Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 13
Postural Control Alterations in Children with Mild Forms of Spastic Cerebral Palsy
Authors Özal C , Aksoy S, Kerem Günel M
Received 21 June 2022
Accepted for publication 13 September 2022
Published 23 November 2022 Volume 2022:13 Pages 367—376
DOI https://doi.org/10.2147/PHMT.S378451
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Cemil Özal,1 Songül Aksoy,2 Mintaze Kerem Günel1
1Department of Fundamental Physiotherapy and Rehabilitation, Hacettepe University, Faculty of Physical Therapy and Rehabilitation, Ankara, Turkey; 2Department of Audiology, Lokman Hekim University, Faculty of Health Sciences, Ankara, Turkey
Correspondence: Cemil Özal, Department of Fundamental Physiotherapy and Rehabilitation, Faculty of Physical Therapy and Rehabilitation, Hacettepe University, Ankara, Turkey, Tel +905376054373, Email [email protected]; [email protected]
Purpose: To determine the postural control responses’ differences between children with mild spastic Cerebral Palsy (CP) and children who are typically developing (TD).
Patients and Methods: Children with spastic CP, Level I–II (n=20, mean age=9.42± 4.59 years, 50% girls, 50% boys) and children with TD (N=20, mean age=9.65± 3.03, 55% girls, 45% boys) were included in the study. All participants were evaluated with Computerized Dynamic Posturography, Sensory Organization Test (SOT).
Results: There were differences between children with spastic CP and children with TD in visual and composite balance score of SOT significantly (p< 0.05); there were no differences at vestibular and somatosensory scores of SOT. Children with CP had more postural sway than children with TD (p< 0.05).
Conclusion: There were differences between children with mild CP and TD in terms of postural control responses.
Keywords: Cerebral Palsy, computerized dynamic posturography, balance, postural control, rehabilitation
Introduction
Cerebral palsy (CP) is a common non-progressive neurodevelopmental condition resulting from a brain lesion that occurs before, during, or shortly after birth; causing posture and activity disturbance.1 According to the population-based observational studies as Surveillance of CP in Europe (SCPE) and Australian registry, spastic type is the most common clinical type and nearly 80% of the total CP population is classified as spastic type.2,3
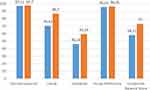 |
Figure 1 Comparison of sensory ratio analysis. Notes: Blue bars: Children with CP. Orange bars: TD children. |
In CP; the clinical features include variable impairments of a wide range of severity that affect daily lives and that persist through the lifespan,4 and postural control (PC) problems are key problems in children with CP and lead to balance and/or orientation inefficiency in children with CP.5,6
PC is the ability to maintain control of the body’s position in space for the dual purposes of postural stability and postural orientation. Postural stability, also described as balance, is the ability to maintain and regain the center of mass (CoM) within the base of support (BoS).6,7
PC is a complicated sensory-motor skill based on interaction between dynamic sensory–motor processes. Sensory processes, including visual, vestibular, and somatosensory systems, create anticipatory and adaptive components of PC. The Central Nervous System (CNS) describes the body position in space, organizing data coming from sensory receptors in the whole body. Each sensor provides specific data about movement and position of the body and creates a reference frame for PC. Peripheral inputs coming from visual, somatosensory, and vestibular systems provide body position perception and movement in space related with position and gravity.8
Today, it is known that children with CP have problems with sensory deficits, muscular weakness, and biomechanical misalignment, all of which lead to problems with PC that adversely affect their performance of daily activities.9 This dysfunction provokes limitations in motor skills that require balance, such as walking, and results in participation limitation in a wide range of daily living aspects including self-care, education, entertainment, and social relationships.9 Therefore, improvement of PC is one of the ultimate aims in physiotherapy and rehabilitation interventions.8,9
Although in assessing the severity of motor impairment seen in CP, a number of scales are used, today the Gross Motor Function Classification System (GMFCS) is the most common and easy to use, being based on the assessment of a child’s level of functionality when performing ultimate motor functions, like walking or with hand hold mobility devices as crutches, walkers, and wheelchairs. Assessment of a child with this system allows us to classify them into five levels of performance.10,11 According to the GMFCS, children in level I and II walk without and with limitations, respectively, and are classified together as mild;12 moreover, according to Horber et al, 13 children classified as level I–II without any comorbidity such as hearing or vision loss are defined as low impairment.
According to findings of studies of typically-developing (TD) children, postural stability and PC responses were related with age and affected by sensory condition. The ability to perform direction adjustments was more evident and sensory maturation occurred in the visual system first, followed by somato-sensory, and functional maturity of the vestibular system is almost reached at 9 years of age and, in general, particularity of PC is differentiated at 7 years of age;14 whereas in children with CP, Rose et al15 indicate that PC in standing is not one of the main problems in the majority of ambulatory children with spastic diplegia, on the other hand, different studies have shown that children with spastic unilateral and bilateral CP have to take a step at lower platform displacement velocities than children with TD peers, stability recovery takes longer time, and center of pressure movement are more at recovery period as well.15 However, it is not well known if and how PC responses are impaired in children with mild involved spastic CP.
Considering the role of PC in the performance of motor skills it is important to understand how PC responses are altered in the CP population, while these dysfunctions lead to important functional constraints. Therefore, it becomes important to assess the balance in these subjects. There are many evaluation protocols, from precise instruments to observational evaluations, with qualitative and quantitative methods. The most precise way to assess PC is posturography, measuring body oscillation during erect posture by means of force platforms.16 Computerized dynamic posturography (CDP) is the gold standard to differentiate between sensory, motor, and central adaptive impairments to PC.8 However, few studies have used this instrument in children with CP. Moreover, Pavao et al17 evaluated the use of sensory information in PC in children with CP and showed that the assessments are mostly static assessments and a significant part of them focuses on somatosensory and visual senses. Therefore, it is important to evaluate PC in children with CP under dynamic conditions. Understanding under which static conditions and under which conditions the level I–III children differ from their peers who TD in balance parameters is important in the development of effective PC interventions.
Therefore, the aim of this study was to evaluate the PC in children with mild spastic CP and to compare them to a group of TD peers. We hypothesized that PC responses are altered in terms of sensory organization, balance, and postural strategies in children with mild spastic CP, and children with mild spastic CP have a lower sensory ratio than TD peers. The PC parameters used to detect PC impairments in the current study may potentially have practical clinical interventions.
Materials and Methods
This study was conducted in accordance with the Declaration of Helsinki. The ethical approval to conduct the study was gathered from Hacettepe University Non-Interventional Clinical Researches Ethical Committee (permission no: HEK11/105, 11.08.2011). An informed consent form regarding the aim and methods of the study was explained to every child and parent and was then signed.
Participants
Children with spastic CP aged 5–8 years who presented to the Hacettepe University, Faculty of Physical Therapy and Rehabilitation between January and June 2012 were included in the study.
The required sample size was calculated using the G*power 3.1 program based on an effect size of dz ¼ 0.5, an error probability of 0.05, and statistical power of 0.80. When calculating the effect of the reference article18 95% confidence (1-α), 95% test power (1-β), d>0.80 (large), the study size was identified as 16 children with CP, but we added 25% to account for possible data loss and finally 20 children with mild spastic CP and 20 TD children were included.
Ten children were classified as level I and 10 were classified as level II according to GMFCS (10 hemiplegic, 10 diplegic) and there were 20 TD children. Inclusion criteria for children with CP were being able to walk without the use of any orthotics, GMFCS level I and II, not having cognitive impairment, not having any vision or hearing loss, and not having undergone Botulinum toxin injections and/or surgical intervention for the musculoskeletal system in the past year. Children who were using any medication or had a systemic disease in addition to CP were not included in the study. Children who had any vision or seizure problem according to the medical reports and records were excluded. Twenty children with TD, without any hearing or vision loss and who participated voluntarily with their parents approved this study. One child per family included into the study and neither child with CP nor TD were undergone to the posturographic study before.
Procedure and Measurements
All data were gathered by the same experienced physiotherapist who did not know the study design. Gender, weight height, and medical history were recorded as demographic characteristics of children. Additionally, spasticity of lower limbs in children with CP were evaluated with Modified Ashworth Scale including muscles of Gastrocnemius, Soleus, Hamstrings, Hip Adductors, and Flexors. The MAS is a 6-point rating scale (0–5) which assesses muscle tone by manually manipulating the joint through its available range of motion and clinically recording the resistance to passive movements.19
Computerized Dynamic Posturography Testing
Computerized Dynamic Posturography (CDP) The NeuroCom® Balance Master™ EquiTest® (NeuroCom International, Inc., Clackamas, OR, USA)20 is a system composed of a moveable dual force platform and a moveable visual surround and was used to evaluate PC of children with CP and TD which is a golden standard evaluation. The Balance Master is a computerized system which analyzes movement on a force plate at real time and provides an objective and comprehensive evaluation of PC. Smart Balance Master (SBM) assesses an individual’s ability to use visual, vestibular, and somatosensory information with dynamic force plate with rotation capabilities to quantify the forces applied vertically through the individual’s feet to evaluate the position of gravity center (COG) and PC; and a dynamic visual environment to evaluate the individual’s use of visual input to keep their balance.21,22 In this study, the Sensory Organization Test (SOT) was used.
Sensory Organization Test
The SOT is a test protocol that evaluates abilities of postural balance under six test conditions in which visual, somato-sensory, and vestibular inputs differ. Inputs delivered to the individual’s eyes, feet, and joints is eliminated with “sway referencing” of both the support surface and visual environment, which tilt to directly follow the individual’s antero-posterior body sway during the test. A balance score determines the amount of the anteroposterior COG and is compared with maximal limits of sway which was calculated for six conditions. Additionally, a composite balance score (CBS) is calculated by the system. The scores range from 0–100, higher values indicate better stability. The six different test conditions were: SOT-1, eyes open on stable surface; SOT-2, eyes closed on stable surface; SOT-3, sway referenced environment, eyes open; SOT-4, sway referenced surface, eyes open; SOT-5, sway referenced surface, eyes closed; SOT-6, referenced surface and environment, eyes open. The static conditions are SOT-1, 2, and 3; while dynamic conditions are SOT-4, 5, and 6. SOT 1 and 2 refer to an individual’s ability to use input from the somato-sensory system and keep balance. SOT-4 and 1 provide objective information about an individual’s ability of the visual system to keep balance. SOT-5 and 1 provide vestibular system input.
SOT task values evaluating corporal stability vary from 0% (null stability) to 100% (maximum stability), and the equilibrium index (EI) is represented by the pondered mean of values obtained during all test conditions with a higher impact of conditions 3–6, somatosensory analysis: ratio of mean values condition 2/condition 1, visual analysis: ratio of mean values condition 4/condition 1, vestibular analysis: ratio of mean values condition 5/condition 1, number of falls (we considered a “fall” to mean the use of arms to support the individual or feet movements to keep balance).23
The SOT consisted of equilibrium score, strategy score, and Center of Gravity Score: Antero-posterior and medio-lateral scores were calculated for each test condition. In this study, two postural adjustment strategies were examined: ankle strategy, that defines relative movements of the ankle, or hip strategy, that defines relative movements of the hip. An equilibrium score is calculated by a software program that identifies the accomplishment of the individual’s sway for each sensory condition.22
Testing Procedure
Prior to testing, subjects were secured in a harness and their stockinged feet were positioned according to the system protocol and instructions.18 Subjects were instructed to maintain a static standing position during testing. Every test condition was repeated three times, and the mean of these trials was used. Each trial lasted 20 seconds. If an individual moved their feet during testing, the examiner repositioned their feet prior to the next trial. Participants were allowed a seated rest between tests at their request. All assessments were completed in the same day. Neither children with CP nor TD children had undergone posturographic assessment before. All tests were performed by the second authors with standard commands and computerized calculation of results.
Statistical Analysis
The statistical software program SPSS for Windows v.21.0 (SPSS Inc., Chicago, IL) was used for data analysis. The Kolmogorov Smirnov test was used to test normal distribution of the variables. Descriptive statistics were calculated for age, height, and body mass index (BMI) and given by the means, standard deviations, were calculated for the SOT scores for each condition, and SOT composite score. Since parametric conditions were not met, Mann–Whitney U-test was used to compare means between groups. p<0.05 was accepted as the statistical significance level.
Results
The mean age of participants was 9.42±4.59 years for children with CP, and 9.65±3.03 for TD children. Ten children with CP were Level I according to the GMFCS and 10 were Level II. There were not any statistically significant differences in characteristics such as age, height, weight, or body mass index (p<0.05) between the CP and TD groups, which is shown in Table 1. The higher muscle tone in the lower limbs of children with CP was in M. Gastrocnemius, in both the left and right sides (Table 2).
 |
Table 1 Participant Characteristics |
 |
Table 2 Distribution of Spasticity in the Lower Limbs of Children with CP |
Findings of SOT
In equilibrium score, children with TD have statistically higher scores (p<0.0) in Conditions 1–4, but in Conditions 5 (sway referenced surface, eyes closed; p=0.2) and 6 (referenced surface and environment, eyes open; p=0.116) they are similar with children with CP.
In strategy score, children with TD have statistically higher scores in all conditions (p<0.01) except Condition 2 (eyes closed on stable surface; p<0.195).
In both antero-posterior and medio-lateral COG alignment, children with CP have statistically higher scores (p<0.05) than TD children, which reflects more postural sway (Table 3).
 |
Table 3 Comparing Findings of Sensory Organization Test of Children with Cerebral Palsy and Typically-Developing Children |
According to comparing of sensory ratio analysis of children with CP and TD, visual score (p=0.004) and composite equilibrium score (p=0.001) were statistically higher in children with TD; however, somatosensory (p=0.321), vestibular (p=0.261), and visual preference (p=0.28) scores were similar (Figure1; Table 4). These findings show children with mild CP have less effective equilibrium and have problems with using visual input to maintain balance.
 |
Table 4 Comparison of Sensory Ratio Analysis of Children with Cerebral Palsy and Typically-Developing Children |
When postural adjustment strategies were examined, 16 (80%) of the children with CP had an abnormal ankle strategy, three (15%) of them had an abnormal hip strategy, and one child had a normal range of postural adjustment strategy; in children with TD, three (15%) of these children had an abnormal ankle strategy and 17 (85%) of them had a normal postural adjustment strategy. The abnormal hip strategies show that children with CP use hip flexion instead of an ankle strategy. When the alignment of COG line was examined, 19 (95%) children with CP had abnormal alignment; regarding the body mass line of these children, nine (45%) of them were right- anterior, four (20%) of them were frontally-anterior, three (30%) were left-anterior, one (5%) was right-posterior, and one (5%) was in normal border. In children with TD, 19 (95%) were in normal border and one (5%) was in anterior.
Discussion
As the result of this study that we conducted, we believe that the PC deficiency in children with CP is one of the reasons of motor dysfunction. Maintaining a stable posture, even during daily functional activities, is challenging because stability demands complex interactions between the sensory system, central nervous system, and musculo-skeletal system.7 Therefore, participation limitations of these children in daily activities, and a detailed evaluation involving the postural responses in children with CP should be performed to develop effective treatment approaches and to evaluate the efficiency of physical therapy and rehabilitation. As a result, we found statistical significance between the children with CP and their healthy peers in terms of PC.
There was no significant difference between the children with CP and children with TD in terms of somatosensory data in our study and values close to each other were found in the groups in terms of CDP somatosensory data. Shumway-Cook and Woollacott24 reported that sensory adaptation problems are not often seen in spastic type CP. Visual-spatial processing and visual kinesthetic integration in CDP has an important role in terms of the continuity of stabilization.25 The ratio between the balance scores obtained from the SOT-1 and SOT-4 in the SOT represents the ability of the individual to use the visual input effectively to maintain balance. When individuals with CP were compared with TD peers in our study, this ratio was found to be significantly lower than in CP patients. The significantly lower SOT-1 and SOT-4 scores in the CP group reflects a problem in the ability of these children to use visual input effectively. The difference between the groups in the ability to use visual input effectively in our study suggests a problem in the processing of vision for PC rather than visual ability itself. It is well documented that visual impairment plays a key role in psychokinetic development of children with CP. Although in the current study children with CP were checked for vision problems, the results underline visuo-perceptual assessment that is very important for balance as well. Therefore, the accurate detection of visual disorders not only leads to a complete clinical diagnosis but also to an appropriate intervention plan.26
The vestibular system is an important and reliable sense in PC as it controls the acceleration of the head in relation to gravity in standing posture and it is critical for balance control.27 When the vestibular CDP data of the CP children was compared with children TD in this study, the vestibular ratio of the CP group was lower compared to children with TD, but this was not statistically significant. The SOT was used for the evaluation of vestibular responses in this study. Although the SOT has provided insight on the vestibular system, it is reported that vestibular function tests should be used to evaluate the contribution of the complex vestibular system to the active postural control.25,27 Steindl et al28 showed that vestibular function development continues even after the age of 15 in their study where the SOT was used. The mean age of the participants in the current study was 9.42±4.59 years in the CP group and 9.65±3.03 years in the TD group, and it is considered that vestibular development was continuing in both groups. CDP provides significant quantitative data on vestibular, visual and somatosensory systems and is important for the clinical evaluation of children. CBS was significantly higher in the TD group than the CP group. Although there was no difference between somatosensory and vestibular data, this significant difference shows inputs coming from the sensory systems can be effective cumulatively in ensuring the balance. Donker et al29 found fluctuations of COG in children with CP is larger than TD children and linked this finding to the balance disorder. We found body sways of the CP group were higher than the TD children in all test positions in our study. Stins et al30 established a relationship between the pathology and balance and reported that as the body sways increases the pathology increases. The data in our study are compatible with this information and the increase in the body swing is characterized with balance disorder. When the CDP, SOT strategy analyzes’ results were evaluated, the ankle movements in the majority of children with CP were found to be abnormal. The hip and ankle movements of only one child with CP were within normal limits. The ankle strategy is the first movement pattern that the body applies to control its perpendicular status while the hip strategy is used for control in a more unstable state.31 Our results show that children with CP cannot adapt their body movements to changing environmental conditions and have poor PC. The use of the hip strategy when the ankle strategy is not effective results in increasing the risk of falls as it is inadequate in providing balance on unstable surfaces in children and also increases energy consumption.31 Additionally, problems in the use of an appropriate strategy cause an inability to fine-tune the postural activity, which may also explain the reduced capacity to manipulate the center of mass. Furthermore, these PC aspects are influenced by the difficulty of the motor task. Therefore, functional activities such as walking and, even more so, running pose an increased challenge for people with CP, potentially making deficits in PC and coping mechanisms more visible.32
Our results show children with CP have difficulties in maintaining balance in different positions. A significant proportion of children with CP showed impaired somatosensory information and anomalies in strategies in the SOT 4th position together with impaired balance between the hip and ankle strategies. Horak33 reported the somatosensory loss results within CP supports, again supporting our study. The strategy findings in our study conducted with CDP are similar to the results obtained by Tedroff et al34 with the electromyographic method. Displacements of COG were evaluated separately for each position of CDP. Displacement of COG was significantly more prominent in the CP group compared to the TD group in all SOT positions, both in antero-posterior direction and medio-lateral directions. The lateral sway was larger in the CP group in SOT 3rd position where the ground is stable and visual screen is moving. Supporting these findings, Donker et al29 and Hsue et al35 found children with CP had a greater postural sway than children with TD. Increased postural sway with visual stimuli can be explained as CP patients trusting visual information more than TD children as in early stages of development. Stins et al30 reported that individuals participating in activities including a combination of balance and intense physical activity had less postural swing. Based on this knowledge, low levels of physical activity can be among the potential causes of the increased postural sways in children with CP. Moreover, recently, Krishnaprasad et al36 investigated the relationship between postural stability and functional activities, and they indicated a good association between postural stability and functional abilities in children with spastic CP. Therefore, to understandthis relationship as well as to develop efficient interventions, it is important to understand how differences in the postural sway between children with CP and TD is quite important.
Although it is known that PC is one of the key problems in children with CP, there are only a few detailed studies on why these problems develop. There is a need for further information in this regard so that all treatment approaches and especially physiotherapy and rehabilitation can be planned efficiently.
Study Limitations
The main limitation of this study was not including children with different types of CP; in the future, beside children with TD, different types of CP may compare in this framework. Another limitation of the study was not investigating the factors that may influence PC mechanisms as deformities, range of motion limitations, and muscle tone problems. Although the current study was based on the golden standard assessment of PC, the lack of assessments during functional activities such as sitting or hand using is an important limitation. Therefore, it is suggested that research in the future may focus on these limitations. The current study has enough samples to compare PC responses between children with CP and TD; however, to compare different GMFCS levels, a larger sample size is needed, which is another limitation.
Conclusions
According to the results of the current study, children with mild CP differs in terms of PC from their TD peers in maintaining balance, use of vision for balance and in postural strategies. Children with CP were in the mild group according to GMFCS, our results have increased in hip strategy even when the ankle strategy can be effective, and that this is a general problem which shows that PC is still a key problem which may have resulted from difficulties in fine tuning mechanism during functional activities requiring balance such as walking on different surfaces. Therefore, in rehabilitation programs it is necessary to include balance and postural strategy training in these children. As the hypothesis of the current study was to determine the differences of children with and without CP, in clinical settings, it has been suggested that these findings might be considered. According to results of this study, children with mild CP differentiate in balance, as well as to using vision for maintenaining balance. Therefore, a comprehensive and objective assessment is needed for clinical implications.
Acknowledgements
We would like to thank to Yavuz Yakut, PhD. Prof. for his statistical supports.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy. Dev Med Child Neurol. 2007;49:8–14.
2. Galea C, Mcintyre S, Smithers‐Sheedy H, et al. Cerebral palsy trends in Australia (1995–2009): a population‐based observational study. Dev Med Child Neurol. 2019;61(2):186–193. doi:10.1111/dmcn.14011
3. Arnaud C, Ehlinger V, Delobel-Ayoub M, et al. Trends in prevalence and severity of pre/perinatal cerebral palsy among children born preterm from 2004 to 2010: a SCPE collaboration study. Front Neurol. 2021;12. doi:10.3389/fneur.2021.624884
4. Smithers-Sheedy H, Badawi N, Blair E, et al. What constitutes cerebral palsy in the twenty-first century? Dev Med Child Neurol. 2014;56:323–328. doi:10.1111/dmcn.12262
5. Abd El-Nabie WA, Attia A. Immediate effect of maximal treadmill walking on muscle fatigue and postural stability in children with cerebral palsy. Bull Faculty Phys Ther. 2019;24(2):79. doi:10.4103/bfpt.bfpt_26_18
6. Ozal C, Ari G, Kerem Gunel M. Inter–intra observer reliability and validity of the Turkish version of Trunk Control Measurement Scale in children with cerebral palsy. Acta Orthopaedica et Traumatologica Turcica. 2019;53(5):381–384. doi:10.1016/j.aott.2019.04.013
7. Pavão SL, Dos Santos AN, Woollacott MH, Rocha NA. Assessment of postural control in children with cerebral palsy: a review. Res Dev Disabil. 2013;34(5):1367–1375. doi:10.1016/j.ridd.2013.01.034
8. Trueblood PR, Rivera M, Lopez C, et al. Age-based normative data for a computerized dynamic posturography system that uses a virtual visual surround environment. Acta Otolaryngol. 2018;138(7):597–602. doi:10.1080/00016489.2018.1429653
9. de Araújo PA, Starling JMP, Oliveira VC, et al. Combining balance-training interventions with other active interventions may enhance effects on postural control in children and adolescents with cerebral palsy: a systematic review and meta-analysis. Braz J Phys Ther. 2020;24(4):295–305. doi:10.1016/j.bjpt.2019.04.005
10. Palisano RJ, Cameron D, Resenbaum PL, et al. Stability of the gross motor function classification system. Dev Med Child Neurol. 2006;48(6):424–428. doi:10.1017/S0012162206000934
11. Sadowska M, Sarecka-Hujar B, Kopyta I. Cerebral palsy: current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat. 2020;16:1505–1518. doi:10.2147/NDT.S235165
12. Kruse A, Schranz C, Tilp M, Svehlik M. Muscle and tendon morphology alterations in children and adolescents with mild forms of spastic cerebral palsy. BMC Pediatr. 2018;18(1):1–9. doi:10.1186/s12887-017-0974-x
13. Horber V, Fares A, Platt MJ, et al. Severity of cerebral palsy—the impact of associated impairments. Neuropediatrics. 2020;51(02):120–128. doi:10.1055/s-0040-1701669
14. de Sá CD, Boffino CC, Ramos RT, Tanaka C. Development of postural control and maturation of sensory systems in children of different ages a cross-sectional study. Braz J Phys Ther. 2018;22(1):70–76. doi:10.1016/j.bjpt.2017.10.006
15. Rose J, Wolff DR, Jones VK, et al. Postural balance in children with cerebral palsy. Dev Med Child Neurol. 2002;44:58–63. doi:10.1017/S0012162201001669
16. Lopes GHR, David ACD. Posturography in the analysis of postural control in children with cerebral palsy: a literature review. Fisioterapia e Pesquisa. 2013;20:97–102. doi:10.1590/S1809-29502013000100016
17. Pavão SL, Silva FP, Savelsbergh GJ, Rocha NA. Use of sensory information during postural control in children with cerebral palsy: systematic review. J Mot Behav. 2015;47(4):291–301. doi:10.1080/00222895.2014.981498
18. Bickley C, Linton J, Sullivan E, Mitchell K, Slota G, Barnes D. Comparison of simultaneous static standing balance data on a pressure mat and force plate in typical children and in children with cerebral palsy. Gait Posture. 2019;67:91–98. doi:10.1016/j.gaitpost.2018.08.012
19. Numanoglu A, Kerem Gunel M. Intraobserver reliability of modified Ashworth scale and modified Tardieu scale in the assessment of spasticity in children with cerebral palsy. Acta Orthopaedica et Traumatologica Turcica. 2012;46(3):196–200. doi:10.3944/AOTT.2012.2697
20. Woollacott MH, Shumway-Cook A. Postural dysfunction during standing and walking in children with cerebral palsy: what are the underlying problems and what new therapies might improve balance? Neural Plast. 2005;12(2–3):211–219. doi:10.1155/NP.2005.211
21. NeuroCom International, Inc. Objective Quantification of Balance and Mobility. Clackamas, OR: NeuroCom International, Inc; 2007.
22. Aksoy S, Öztürk B. Bilgisayarlı Dinamik Postürografi, Bulak Burun Boğaz Hastalıklarında İleri Teknoloji [Computerized Dynamic Posturography, Advanced Technology in Otolaryngology]. İstanbul: American Hospital. 2011:32–47.
23. Pedalini MEB, Cruz OLM, Bittar RSM, Lorenzi MC, Grasel SS. Sensory organization test in elderly patients with and without vestibular dysfunction. Acta Otolaryngol. 2009;129(9):962–965. doi:10.1080/00016480802468930
24. Bourelle S, Berge B, Gautheron V, Cottalorda J. Computerized static posturographic assessment after treatment of equinus deformity in children with cerebral palsy. Pediatr Orthopead. 2010;19:211–220. doi:10.1097/BPB.0b013e32832e957a
25. Plandowska M, Lichota M, Górniak K. Postural stability of 5-year-old girls and boys with different body heights. PLoS One. 2019;14(12):e0227119. doi:10.1371/journal.pone.0227119
26. Kozeis N, Jain S. Visual impairment in cerebral palsy. In: Cerebral Palsy. Cham: Springer; 2018:295–302.
27. Black FD. What can posturography tell us about vestibular function? Ann NY Acad Sci. 2001;942:446–464. doi:10.1111/j.1749-6632.2001.tb03765.x
28. Steindl R, Kunz K, Schrott-Fischer A, Scholtz AW. Effect of age and sex on maturation of sensory systems and balance control. Dev Med Child Neurol. 2006;48(6):477–482. doi:10.1017/S0012162206001022
29. Donker SF, Ledebt A, Roerdink M, Savalsbergh GJP, Beek PJ. Children with cerebral palsy exhibit greater and more regular postural sway than typically developing children. Exp Brain Res. 2008;184:363–370. doi:10.1007/s00221-007-1105-y
30. Stins JF, Michielsen ME, Roerdink M, Beek PJ. Sway regularity reflects of expertise, vision and cognition. Gait Posture. 2009;30:106–109. doi:10.1016/j.gaitpost.2009.04.001
31. Hof AL, Duysens J. Responses of human ankle muscles to mediolateral balance perturbations during walking. Hum Mov Sci. 2018;57:69–82. doi:10.1016/j.humov.2017.11.009
32. Rethwilm R, Böhm H, Haase M, Perchthaler D, Dussa CU, Federolf P. Dynamic stability in cerebral palsy during walking and running: predictors and regulation strategies. Gait Posture. 2021;84:329–334. doi:10.1016/j.gaitpost.2020.12.031
33. Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent Falls. Age Ageing. 2006;2006:35-S2, 7–11.
34. Tedroff K, Knutson LM, Soderberg GL. Synergistic muscle activation during maximum voluntary contractions in children with and without spastic cerebral palsy. Dev Med Child Neurol. 2006;48:789–796. doi:10.1017/S0012162206001721
35. Hsue BJ, Miller F, Su FC. The dynamic balance of the children with cerebral palsy and typical developing during gait. Part I: spatial relationship between COM and COP trajectories. Gait Posture. 2009;29:465–470. doi:10.1016/j.gaitpost.2008.11.007
36. Krishnaprasad KM, Narayan A, Kumar KV. Association between postural stability and functional abilities in children with spastic cerebral palsy. Critical Rev. 2022;34(2):67–75.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
