Back to Journals » Psychology Research and Behavior Management » Volume 16
Positive Religious Coping and Associated Factors Among Participants with Severe Mental Illness Attending Felege Hiwot Comprehensive Specialized Hospital, Bahir Dar, Ethiopia, 2021
Received 17 May 2023
Accepted for publication 27 July 2023
Published 2 August 2023 Volume 2023:16 Pages 2931—2941
DOI https://doi.org/10.2147/PRBM.S421684
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Belete Birhan,1 Netsanet Eristu2
1Department of Psychiatry, Wolaita Sodo University, College of Health Science and Medicine, Wolaita Sodo, Ethiopia; 2Department of Psychiatry, Dire Dawa University, College of Medicine and Health Science, Dire Dawa, Ethiopia
Correspondence: Belete Birhan, Tel +251-935-55-94-05, Email [email protected]
Background: Religion has been reported to be the most widely used coping resource in stressful conditions including physical and mental illnesses. Different studies consistently find that positive religious coping is associated with a reduced level of severe mental illness such as depression. Despite its high prevalence and being a significant coping mechanism for persons with severe mental illness, there are no published studies on positive religious coping in Ethiopia.
Objective: To assess the prevalence of positive religious coping and associated factors among people with severe mental illness attending outpatient service at Felege Hiwot Comprehensive Specialized Hospital, Bahir Dar, northwest Ethiopia, 2021.
Methods: A cross-sectional institution-based study was conducted and systematic random sampling was applied to select participants. Data were collected through a face-to-face interview. The collected data were entered into EpiData version 3.1 and exported to SPSS version 20 for processing and analysis. Multivariable logistic regression was used to identify independent factors associated with religious coping. P-value < 0.05 was declared a statistically significant association with a 95% confidence interval.
Results: The prevalence of positive religious coping among severe mental illness was 72.4% (95% CI= 68.2, 76.4). Having no comorbid medical illness, good quality of life, good medication adherence, and mild subjective severity scale were associated with positive religious coping.
Conclusion: The magnitude of positive religious coping among severe mental illness was relatively high. Not having a comorbid medical illness, good medication adherence, good quality of life, and mild subjective severity scale were factors associated with it. Patients report different factors that affect practicing positive religious coping factors. In the other direction, positive religious coping was reported to contribute to symptom alleviating and increasing a sense of well-being.
Keywords: religious, positive religious coping, severe mental illness
Introduction
Background
Religion is defined as human beings’ relation to that which they regard as holy, sacred, absolute, spiritual, divine, or worthy of special reverence. It is also commonly regarded as consisting of the way people deal with ultimate concerns about their lives and their fate after death. Believers and worshippers participate and engage in devotional practices such as prayer, meditation, or particular rituals. Worship, moral conduct, right belief, and participation in religious institutions are among the constituent elements of religious life.1 Spirituality is the capacity of persons to transcend themselves through knowledge and love, that is, to reach beyond themselves concerning others and thus become more than self-enclosed monads. It can be religious or secular,2 while religiousness is an admission of one’s total dependence as a creature on the source of being and the life which is spoken of as reverence, gratitude for being, and life through an institutionalized system of relating with God or gods, which is concerned whatever society or group considers ultimately important.3
A religious person has a particular religion to follow and be guided by, while a spiritual person does not follow a particular organized religion, but maintains a belief larger than themselves, and they may believe in God without engaging in any religious organization.4 According to previous studies religion has been reported to be the most widely used coping resource (up to 90%) in stressful conditions including physical and mental illnesses, which is practiced across a variety of situations in everyday life.5,6
It is proved that there is an association between religious coping and the health and wellbeing of individuals including the significant association between positive religious coping with mental and physical health.7 While compared to physical health there is a stronger relationship between religious coping and mental health.2 Spiritual, religious, or personal belief system positively affects active and adaptive coping skills in patients with schizophrenia during their remission and helps the individual to cope with illness-related stressors. Understanding and assessing the spirituality and religiousness of Patients with schizophrenia helps in better management of the problem.8
Another study also shows that early insecure attachment is a risk for depression as well as psychosis, due to this having a positive religious coping involving a secure attachment to a spiritual figure have a soothing effect and it improves symptoms like low mood and some psychotic features because God is perceived as a loving attachment figure.9
There is a significant positive association between religiosity and treatment adherence in patients with mental illness including severe mental illness, which in turn has significance for a favorable outcome, making it preferable to be integrated with treatment strategies.10 Another study also showed that More than 80% of psychotic patients engage in religious coping, those patients also give more value to the significance of religion in their day-to-day life, and are frequently engaged both in individual and group religious activities, positive religious coping is positively associated with increased quality of life in schizophrenia patients.11
Religious coping is religiously framed in cognitive, emotional, and behavioral dimensions.12 It can also be defined as the use of religious resources like institutions, beliefs, attitudes, and practices for understanding and coping with stress and reducing emotional distress caused by unfavorable life events.6,13
The two religious coping dimensions with different outcomes in mental illness are; positive religious coping and negative religious coping. Positive religious coping reflects a secure relationship with God which is expected to have a greater meaning to be found and a sense of connectedness with others, which has been associated with better adaptation and outcome with severe mental illness.13,14
Positive religious coping appears to be associated with greater well-being, and is frequently, but not invariably, inversely associated with psychopathology.13 It is used in the recovery process of patients with severe mental illness.15 Because most people affiliate themselves with religion in Ethiopia, it is expected that religion emerges as the main resource for coping with symptoms of distress and stressful experiences.16
Religious coping has particularly an impact on the quality of life of bipolar patients; specifically, positive religious coping leads to increased quality of life.17 It has also been found to have an association with a reduced level of depression.18 Despite its significance more severely depressed patients may not practice it by considering their illness as a punishment for their wrongs and they may have a feeling as if “God has left them”, during these clinical interventions may be expected.19 Interventions working on improving positive religious coping and diminishing spiritual questioning may help in solving psychological problems when individuals are faced with stressful life events; because when individuals are neither motivated nor capable of applying positive religious coping social support could be used as a complementary coping way.20 The limited research that does exist on religious coping among persons with severe mental illness indicates that it may be a basic and frequently used mechanism for dealing with chronic symptoms and related life challenges.21 It is evidenced that even simply taking (2–5 minutes) a spiritual history during assessing a patient, is associated with greater satisfaction with treatment and better QOL.17 Although positive religious coping is a popular method used by patients with severe mental illness, less attention has been given during treatment. Despite its significance, there are limited studies on positive religious coping. This study assessed the prevalence and associated factors of religious coping with severe mental illness in Ethiopia.
Methods and Materials
Study Design, Setting, and Period
An institutional-based cross-sectional study was conducted at Felege Hiwot Comprehensive Specialized Hospital, which is found in Amhara region, Bahir Dar City, North West Ethiopia, from March 2021 to April 2021, which is located 390 km away from Addis Ababa. The hospital is currently providing services like medical, surgical, obstetrics and gynecology, orthopedics, and psychiatry. The psychiatry unit has 4 MSC and 5 BSC mental health professionals, 3 OPDs, and 7 beds (3 for females and 4 for males). The outpatient service benefits about 1800–2200 patients per month, and the majority of them are schizophrenics followed by a mood disorder.
Participants
The study was targeting all people with severe mental illness attending FHCSH psychiatry outpatient service. Participants aged 18 and above with severe mental illness that follow any religion and have follow up for at least one month were included. While those who have a religious delusion, have no insight, and are unable to communicate during data collection were excluded.
Sample Size Determination
The sample size was calculated using the single population proportion calculation under the following presumptions: N=Zα/2 × P (1-P)/W2 by taking the proportion of 50% since there were no studies on the prevalence of positive religious coping on severe mental illness in Ethiopia.
n= 385
Then by adding a 10% non-response rate, the final sample size was n=385+38=423.
Sampling Method and Technique
Systematic random sampling was applied to select patients with severe mental illness who fulfilled the inclusion criteria. Taking the average monthly flow of patients at FHCSH (2000), an interval k was determined by k = 2000 / 423 = 5, the first person was selected randomly, and then every 5-person data were collected.
Study Variables
Dependent Variable
Positive religious coping.
Independent Variables
- Socio-demographic factors; Age, sex, religion, educational level, marital status, occupation.
- Illness and treatment-related factors, the severity of illness.
- Medication adherence.
- Quality of life.
- Type of mental illness.
- Religious role (follower, priest, daikon, sheik, merigeta).
- Functional remission.
Operational Definition
Considered Positive Religious Coping
Individuals who scored a subscale of ≥20 from the first 7 items of a 14-item Brief religious coping tool.10
Quality of Life
Respondents who scored above the mean score (>86.6) of the WHOQOL-BRIEF26 item index were taken as having a good quality of life.22
Poor Adherence
Individuals who scored in MARS (medication adherence rating scale) a score ≥ 6 were taken as adherents and those with a score less than 6 as non-adherents.23
Severe Mental Illness
Respondents who were diagnosis with either Schizophrenia, Bipolar disorder, or Major depressive disorder thought to cause major morbidity and mortality.24
The Severity of Illness
For both subjective and objective severity assessment, responses 1–3 on the clinical global impression (CGI) severity scale were considered mild, 4 as moderate, and 5–7 as severe.25
Functional Remission
From the WHODAS score, <20 was taken as having functional remission, and ≥ 20 was taken as not having functional remission.26
Data Collection Tool and Procedure
Positive religious coping was measured by using the BRCOOP tool. Which has two separate parts with 14 items to assess PRC and NRC, the first 7 items assess positive religious coping with a 4 Likert scale. A score≥20 was considered positive religious coping. The PRC part has Cronbach’s alpha of 0.90.10
Quality of Life was assessed using WHOQOL-BRIEF 26-item index. It’s prepared by World Health Organization and cross-culturally validated. The higher the score the better quality of life, in this regard, the sum of scores above the mean (>86.6) was considered a good quality of life.22
Medication adherence was assessed using the Medication Adherence Rating Scale. It has 10 “YES” or “NO” questions with internal consistency (Cronbach’s alpha) 0.86. The patients were required to answer “NO” for questions 1 up to 6 and 9 up to 10, and “YES” for questions 7 and 8 to become fully adherent. A total score of 6 or more indicates adherence and less than 6 indicate non-adherence.23
The severity of illness was assessed using the clinical global impression (CGI) severity scale which has a question with 7 responses, and responses 1–3 were taken as mild, 4 as moderate, and 5–7 were taken as severe illness for both subjective and objective severity assessment.25
The questionnaire was translated into the local language (Amharic) and then back to English by another translator. Data were collected using a semi-structured questionnaire and taking information on the patient card about the diagnosis, mental health professionals were selected for data collection, and supervisors were assigned for the data collection. The training was given to data collectors as well as supervisors about the data collection procedure and the questionnaire.
Data Processing and Analysis
Data were entered into EpiData version 3.1 and cleaned, coded, and analyzed using SPSS Statistical software version 20. Descriptive statistics were conducted to summarize and present variables. Bivariable logistic regression was done, and variables with a p-value less than 0.25 were taken to multivariable logistic regression which was used to identify independent factors associated with religious coping. P-value <0.05 declared statistically significant association with a 95% confidence interval.
Data Quality Control
To assure the data quality, training was given to data collectors and supervisors preceding the data collection time. Before the actual data were collected, the questionnaire was tested on 5% of the total sample size (21 individuals) at Tibebe-Ghion specialized hospital. The collected data were counted and cross-checked for completeness and consistency before the actual data entry.
Ethical Consideration
Ethical clearance was obtained from Bahir Dar University’s ethical review board. The objective of the study was explained to participants, and written Informed consent was obtained from participants. The privacy and confidentiality of the participant were kept at every stage. There were no mentioning names of participants on the questionnaire rather they were coded using numbers. There were no forcing participants to participate unless they are volunteer; they were also told that they have the right to discontinue the interview at any time.
Result
Socio-Demographic Characteristics of Respondents
A total of 402 participants with severe mental illness have participated with a response rate of 95%. Among participants 54.7% (220) were male. 36.1% of respondents were between the ages of 25 and 34. The majority of participants were Orthodox religion followers 68.9% (277). Regarding marital status 48% (193) were married. About 26% were grade level 9–12, based on their religious role about 95.8% were followers. For detail, see Table 1.
 |
Table 1 Description of Socio-Demographic Characteristics of the Respondents with Severe Mental Illnesses at Felege Hiwot Comprehensive Specialized Hospital, North West Ethiopia, 2021 (n=402) |
Clinical and Psychosocial Factors of Respondents
About 38.1% (153) of respondents had a diagnosis of major depressive disorder. More than half of the participants 273 (67.91%) had a duration of illness less than or equal to five years, and about 317(78.86%) were on treatment for a maximum of five years. Regarding their medication frequency, 247 (61.44%) took medication one time per day and 224 (55.72%) of respondents were on monotherapy. Only 31.3% (126) had a history of admission, and about 45.5% (183) had a history of relapse. Regarding comorbid medical illness, about 18.4% (74) had known medical illness. Most of the participants 75.9% (305) had good medication adherence. About 80.8% (325) had a mild score on the objective severity scale and 82.8% (333) had a mild score on the subjective severity scale. Regarding the functional status of participants, most of the respondents 68.9% (277) had no functional remission, and half of the respondents 50.0% (201) had a good quality of life. More to see Table 2.
 |
Table 2 Description of Clinical and Psychosocial Factors of the Respondents with Severe Mental Illnesses at Felege Hiwot Comprehensive Specialized Hospital, North West Ethiopia, 2021 (n=402) |
Prevalence of Positive Religious Coping
The prevalence of positive religious coping among participants with severe mental illness was 72.4% (291). Detail see Figure 1
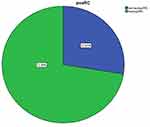 |
Figure 1 Graphical presentation of the magnitude of positive religious coping of respondents with severe mental illnesses (n=402). |
Factors Associated with Positive Religious Coping
Variables with a p-value less than 0.25 in Bivariable logistic regression were taken to multivariable logistic regression; then a variable with a p-value less than or equal to 0.05 was taken as the significantly associated in multivariable logistic regression. Model fitness was tested in multivariable logistic regression and the value of the Hosmer and Lemeshow test result was 0. 348. Comorbid medical illness, quality of life, medication adherence, and subjective severity scale were associated with positive religious coping.
The variable group expected to be against PRC was treated as the reference group. The odds of having positive religious coping among females were 1.4 times higher than in males. The odds of having PRC among those without comorbid medical illness were 3.34 (1.5, 7.4) times higher compared to those with comorbid medical illness. Regarding participants’ medication adherence, the odds of having PRC among those with good medication were 6.45 (3.39, 12.4) times higher than those with poor medication adherence. The odds of having PRC among participants with a mild subjective severity scale were 4.9 (1.14, 21) times higher compared to those with a severe subjective severity scale. Regarding the quality of life, the odds of having PRC among those with good quality of life were 5 (2.6, 9.5) times higher than those with poor quality of life (details see Table 3).
Discussion
Magnitude of Positive Religious Coping
At the current level of knowledge, most studies use means to show positive religious coping, and that makes it a challenge to compare the current study with the previous studies. This study showed that the prevalence of positive religious coping among people with severe mental illness was 72.4% (95% CI = 68.2, 76.4). It may be due to the unconscious use of positive religious coping (preference to be attached to God) as compensation for early insecure attachment with attachment figures, which is hypothesized to be part of the etiology of mental illness, especially in psychosis.9 It may also be because a secure attachment to a spiritual figure may have a soothing effect and possibly improve symptoms like anxiety, lowered mood, and psychosis. Because Ethiopia has a deeply religious society and Faith is deeply important to day-to-day life as well as the identity of its society, there will be frequent attendance at religious places and strict following of religious commandments and sermons by followers of most of the religions. Religious followers are expected to be positively attached to God, and they are preached to take stressful life events as tests from God, that “God challenges whom he loves most”, and to wait for his mercy by having an absolute faith in him, which makes them hopeful. So many societies will choose to stick to God and install hope in their lives while facing challenges like severe mental illness ratherthan choosing other ways of coping. Positive religious copingmay have important implications for the remediation and prevention of mental health problems in the wake of stressful life events.
In this study, no comorbid medical illness, good medication adherence, a low subjective severity score, and a good quality of life were associated with positive religious coping. The odds of having PRC among those without comorbid medical illnesses were higher compared to those with comorbid medical illnesses. This might be due to increased hopelessness because of many stressorsand the association of chronic illnesses with psychopathology, which may worsen already existing mental illnesses, and negatively affects positive religious coping. Religious involvement appears to enable the sick, particularly those with serious and disabling medical illnesses, to cope better and experience psychological growth from their negative health experiences rather than be defeated or overcome by them.
Regarding participants’ medication adherence, the odds of having PRC among those with good medication adherence were higher than those with poor medication adherence. This is supported by Iranian studies which found positive religious coping to be positively associated with medication adherence.10 This might be due to decreased severity of illness in those with good medication adherence, and when the illness becomes less severe, they become engaged in positive religious coping. Having positive religious coping by itself might help medication adherence by installing hope in patients.
The odds of having PRC among patients with a mild subjective severity scale were higher compared to those with a severe subjective severity scale. This might be due to the inability to engage in religious activities and problems with rationalizing things, which are related to the nature of the illness. Regarding quality of life, the odds of having PRC among those with good quality of life were higher than those with poor quality of life. This is supported by US studies on schizophrenia patients, Brazilian studies on bipolar patients, and Nigerian studies on DM and depression patients.5,11,17 The association between positive religious coping and quality of life might be due to the positive aspect of good quality of life that makes patients more satisfied and become close to God. Positive religious coping is generally viewed as being adaptive, and it reflects beliefs about the meaningfulness of life and a reliance on a secure relationship with a merciful God.
Limitations of the Study
The study has its limitation. The cross-sectional nature of the study did not show the direction of causality between positive religious coping and independent variables. Social desirability bias may affect the study, as religion is a sensitive aspect in Ethiopia, and participants may not be psychologically free to say what they feel. The tool is not validated in Ethiopia.
Conclusion and Recommendation
The prevalence of positive religious coping among participants with severe mental illness attending Felege Hiwot Comprehensive Specialized Hospital outpatient service was high. Having no comorbid medical illness, good medication adherence; mild subjective severity score, and good quality of life were associated with positive religious coping.
This study recommends that religious bodies should be integrated with clinical services to benefit all patients with severe mental illness. Mental health professionals working with this population should use therapeutic relationships mindfully in terms of how contextual variables related to cultural, religious, and traditional beliefs. Additionally mental healthprofessionalsl should understand the conceptual framework of religious coping and its association with severe mental ill individuals.
More generally, a better understanding of religious coping might also help psychotherapeutic practitioners better integrate religious and spiritual dimensions into the treatment and relapse prevention of common mental health problems.
Future cohort studies should be done to clearly understand the cause-and-effect relationship between positive religious coping and severe mental illness.
Abbreviation
BDo, Bipolar Disorder; BRCOOP, Brief Religious Coop; FHCSH, Felege Hiwot Comprehensive Specialized Hospital; MDD, Major Depressive Disorder; NRC, Negative Religious Coping; PRC, Positive Religious Coping; QOL, Quality of Life; RC, Religious Coping; WHODAS, World Health Organization Disability Assessment Scale.
Data Sharing Statement
The data set used and/or analyzed during the current study are available from the corresponding author and they will be deposited in publically available repositories or those wishing to use them for non-commercial purposes, without breaching participants’ confidentiality.
Ethical Approval and Consent to Participate
All method was conducted according to the ethical standard of the Declaration of Helsinki. Ethical clearance was obtained from the institutional review board of Bahir Dar University. Detailed information about the study was explained to participants in the information sheet. Written informed consent was obtained from participants who have formal education and informed verbal consent was obtained from participants who have no formal education because they did not read the written informed consent and approved by the institutional review board (IRB) of Bahir Dar University. The Privacy and confidentiality of study participants’ information were kept at every stage of data processing by excluding any personal identifiers in the questionnaire.
Acknowledgment
We would like to express our deepest heartfelt thanks to Bahir Dar University and the study participants.
Author Contributions
NE and BB made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas. NE and BB took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. The editors of encyclopaedia Britannica. Religion; 2020.
2. Charzyńska E. Multidimensional approach toward spiritual coping: construction and validation of the Spiritual Coping Questionnaire (SCQ). J Relig Health. 2015;54(5):1629–1646. doi:10.1007/s10943-014-9892-5
3. Shenider S. Religion and spirituality; 2000.
4. Kitchnere K. What it means to be spiritual but not religious; 2018.
5. Amadi K, Uwakwe R, Odinka PC, et al. Religion, coping and outcome in out-patients with depression or diabetes mellitus. Acta Psychiatr Scand. 2016;133(6):489–496. doi:10.1111/acps.12537
6. Andrew ND. Religious coping measurement in the context of long-term care; 2019.
7. Abu-Raiya H, Sasson T, Pargament KI, Rosmarin DH. Religious coping and health and well-being among Jews and Muslims in Israel. Int J Psychol Relig. 2020;30:1–14.
8. Das S, Punnoose VP, Doval N, et al. Spirituality, religiousness and coping in patients with schizophrenia: a cross sectional study in a tertiary care hospital. Psychiatry Res. 2018;265:238–243. doi:10.1016/j.psychres.2018.04.030
9. Huguelet P, Mohr S, Rieben I, et al. Attachment and coping in psychosis in relation to spiritual figures. BMC Psychiat. 2015;15(1):1–12. doi:10.1186/s12888-015-0617-4
10. Movahedizadeh M, Sheikhi M, Shahsavari S, et al. The association between religious belief and drug adherence mediated by religious coping in patients with mental disorders. Soc Health Behav. 2019;2(3):77. doi:10.4103/SHB.SHB_9_19
11. Nolan JA, McEvoy JP, Koenig HG, et al. Religious coping and quality of life among individuals living with schizophrenia. Psychiatr Serv. 2012;63(10):1051–1054. doi:10.1176/appi.ps.201000208
12. Wortmann J. Religious Coping, in Encyclopedia of Behavioral Medicine. New York, NY: Springer New York; 2013:1647–1648.
13. Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol. 2000;56(4):519–543. doi:10.1002/(SICI)1097-4679(200004)56:4<519::AID-JCLP6>3.0.CO;2-1
14. Pargament K, Feuille M, Burdzy D. The Brief RCOPE: current psychometric status of a short measure of religious coping. Religions. 2011;2(1):51–76. doi:10.3390/rel2010051
15. Yangarber-Hicks N. Religious coping styles and recovery from serious mental illnesses. J Psychol Theol. 2004;32(4):305–317. doi:10.1177/009164710403200403
16. Azale T, Fekadu A, Medhin G, et al. Coping strategies of women with postpartum depression symptoms in rural Ethiopia: a cross-sectional community study. BMC Psychiat. 2018;18(1):1–13. doi:10.1186/s12888-018-1624-z
17. Stroppa A, Colugnati FA, Koenig HG, et al. Religiosity, depression, and quality of life in bipolar disorder: a two-year prospective study. Braz J Psychiatry. 2018;40(3):238–243. doi:10.1590/1516-4446-2017-2365
18. Mawji A. Religious Coping and Depression. University of Leicester; 2017.
19. Kos L, Šagud M, Mihaljević-Peleš A, et al. Religiosity and severity of symptoms in Croatian patients with major depressive disorder or schizophrenia. J Nerv Ment Dis. 2019;207(6):515–522. doi:10.1097/NMD.0000000000001003
20. García FE, Páez D, Reyes-Reyes A, et al. Religious coping as moderator of psychological responses to stressful events: a longitudinal study. Religions. 2017;8(4):62. doi:10.3390/rel8040062
21. Tepper L, Rogers SA, Coleman EM, et al. The prevalence of religious coping among persons with persistent mental illness. Psychiatr Serv. 2001;52(5):660–665. doi:10.1176/appi.ps.52.5.660
22. World Health Organization. Programme on Mental Health: WHOQOL User Manual. World Health Organization; 1998.
23. Thompson K, Kulkarni J, Sergejew A. Reliability and validity of a new Medication Adherence Rating Scale (Mars) for the psychoses. Schizophr Res. 2000;42(3):241–247. doi:10.1016/S0920-9964(99)00130-9
24. Fekadu A, Medhin G, Kebede D, et al. Excess mortality in severe mental illness: 10-year population-based cohort study in rural Ethiopia. Br J Psychiat. 2015;206(4):289–296. doi:10.1192/bjp.bp.114.149112
25. Kadouri A, Corruble E, Falissard B. The improved Clinical Global Impression Scale (iCGI): development and validation in depression. BMC Psychiat. 2007;7(1):1–7. doi:10.1186/1471-244X-7-7
26. Sjonnesen K, Bulloch AGM, Williams J, et al. Characterization of disability in Canadians with mental disorders using an abbreviated version of a DSM-5 emerging measure: the 12-item WHO disability assessment schedule (WHODAS) 2.0. Can J Psychiatry. 2016;61(4):227–235. doi:10.1177/0706743716632514
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.