Back to Journals » International Journal of Women's Health » Volume 16
Postoperative Coagulation State Predicts Deep Vein Thrombosis After Cesarean Section in Elderly Pregnant Women
Authors Feng X, Ding L, Zhang S, Zhang H
Received 7 September 2023
Accepted for publication 13 December 2023
Published 22 January 2024 Volume 2024:16 Pages 111—118
DOI https://doi.org/10.2147/IJWH.S439212
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Xiaojie Feng, Lige Ding, Shangzhu Zhang, Huan Zhang
Department of Emergency, Shijiazhuang Obstetrics and Gynecology Hospital, Shijiazhuang, Hebei, People’s Republic of China
Correspondence: Lige Ding, Department of Emergency, Shijiazhuang Obstetrics and Gynecology Hospital, Zhongshan Road, Shijiazhuang, 050000, Hebei, People’s Republic of China, Tel +86-13673113998, Email [email protected]
Introduction: We aimed to evaluate the risk factors for the development of deep vein thrombosis (DVT) within one month after delivery in pregnant women of advanced maternal age undergoing cesarean section and explore the predictive value of fasting coagulation indicators in relation to the development of DVT.
Methods: A total of 176 eligible postpartum women were included in this study. Sixty-seven cases developed DVT within one month after delivery (DVT group), while 109 cases did not experience DVT (NDVT group). Within 24 hours after cesarean section, fasting coagulation indicators are measured. Coagulation system analysis was performed using the STA-R Evolution fully automated coagulation analyzer.
Results: The women who developed DVT were found to be older, had a higher proportion of women with previous childbirth experiences, and had a higher proportion of women with comorbidities. Our results revealed significant differences in the levels of activated partial thromboplastin time and prothrombin time between the NDVT group and the DVT group. In contrast, the DVT group displayed significantly higher levels of D-dimer, plasma fibrinogen and platelet count when compared to the NDVT group. The AUC for the combined test model was substantially higher compared to individual parameters.
Discussion: Multiple parameters of the postoperative coagulation state in the combined test model provided a more accurate prediction of DVT occurrence in elderly pregnant women after cesarean section.
Keywords: deep vein thrombosis, cesarean section, coagulation, postpartum women
Introduction
Venous thromboembolism (VTE) refers to the abnormal blood coagulation within veins, leading to vessel obstruction and impaired venous return. The global incidence of VTE in pregnant women ranges from 0.1% to 0.2%, which is five times higher than that in non-pregnant women of the same age, and the incidence increases 60 times in postpartum women.1,2 VTE is one of the leading causes of maternal mortality worldwide.3,4 VTE can occur in various veins throughout the body, with both deep venous thrombosis (DVT) and pulmonary thromboembolism (PE) having high early morbidity and mortality rates.3,5
In China, it is a cultural practice for postpartum women to undergo a “lying-in” rest lasting around 30 to 40 days after giving birth. During the “lying-in” rest period, women aim to spend significant time seated or reclined on the bed. However, the previous study found that the highest risk of VTE occurs during the initial three weeks after childbirth.6 In addition, the prevalence of pregnancies in advanced maternal age (age above 35 years) has been steadily increasing.7 Pregnant women with advanced maternal age are more prone to thrombotic events due to physiological changes associated with ageing and the increased prevalence of comorbidities.8,9 Cesarean section is also recognized as a risk factor for VTE, mainly when performed as an emergency procedure.10,11 Advanced maternal age is usually associated with the rate of cesarean delivery.9 Therefore, advanced maternal age, cesarean delivery and the practice of ‘lying-in’ rest seem to be risk factors contributing to the pathological basis for the development of VTE.
In our study, we aimed to evaluate the risk factors for the development of DVT within one month after delivery in pregnant women of advanced maternal age undergoing cesarean section. Early prevention, diagnosis and treatment are the leading measures to reduce VTE-related maternal deaths. We examined the relationship between fasting coagulation indicators, including activated partial thromboplastin time (APTT), prothrombin time (PT), plasma fibrinogen (FIB), plasma D-dimer (D-D), platelet count (PLT), and the occurrence of DVT. Furthermore, we aimed to explore the predictive value of the combined detection of these indicators in relation to the development of DVT.
Materials and Methods
Inclusion and Exclusion Criteria
Inclusion criteria: women with 1. advanced maternal age, age ≥35 years; 2. full-term pregnancy, after 39 weeks; 3. indication for cesarean section and completion of delivery by cesarean section; 4. no history of lower limb surgery within the past year; 5. preoperative ultrasonography without lower limb DVT.
Exclusion criteria: women with 1. presence of chronic liver or kidney dysfunction, malignant tumors, or blood disorders; 2. history of surgery or trauma within the three months; 3. prior to delivery; 4. receiving medication during pregnancy that affects blood clotting function.
Participants
This study was approved by the ethics committee of Shijiazhuang Obstetrics and Gynecology Hospital. Informed consent was obtained from all participants and their family members. All methods were performed following the relevant guidelines and regulations. The study complies with the Declaration of Helsinki, Ethical Principles for Medical Research Involving Human Subjects.
A total of 176 eligible postpartum women enrolled in Shijiazhuang Obstetrics and Gynecology Hospital were included in this study. If postpartum women exhibited symptoms such as leg swelling, skin redness, dizziness, or difficulty breathing, CT venography was conducted to confirm the presence of DVT. For asymptomatic postpartum women, CT venography was performed within one month after delivery to ascertain the presence of DVT. Among the participants, 67 cases developed DVT within one month after delivery (DVT group), while 109 cases did not experience DVT (NDVT group).
Measurement
Within 24 hours after cesarean section, fasting coagulation indicators are measured, including activated partial thromboplastin time (APTT, Manassas, VA), PT, plasma FIB, plasma D-D, and PLT. Coagulation system analysis was performed using the STA-R Evolution fully automated coagulation analyzer. The analyzed parameters included APTT (reference range: 21–37 seconds), PT (reference range: 9–15 seconds), FIB (reference range: 2.00–4.00 g/L), D-dimer (reference range: 0–0.50 μg/mL), and PLT measured in the complete blood count (normal range: 100–300 × 109/L).
Statistical Analysis
Statistical analyses were performed by SPSS software (version 22.0, SPSS Inc., USA). The data were presented as mean ± standard deviation (SD) or number (n) and proportion (%). Sample size was determined using established statistical power analysis tool (power and sample size collection). The prediction value was evaluated by non-parametric receiver operating characteristic (ROC) analyses. The area under the curve (AUC) showed diagnostic accuracy. P < 0.05 was considered statistically significant.
Results
Univariate Analysis of Clinical Factors for DVT After Delivery
This study included 176 eligible postpartum women, among whom 67 developed DVT within one month after delivery, while 109 did not develop DVT. A comparison was made between the clinical data of the two groups of women, including age, body mass index (BMI) at the time of delivery, gestational age, primiparity (whether it was their first childbirth), multiple pregnancies, history of venous thromboembolism, presence of preeclampsia or gestational diabetes, abnormal blood lipids, and coagulation-related indicators.
The results revealed several significant differences between the women who developed DVT and those who did not (Table 1). The women who developed DVT were found to be older, had a higher proportion of women with previous childbirth experiences, and had a higher proportion of women with comorbidities such as gestational diabetes and preeclampsia. Additionally, significant differences were observed in the coagulation-related indicators between the two groups.
 |
Table 1 Univariate Analysis of Clinical Factors for Deep Vein Thrombosis (DVT) After Delivery in Elderly Pregnant Women Who Delivered by Cesarean Section |
Independent Risk Factors for DVT After Cesarean Section in Advanced Maternal Age
Table 2 presents a multivariate analysis of risk factors for postpartum DVT following cesarean section in elderly pregnant women. The occurrence of DVT was used as the dependent variable (DVT = 1, non-DVT = 0), while the variables with significant differences identified in Table 1 were treated as independent variables. The aim was to analyze the risk factors associated with DVT formation in elderly primiparous women after cesarean section.
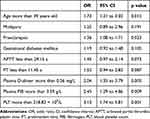 |
Table 2 Multivariate Logistic Analysis for Deep Vein Thrombosis (DVT) After Delivery in Elderly Pregnant Women Who Delivered by Cesarean Section |
The results indicated that being aged 39 years or older, having comorbid preeclampsia, a plasma D-dimer level greater than 0.56 mg/L, a plasma fibrinogen (FIB) level exceeding 3.59 g/L, and a platelet count (PLT) higher than 218.82 × 10^9/L were identified as independent risk factors for postpartum DVT following cesarean section in elderly pregnant women.
The result suggests that advanced maternal age, the presence of preeclampsia, elevated levels of plasma D-dimer and FIB, and an increased platelet count are associated with an increased risk of DVT formation in this population.
Differences of Coagulation and Platelet-Related Parameters Between DVT and NDVT Group
Figure 1 illustrates the comparisons of various coagulation and platelet-related parameters within 24 hours after surgery between elderly pregnant women who underwent cesarean section and experienced DVT (DVT) and those who did not develop DVT (NDVT). The parameters measured include APTT, PT, D-dimer, FIB and PLT (Figure 1a–e).
The results indicated that the APTT and PT levels were significantly higher in the NDVT group compared to the DVT group (p = 0.002, p < 0.001, respectively). Conversely, the DVT group exhibited significantly higher levels of D-dimer, FIB and PLT than the NDVT group (p < 0.001).
These findings suggest significant differences in coagulation and platelet-related parameters between elderly pregnant women who developed DVT after cesarean section and those who did not.
The Effectiveness of Predicting the Occurrence of DVT Following Cesarean Section in Elderly Pregnant Women After Delivery
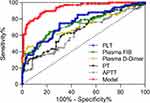
Figure 2 and Table 3 present the receiver operating characteristic (ROC) analysis of various coagulation and platelet-related parameters: APTT, PT, D-dimer, FIB, PLT and their combined test model, for predicting the occurrence of DVT after delivery in elderly pregnant women who underwent cesarean section.
 |
Table 3 Predictive Values in ROC Analysis |
The factors for the combined predictive model were obtained through SPSS analysis and calculated as follows:  . The sensitivity, specificity, and maximum Youden index of the combined test model were determined as 86.57%, 85.32%, and 0.72, respectively (Table 3). The ROC analysis results revealed the area under the curve (AUC) for APTT, PT, D-dimer, FIB, PLT, and the combined test model to predict the occurrence of DVT in elderly pregnant women after cesarean section. The AUC values were found to be 0.64, 0.68, 0.72, 0.75, 0.76, and 0.94, respectively. Notably, the AUC for the combined test model was higher than that of APTT, PT, D-dimer, and FIB individually, indicating that the combined test model incorporating multiple parameters provided a more accurate prediction of DVT occurrence in elderly pregnant women after cesarean section.
. The sensitivity, specificity, and maximum Youden index of the combined test model were determined as 86.57%, 85.32%, and 0.72, respectively (Table 3). The ROC analysis results revealed the area under the curve (AUC) for APTT, PT, D-dimer, FIB, PLT, and the combined test model to predict the occurrence of DVT in elderly pregnant women after cesarean section. The AUC values were found to be 0.64, 0.68, 0.72, 0.75, 0.76, and 0.94, respectively. Notably, the AUC for the combined test model was higher than that of APTT, PT, D-dimer, and FIB individually, indicating that the combined test model incorporating multiple parameters provided a more accurate prediction of DVT occurrence in elderly pregnant women after cesarean section.
Discussion
Virchow’s triad believed that blood in a hypercoagulable state, along with endothelial damage and stagnant blood flow, can lead to intravascular coagulation, which is the pathological mechanism underlying the occurrence of venous thromboembolism.12 During pregnancy and the postpartum period, women experience significant changes in their coagulation function and hemodynamics, making this stage a high-risk period for the development of VTE.13 The postpartum phase already carries an elevated risk of VTE. The cultural practice of extended bed rest during the “lying-in” period can intensify the risk of DVT. In addition, the risk of VTE after cesarean section is four times higher compared to vaginal delivery, and the risk is even higher for those undergoing emergency cesarean section, independent of other VTE risk factors.14 Pregnant women who are of advanced maternal age have a higher susceptibility to experiencing thrombotic events. In our study, the women who developed DVT were found to be older, had a higher proportion of women with previous childbirth experiences, and had a higher proportion of women with comorbidities. We also found several independent risk factors for postpartum DVT following cesarean section in elderly pregnant women. These risk factors included being aged 39 years or older, having comorbid preeclampsia, a plasma D-dimer level greater than 0.56 mg/L, a plasma FIB level exceeding 3.59 g/L, and a PLT higher than 218.82 × 109/L. These findings provided valuable insights into identifying high-risk individuals and implementing preventive measures to reduce the occurrence of DVT in elderly pregnant women who undergo a cesarean section.
Then, we explored the predictive value of APTT, PT, D-dimer, FIB, PLT and their combined test mode in relation to the development of DVT. Our results revealed significant differences in the levels of APTT and PT between the NDVT group and the DVT group. In contrast, the DVT group displayed significantly higher levels of D-dimer, FIB and PLT when compared to the NDVT group. These results suggest distinct differences in coagulation and fibrinolysis markers between the NDVT and DVT groups. A decrease in APTT and PT indicates that the blood is in a hypercoagulable state and there is a tendency for blood clot formation.15 The higher levels of APTT and PT in the NDVT group indicate a prolonged clotting time and impaired coagulation function, possibly contributing to a reduced risk of developing DVT. D-Dimer is currently a widely used specific biomarker in clinical practice for secondary fibrinolysis and clot activation.16 FIB is one of the leading causes of thrombus formation and is also the highest-concentration coagulation factor in the plasma, with its concentration reflecting the blood viscosity.17 The activation of PLT also leads to the release of numerous bioactive substances, such as platelet-derived growth factors and platelet aggregation factors, further promoting thrombus formation.18 Therefore, the significantly elevated levels of D-dimer, FIB, and PLT in the DVT group suggest increased fibrin degradation, higher fibrinogen levels, and potential platelet activation, indicating an ongoing thrombotic process and an increased risk of DVT.
The ROC analysis results further revealed the AUC values for APTT, PT, D-dimer, FIB, PLT and the combined test model in predicting the occurrence of DVT in elderly pregnant women after cesarean section. The AUC for the combined test model was substantially higher than individual parameters (APTT, PT, D-dimer, and FIB), suggesting that incorporating multiple parameters into the combined test model provided a more accurate prediction of DVT occurrence in elderly pregnant women after cesarean section. These findings highlight the potential of the combined test model in clinical practice, as it demonstrated superior predictive ability compared to individual coagulation and platelet-related parameters. Including multiple factors in the model enhances the overall performance and could aid in identifying elderly pregnant women at a higher risk of developing DVT after cesarean section. However, further validation studies are necessary to confirm the utility and reliability of the combined test model in larger populations and different clinical settings.
Our study has several limitations, the first being the small cohort size. Conducting a more extensive study would provide more comprehensive information, allowing for a better understanding. Second, although we mentioned the cultural practice of “lying-in” rest as a possible factor contributing to developing DVT in Chinese women, we did not document relevant information or conduct specific investigations on this aspect. In future research, it would be beneficial to include this factor and explore its potential association with DVT occurrence.
Conclusion
Multiple parameters of the postoperative coagulation state in the combined test model provided a more accurate prediction of DVT occurrence in elderly pregnant women after cesarean section.
Data Sharing Statement
The data could not be shared openly, as required by our department. The raw data could be obtained upon reasonable request to the corresponding author.
Ethical Approval
This study was approved by the ethics committee of Shijiazhuang Obstetrics and Gynecology Hospital. Informed consent was obtained from all participants and their family members. All methods were performed following the relevant guidelines and regulations. The study complies with the Declaration of Helsinki, Ethical Principles for Medical Research Involving Human Subjects.
Consent for Publication
Not applicable.
Funding
There is no funding to report.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Pomp ER, Lenselink AM, Rosendaal FR, Doggen CJ. Pregnancy, the postpartum period and prothrombotic defects: risk of venous thrombosis in the MEGA study. J Thromb Haemost. 2008;6(4):632–637. doi:10.1111/j.1538-7836.2008.02921.x
2. Jackson E, Curtis KM, Gaffield ME. Risk of venous thromboembolism during the postpartum period: a systematic review. Obstet Gynecol. 2011;117(3):691–703. doi:10.1097/AOG.0b013e31820ce2db
3. Acharya G, Singh K, Hansen JB, Kumar S, Maltau JM. Catheter-directed thrombolysis for the management of postpartum deep venous thrombosis. Acta Obstet Gynecol Scand. 2005;84(2):155–158. doi:10.1111/j.0001-6349.2005.00565.x
4. Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–e333. doi:10.1016/S2214-109X(14)70227-X
5. Essien EO, Rali P, Mathai SC. Pulmonary Embolism. Med Clin North Am. 2019;103(3):549–564. doi:10.1016/j.mcna.2018.12.013
6. Sultan AA, Tata LJ, West J, et al. Risk factors for first venous thromboembolism around pregnancy: a population-based cohort study from the United Kingdom. Blood. 2013;121(19):3953–3961. doi:10.1182/blood-2012-11-469551
7. Claramonte Nieto M, Meler Barrabes E, Garcia Martinez S, Gutierrez Prat M, Serra Zantop B. Impact of aging on obstetric outcomes: defining advanced maternal age in Barcelona. BMC Pregnancy Childbirth. 2019;19(1):342. doi:10.1186/s12884-019-2415-3
8. Lean SC, Derricott H, Jones RL, Heazell AEP, Bhutta ZA. Advanced maternal age and adverse pregnancy outcomes: a systematic review and meta-analysis. PLoS One. 2017;12(10):e0186287. doi:10.1371/journal.pone.0186287
9. Salvetti MG, Lauretti LG, Muniz RC, et al. Characteristics of pregnant women at risk and relationship with type of delivery and complications. Rev Bras Enferm. 2021;74(4):e20200319. doi:10.1590/0034-7167-2020-0319
10. Jennings JA. Thromboembolic disease in Obstetrics and Gynecology. Henry Ford Hosp Med Bull. 1963;11:289–307.
11. Sia WW, Powrie RO, Cooper AB, et al. The incidence of deep vein thrombosis in women undergoing cesarean delivery. Thromb Res. 2009;123(3):550–555. doi:10.1016/j.thromres.2008.06.004
12. Bagot CN, Arya R. Virchow and his triad: a question of attribution. Br J Haematol. 2008;143(2):180–190. doi:10.1111/j.1365-2141.2008.07323.x
13. Bitsadze V, Khizroeva J, Alexander M, Elalamy I. Venous thrombosis risk factors in pregnant women. J Perinat Med. 2022;50(5):505–518. doi:10.1515/jpm-2022-0008
14. Blondon M, Casini A, Hoppe KK, Boehlen F, Righini M, Smith NL. Risks of venous thromboembolism after cesarean sections: a meta-analysis. Chest. 2016;150(3):572–596. doi:10.1016/j.chest.2016.05.021
15. Ganter MT, Hofer CK. Coagulation monitoring: current techniques and clinical use of viscoelastic point-of-care coagulation devices. Anesth Analg. 2008;106(5):1366–1375. doi:10.1213/ane.0b013e318168b367
16. Dai H, Zhou H, Sun Y, et al. D-dimer as a potential clinical marker for predicting metastasis and progression in cancer. Biomed Rep. 2018;9(5):453–457. doi:10.3892/br.2018.1151
17. Sharma SK, Philip J, Wiley J. Thromboelastographic changes in healthy parturients and postpartum women. Anesth Analg. 1997;85(1):94–98. doi:10.1097/00000539-199707000-00017
18. Yun SH, Sim EH, Goh RY, Park JI, Han JY. Platelet activation: the mechanisms and potential biomarkers. Biomed Res Int. 2016;2016:9060143. doi:10.1155/2016/9060143
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.