Back to Journals » Journal of Pain Research » Volume 10
Positive medium-term influence of multimodal pain management on socioeconomic factors and health care utilization in patients with lumbar radiculopathy: a prospective study
Authors Benditz A , Loher M, Boluki D, Grifka J, Völlner F, Renkawitz T, Maderbacher G, Götz J
Received 18 November 2016
Accepted for publication 12 December 2016
Published 14 February 2017 Volume 2017:10 Pages 389—395
DOI https://doi.org/10.2147/JPR.S128090
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Achim Benditz, Martin Loher, Daniel Boluki, Joachim Grifka, Florian Völlner, Tobias Renkawitz, Günther Maderbacher, Jürgen Götz
Department of Orthopedics, University Medical Center Regensburg, Asklepios Klinikum Bad Abbach, Bad Abbach, Germany
Background: Multimodal pain management (MPM) represents a central approach to avoiding surgery in patients with lumbar radiculopathy. Independent of the type of health system, cost effectiveness and socioeconomic factors are becoming increasingly important. This study investigated the medium-term influence of conservative MPM on health care utilization and socioeconomic factors.
Methods: This study compared subjective, objective, and socioeconomic factors of 60 patients after inpatient MPM because of lumbar radiculopathy, before and 1 year ± 2 weeks after treatment.
Results: Over the course of the 1-year follow-up, one-third of the patients had not required any conservative treatment in comparison to 100% of patients before MPM therapy. The number of patients requiring analgesics could be significantly reduced from 26 to 12, and the number of patients who did not require any analgesics had increased from 14 to 32. After 1 year, the number of patients who had to regularly contact a physician because of low back pain (once per month for 6 months) had been reduced from 58 to 27.
Conclusion: MPM is an effective approach to treating lumbar radiculopathy and reducing its negative influence on socioeconomic factors. Therapeutic benefits also include a decrease in health care utilization. Therefore, health care providers should place the mid-term success for patients and socioeconomic factors before the short-term costs of therapy.
Keywords: lumbar spinal stenosis, multimodal therapeutic treatment, spinal injection, conservative treatment
Background
Low back pain (LBP) is one of the most disabling health conditions in the world.1 In 10–20% of patients, LBP is associated with lumbar radiculopathy. Back pain is one of the most important causes of lifelong disability worldwide and results in enormous medical and social costs.2 Although all age groups are affected, elderly people are the largest population presenting with lumbar spine diseases.3 Irrespective of the type of health system, the growing number of people with back pain also presents a socioeconomic problem.4 The longer the patients are unable to work, the higher is the number of patient visits to a physician. The lower the number of effective treatment options available, the higher are the costs for public health systems. Therefore, it is very important to find the right treatment as quickly as possible to prevent pain chronification5 and to avoid surgery if possible. Although comparing treatment options is difficult because of the lack of standardization, we could show the positive mid-term effect of an injection-based multimodal pain management (MPM) concept in patients with lumbar radiculopathy in a previously published study.3
At the same time, concerns have been expressed in the media as well as in clinical studies with regard to the efficacy, cost, and overuse of low back injections.6–9 Although evidence indicates that LBP injections for radiculopathy may delay more expensive surgical interventions and decrease the use of opiods,10,11 more and more health care providers and insurances try to avoid MPM as an inpatient option to save costs in the short term. In Germany, for example, patients have to fulfill 3 out of 5 criteria to be eligible for inpatient MPM; otherwise, treatment will not be paid for (Table 1).
  | Table 1 Inclusion criteria for multimodal pain management in Germany (OPS 8-918); 3 of 5 criteria have to be present Notes: Data from OPS: Operationen- und Prozedurenschlüssel [Operation and Procedure Code] German modification of the International Classification of Procedures in Medicine [Internationalen Klassifikation der Prozeduren in der Medizin (ICPM)].27 |
Because of these contradictory facts and the positive mid-term results regarding clinical outcome shown by our group,3 this further investigation of our cohort aimed at showing the positive mid-term effects of a multimodal inpatient therapeutic concept on socioeconomic factors and health care utilization in patients with lumbar radiculopathy.
Methods
Study design and eligibility criteria
The study design was already described in the previous study.3 This non-randomized unblinded prospective clinical study included male and female patients with lumbar radiculopathy aged between 29 and 79 years who were treated according to a multimodal therapeutic concept at the Department of Orthopedics of an University Medical Center within 12 months. Participation in the study was voluntary. Inclusion criterion was radicular pain arising from one specific nerve root diagnosed by the presence of either a positive straight leg raising sign, pain radiating distal to the knee, or clearly attributable motoric failure. In addition, patients had to participate in at least 5 psychological sessions during therapy. Exclusion criteria were post-discectomy syndrome, rheumatic or inflammatory spinal disorders, tumors with spinal involvement, and congenital spinal deformities. For ethical reasons, no control group was formed because such patients would have received placebo injections instead of effective drugs. The study was approved by the Ethics Committee of the University of Regensburg (21 April 2010, ref. no. 10-101-0061) and carried out in accordance with the guidelines of the Declaration of Helsinki of 1975. Written informed consent was obtained from all participants. The study is registered in the Deutsches Register Klinischer Studien (DRKS) with the number DRKS00010257 (World Health Organization register).3
Patients
After evaluation of the patient files for exclusion criteria, 88 of the 285 patients meeting the inclusion criteria were included in the study. The study population was the same cohort as described in our previous study.3 These 88 patients were contacted by telephone interview 11 months after therapy. Twenty-eight patients refused to undergo the follow-up examination because of the travel distance to the hospital or had not recorded the necessary data over the year. Eight of these 28 patients had received surgery during this period. Sixty volunteers finally remained in the study (Figure 1).
  | Figure 1 Flowchart of the study. Note: Adapted from Benditz A, Madl M, Loher M, Grifka J, Boluki D, Linhardt O. Prospective medium-term results of multimodal pain management in patients with lumbar radiculopathy. Sci Rep. 2016;6:28187. The Creative Commons license is available at: https://creativecommons.org/licenses/by/4.0/legalcode.3 |
Intervention
Because this study was more focused on socioeconomic factors and health care utilization than on the direct therapeutic effect, the interventions were only shortly summarized in comparison to our previous study, in which the effects of each single intervention had been explained in more detail.3
On average, each patient received 2 injections daily, 1 in the morning and 1 at noon. Injections consisted of lumbar spinal nerve root analgesia into the affected nerve root using “freehand technique”,12 1 injection into the facet joints under X-ray guidance, and 1 epidural injection using “loss-of-resistance technique” per stay.13,14 Treatment duration was 8–12 days (mean 10.8 days) for each patient. In addition, patients were offered physiotherapy, sports therapy, group exercises, aqua training, electrotherapy, thermotherapy, progressive muscle relaxation according to Jacobsen,15 and coordination training.16
The psychotherapeutic program of MPM17 consists of an individual interview and group therapy.5,18,19
Follow-up
Baseline data were recorded immediately before the start of therapy. After the hospital stay, the participants received a patient diary and were asked to record all necessary data over the course of the follow-up period. The data included the reason and date of contacting a doctor of any medical specialty, the use of physiotherapy, daily use of pain killers, sports activity, and any severe problems regarding the initial treatment (hospital stay, surgery, and rehabilitation).
One year (± 2 weeks) after hospitalization, patients were seen again. Data recording was focused on profession, disability, retirement, sports behavior, and body mass index (BMI). Data to be assessed also included the detailed medical history and clinical examination of the patient by an orthopedic surgeon at baseline and at the 1-year follow-up.
Statistical analysis
Statistical analysis was done with SPSS (IBM SPSS Statistics, Version 23.0.; IBM Corp., Armonk, NY, USA). Metric variables were descriptively reported as mean and standard deviation. Statistical data were not normally distributed. Analyses included the chi-square test and the nonparametric Mann–Whitney U test to compare the effects. Statistical significance was set at p < 0.05. With a sample size of n = 60, we had 80% power to detect an effect size of d = 0.35, which can be considered small. A per-protocol analysis was carried out.
Results
Profession, disability, and retirement
At follow-up, 5 patients had changed their profession, partly within the company, because they were unable to perform their previous occupational duties any longer due to back pain. Particularly, people with jobs involving high physical stress (such as bricklayers or industrial mechanics) were affected. One patient had to give up her job as a geriatric nurse and was seeking other work. During the follow-up period, none of the patients had applied for disability benefits. Forty patients (66.7%) were employed, 15 (25%) retired, 4 were housewives (6.7%), and 1 was seeking work. The average loss of working time was 41.91 days, which represented an improvement of 48.2% in comparison to the year before hospitalization (86.95 days). These statistics only included patients with a job (n = 40) but not housewives (n = 4), retired people (n = 15), or patients seeking work (n = 1).
Sports behavior and BMI
The sports behavior of patients at baseline (period of 6 months previously) and at follow-up was recorded. Thirty-five patients had participated in sports on a regular basis and 13 people on an irregular basis; only 12 patients had not practiced any sports at all at follow-up. These 12 patients were part of the 24 participants who had refused to participate in any sports before baseline assessment. This result represented improvement in every category (Table 2). Activities included cycling (n = 21), Nordic walking or jogging (n = 21), exercising (n = 14), and swimming (n = 9). Sports intensity and duration differed according to age and personal interests.
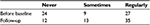  | Table 2 Patients’ frequency of sports participation before baseline and at follow-up (n = 60) Notes: Sometimes: less than twice a week and not every week; regularly: twice a week or more. |
The BMI was also measured at follow-up. The mean BMI was 28.62 (± 4.3) kg/m2, ranging between 21.48 and 40.49 kg/m2; thus, there was hardly any change within the follow-up period (Table 3). At follow-up, 10 patients had normal weight, 25 patients were overweight, 15 patients were obese, and 1 patient was severely obese.
  | Table 3 Descriptive statistics for body mass index (kg/m2) of patients before baseline and at follow-up (n = 60) |
Use of health services
The study also analyzed the use of analgesics and nonsurgical treatment received during the 1-year follow-up period after MPM. With regard to analgesics, patient statements ranged from “no use” to “regular use of 2 painkillers per day”. The number of patients who had used analgesics on a regular basis was reduced from 26 to 12. The number of patients who did not require any analgesics at all was increased from 14 to 32. The median had shifted from “regularly” to “no use”. Therefore, the use of analgesics was significantly (p < 0.05) reduced. In addition, the need for nonsurgical treatment was recorded for the period between discharge and follow-up. At follow-up, 40 patients reported to have received nonsurgical treatment since discharge from hospital. Multiple answers were possible. Twenty patients had not required any conservative treatment.
Discussion
This study aimed at proving the positive mid-term effect – particularly on socioeconomic factors and health care utilization – of a multimodal inpatient therapeutic concept based on drug injections for patients with lumbar radiculopathy. Socioeconomic factors included profession, disability, and retirement as well as sports behavior and BMI. These factors cannot be simply used as parameters to compare international systems but should rather be used to complement the holistic picture of the disease and its accompanying factors, particularly in view of the widely varying international conditions regarding sick leave, job situations, and legal provisions.
Profession, disability, and retirement
The number of working years lost is used to present potential losses for an economy. This number is calculated by means of incapacity, disability, and premature death. In 2002, the number of employment years in Germany was 5.1 million years. Injuries and poisoning caused almost a quarter of all working years lost. Approximately 0.8 million working years (15.5%) were lost because of musculoskeletal diseases and connective tissue disorders and 0.4 million working years because of dorsopathy. In the present study, none of the patients had retired prematurely. However, the follow-up examination took place already after 1 year, so no accurate conclusion was possible in this respect. A follow-up examination after several years would be more useful in this respect.
Of much greater importance is the loss of production caused by people not being able to work, both in a socioeconomic and an economic sense. Total treatment costs are only marginally influenced by the reduced use of drugs. Ultimately, treatment costs can only be reduced by decreasing recurrence rates, trends in chronicity, and absenteeism rates and be curbed by successful prevention in the long run.20
The average loss of working hours of our patients was 41.91 days in the follow-period, which represented an improvement of 48.2% in comparison to the year before therapy. However, our study excluded retired patients. Average days of the follow-up in our study included the time for inpatient treatment. Patients did not work immediately after discharge from hospital. Work reintegration was also a substantial proportion of the prolonged loss of working time because some patients only worked on an hourly basis. The possibility to start work on an hourly basis per day was viewed very positively by the participants. As reported by Nagel and Korb, the cost effectiveness of multimodal treatment was shown because patients were able to return to work earlier, other health services were rarely used, and premature retirement could be avoided.21
Sports behavior and BMI
At follow-up, 35 patients had practiced sports on a regular basis, 13 occasionally, and only 12 had never exercised. These 12 patients were part of the 24 participants who had refused any sports activity before baseline. Activities included cycling (n = 21), Nordic walking or jogging (n = 21), exercising (n = 14), and swimming (n = 9). Sports intensity and duration differed according to age and personal interests. Because exercising and sports are important for the long-term improvement of spinal disorders, such activities are also part of the multimodal treatment concept. It is important that – after discharge from hospital – patients continue working on their personal fitness and the stability of their back muscles, which ensures muscular support of the spine. Such measures also strengthen the health awareness of patients. Patients need to understand that they have to contribute to MPM to achieve the desired outcome. It should be noted that 1 year after therapy, most patients (80%) participated in sports activities or were physically active, and this rate was 20% higher than that before treatment. This fact is also important for the outcome of MPM because physical activity may be assumed to not only result in stronger back muscles but also increase the health awareness of patients.
Furthermore, excess body weight represents an additional burden to an already stressed spine, and regular exercise can counteract elevated BMI values. Obesity is one of the risk factors for back pain but has a lower impact than psychosocial influences.22 The mean BMI at follow-up was still 28.62 (± 4.3) kg/m2; thus, body weight had not decreased during the follow-up period, although some patients had reported some weight loss to release stress from the spine. The average BMI of our study population was slightly higher than that of the general German population (25.9 kg/m2).23 Schmidt and Kohlmann described an about 1.5-fold risk of back pain for overweight people.24 This figure was confirmed by our study, in which the majority of patients were overweight.
Use of health services
The following section is focused on the use of analgesics before and after MPM as well as on the need for nonsurgical treatment between discharge from hospital and follow-up. The National Disease Management Guideline for low back pain recommends the early use of analgesics.25 At the initial examination of our patient group, 14 patients had not taken any analgesics, 20 had taken medication when necessary, and 26 had used analgesics on a regular basis. These figures emphasize the implementation of this guideline. Only 23% of our patients had not been consistently treated with medication, maybe because of the reserved attitude of patients towards analgesics. Patients often fear side effects or becoming addicted to pain medication. At follow-up, 32 patients did not require any analgesics, 16 took analgesics when necessary, and only 12 took them regularly (more than 1 peripheral analgesic). The number of patients with regular use could be decreased from 26 to 12. The number of patients who did not take any analgesics had increased from 14 to 32. According to Theodoridis and Kramer, one aim of MPM should be the decrease in drug use.26 In the medium term, patients should only require small doses of analgesics or, ideally, none at all. This requirement was met by the significant result of reducing the need for analgesics in our study population (p < 0.05). Of course, the need for analgesics is correlated with pain intensity and everyday limitations.
Another aspect of the use of health services is the need for nonsurgical treatment options and their perception. In our study, the number of citations was 27 for “physiotherapy”, 12 for “rehabilitation”, 5 for “acupuncture”, and 2 for “other treatments”. Multiple answers were possible. Twenty patients had not used any of these therapeutic options during the year after treatment. In addition, patients had been instructed in isometric exercises and back pain prevention during their inpatient stay. These issues and their individual implementation at home in addition to sports activities are important for ensuring treatment success. However, it is difficult to regard the use of health services as a hard indicator for treatment success because several other factors are also crucial but difficult to compare on an international basis. Treatment outcome critically depends on health insurance companies, the personal motivation of the patients, and − last but not least − the availability and accessibility of medical care.
Although this study yielded satisfactory results, it had some limitations. We have no data on how far patients were influenced by the principle of social desirability when answering the questions and how reliably the medical diaries were recorded over the year of observation.
Another limiting factor is the lack of a control group. However, because we aimed at evaluating the overall concept of MPM and not just the subitem of a single injection as seen in other studies, we considered the implementation of a control group ethically difficult. Patients in the control group would have received placebo injections instead of effective drugs, which can also be seen as crucial. On the other hand, due to a missing control group without MPM, the natural history of the complaints after 1 year cannot be ruled out.
The per-protocol analysis may also have a selection bias. However, patients who had to be excluded after 1 year were excluded either because of their unwillingness to participate due to the long travel distance to the hospital or because they had not completed their follow-up diary, but none of them mentioned any medical issues.
Conclusion
MPM is an effective approach to treating lumbar radiculopathy and reducing its negative influence on socioeconomic factors. Therapeutic benefits also include a decrease in health care utilization. Therefore, health care providers should place the mid-term success for patients and socioeconomic factors before the short-term costs of therapy.
Acknowledgments
The authors thank Monika Schoell for the linguistic review of the manuscript. This work was supported by the German Research Foundation [Deutsche Forschungsgemeinschaft] within the funding program Open Access Publishing.
Disclosure
The authors report no competing financial interests or conflicts of interest in this work.
References
Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. | ||
Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. | ||
Benditz A, Madl M, Loher M, Grifka J, Boluki D, Linhardt O. Prospective medium-term results of multimodal pain management in patients with lumbar radiculopathy. Sci Rep. 2016;6:28187. | ||
Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88 Suppl 2:21–24. | ||
Arnold B, Brinkschmidt T, Casser HR, et al. Multimodale Schmerztherapie Konzepte und Indikation [Multimodal pain therapy: principles and indications]. Schmerz. 2009;23(2):112–120. German [with English abstract]. | ||
Anson P. Experts say epidural steroid injections overused. Available from: http://www.painnewsnetwork.org/stories/2015/8/19/experts-say-epidural-injections-overused. Accessed May 1, 2016. | ||
Berkman ND, Lohr KN, Ansari M, et al. Grading the strength of a body of evidence when assessing health care interventions: an EPC update. J Clin Epidemiol. 2015;68(11):1312–1324. | ||
Kreiner DS, Hwang SW, Easa JE, et al; North American Spine Society. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014;14(1):180–191. | ||
Manchikanti L, Kaye AD, Manchikanti K, Boswell M, Pampati V, Hirsch J. Efficacy of epidural injections in the treatment of lumbar central spinal stenosis: a systematic review. Anesth Pain Med. 2015;5(1):e23139. | ||
Chou R, Hashimoto R, Friedly J, et al. Pain Management Injection Therapies for Low Back Pain. Rockville, MD: Agency for Healthcare Research and Quality (US); 2015. | ||
National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management. NICE guideline [NG59]; published November 2016. Available from: https://www.nice.org.uk/guidance/NG59. Accessed October 1, 2016 [Draft version]. | ||
Kraemer J, Ludwig J, Bickert U, Owczarek V, Traupe M. Lumbar epidural perineural injection: a new technique. Eur Spine J. 1997;6(5):357–361. | ||
Manchikanti L, Pampati V, Benyamin RM, Boswell MV. Analysis of efficacy differences between caudal and lumbar interlaminar epidural injections in chronic lumbar axial discogenic pain: local anesthetic alone vs. local combined with steroids. Int J Med Sci. 2015;12(3):214–222. | ||
Manchikanti L, Cash KA, McManus CD, Pampati V, Benyamin RM. A randomized, double-blind, active-controlled trial of fluoroscopic lumbar interlaminar epidural injections in chronic axial or discogenic low back pain: results of 2-year follow-up. Pain Physician. 2013;16(5):E491–E504. | ||
Jacobson E, editor. Entspannung als Therapie. Progressive Relaxation in Theorie und Praxis [Relaxation as a therapy. Progressive relaxation in theory and practice]. 7th ed. Stuttgart: Klett-Cotta; 1990. German. | ||
Hamel M, Maier A, Weh L, Klein A, Lucan S, Marnitz U. “Work hardening” bei chronischen Rückenschmerzen. Ein integraler Bestandteil multimodaler Therapieprogramme [“Work hardening” for chonic back pain. An integral component of multimodal therapy programs]. Orthopade. 2009;38(10):928, 930–936. German [with English abstract]. | ||
Casser HR, Arnold B, Brinkschmidt T, et al. Interdisziplinäres Assessment zur multimodalen Schmerztherapie Indikation und Leistungsumfang [Multidisciplinary assessment for multimodal pain therapy. Indications and range of performance]. Schmerz. 2013;27(4):363–370. German [with English abstract]. | ||
Hirsch O, Strauch K, Held H, et al. Low back pain patient subgroups in primary care: pain characteristics, psychosocial determinants, and health care utilization. Clin J Pain. 2014;30(12):1023–1032. | ||
Nagel B, Pfingsten M, Brinkschmidt T, et al. Struktur- und Prozessqualität multimodaler Schmerztherapie Ergebnisse einer Befragung von schmerztherapeutischen Einrichtungen [Structure and process quality of multimodal pain therapy. Results of a survey of pain therapy clinics]. Schmerz. 2012;26(6):661–669. German [with English abstract]. | ||
Bolten W. Rheumatische Krankheiten [Rheumatic Diseases]. In: Fritze J, Mehrhoff F, editors. Die ärztliche Begutachtung. Stuttgart: Steinkopf; 2008;441–451. German. | ||
Nagel B, Korb J. Multimodale Therapie [Multimodal therapy]. Orthopade. 2009;38(10):907–912. | ||
Gray DT, Hollingworth W, Onwudiwe N, Jarvik JG. Costs and state-specific rates of thoracic and lumbar vertebroplasty, 2001–2005. Spine (Phila Pa 1976). 2008;33(17):1905–1912. | ||
Mikrozensus - Fragen zur Gesundheit - Körpermaße der Bevölkerung [Micro-census - questions about health - body measurements of the population]. German Federal Office for Statistics; 2013. Available from: https://www.destatis.de/DE/Publikationen/Thematisch/Gesundheit/Gesundheitszustand/Koerpermasse5239003139004.pdf?__blob=publicationFile. Accessed March 20, 2016. German. | ||
Schmidt CO, Kohlmann T. Was wissen wir über das Symptom Rückenschmerz? Epidemiologische Ergebnisse zu Prävalenz, Inzidenz, Verlauf, Risikofaktoren [What do we know about the symptoms of back pain? Epidemiological results on prevalence, incidence, progression and risk factors]. Z Orthop Ihre Grenzgeb. 2005;143(3):292–298. German. | ||
National Disease Management Guideline; Low back pain. Short Version; 1st Edition; Version 5; January 2011. Last amended: October 2015. National Programme for Disease Management Guidelines. http://www.leitlinien.de/mdb/downloads/nvl/kreuzschmerz/kreuzschmerz-1aufl-vers5-short.pdf. Accessed October 4, 2015. | ||
Theodoridis T. Stellenwert der injektionstherapie bei degenerativen erkrankungen der lendenwirbelsäule [Value of injection therapy for degenerative diseases of lumbar spine]. Orthopade. 2012;41(2):94–99. German. | ||
Operationen- und Prozedurenschlüssel [Operation and Procedure Code] German modification of the International Classification of Procedures in Medicine [Internationalen Klassifikation der Prozeduren in der Medizin (ICPM)]. Available from: https://www.dimdi.de/static/de/klassi/ops/kodesuche/onlinefassungen/opshtml2017/. Accessed May 1, 2016. German. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
