Back to Journals » Psychology Research and Behavior Management » Volume 16
Potential Correlation Between Self-Compassion and Bedtime Procrastination: The Mediating Role of Emotion Regulation
Authors Rehman S , Rehman E, Liu B
Received 17 August 2023
Accepted for publication 10 November 2023
Published 22 November 2023 Volume 2023:16 Pages 4709—4723
DOI https://doi.org/10.2147/PRBM.S431922
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Shazia Rehman,1,2 Erum Rehman,3 Bangshan Liu1,2
1Department of Psychiatry, National Clinical Research Center for Mental Disorders, and National Center for Mental Disorders, The Second Xiangya Hospital of Central South University, Changsha, Hunan, 410011, People’s Republic of China; 2Mental Health Institute of Central South University, China National Technology Institute on Mental Disorders, Hunan Technology Institute of Psychiatry, Hunan Key Laboratory of Psychiatry and Mental Health, Hunan Medical Center for Mental Health, Changsha, Hunan, 410011, People’s Republic of China; 3Department of Mathematics, Nazarbayev University, Nur-Sultan, Kazakhstan
Correspondence: Bangshan Liu, Department of Psychiatry, National Clinical Research Center for Mental Disorders, and National Center for Mental Disorders, The Second Xiangya Hospital of Central South University, Changsha, Hunan, 410011, People’s Republic of China, Tel +86 15111082510, Email [email protected]
Purpose: The present research aims to investigate the potential correlations between self-compassion and bedtime procrastination, a significant behavior related to sleep. In this research, we put forward the hypothesis that a reduction in negative affect and the implementation of adaptative emotion regulation strategies can elucidate the established connections between self-compassion and a decreased tendency for bedtime procrastination.
Methods: Two cross-sectional online surveys (Survey I: n=241 and Survey II: n=546) were carried out via a convenient sampling method. Prior to their inclusion, all participants underwent a thorough assessment to confirm no evidence of clinical insomnia. The study participants in both survey investigations were asked to complete various psychometric assessments, including self-compassion, positive and negative affect, and bedtime procrastination; however, the study participants in Survey II additionally underwent the administration of a cognitive reappraisal assessment.
Results: In Survey I, a multiple mediation analysis was conducted to examine the mediating effects of self-compassion on reducing bedtime procrastination through a reduction in negative affect. The results supported the hypothesized relationships, indicating that self-compassion had the expected mediated effects by mitigating negative affective states. However, contrary to expectations, higher positive affect did not mediate the relationship between self-compassion and reduced bedtime procrastination. The findings of Survey II were confirmed through the utilization of path analysis. Moreover, this analysis provided additional evidence to suggest that the mechanism of cognitive reappraisal could account for the observed decrease in negative affect associated with self-compassion. The present study found a notable and sustained impact of self-compassion on reducing instances of delaying bedtime activities.
Conclusion: The present research contributes novel empirical evidence suggesting a negative association between self-compassion and the propensity to engage in bedtime procrastination. This relationship can be attributed partly to the implementation of an adaptative emotion regulation mechanism that effectively alleviates negative affect.
Keywords: bedtime procrastination, sleep-related behavior, self-compassion, negative affect, emotion regulation, positive affect
Introduction
Self-compassion (SC) encompasses both a transient mental state and a stable personality trait, involving the adoption of a benevolent, receptive, and unbiased attitude toward oneself during instances of adversity or failure. It entails mindfully addressing the adverse emotions arising from challenging circumstances while recognizing that one’s suffering is not an isolated experience.1 There is a mounting body of evidence suggesting a positive correlation between the practice of SC in response to one’s shortcomings and failures, and a variety of advantageous health-related consequences. SC is positively correlated with a reduction in physical symptoms,2,3 a decrease in perceived stress,4–6 and a moderating effect on physiologic responses to stress.7,8 SC has been recognized as a significant factor in predicting various health-related practices, such as adhering to a healthy diet,6,9 engaging in regular physical activity,10 quitting smoking,11 complying with healthcare instructions,12 pursuing medical attention,2 and adopting general health-promoting practices.13
Significantly, there is an increasing body of evidence suggesting that the association between SC and enhanced physical well-being can be elucidated, at least in part, by an improved adherence to health-promoting behaviors.14,15 In current literature, the focus on SC has primarily centered around its disposition to individuals’ health outcomes. However, recent research has accentuated the potential of implementing uncomplicated interventions to enhance and sustain levels of SC.16 The investigation of the various mechanisms and advantages by which SC facilitates the promotion of pivotal health behaviors holds significant importance in the realm of health promotion. SC plays a role in improving the self-regulation of health-promoting practices by fostering adaptative self-regulatory processes, specifically in terms of goal-setting, proactive behavior, behavioral monitoring, and emotional regulation.17,18 Nevertheless, there is a dearth of substantial and decisive evidence correlating SC with comprehensive indicators of self-regulation. The findings derived from a meta-analysis provide substantiation for this claim and categorically propose that SC is correlated with an emotion regulation approach characterized by greater proportions of positive affect, expeditious recuperation from, and decreased responsiveness to stress, as well as the utilization of adaptative emotional regulation abilities and tactics.19 Empirical evidence has indicated that SC is connected to the utilization of emotion-focused regulating approaches that augment positive affect, specifically embracing and positively reassessing one’s experiences. Conversely, SC exhibits an inverse association with the adoption of regulating strategies that amplify negative affect, such as taking responsibility or engaging in self-reproach.20,21 Moreover, there exists empirical corroboration illustrating the correlation between trait SC and physiologic indicators of emotion regulation, including fluctuations in heartbeat rate.22 One efficacious approach for the attenuation of negative emotions is cognitive reappraisal, which involves modifying a scenario to alter one’s emotional response to it.23 The association between SC and cognitive reappraisal in mitigating negative mood implies that cognitive reappraisal serves as an emotion regulation technique that is particularly pertinent in comprehending the potential benefits of SC in emotion regulation.23,24 In addition, the significant mediating effects of SC on health-related practices were observed to have both positive and negative affect, implying that emotional regulation could potentially serve as a pivotal factor in promoting advantageous health behaviors among individuals who exhibit SC.13,25
Sleep insufficiency has been found to elevate individuals’ susceptibility to contracting severe illnesses encompassing communicable diseases, malignancy, cardiac disorders, and mental health issues.26,27 The quality and quantity of an individual’s sleep are significantly influenced by behavioral factors. For instance, individuals often choose to postpone their bedtime unnecessarily, despite being aware of the potential negative consequences that may arise from such a decision.28–30 Bedtime procrastination (PRBT) shares traits with other forms of procrastination, highlighting the relevance of trait self-control in individuals’ ability to achieve a desirable sleeping pattern. This implies that individuals must apply considerable diligence to ensure timely bedtime adherence. Consistent with the aforementioned perspective, within a phenomenological investigation, individuals identified as bedtime procrastinators revealed that the act of transitioning from gratifying leisure activities to the act of falling asleep generally demands considerable exertion.31 In addition, a considerable number of individuals displaying PRBT in this investigation reported postponing their sleeping hours following fatiguing or demanding days as a means to allocate time for viewing television or engaging in video game activities, to achieve a state of relaxation. Hence, the phenomenon of delaying bedtime can be viewed as a mechanism for immediate mood regulation. In the context of PRBT, individuals tend to delay their bedtime routine and engage in activities that are pleasurable or enjoyable, thereby postponing the initiation of sleep. This behavior mirrors the broader phenomenon of procrastination, where individuals opt for activities that offer immediate gratification instead of tackling tasks that may induce stress or anxiety. The allure of momentary pleasure serves as a means of escape from the demands and pressures associated with the pending task, allowing individuals to experience a temporary sense of relief. The concept of mood repair pertains to the psychological processes involved in restoring positive affect or alleviating negative affect in individuals.32 Following the aforementioned proposition, we posit that the phenomenon of PRBT could serve as a suboptimal means of regulating immediate affective states by individuals. This perspective aligns with prevailing theories and empirical studies concerning the phenomenon of procrastination in general. It suggests that the regulation of emotions plays a crucial role in their perpetuation, and endeavors to enhance one’s competence in managing emotions can effectively mitigate or alleviate procrastination tendencies.33 Procrastination has the potential to initiate a detrimental looping process wherein individuals involved in procrastination as a means of mood regulation, experience negative emotions as a consequence, subsequently intensifying their inclination to procrastinate.34 In the scope of the current investigation, we put forward the notion that these results could potentially relate to the phenomenon of PRBT. Bedtime procrastinators, in particular, tend to defer the act of retiring to bed to alleviate their negative emotional state. Consequently, this behavior leads to an increased vulnerability to sleep deprivation, thereby diminishing their ability to effectively manage stress. As a consequence, individuals are more inclined to indulge in the practice of delaying bedtime, commonly referred to as PRBT.
The Present Study
Based on existing evidence, it can be inferred that there exists a correlation between engagement in health-promoting practices and the cultivation of SC. An explanation for this relationship could be attributed to the fostering of adaptative emotional reactions towards intrinsic imperfections and setbacks, which enhance positive emotions and diminish negative ones. Thus far, limited research exists that directly investigates the extent to which emotion regulation, specifically through cognitive reappraisal, contributes to the advantageous levels of positive and negative emotions linked to SC, ultimately promoting positive health-promoting practices. Furthermore, the association between SC and PRBT, significant sleep-related conduct connected to inadequate self-regulation and conceivably deficient emotion regulation, remains unexplored. In alignment with prior empirical evidence, the present research anticipated a similar relationship wherein individuals possessing SC would exhibit reduced instances of PRBT. Also, it was hypothesized that the elevated levels of positive affect and low levels of negative affect arising from SC would serve as determining factors in reducing the occurrence of PRBT. These hypotheses were assessed in two distinct populations regarding the presence of sleep disorders. Determining the causality between delayed bedtimes and sleep disorders or PRBT is a challenging task among individuals afflicted with sleep disorders.
Survey I
In Survey I, an investigation was conducted to examine the associations between dispositional SC and various aspects of sleep quality and behavior. The hypothesis posited that higher levels of SC would correspond to improved sleep quality, reduced difficulty in falling asleep, and decreased likelihood of engaging in PRBT. In addition, we examined the potential mediating influences of positive and negative affect in establishing a connection between SC and the phenomenon of PRBT. The schematic diagram illustrating the study design employed in participant recruitment for both surveys is visually presented in Figure 1.
 |
Figure 1 Study design. |
Methods
Participants
A total of 241 individuals were included in the sample, with a mean age of 29.72 years and a standard deviation of 9.3. The majority of participants were female, accounting for 87.5% of the total sample. A slight majority (51.71%) of the individuals in the study did not possess the status of being enrolled as students. Of the respondents who were indeed students, the majority were identified as undergraduate students, constituting 48.32% of the total cohort.
Procedure
A convenience sampling method was employed to recruit participants for the investigation. Recruitment efforts were made by sending emails to a volunteer list consisting of university students, posting notices on various social media platforms, and placing advertisements on online psychology websites. Participants were asked to complete an online survey after indicating their agreement to provide informed consent. All individuals involved in the survey were provided with an opportunity to potentially receive a gift voucher valued at 5000 PKR. The data collection period spanned from September 2022 to November 2022.
Questionnaire
Demographics
The study incorporated the demographic characteristics of the participants, which comprised their gender, age, status as students, fields of study, and the following psychological indicators.
Self-Compassion (SC)
The study participants underwent administration of the 26-item Self-Compassion Scale (SCS),8 a tool designed to evaluate the three primary constituents of SC as well as their respective negative constructs. The scale comprises a symmetry of positively and negatively worded items that are of equal number, whereas subcomponents can be elucidated through the consideration of a unified overarching factor of SC. The assessment of the response was conducted using a Likert scale consisting of five points ranging from 1: never to 5: always. The average of the items was calculated, and after applying reverse coding, a score was obtained to indicate elevated levels of SC. The SCS has been observed to exhibit a favorable degree of validity concerning both convergence and discriminant aspects, with prior research revealing excellent test-retest reliability of 0.93 (Cronbach’s alpha).1,35 The Cronbach’s alpha (0.91) value for SC showed greater reliability.
Bedtime Procrastination (PRBT)
A 9-item PRBT scale was adapted as an instrument to assess the level of PRBT among study participants. This scale was developed by Kroese et al to evaluate the tendency to postpone going to bed without apparent reason, with a high value indicative of a greater tendency towards procrastination.30,31 On a 5-point Likert scale; 1 (never) – 5 (always), PRBT comprises 4 positively phrased and 5 negatively phrased questions with a good internal consistency of 0.79 as evidenced by prior investigations.31,36 The Cronbach alpha for the current study showed a reliability of 0.92 for PRBT.
Sleep Quality
To assess the quality of sleep, two measures derived from the frequently adopted and highly reliable Pittsburgh Sleep Quality Index (PSQI) were employed,37 which evaluates seven distinct dimensions of sleep quality. In the context of the present investigation, and intending to present a comprehensive overview of the sleep patterns of the study participants, we exclusively relied on the PSQI global sleep quality assessment and sleep-related difficulty metrics. The quality of sleep experienced by the individuals was evaluated through a self-reported survey question. Specifically, participants were asked to assess their overall sleep quality for the past two weeks using a 4-point Likert scale ranging from 1 (referring to very good quality) to 4 (referring to very poor quality), wherein a high value indicated an aberrant sleep pattern. Participants were also asked to indicate their frequency of experiencing sleep difficulties within thirty minutes in the past two weeks by rating on a 4-point Likert scale of 1(not during the past two weeks) to 4 (3 or more times), where a score of 1 indicated no occurrences while a score of 4 indicated frequent difficulties (three or more times a week), wherein high value was indicative of more frequent sleep issues. The Cronbach’s alpha reliability coefficient for the sleep quality subscales varied from 0.90 to 0.93.
Positive and Negative Affect
The Positive and Negative Affect Schedule (PANAS) comprises two distinct subscales, namely, positive affect and negative affect, encompassing a total of twenty components each.38 These items are designed to depict various affective conditions through the use of descriptive language and are divided equally between the positive affect and negative affect subscales, with each subscale containing ten components. The participants were requested to evaluate their present degree of experience with various affective conditions using a 5-point Likert scale comprising five points, which ranged from 1 (signifying very little or no experience) to 5 (indicating an extremely high level of experience). The PANAS has been widely recognized for its robust internal consistency reliability, as evidenced by alpha coefficients ranging between 0.85 to 090 for positive affect and 0.84 to 0.87 for negative affect.39 For the current study, Cronbach’s alpha coefficient of positive and negative affect turned out to be 0.91 and 0.89, respectively.
Results
Common Method Deviation Analysis
To predict common method bias variation among the scale items, we estimated Harman’s single-factor test. The findings showed that the total variance explained by the first factor was 31.28% which was below the threshold of 40%, indicating no issue of common method deviation among the items on the questionnaire.
Reliability and Validity Analysis of the Questionnaire in Survey I
Table 1 illustrates the findings of the reliability analysis, as well as the assessment of discriminant and divergent validity for the psychometric constructs. The reliability analysis was evaluated through the utilization of Cronbach’s alpha coefficient and McDonald’s omega. The assessment of construct validity involved the examination of model fit statistics and the average variance extracted index (AVE). The results of the study demonstrated a satisfactory degree of reliability and validity to the SCS, PRBT, PSQI, and PANAS scales.
 |
Table 1 Dicriminant validity, Reliablity, and Construct Validity Analysis results (Survey I) |
Descriptive and Bivariate Correlation Analysis of the Variables
Table 2 exhibits the findings of the Pearson correlation analysis performed on the study parameters. The outcomes supported the proposed hypotheses, wherein SC demonstrated a negative correlation with PRBT (r=−0.346; p-value: 0.001), trouble falling asleep within half an hour (r=−0.388; p-value: 0.002), poor sleep quality (r=−0.511; p-value: 0.002), and negative affect (r=−0.509; p-value<0.000), whereas displaying a positive association with positive affect (r=0.403; p-value<0.000). However, an exclusively significant association was observed between negative affect and PRBT (r=0.359; p-value<0.000), with positive affect showing no significant relationship to such procrastination. The associations between predictor and mediator variables at the same point did not exceed 0.7, demonstrating any evidence of multicollinearity.
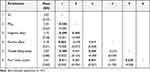 |
Table 2 Bivariate Correlations Among SC, PRBT, Positive/Negative Effect, and Sleep Quality in Survey I |
Mediating Effects of SC on PRBT Through Negative Affect
Due to the absence of a correlation between positive affect and PRBT, the multiple mediation model originally intended for analysis was discarded and a simple mediation model utilizing negative affect was subsequently assessed. The statistical relevance of the mediating effects of SC on PRBT via negative affect was also examined. The study assessed the statistical relevance of mediating the effects of SC on PRBT via negative affect. This was performed utilizing macro-PROCESS SPSS by drawing 10,000 bootstrapped replications with bootstrapped confidence intervals to determine the mediating effect. Cohen’s kappa measure (κ) was applied to evaluate how much negative effect accounted for the variation between SC and PRBT. This particular metric is not contingent upon the sample size and serves as an approximation of the optimum proportion of the mediating effect that is present and explainable via indirect means, specifically through a mediator.40 The outcomes showed SC had significantly mediated effects on PRBT due to negative affect, as expected, resulting in 9% of the overall model’s variability in PRBT. A moderate association was observed between SC and PRBT, with almost 8% of the variance in the latter being attributed to negative affect (Table 3).
 |
Table 3 Mediating Effects of SC on PRBT Through Negative Affect in Survey I |
Survey II
In the second phase of the study, we extended the aforementioned model (Survey I) by incorporating cognitive reappraisal as a predisposing factor for both positive and negative affect, aiming to empirically examine the hypothesis that individuals with SC exhibit reduced tendencies to procrastinate at bedtime due to their proficient ability to regulate emotions in a healthy manner. Cognitive reappraisal was selected as the preferred emotion regulation strategy due to compelling evidence that it successfully diminishes negative affect and, although to a lesser extent, enhances positive affect.41 Furthermore, a significant association has been established in prior research between SC and the employment of cognitive reappraisal in mitigating negative mood.42
Methods
Participants
A cohort of 546 individuals successfully participated in an online survey. In this particular sample, 36 participants who exhibited characteristics indicative of clinical insomnia and 19 participants who had not provided complete responses on the insomnia measure were excluded. Finally, an aggregate of 491 individuals were included in the sample, with a mean age of 29.54 years and a standard deviation of 8.5. The majority of participants were female, accounting for 85.3% of the total sample.
Procedure
A convenience sampling method was employed to recruit participants for the investigation. Recruitment efforts were made by sending emails to a volunteer list consisting of university students, posting notices on various social media platforms, and placing advertisements on online psychology websites. Participants were asked to complete an online survey after indicating their agreement to provide informed consent. All individuals involved in the survey were provided with an opportunity to potentially receive a gift voucher valued at 5000 PKR. The data collection period spanned from December 2022 to February 2022.
Questionnaire
Demographics
In Survey II, participants were asked to provide demographic information related to their age and gender. Furthermore, they were presented with the PRBT scale, which had been previously utilized in Survey I. In addition to these measures, participants were also presented with the accompanying assessments.
Self-Compassion and Affect
The individuals were administered the brief 12-item SCS43 and a brief 10-item PANAS-X38 measure, which was provided to them as a visual analog measure (6: negative affect adjectives and 4: positive affect adjectives). Ratings were assigned on an 8-point Likert scale ranging from not at all as “1” to extremely as “8”. Measures from the PANAS-X were selected to represent guilt and distress, two affective disorders shown to be associated with procrastination, for negative affect.44,45 To elicit positive affect, the selection of items was based on their ability to evoke positive self-consciousness (ie, pride), as well as future-oriented affective disorders (ie, pride and inspiration). This decision was made due to the established connection between these variables and decreased inclination toward procrastination.46,47 An auxiliary measure was selected to express gratitude and a positive affective state connected to regular sleeping habits.48 Participants also accomplished the subsequent auxiliary item specifically designed for this investigation.
Insomnia
The Insomnia Severity Index (ISI) is a validated instrument comprised of seven items designed to assess and diagnose insomnia as well as evaluate various aspects of sleep difficulties.49 The assessed items are systematically evaluated using a five-point Likert scale, inclusive of values ranging from 0 to 4. This rating scale is employed in two distinct sets for evaluation. The initial set of three queries assesses the intensity of symptoms associated with insomnia, ranging from none to extremely severe. Subsequently, the following four queries aim to evaluate individuals’ perceptions of sleep issues, encompassing distress, dissatisfaction, noticeable, and the impact of sleep problems.
Emotion Regulation
The variability among individuals in utilizing emotion regulation strategies was achieved by employing the Emotion Regulation Questionnaire (ERQ),23 encompassing a total of ten items which are further categorized into two distinct strategies ie, (1) cognitive reappraisal (consisting of 6 items) and (2) expressive suppression (consisting of 4 items). The items are evaluated using a 7-point Likert scale that ranges from 1: strong disagreement to 7: strong agreement. Subsequently, scores for each subscale are computed by taking the average, whereby higher scores suggest a higher degree of utilization of the emotion regulation strategy. In the present investigation, the emphasis was placed solely on scrutinizing the cognitive reappraisal subscale. This deliberate focus was motivated by prior studies that have presented evidence linking the cognitive reappraisal subscale to the constructs of SC, as well as positive and negative affect.41,42
Ethical Approval
All procedures performed in studies involving human participants followed the ethical standards of the Research Ethics Board of the Quaid-e-Azam University, Pakistan, and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards (Approval No. QUI/2022-0729). Informed consent was obtained from all individual participants included in the study.
Analytical Procedure
The study employed correlation analyses to examine the hypothesized associations among SC, cognitive reappraisal, positive and negative affect, and PRBT. In the realm of multivariate analyses, we hypothesized that SC bears a correlation with augmented cognitive reappraisal. This correlation, in turn, is hypothesized to result in heightened positive affect and diminished negative affect. Furthermore, such emotional states are anticipated to lead to a reduction in the tendency to engage in PRBT. The statistical analysis included the variables of age and gender of the participants in the model. The study utilized the full-information maximum likelihood (FIML) estimation techniques, as suggested by Arbuckle.50 We explored the effects of SC on PRBT, including its composite, direct, and mediating effects. We also examined the direct effects of SC on reappraisal, positive affect, and negative affect, as well as the direct effects of these variables on PRBT. The saturated path model had uninformative fit indices. Hence, our main focus was on the decomposition of self-compassion’s overall predictive effects on PRBT into direct and mediating effects. The mediating effects were assessed using the biased-corrected bootstrap method, employing 10,000 resamples and constructing the 95% bias-corrected confidence intervals (CIs). This technique offers an enhanced level of precision in achieving a balanced trade-off between type-1 and type-2 errors, as compared to alternative approaches employed to evaluate indirect effects.51 The analyses were done using SPSS (v.26) and AMOS (v.24).
Results
Common Method Deviation Analysis
To predict common method bias variation among the scale items, we estimated Harman’s single-factor test. The findings showed that the total variance explained by the first factor was 27.16% which was below the threshold of 40%, indicating no issue of common method deviation among the items on the questionnaire.
Reliability and Validity Analysis of the Questionnaire in Survey II
Table 4 illustrates the findings of the reliability analysis, as well as the assessment of discriminant and divergent validity for the psychometric constructs. The reliability analysis was evaluated through the utilization of Cronbach’s alpha coefficient and McDonald’s omega. The assessment of construct validity involved the examination of model fit statistics and the average variance extracted index (AVE). The results of the study demonstrated a satisfactory degree of reliability and validity to the SCS, ERQ, PRBT, PSQI, and PANAS-X scales.
 |
Table 4 Dicriminant validity, Reliablity, and Construct Validity Analysis results (Survey II) |
Descriptive and Bivariate Correlation Analysis of the Variables
All variables in the study exhibited a normal distribution, as evidenced by the skewness and kurtosis values falling within the range of −1 to +1. To attenuate the impact of outliers on analytical procedures, we substituted any values exceeding 3 standard deviations above the mean of the group with a value equivalent to the group mean incremented by 3 standard deviations. The current study provides a tabular presentation of descriptive statistics and the correlations observed among all study variables under investigation in Table 5. The findings of the study demonstrated a positive correlation between SC, positive affect, cognitive reappraisal, and age. On the contrary, SC exhibited a negative correlation with negative affect and PRBT. Likewise, the findings demonstrate a positive correlation between cognitive reappraisal and positive affect while uncovering a negative correlation between negative affect and PRBT. The study found a significant association between positive affect and reduced levels of negative affect and PRBT, as well as a positive correlation with age. Conversely, negative affect demonstrated a positive link with increased PRBT, particularly among younger individuals. The findings of this study demonstrate a negative correlation between PRBT and age.
 |
Table 5 Bivariate Correlations Among SC, Cognitive Reappraisal, Positive/Negative Affect, and PRBT (Survey II) |
Multivariate Analysis of the Effects of SC on PRBT Through Cognitive Reappraisal and Negative Affect
Table 6 depicts the outcomes of the path model analysis examining the impact of SC on PRBT, mediated by cognitive reappraisal and negative affect (Survey II). According to the statistics, the path model was able to explain 15% of the variability in PRBT. In addition, cognitive reappraisal and negative affect were significant predictors, accounting for 21.0% and 24.0% of the variability, respectively, in PRBT. Conversely, positive affect accounted for 19.0% of the variability in PRBT. After controlling for the confounding variables of age and gender, it was found that SC exhibited a significant and positive correlation with reappraisal. Additionally, SC was associated with elevated levels of positive affect and decreased levels of negative affect. The findings also indicate a significant negative correlation between SC and PRBT. The cognitive reappraisal measure was found to be positively correlated with heightened levels of positive affect and negatively correlated with reduced levels of negative affect. The study findings indicated that there was no significant correlation between positive affect and the tendency to procrastinate at bedtime. However, it was observed that individuals experiencing negative affect exhibited a higher tendency to engage in PRBT. In regards to indirect impacts, the attribute of SC exhibited notable and adverse indirect connections with PRBT, mediated by the cognitive strategy of reappraisal and the experience of negative affect. Following the suggestions put forth by Simmons et al,52 path analysis was conducted without incorporating any covariates into the model, resulting in insignificant disparities in the findings.
 |
Table 6 Multivariate Analysis of the Effects of SC on PRBT Through Cognitive Reappraisal and Negative Affect (Survey II) |
Discussion
In two empirical investigations, individuals with elevated levels of SC exhibited greater levels of positive affect while concurrently demonstrating decreased levels of negative affect. Moreover, these individuals demonstrated a decreased tendency to engage in procrastination behaviors specifically concerning bedtime activities. In general, the results exhibited congruity with our hypothesized perspective on emotion regulation. It was observed that individuals who displayed higher levels of SC manifested a reduced tendency to engage in delaying bedtime activities, primarily due to lower levels of negative affect. However, it is noteworthy that heightened positive affect did not demonstrate a significant influence on PRBT among these self-compassionate individuals. Significantly, the path analysis conducted in Survey II revealed that the impact of SC on PRBT is mediated, to some extent, by the utilization of cognitive reappraisal. Cognitive reappraisal is recognized as an adaptive technique for regulating emotions, which in turn is associated with diminished levels of negative affect. However, it is noteworthy that the significant relationship between SC and not staying up later than intended is not exclusively attributable to the indirect effects mediated by negative affect or the direct effect on PRBT. This indicates that there may be additional factors besides possessing an efficient emotion regulation pattern that contribute to self-compassionate individuals’ ability to adhere to their intended bedtime.19 The results of our investigation provide empirical evidence that supports and builds upon existing theoretical perspectives and prior research regarding the relationship between SC and health-promoting practices. This study confirmed that SC demonstrates a significant association with reduced instances of PRBT, which is deemed a crucial behavior in sleep. This study contributes to a growing body of evidence that suggests practicing SC can be advantageous not only for promoting significant health-related practices but also for mitigating behaviors that undermine health.13,15,53 When considering the repercussions of delaying bedtime on the duration of sleep and the resulting fatigue experienced throughout the day, as well as the potential impact of inadequate sleep on overall health, it can be argued that PRBT manifests as a sleep-related behavior that potentially undermines one’s health.26,30,31
It can be inferred from the results of this investigation that the relationship between SC and PRBT is more closely linked to the presence of a low negative affect as opposed to a high positive affect. The current discursive debate surrounding the underlying framework of the SC concept offers a plausible rationale for the aforementioned result. Several scholars have argued that the measurement of SC through the SCS should consider the positive (SC) and negative (self-criticism) aspects as distinct and separate constructs, rather than treating them as a singular entity.1,54,55 In a notable demonstration, an extensive meta-analysis incorporating eighteen distinct analyses revealed that the negatively rated items within the SCS exhibited a more robust association with psychopathology in comparison to the positive items. Consequently, this prompted the researchers to propose that the utilization of an overall scale score may exaggerate the connections between SC and negative affective disorders.56 An investigation of the factor structure of the SCS using twenty distinct samples contrasting six-factor, one-factor, and bi-factor modeling revealed that bi-factor modeling had poor fit in all samples, while single-factor modeling predicted 95% of the item variability.57 Conversely, it is plausible to posit that the correlation between SC and PRBT is elucidated more by theoretical grounds related to emotion regulation, as opposed to empirical grounds concerning the validity of the scale. This substantiates the premise that negative affect, rather than positive affect, serves as an explanatory factor in elucidating the stated relationship.
Prior investigations have explored the extent to which SC may be linked to health-related practices, considering the presence of positive and negative affect. These findings imply a potential association between SC and effective management of emotions that promote well-being.13,25 This study is the first of its kind to explore the relationship between emotion regulation, and the positive affective states that connect SC with health-related practices. Cognitive reappraisal entails the act of interpreting a situation that has the potential to evoke emotions in a manner that alters its emotional influence.23 From an emotional regulation standpoint, the present findings correlate with the concept that individuals characterized by SC engage in the cognitive reappraisal of difficulties and possible stress-inducing factors as less distressing and unpleasant. Thus, they effectively diminish their negative emotional responses.19 Consequently, the aforementioned outcome may diminish the necessity to partake in delaying bedtime as a strategy to rectify negative affect.
The existing study further enhances our comprehension of PRBT through its integration within the framework of emotion regulation, specifically focusing on the cognitive reappraisal strategy. Examining the results from an alternative perspective, it is observed that individuals with lower levels of SC demonstrate reduced utilization of cognitive reappraisal, thereby experiencing elevated levels of negative mood. Furthermore, they exhibit an increased tendency to engage in PRBT. This evidence lends some credence to the notion that PRBT may fulfill a role in regulating mood. A prior investigation has demonstrated that participation in entertaining pursuits, such as the observation of amusing feline videos, exhibits a hedonistic propensity, characterized by the restoration of affirmative emotional states and the provision of alleviation from stress. However, when the underlying reason for engaging in such behavior is to evade imperative responsibilities, such as adhering to a disciplined sleep schedule, it is plausible that sentiments of culpability will supplant those of pleasurable gratification.58 From this perspective, the act of delaying bedtime can be construed as a transitory method of managing one’s emotions, comparable to the broader concept of procrastination, ultimately resulting in negative implications for one’s health.13,32
In light of the persistent statistical significance of self-compassion’s direct impact, our research further suggests that individuals who possess higher levels of SC exhibit a decreased propensity to PRBT due to factors unrelated to affective conditions and the regulation of emotions. One possible manifestation of self-kindness and ensuring adequate sleep is the conscientious act of PRBT. Studies examining the concept of mindfulness, which is a key element in SC, also propose that the efficacy of sleep regulation may elucidate the observed direct impacts. In an empirical investigation conducted on undergraduate students, the practice of mindfulness exhibited a significant correlation with various patterns of healthful sleep-regulating conducts and measures. This includes a reduction in pre-sleep arousal.59 Likewise, individuals who exhibit SC may possess superior skills in effectively preparing themselves to attain a restful night’s sleep. This may involve the intentional avoidance of interactions with potential distractions to prevent indulging in PRBT. Additional research is warranted to investigate alternative explanations, including those beyond the scope of the current study, to obtain a comprehensive understanding of the factors underlying the propensity of self-compassionate individuals to refrain from engaging in PRBT.
There is a mounting body of empirical research advocating that SC could be augmented via deliberate guidance and targeted interventions.16 These approaches have exhibited effectiveness in mitigating deleterious health risk behaviors, including but not limited to binge eating,60 tobacco use,53 consuming alcohol,61 and other detrimental conduct.11 Despite the seemingly insignificant extent to which SC elucidates the variance in PRBT, as observed in both investigations, it can be considered comparable to prior research wherein SC accounted for approximately 6% of the variability in a composite measure incorporating various health-related practices, such as sleep patterns.13 Previous studies have established the clinical significance of modest alterations in SC, which have proven efficacious in mitigating detrimental health practices such as alcohol consumption and tobacco smoking.53 In light of the aforementioned statistics, the present research outcomes offer initial indications supporting the notion that fostering SC in reaction to the everyday stressors and disappointments that may undermine one’s emotional state and perpetuate the tendency to delay sleep could potentially serve as an effective method for decreasing this deleterious sleep-related conduct.
Limitations and Future Directions
We need to take several limitations into account when interpreting the results of this study. First, the sole emphasis in the present investigation was placed on examining cognitive reappraisal. Based on the available cross-sectional nature of the data, the suggested causal relationships between SC and affect cognitive reappraisal, and PRBT cannot be definitively validated. Considering the constraints inherent in our research design, there exists the potential for individuals experiencing sleep deprivation to encounter challenges with cultivating SC and may instead demonstrate a tendency towards self-criticism. Furthermore, it is noteworthy that the association between emotion regulation and sleeping patterns can exhibit a reciprocating and mutually enhancing nature. This implies that there may exist more intricate connections between emotion regulation and the act of delaying bedtime than those originally posited in the present investigation. Therefore, it is highly recommended that further investigations be conducted to thoroughly examine our model utilizing empirical and/or observational data to establish the chronological cause-effect relationship proposed by our model. The present investigation is subject to an important limitation, ie, the disproportionate representation of female participants. This discrepancy may have introduced bias or discrimination that influenced the findings of the study. Besides, the convenience sampling choice may not be representative of the broader population along with a higher risk of bias and low representativeness. However, this choice has been made due to constraints on time, budget, and access to the population of interest. So, we emphasize the need for future investigations that use more rigorous sampling methods to confirm or extend the findings of our research.
Several additional concerns stemming from the longitudinal approach of our research encompass the reliance on retrospective self-reported information of PRBT, as well as the evaluation of affect at a solitary and static timeframe, rather than immediately preceding the occurrence of PRBT conduct. This particular perspective may be perceived as suboptimal in evaluating the suggested contributions of affect (positive/negative) and emotion regulation in the associations between SC and procrastinating in going to bed. Nonetheless, a premise supposition rooted in prior scholarly investigations posits that affective states are reasonably steadfast assets that either pose a potential threat or provide fortitude for the self-monitoring and management of health-related conducts.4,25 Thus, one could argue that the single assessment of affect in both studies was primarily indicative of long-lasting affective conditions related to SC. Additional research is warranted to acquire a more in-depth insight into the significance of SC in addressing everyday difficulties, as well as the impact of emotional responses on mitigating the tendency to procrastinate before bedtime.
Conclusion
The findings offer innovative empirical evidence indicating a negative correlation between SC and the proclivity to procrastinate in bed. This relationship is partly explained by the utilization of cognitive reappraisal, an effective strategy in regulating emotions known for its capability to attenuate negative affect. This mood regulation approach related to PRBT offers a novel framework for comprehending and effectively addressing the adverse health consequences associated with this behavior. Previous research on the origins of PRBT has predominantly relied on observational approaches rather than analytical ones, thus rendering this new approach an invaluable opportunity for further investigation and intervention. Additional empirical investigations are indispensable to gain further understanding regarding the prospective benefits of adopting SC and mindfulness as buffering mechanisms for effectively managing daily stressors. Particularly, investigating how these adaptive responses can facilitate individuals in deterring engagement in enjoyable distractions and subsequently aid in adhering to consistent bedtimes.
Data Sharing Statement
The original data used to support the findings of this study are available from the first author upon reasonable request (Shazia Rehman: [email protected]).
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Research Ethics Board of the Quaid-e-Azam University and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards (Approval No. QUI/2022-0729).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Acknowledgment
We would like to thank Dr. Yan Zhang for her invaluable guidance and assistance during the revision phase of the study.
Funding
This study was supported by the National Key Research and Development Program of China (2019YFA0706200), the STI2030-Major Projects (2021ZD0202000), and the Science and Technology Innovation Program of Hunan Province (2023RC3083).
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Neff KD. The development and validation of a scale to measure self-compassion. Self Identity. 2003;2(3):223–250. doi:10.1080/15298860309027
2. Terry ML, Leary MR, Mehta S, Henderson K. Self-compassionate reactions to health threats. Personal Soc Psychol Bull. 2013;39(7):911–926. doi:10.1177/0146167213488213
3. Li Y, Deng J, Lou X, Wang H, Wang Y. A daily diary study of the relationships among daily self‐compassion, perceived stress and health‐promoting behaviours. Int J Psychol. 2020;55(3):364–372. doi:10.1002/ijop.12610
4. Sirois FM. Perfectionism and health behaviors: a self-regulation resource perspective. In: Perfectionism, Health, and Well-Being. Springer; 2015:45–67.
5. Molnar DS, Sirois FM, Flett GL, Janssen WF, Hewitt PL. The roles of health behaviors and stress-related processes. In: The Psychology of Perfectionism: Theory, Research, Applications; 2017:200–221.
6. Chang EC, Ivezaj V, Downey CA, Kashima Y, Morady AR. Complexities of measuring perfectionism: three popular perfectionism measures and their relations with eating disturbances and health behaviors in a female college student sample. Eat Behav. 2008;9(1):102–110. doi:10.1016/j.eatbeh.2007.06.003
7. Bluth K, Roberson PN, Gaylord SA, et al. Does self-compassion protect adolescents from stress? J Child Fam Stud. 2016;25:1098–1109. doi:10.1007/s10826-015-0307-3
8. Neff KD, Knox MC. Self-compassion. In: Encyclopedia of Personality and Individual Differences. Springer; 2020:4663–4670.
9. Miller CL, Strachan SM. Understanding the role of mother guilt and self-compassion in health behaviors in mothers with young children. Women Health. 2020;60(7):763–775. doi:10.1080/03630242.2020.1713966
10. Wong MYC, Chung P-K, Leung K-M. The relationship between physical activity and self-compassion: a systematic review and meta-analysis. Mindfulness (N Y). 2021;12:547–563. doi:10.1007/s12671-020-01513-4
11. Biber DD, Ellis R. The effect of self-compassion on the self-regulation of health behaviors: a systematic review. J Health Psychol. 2019;24(14):2060–2071. doi:10.1177/1359105317713361
12. Sirois FM, Hirsch JK. Big Five traits, affect balance and health behaviors: a self-regulation resource perspective. Pers Individ Dif. 2015;87:59–64. doi:10.1016/j.paid.2015.07.031
13. Sirois FM. Is procrastination a vulnerability factor for hypertension and cardiovascular disease? Testing an extension of the procrastination–health model. J Behav Med. 2015;38:578–589. doi:10.1007/s10865-015-9629-2
14. Homan KJ, Sirois FM. Self-compassion and physical health: exploring the roles of perceived stress and health-promoting behaviors. Health Psychol Open. 2017;4(2):2055102917729542.
15. Dunne S, Sheffield D, Chilcot J. Brief report: self-compassion, physical health and the mediating role of health-promoting behaviours. J Health Psychol. 2018;23(7):993–999. doi:10.1177/1359105316643377
16. Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self‐compassion program. J Clin Psychol. 2013;69(1):28–44. doi:10.1002/jclp.21923
17. Morgan TL, Semenchuk BN, Ceccarelli L, et al. Self-compassion, adaptive reactions and health behaviours among adults with prediabetes and type 1, type 2 and gestational diabetes: a scoping review. Can J Diabetes. 2020;44(6):555–565. doi:10.1016/j.jcjd.2020.05.009
18. Semenchuk BN, Kullman SM, Neilson CJ, et al. Self-compassion, health behaviors, self-regulation, and affective states among individuals at risk of or diagnosed with a chronic disease: a scoping review. Mindfulness (N Y). 2022;13(5):1085–1111. doi:10.1007/s12671-021-01821-3
19. Finlay‐Jones AL. The relevance of self‐compassion as an intervention target in mood and anxiety disorders: a narrative review based on an emotion regulation framework. Clin Psychol. 2017;21(2):90–103. doi:10.1111/cp.12131
20. Mantelou A, Karakasidou E. The effectiveness of a brief self-compassion intervention program on self-compassion, positive and negative affect and life satisfaction. Psychology. 2017;8(4):590–610. doi:10.4236/psych.2017.84038
21. Johnson EA, O’Brien KA. Self-compassion soothes the savage ego-threat system: effects on negative affect, shame, rumination, and depressive symptoms. J Soc Clin Psychol. 2013;32(9):939–963. doi:10.1521/jscp.2013.32.9.939
22. Svendsen JL, Osnes B, Binder P-E, et al. Trait self-compassion reflects emotional flexibility through an association with high vagally mediated heart rate variability. Mindfulness (N Y). 2016;7:1103–1113. doi:10.1007/s12671-016-0549-1
23. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85(2):348. doi:10.1037/0022-3514.85.2.348
24. Preuss H, Capito K, van Eickels RL, Zemp M, Kolar DR. Cognitive reappraisal and self-compassion as emotion regulation strategies for parents during COVID-19: an online randomized controlled trial. Internet Interv. 2021;24:100388. doi:10.1016/j.invent.2021.100388
25. Sirois FM. A self-regulation resource model of self-compassion and health behavior intentions in emerging adults. Prev Med Rep. 2015;2:218–222. doi:10.1016/j.pmedr.2015.03.006
26. Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80(1):40–52. doi:10.1016/j.biopsych.2015.05.014
27. Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005;6(1):23–27. doi:10.1016/j.sleep.2004.06.003
28. Brown FC, Buboltz WC, Soper B. Relationship of sleep hygiene awareness, sleep hygiene practices, and sleep quality in university students. Behav Med. 2002;28(1):33–38. doi:10.1080/08964280209596396
29. Barber L, Grawitch MJ, Munz DC. Are better sleepers more engaged workers? A self‐regulatory approach to sleep hygiene and work engagement. Stress Health. 2013;29(4):307–316.
30. Kroese FM, Nauts S, Kamphorst BA, Anderson JH, de Ridder DTD. Bedtime procrastination: a behavioral perspective on sleep insufficiency. In: Procrastination, Health, and Well-Being. Elsevier; 2016:93–119.
31. Kroese FM, Evers C, Adriaanse MA, de Ridder DTD. Bedtime procrastination: a self-regulation perspective on sleep insufficiency in the general population. J Health Psychol. 2016;21(5):853–862. doi:10.1177/1359105314540014
32. Sirois F, Pychyl T. Procrastination and the priority of short‐term mood regulation: consequences for future self. Soc Pers Psychol Compass. 2013;7(2):115–127. doi:10.1111/spc3.12011
33. Eckert M, Ebert DD, Lehr D, Sieland B, Berking M. Overcome procrastination: enhancing emotion regulation skills reduce procrastination. Learn Individ Differ. 2016;52:10–18. doi:10.1016/j.lindif.2016.10.001
34. Sirois FM, Giguère B. Giving in when feeling less good: procrastination, action control, and social temptations. Br J Soc Psychol. 2018;57(2):404–427. doi:10.1111/bjso.12243
35. Neff KD, Pommier E. The relationship between self-compassion and other-focused concern among college undergraduates, community adults, and practicing meditators. Self Identity. 2013;12(2):160–176. doi:10.1080/15298868.2011.649546
36. Hill VM, Rebar AL, Ferguson SA, Shriane AE, Vincent GE. Go to bed! A systematic review and meta-analysis of bedtime procrastination correlates and sleep outcomes. Sleep Med Rev. 2022;101697. doi:10.1016/j.smrv.2022.101697
37. Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
38. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063. doi:10.1037/0022-3514.54.6.1063
39. Crawford JR, Henry JD. The Positive and Negative Affect Schedule (PANAS): construct validity, measurement properties and normative data in a large non‐clinical sample. Br J Clin Psychol. 2004;43(3):245–265. doi:10.1348/0144665031752934
40. Preacher KJ, Kelley K. Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychol Methods. 2011;16(2):93. doi:10.1037/a0022658
41. Engen HG, Singer T. Compassion-based emotion regulation up-regulates experienced positive affect and associated neural networks. Soc Cogn Affect Neurosci. 2015;10(9):1291–1301. doi:10.1093/scan/nsv008
42. Diedrich A, Hofmann SG, Cuijpers P, Berking M. Self-compassion enhances the efficacy of explicit cognitive reappraisal as an emotion regulation strategy in individuals with major depressive disorder. Behav Res Ther. 2016;82:1–10. doi:10.1016/j.brat.2016.04.003
43. Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the self‐compassion scale. Clin Psychol Psychother. 2011;18(3):250–255. doi:10.1002/cpp.702
44. Blunt A, Pychyl TA. Project systems of procrastinators: a personal project-analytic and action control perspective. Pers Individ Dif. 2005;38(8):1771–1780. doi:10.1016/j.paid.2004.11.019
45. Flett GL, Stainton M, Hewitt PL, Sherry SB, Lay C. Procrastination automatic thoughts as a personality construct: an analysis of the procrastinatory cognitions inventory. J Ration Cogn Ther. 2012;30:223–236. doi:10.1007/s10942-012-0150-z
46. Blouin-Hudon E-MC, Pychyl TA. Experiencing the temporally extended self: initial support for the role of affective states, vivid mental imagery, and future self-continuity in the prediction of academic procrastination. Pers Individ Dif. 2015;86:50–56. doi:10.1016/j.paid.2015.06.003
47. Giguère B, Sirois FM, Vaswani M. Delaying things and feeling bad about it? A norm-based approach to procrastination. In: Procrastination, Health, and Well-Being. Elsevier; 2016:189–212.
48. Wood AM, Joseph S, Lloyd J, Atkins S. Gratitude influences sleep through the mechanism of pre-sleep cognitions. J Psychosom Res. 2009;66(1):43–48. doi:10.1016/j.jpsychores.2008.09.002
49. Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi:10.1016/S1389-9457(00)00065-4
50. Arbuckle JL, Marcoulides GA, Schumacker RE. Full information estimation in the presence of incomplete data. Adv Struct Equ Model Issues Tech. 1996;243:277.
51. MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behav Res. 2004;39(1):99–128. doi:10.1207/s15327906mbr3901_4
52. Simmons JP, Nelson LD, Simonsohn U. False-positive psychology: undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychol Sci. 2011;22(11):1359–1366. doi:10.1177/0956797611417632
53. Kelly AC, Zuroff DC, Foa CL, Gilbert P. Who benefits from training in self-compassionate self-regulation? A study of smoking reduction. J Soc Clin Psychol. 2010;29(7):727–755. doi:10.1521/jscp.2010.29.7.727
54. Martínez-Rubio D, Colomer-Carbonell A, Sanabria-Mazo JP, et al. How mindfulness, self-compassion, and experiential avoidance are related to perceived stress in a sample of university students. PLoS One. 2023;18(2):e0280791. doi:10.1371/journal.pone.0280791
55. Montero-Marín J, Gaete J, Demarzo M, Rodero B, Lopez LCS, García-Campayo J. Self-criticism: a measure of uncompassionate behaviors toward the self, based on the negative components of the self-compassion scale. Front Psychol. 2016;7:1281. doi:10.3389/fpsyg.2016.01281
56. Muris P, Petrocchi N. Protection or vulnerability? A meta‐analysis of the relations between the positive and negative components of self‐compassion and psychopathology. Clin Psychol Psychother. 2017;24(2):373–383. doi:10.1002/cpp.2005
57. Neff KD, Tóth-Király I, Yarnell LM, et al. Examining the factor structure of the Self-Compassion Scale in 20 diverse samples: support for use of a total score and six subscale scores. Psychol Assess. 2019;31(1):27. doi:10.1037/pas0000629
58. Myrick JG. Emotion regulation, procrastination, and watching cat videos online: who watches Internet cats, why, and to what effect? Comput Human Behav. 2015;52:168–176. doi:10.1016/j.chb.2015.06.001
59. Howell AJ, Digdon NL, Buro K. Mindfulness predicts sleep-related self-regulation and well-being. Pers Individ Dif. 2010;48(4):419–424. doi:10.1016/j.paid.2009.11.009
60. Adams CE, Leary MR. Promoting self–compassionate attitudes toward eating among restrictive and guilty eaters. J Soc Clin Psychol. 2007;26(10):1120–1144. doi:10.1521/jscp.2007.26.10.1120
61. Brooks M, Kay-Lambkin F, Bowman J, Childs S. Self-compassion amongst clients with problematic alcohol use. Mindfulness (N Y). 2012;3:308–317. doi:10.1007/s12671-012-0106-5
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
