, and creatinine level, were included in the multivariable regression model. The results are expressed as adjusted hazard ratios (HR) with 95% confidence intervals. Statistical significance was set at p <0.05. Data analysis was performed using SPSS version 26.0.
Results
Baseline Characteristics
Our study included 1113 young patients with new-onset acute coronary syndrome (ACS). Among the 1113 young patients with new-onset ACS, 1045 (93.9%) were men, and the mean age of the adults was 40.3 ± 4.3 years. According to the American Diabetes Association (ADA) criteria, the NGM group accounted for 45.9% (n=511), pre-DM group accounted for 27.0% (n=301), and DM group accounted for 27.0% (n=301). The baseline characteristics of the NGM, pre-DM, and DM groups are showed in Table 1 and Table 2. Compared with the NGM group, the pre-DM and DM groups tended to be older (P=0.017) and had higher BMI, SBP, DBP, heart rate, prior cerebral infarction, TC, FPG, HbA1c, and Hs-CRP levels (all p<0.05), while the Pre-DM and DM groups had lower LVEF and creatinine levels (all p<0.001). Interestingly, we found that the smoking rate was the highest in the NGM group (72.6%; n=371). Moreover, we observed a higher incidence of ST-elevation myocardial infarction (STEMI) in the pre-DM and DM groups, whereas acute non-ST-elevation myocardial infarction (NSTEMI) had the highest incidence in the NGM group. The baseline Grace and Gensini scores were not significantly different between groups. Nevertheless, regarding angiographic stenosis, the proportion of single-vessel lesions and left main stem lesions decreased progressively in the groups (P=0.004). Among the three groups, the DM group had the highest proportion of triple-vessel lesions (34.9%, n=105) and the pre-DM group had the highest proportion of double-vessel lesions (38.9%, n=117). In terms of target vessels, the NMG group had the highest proportion of left anterior descending artery lesions (61.8%, n=315), whereas the circumflex and right coronary arteries had the highest proportions in the pre-DM group (27.6% and 39.9%, respectively). The three groups had similar stent implantation rates. Beta blockers were sequentially elevated in all three groups (p<0.001). There were no statistically significant differences in the number of target vessels, percutaneous transluminal coronary angioplasty (PTCA), HDL-C, LDL-C, TC, family history of CAD, or other drug treatments between the three groups.
 |
Table 1 Baseline Characteristics of Patients According to Glucose or HbA1c on Admission |
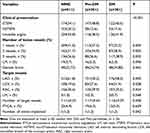 |
Table 2 Clinical Presentation and Coronary Angiography Outcomes of Patients According to Glucose or HbA1c on Admission |
The Relationship Between Glucose Metabolism and Prognosis of New-Onset Acute Coronary Syndrome in Young Patients
During the median follow-up period of 65 months, 28.1% (n=312) of the patients experienced adverse cardiovascular events. The incidence rates of MACE, Death, MI and stroke, and all-cause death during the period of follow-up were higher in the three groups (NGM, Pre-DM, and DM) (MACE:23.5%, 29.2%, and 34.6%, P=0.003; Death, MI and stroke:5.7%, 8.0%, 9.6%, P=0.056; all-cause death:0.6%, 1.3%, 2.7%, P=0.048, Table 3). In the Univariate Cox regression analysis, pre-DM was confirmed to be related to the incidence of MACE (Hazard Ratio (HR):1.38, 95% confidence interval (CI):1.05–1.83, p=0.023, Table 4) and hard endpoint events (HR, 1.69; 95% CI:0.97–2.96, p=0.064; Table 3). Compared to NMG, DM was confirmed to be related to outcomes (all p < 0.05). Furthermore, after adjusting for potential confounders including age, hypertension, dyslipidemia, Gensini Score, LDL-C, HDL-C, TG, and creatinine, both pre-DM and DM were independent predictors of MACE and Death, MI and stroke (HR:1.38, 95% CI 1.05–1.83, P=0.023, HR:1.65, 95% CI 1.27–2.16, P<0.001; HR:1.65,95% CI 1.27–2.16, P<0.001, HR:1.93, 95% CI 1.14–3.28, P=0.015, respectively, Table 4). No significant differences were observed between the pre-DM and the DM groups. In the Kaplan-Meier analysis, pre-DM showed adverse prognosis in MACE (log-rank p =0.002, Figure 2A), Death, MI and stroke (log-rank p=0.014, Figure 2B), all-cause death (log-rank p=0.008, Figure 2C), repeat revascularization (log-rank p=0.007, Figure 2D), myocardial infarction (log-rank p=0.071, Figure 2E), and stroke (log-rank p=0.007, Figure 2F).
 |
Table 3 Clinical Outcomes of Young Patients with ACS During the Follow-Up |
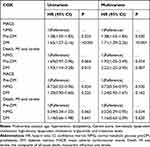 |
Table 4 Univariate and Multivariate Cox Regression Analysis of Events According to Glucose or HbA1c on Admission |
Discussion
The present study is the first to investigate the association between pre-DM and long-term clinical prognosis in patients aged ≤ 45 years with new-onset ACS who underwent PCI. The major findings of this study are as follows: First, pre-DM was present in 27% of young patients who first presented with ACS at ≤ 45 years of age. Second, patients with pre-DM or DM at admission had a higher risk of long-term MACE after PCI than did those with NGM. Third, pre-DM had a similar impact on MACE as DM did in young patients with ACS. These results indicate that the routine assessment of glycemic metabolism may contribute to the early identification of pre-DM and thus facilitate risk stratification in young patients with ACS. Furthermore, effective measures should be taken to reverse the pre-DM state to normoglycemia to reduce the corresponding cardiovascular risk.
Pre-DM is an intermediate stage between NGM and DM, affecting nearly 720 million individuals worldwide by 2021.13 The prevalence of pre-DM is increasing around the world, and the prevalence of pre-DM is 27.8% in young individuals.13 The prevalence of pre-DM in young patients undergoing coronary angiography (CAG) was reported higher than in the normal population. A retrospective study found that pre-DM was present in 36.5% of young patients undergoing CAG.11 However, only few data are available concerning the prevalence of pre-DM in young patients with CAD. Prediabetes can enhance cardiovascular disease risk by 20% and is related to the increase of incidence of ACS. Among patients with STEMI aged ≤ 45 years, the incidence of pre-DM was 33%.14 Similar with DM patients, gender, dyslipidemia, hypertension, and obesity may increase the risk of ACS in patients with Pre-DM. In the present study, the age range of young individuals was confined to 18–45 years to determine the prevalence of pre-DM. The results showed that pre-DM accounted for 27% of the patients aged ≤ 45 years with new-onset ACS. The relatively high prevalence of pre-DM highlights the importance of routine screening among young patients who present with ACS.
Previous studies have explored the relationship between pre-DM and cardiovascular events in patients after acute coronary events. Many studies have confirmed that pre-DM is independently associated with MACE. Patients with pre-DM (OGTT) had an increased MACE risk at an average age of 63.5 years with a median follow-up of 34 months.6 Timmer et al demonstrated that pre-DM was related to poor prognosis for STEMI patients with STEMI with a mean age of 62 years who underwent PCI.15 A US study revealed that among patients with ACS and a median age of 75 years, pre-DM did not increase the risk of 28-days or 1-year death but was associated with 12-month acute coronary syndrome recurrence.16 Gao et al suggested that pre-DM increased the risk of MACE in patients with myocardial infarction with non-obstructive coronary arteries (MINOCA) and a mean age of 58 years.17 All these findings suggested that pre-DM may be an independent predictor of MACE in patients with ACS.
Contrary to these studies, several failed to find a significant association between pre-DM and prognosis in patients with ACS. The EARLY ACS trial enrolled 8795 ACS patients, with an average age of 67.5 years, suggesting that pre-DM (by ADA) was a predictor of 30-days death, but did not increase the risk of 1-year mortality.18 Xue et al suggested that pre-DM was not related to an increased risk of ACS readmission.19 But it defined pre-DM by Hb1Ac of 6.0% to 6.4%, which may result in some pre-DM patients being included in the NGM by mistake, and this study enrolled ACS patients with a mean age of 65.9 years. In the PLATelet inhibition and patient Outcomes (PLATO) trial, Akerblom et al proposed that pre-DM, defined by an HbA1c of 5.7% to 6.4%, was not a negative predictor of MACE in ACS patients of similar age.20 The TARTEMIS Study enrolled patients with CAD, and a mean age of 69 years suggested that pre-DM, defined by an FBP of 6.1 mmol/L to 7.0 mmol/L, had no significant statistical difference for MACE (cardiac death, heart failure, and ACS) compared with NGM.21 This study only used FPG to diagnose pre-DM, which would have missed a proportion of patients with IGT, leading to an underestimation of the prevalence of pre-DM. An Analysis from the PROSPECT Study indicated that pre-DM was not associated with MACE in patients with ACS.22 Differences in sample size, duration of the follow-up period, baseline characteristics, or diagnostic criteria for pre-DM may have led to the opposite results.
Young age is associated with an increased incidence of pre-DM in patients undergoing CAG. Therefore, it is important to clarify the role of pre-DM in young patients with established CAD. To date, no study has specifically probed the association between pre-DM and cardiovascular outcomes in individuals aged ≤45 years with ACS who have undergone PCI. The present study extended previous findings to young patients whose recurrent cardiovascular outcomes were not significantly improved using contemporary preventive strategies. An enhanced risk of MACE was observed in patients with pre-DM during the follow-up. Moreover, after controlling for potential confounders, the pre-DM status remained independently predictive of adverse cardiovascular outcomes. These outcomes underlined that pre-DM increases the risk of recurrent events in patients with acute coronary events. More importantly, pre-DM conferred a similar magnitude of risk to established DM for the development of adverse cardiovascular events among young patients with ACS. Therefore, pre-DM may be a stronger cardiovascular risk factor in young ACS patients. These findings highlight the importance of monitoring blood glucose levels and maintaining normoglycemia in young ACS patients.
The exact mechanisms underlying the negative impact of pre-DM on MACE in young patients with ACS undergoing PCI remain unclear. The higher incidence of conventional cardiovascular risk factors in the pre-DM group than that in the NGM group may partly contribute to this association. However, after adjusting for traditional risk factors, the association between pre-DM and MACE remained, suggesting the involvement of other factors. Hyperglycemia can damage endothelial and microvascular functions, resulting in a larger infarct area, reduced functional recovery, increased platelet aggregation, and stimulation of coagulation,23 both of which lead to an elevated risk of MACE. Insulin resistance and activated inflammatory response mediated by pre-DM may be implicated in the rapid progression of atherosclerosis.24 Furthermore, compared with non-diabetic patients, coronary atherosclerosis burden is more advanced in patients with pre-DM.25 Patients with pre-DM may have a smaller coronary size and diffuser coronary stenosis than those with normoglycemia.26 In addition, the possibility that the association between pre-DM and poor prognosis was driven by the progression of pre-DM to DM cannot be ruled out. Nevertheless, pre-DM had a similar impact on MACE as DM did in this study. Further research is required to clarify the exact mechanism underlying the association between pre-DM and cardiovascular events after ACS.
Studies have demonstrated that reversing from pre-DM to normoglycemia may reduce the corresponding cardiovascular risk.27 However, no specific medication has been approved by guidelines for pre-DM prevention. Lifestyle modifications, including weight loss and exercise, have been recommended as the preferred initial approach after a diagnosis of pre-DM.28 Metformin is effective in decreasing the risk of diabetes among individuals with pre-DM.29 New hypoglycemic drugs, such as SGL-2 inhibitors and GLP-1 agonists, have been demonstrated to reduce cardiovascular risk in patients with DM,8 but whether these drugs have the same benefits in patients with pre-DM needs further investigation. Hence, it is important to explore new prevention and control measures for the high prevalence and importance of pre-DM in young patients with ACS.
This study was the first focus on the relationship between prediabetes and long-term outcomes in young patients with ACS. However, it had several limitations. First, because patients with ACS are in a stressful state, their blood glucose levels during hospitalization may be elevated, which could lead to deviations in specific grouping. Second, this study had a long follow-up period; therefore, some prediabetes patients may have progressed to diabetes during the follow-up period. The increased risk of MACE cannot be excluded because of the conversion of pre-diabetes to diabetes; therefore, further studies are recommended to follow the changes in pre-DM in young patients with ACS who underwent PCI. Third, this was a single-center study with a low event rate, which may lead to exaggerated results; therefore, further multicenter prospective studies are needed. Finally, because the selected patients in this study did not undergo a 2-hour OGTT examination, we were unable to further analyze the impact of pre-DM on the long-term prognosis of ACS.
Conclusion
In conclusion, pre-DM was common among patients aged≤ 45 years with new-onset ACS. Pre-DM was associated with an enhanced risk of future MACE compared with NGM. These findings highlight the need for more effective therapeutic strategies to prevent adverse cardiovascular events in young patients with pre-DM.
Ethics Approval and Consent to Participate
The study protocol was approved by the Medical Ethics Committee of Tianjin Chest Hospital (IRB number: 2023LW-008). The study was conducted in accordance with the Declaration of Helsinki and all patients provided written informed consent.
Funding
This study was funded by the Project of Science and Technology of Tianjin Health Commission in 2022 (No. TJWJ2022MS035).
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could influence the work reported in this study.
References
1. Kannel WB, Abbott RD. Incidence and prognosis of unrecognized myocardial infarction. An update on the Framingham study. N Engl J Med. 1984;311(18):1144–1147. doi:10.1056/NEJM198411013111802
2. Han T, Wang Q, Yang H, et al. Risk factors for repeat percutaneous coronary intervention in young patients (≤45 years of age) with acute coronary syndrome. PeerJ. 2019;7:e6804. doi:10.7717/peerj.6804
3. Yandrapalli S, Nabors C, Goyal A, et al. Modifiable risk factors in young adults with first myocardial infarction. J Am Coll Cardiol. 2019;73(5):573–584. doi:10.1016/j.jacc.2018.10.084
4. Tabák AG, Jokela M, Akbaraly TN, et al. Trajectories of glycaemia, insulin sensitivity, and insulin secretion before diagnosis of type 2 diabetes: an analysis from the Whitehall II study. Lancet. 2009;373(9682):2215–2221. doi:10.1016/S0140-6736(09)60619-X
5. Colagiuri S. The prevalence of abnormal glucose regulation in patients with coronary artery disease across Europe. Eur Heart J. 2004;25(21):1861–1862. doi:10.1016/j.ehj.2004.09.002
6. Norhammar A, Tenerz A, Nilsson G, et al. Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: a prospective study. Lancet. 2002;359(9324):2140–2144. doi:10.1016/S0140-6736(02)09089-X
7. Hollander P, Spellman C. Controversies in prediabetes: do we have a diagnosis? Postgrad Med. 2012;124(4):109–118. doi:10.3810/pgm.2012.07.2562
8. Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323. doi:10.1093/eurheartj/ehz486
9. Balakrishnan R, Berger JS, Tully L, et al. Prevalence of unrecognized diabetes, prediabetes and metabolic syndrome in patients undergoing elective percutaneous coronary intervention. Diabetes Metab Res Rev. 2015;31(6):603–609. doi:10.1002/dmrr.2646
10. Chattopadhyay S, George A, John J, et al. Pre-diabetes mellitus newly diagnosed after myocardial infarction adversely affects prognosis in patients without known diabetes. Diab Vasc Dis Res. 2019;16(6):489–497. doi:10.1177/1479164119845561
11. He Y, Lu H, Ling Y, et al. Prediabetes and all-cause mortality in young patients undergoing coronary artery angiography: a multicenter cohort study in China. Cardiovasc Diabetol. 2023;22(1):42. doi:10.1186/s12933-023-01776-w
12. American Diabetes Association. 2. classification and diagnosis of diabetes: standards of medical care in diabetes–2019. Diabetes Care. 2019;42(Supplement_1):S13–S28. doi:10.2337/dc19-S002
13. Echouffo-Tcheugui JB, Perreault L, Ji L, et al. Diagnosis and management of prediabetes: a review. JAMA. 2023;329(14):1206–1216. doi:10.1001/jama.2023.4063
14. Hermanides RS, Kennedy MW, Kedhi E, et al. Impact of elevated HbA1c on long-term mortality in patients presenting with acute myocardial infarction in daily clinical practice: insights from a ‘real world’ prospective registry of the Zwolle Myocardial Infarction Study Group. Eur Heart J Acute Cardiovasc Care. 2020;9(6):616–625. doi:10.1177/2048872619849921
15. Timmer JR, Hoekstra M, Nijsten MW, et al. Prognostic value of admission glycosylated hemoglobin and glucose in nondiabetic patients with ST-segment-elevation myocardial infarction treated with percutaneous coronary intervention. Circulation. 2011;124(6):704–711. doi:10.1161/CIRCULATIONAHA.110.985911
16. Mahendran DC, Hamilton G, Weiss J, et al. Prevalence of pre-existing dysglycaemia among inpatients with acute coronary syndrome and associations with outcomes. Diabetes Res Clin Pract. 2019;154:130–137. doi:10.1016/j.diabres.2019.07.002
17. Gao S, Ma W, Huang S, et al. Impact of prediabetes on long-term cardiovascular outcomes in patients with myocardial infarction with nonobstructive coronary arteries. Diabetol Metab Syndr. 2021;13(1):103. doi:10.1186/s13098-021-00721-9
18. Giraldez RR, Clare RM, Lopes RD, et al. Prevalence and clinical outcomes of undiagnosed diabetes mellitus and prediabetes among patients with high-risk non-ST-segment elevation acute coronary syndrome. Am Heart J. 2013;165(6):918–25.e2. doi:10.1016/j.ahj.2013.01.005
19. Xue M, Dutton H, Arnaout A. Effects of prediabetes on long-term risk of developing cardiac events in patients presenting with acute coronary syndrome. Can J Diabetes. 2023;47(6):490–496. doi:10.1016/j.jcjd.2023.04.014
20. Åkerblom A, Wojdyla D, Steg PG, et al. Prevalence and relevance of abnormal glucose metabolism in acute coronary syndromes: insights from the PLATelet inhibition and patient Outcomes (PLATO) trial. J Thromb Thrombolysis. 2019;48(4):563–569. doi:10.1007/s11239-019-01938-2
21. Kiviniemi AM, Lepojärvi ES, Tulppo MP, et al. Prediabetes and risk for cardiac death among patients with coronary artery disease: the ARTEMIS Study. Diabetes Care. 2019;42(7):1319–1325. doi:10.2337/dc18-2549
22. Farhan S, Redfors B, Maehara A, et al. Impact of pre-diabetes on coronary plaque composition and clinical outcome in patients with acute coronary syndromes: an analysis from the PROSPECT study. JACC Cardiovasc Imaging. 2019;12(4):733–741. doi:10.1016/j.jcmg.2017.06.023
23. Li Y, Woo V, Bose R. Platelet hyperactivity and abnormal Ca 2+ homeostasis in diabetes mellitus. Am J Physiol Heart Circ Physiol. 2001;280(4):H1480–H1489. doi:10.1152/ajpheart.2001.280.4.H1480
24. Inoue T, Croce K, Morooka T, et al. Vascular inflammation and repair: implications for re-endothelialization, restenosis, and stent thrombosis. JACC Cardiovasc Interv. 2011;4(10):1057–1066. doi:10.1016/j.jcin.2011.05.025
25. Amano T, Matsubara T, Uetani T, et al. Abnormal glucose regulation is associated with lipid-rich coronary plaque: relationship to insulin resistance. JACC Cardiovasc Imaging. 2008;1(1):39–45. doi:10.1016/j.jcmg.2007.09.003
26. Ertan C, Ozeke O, Gul M, et al. Association of prediabetes with diffuse coronary narrowing and small-vessel disease. J Cardiol. 2014;63(1):29–34. doi:10.1016/j.jjcc.2013.06.015
27. Vistisen D, Kivimäki M, Perreault L, et al. Reversion from prediabetes to normoglycaemia and risk of cardiovascular disease and mortality: the Whitehall II cohort study. Diabetologia. 2019;62(8):1385–1390. doi:10.1007/s00125-019-4895-0
28. Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1677–1686.
29. Nathan DM, Davidson MB, DeFronzo RA, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30(3):753–759. doi:10.2337/dc07-9920
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


