Back to Journals » Cancer Management and Research » Volume 11
Poor Prognosis With Coexistence Of EGFR T790M Mutation And Common EGFR-Activating Mutation In Non- Small Cell Lung Cancer
Authors Gao X, Zhao Y, Bao Y, Yin W, Liu L , Liu R, Yu Z, Zhou X, Shuai J
Received 22 May 2019
Accepted for publication 9 October 2019
Published 13 November 2019 Volume 2019:11 Pages 9621—9630
DOI https://doi.org/10.2147/CMAR.S216721
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Lu-Zhe Sun
Xuejuan Gao,1,* Yanfeng Zhao,2,* Yi Bao,2,* Wei Yin,3 Liyu Liu,4 Ruchuan Liu,4 Zhengquan Yu,5 Xiao Zhou,2 Jianwei Shuai1,6
1Department of Physics, Xiamen University, Xiamen, People’s Republic of China; 2Department of Thoracic Surgery, Shanghai Pulmonary Hospital Affiliated to Tongji University, Shanghai, People’s Republic of China; 3Key Laboratory of Oral Biomedical Engineering of Education, Hospital of Stomatology, Wuhan University, Wuhan, People’s Republic of China; 4College of Physics, Chongqing University, Chongqing, People’s Republic of China; 5State Key Laboratories for Agrobiotechnology and Beijing Advanced Innovation Center for Food Nutrition and Human Health, College of Biological Sciences, China Agricultural University, Beijing, People’s Republic of China; 6State Key Laboratory of Cellular Stress Biology, Innovation Center for Cell Signaling Network, Xiamen University, Xiamen, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jianwei Shuai
Department of Physics, Xiamen University, Siming South Road 422-19, Xiamen 361005, People’s Republic of China
Tel +86 13959287814
Email [email protected]
Xiao Zhou
Department of Thoracic Surgery, Shanghai Pulmonary Hospital affiliated to Tongji University, 507 Zhengmin Road, Wu Jiao Chang, Yangpu, Shanghai 200433, People’s Republic of China
Tel +86 13916118590
Email [email protected]
Purpose: Previous studies have shown that the presence of EGFR T790M mutation may reduce the treatment efficacy of tyrosine kinase inhibitors (TKIs) in EGFR-mutant lung cancer. However, little is known about the clinical features and outcomes of EGFR T790M mutation in pretreated patients with NSCLC.
Patients and methods: The clinical features of EGFR-activating and T790M mutations were assessed in a large cohort of patients with EGFR-TKI-naïve NSCLC (all/EGFR mutations, n=16,347/7,687). The correlation between the pretreatment T790M mutation status and clinical outcomes was evaluated using univariate and multivariate analyses.
Results: Pretreatment T790M mutation was reported in 1.39% of the patients and coexisted with an EGFR-activating or uncommon mutation. The dual EGFR T790M and common EGFR-activating mutations were more likely to be detected in lung adenocarcinoma, whereas single T790M mutation was more prevalent in non-adenocarcinomas. The presence of de novo T790M mutation correlated with reduced recurrence-free survival (RFS) in patients with NSCLC (odds ratio [OR] 3.37, 95% confidence interval [CI] 1.67–6.79, P = 0.001). After molecular stratification, T790M mutation was shown to exert adverse effects on the RFS of EGFR 19-del group (OR 2.89, 95% CI 1.10–7.91, P = 0.028) and EGFR L858R group (OR 3.43, 95% CI 1.33–8.88, P = 0.013). Furthermore, pretreatment T790M mutation promoted tumor metastasis to different sites.
Conclusion: T790M-positive tumors presented special clinical features, and the coexistence of T790M and common EGFR-activating mutations was associated with poor prognosis in patients with NSCLC.
Keywords: pretreatment T790M mutation, dual EGFR mutations, recurrence-free survival, non-small cell lung cancer
Introduction
Exon 19 deletion and point mutation in L858R are the most common somatic activating mutations in the gene encoding epidermal growth factor receptor (EGFR) that confers sensitivity to EGFR tyrosine kinase inhibitors (TKIs) in non-small cell lung cancer (NSCLC).1,2 However, patients with advanced-stage NSCLC harboring EGFR TKI-sensitive mutations may develop progressive disease after a median response period of 12 months, mainly owing to the acquired resistance to EGFR-TKIs through secondary mutations.3
Substitution of the putative gatekeeper threonine residue at position 790 with methionine (T790M) within exon 20 of EGFR, the most frequently reported secondary mutation, accounts for approximately half of the acquired resistance to EGFR-TKIs.4–6 T790M mutation enhances the ATP-binding affinity of EGFR-mutated cells.7,8 As both first- and second-generation TKIs are competitive ATP inhibitors, their efficacy is decreased in the presence of T790M mutation.9
Although EGFR T790M mutation is common after the development of resistance to EGFR-TKI treatment in patients with NSCLC, T790M is still uncommon in unselected patients with NSCLC at diagnosis. Considering that an estimated 1% of EGFR-mutant lung cancers harbor T790M mutations at diagnosis,10–13 approximately 20,996 patients annually diagnosed in the world with lung cancers are thought to carry de novo EGFR T790M mutations.14 However, the EGFR T790M mutation rate and the clinicopathological features related to its likelihood before treatment remain unknown in Chinese patients. In the present study, we report the clinicopathological and imageological characteristics and clinical outcomes of patients suffering from NSCLC with pretreatment T790M mutation in tumors.
Materials And Methods
Patient Population
A total of 16,347 patients diagnosed with NSCLC were recruited from the Shanghai Pulmonary Hospital affiliated to Tongji University in China between February 2013 and December 2017. All patients were diagnosed with NSCLC and their tumors were genotyped for EGFR mutations. Patients were grouped into two populations based on the status of EGFR T790M mutation as follows: (1) EGFR T790M-positive group and (2) EGFR T790M-negative group. All patients provided a written informed consent. The study was approved by the institutional review board at the Shanghai Pulmonary Hospital (Institutional number of ethics consent: K16-257) and was conducted in accordance with the Declaration of Helsinki.
Candidate Gene Mutation Analysis
The Amplification Refractory Mutation System (ARMS) was used as the molecular diagnostic method in our study. Between February 2013 and December 2015, genomic DNA and total RNA were extracted from fresh tissues using the QIAamp DNA Tissue Kit and RNeasy Kit (Qiagen, Germany), respectively. Mutations in the EGFR and KRAS genes and the echinoderm microtubule-associated protein-like 4 and anaplastic lymphoma kinase (EML4-ALK) rearrangement were detected with Amoy Diagnostics Kits (Xiamen, China) as per the manufacturer’s protocol.15 Between January 2016 and December 2017, DNA and total RNA were extracted from five serial slices of a 5-μm paraffin section using the DNA FFPE Tissue Kit and RNeasy Kit (Qiagen, Germany). Mutations in EGFR and KRAS genes as well as EML4-ALK rearrangement were detected according to the manufacturer’s protocol of the ACCB Diagnostics Kits (Beijing, China).16 The test could detect mutations at a sensitivity of 1% with no less than 5 ng/μL of DNA sample.
Clinical Assessment
Patient characteristics at the time of lung cancer diagnosis, including age, gender, smoking status, tumor size, pathological TNM stage, tumor morphology, location, histological type, internal structure, lobulation, margin, shape, spiculation, and texture, were retrospectively collected. Smoking status is divided into current smoker, previous smoker, and never smoker. Current smokers are defined as people who reported smoking at least 100 cigarettes during their lifetime and who, at the time they participated in a survey about this topic, reported smoking in the last days. Previous smokers are defined as people who have smoked greater than 100 cigarettes in their lifetime but have not smoked in the last 28 days. Never smokers are defined as people who have not smoked greater than 100 cigarettes in their lifetime and do not currently smoke. Recurrence-free survival (RFS) was calculated from the date of surgical resection until the date of confirmed recurrence from any cause. Patients that were alive at the time of analysis were censored at the last known date of follow-up. All the patients had surgery and were followed-up for more than 12 months.
Statistical Analysis
We compared the clinicopathological features of patients harboring EGFR-T790M mutations with patients harboring T790M-negative mutations. The T790M-negative population used for clinicopathological features analysis was consecutively collected at our department from 1st January 2015 to 16th January 2015.17 The RFS for T790M-negative patients were chosen from those that underwent surgery on the same day as the T790M-positive patients or with the surgery time closest to that of T790M-positive patients. No differences in the clinicopathological features were detected between those two T790M-negative populations (Table S1). Statistically significant differences in categorical variables between groups were analyzed with the Χ2 tests or Fisher’s exact test as appropriate. RFS was estimated by the Kaplan–Meier method, and the log-rank test was used for univariate analysis. Cox-proportional hazard model was used for multivariate analysis. The covariates considered for multivariate analysis were gender, aging, TNM stage, tumor size, and smoking. Two-sided values of P < 0.05 were considered statistically significant. SPSS version 20.0 for Windows (IBM SPSS Statistics, Chicago, IL) was used for statistical analyses.
Results
Distribution Of T790M Mutation
Of 16,347 patients with NSCLC, 7687 with EGFR mutations were included in the analysis. All the cases were EGFR-TKI-naïve patients with NSCLC. The uncommon T790M mutation was identified in 106 patients, which corresponded to 1.39% of the patients with EGFR mutations (Figure 1A). EGFR L858R mutation and 19-del mutation comprised 48.34% and 41% of all EGFR mutations, respectively. The dual 19-del and L858R mutations were observed in 44 (0.57%) patients. Other uncommon EGFR mutations observed in the cohort included 139 (1.81%) cases of L861Q mutations, 158 (2.06%) cases of G719X mutations, and 223 (2.9%) cases with 20-ins.
 |
Figure 1 Schematic view of the frequency of EGFR mutations. (A) Comprehensive view of EGFR mutations and (B) distribution of T790M mutation. |
EGFR T790M mutations were observed in 106 patients. As listed in Figure 1B, only 11 (10.38%) of all patients with T790M mutations showed single T790M mutation, while 65 (61.32%) patients were positive for dual L858R and T790M mutations and 26 (24.53%) patients showed dual 19-del and T790M mutations. In addition, 1 (0.94%) patient each showed dual L861Q and T790M mutations and dual G719X and T790M mutations, while 2 (1.89%) patients were positive for multiple 19-del, L858R, and T790M mutations.
Clinicopathological Characteristics
T790M mutation was identified in 106 patients, but 4 patients were excluded owing to the lack of clinicopathological information. The clinical characteristics of 102 T790M-positive and 105 T790M-negative cases are summarized in Table 1. No differences were observed in sex, histology, adenocarcinoma subtype, visceral pleura invasion, TNM stage, tumor size, site, and KRAS mutation between the two groups. However, the proportion of females was higher in T790M-positive group than in T790M-negative group, although no statistical significance was observed (P = 0.092). The incidence of EML4-ALK mutation was significantly higher in T790M-positive group than in T790M-negative group (P = 0.05), indicating that EML4-ALK mutation occurred more frequently in EGFR T790M-positive patients.
 |
Table 1 The Clinicopathological Characteristics Of 207 Patients With NSCLC |
To investigate the clinical significance of T790M mutation, we stratified 102 T790M-positive patients into three groups on the basis of single or dual T790M mutations. As shown in Table 2, no differences in age, sex, adenocarcinoma subtype, visceral pleura invasion, TNM stage, site, KRAS mutation, and EML4-ALK mutation were observed among the three groups. However, the number of patients with tumor size less than 3 cm was higher in dual T790M and L858R mutations group than in single T790M mutation group, although no statistical significance was achieved (P = 0.079). The number of patients that never smoked was significantly higher in T790M mutation group than in dual T790M and L858R mutations group (P = 0.042). The ratio of adenocarcinoma was significantly higher in dual EGFR mutations group than in single T790M mutation group, indicating that the frequency of single T790M mutation was lower in patients with adenocarcinoma.
 |
Table 2 The Clinicopathological Characteristics In Patients With T790M-Positive Mutation |
Patient Imageological Characteristics
The imageological characteristics of patients with NSCLC were analyzed with respect to internal structure, margin, shape, texture, and presence of lobulation and spiculation.18–22 These characteristics of 102 T790M-positive and 105 T790M-negative patients are shown in Table S2. No differences in internal structure, margin, spiculation, and texture were detected between the two groups. The proportion of marked lobulation (P = 0.025) and shape irregularity (P = 0.047) was significantly higher in T790M-positive group than in T790M-negative group.
For T790M-positive cases, no differences in internal structure, margin, shape, texture, and presence of lobulation were reported among the three groups (Table S3). The percentage of cases with spiculation was higher in the single T790M mutation group than in dual T790M and L858R mutations group, although the difference was not statistically significant (P = 0.073). However, the proportion of spiculation was significantly higher in single T790M mutation group than in the group with dual T790M and 19-del mutations (P = 0.005) as well as in dual T790M and L858R mutations group than in dual T790M and 19-del mutations group (P = 0.039).
Analysis Of RFS
Kaplan–Meier analysis revealed the significantly shorter median RFS for patients with EGFR T790M mutations than for those without T790M mutations (odds ratio [OR] 3.37, 95% confidence interval [CI] 1.67–6.79, P = 0.001, Figure 2A). We divided patients into the following two subgroups to investigate the effects of EGFR T790M on EGFR-sensitive mutations: EGFR 19-del mutation group and EGFR L858R mutation group. Of 44 patients with EGFR 19-del mutations, 17 with de novo T790M showed significantly shorter RFS than the 27 patients without T790M (OR 2.89, 95% CI 1.10–7.91, P = 0.028, Figure 2B). Similarly, 54 patients with de novo T790M experienced a significantly shorter RFS than the 27 patients without T790M in EGFR L858R mutation cohort (OR 3.43, 95% CI 1.33–8.88, P = 0.013, Figure 2C). In addition, we stratified all T790M-positive patients into two subgroups based on their need for adjuvant therapy after surgery (Figure 3A and B). The RFS of patients in stage IA group (no specific treatment) (OR 5.18, 95% CI 1.22–10.98, P = 0.008, Figure 3A) and stage IB-IIIA group (adjuvant therapy) (OR 2.56, 95% CI 1.15–5.67, P = 0.045, Figure 3B) with T790M mutation was significantly shorter than that of patients without T790M mutations. In multivariate analysis, patients with EGFR T790M mutation tended to have a shorter RFS than those without T790M mutation, although no statistical significance was achieved (hazard ratio [HR] 1.64, P = 0.123, Table 3). The presence of de novo T790M mutation emerged as a marker of shorter RFS upon coexistence with L858R mutation (HR 3.53, P = 0.043, Table 3). Our data indicate that de novo EGFR T790M mutation may serve as a poor prognostic indicator for patients with EGFR-activating mutations in terms of RFS.
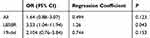 |
Table 3 Multivariate Analysis For Recurrence-Free Survival |
Metastasis Of Patients
As shown in Figure 4, the presence of T790M mutation correlated with the number of metastatic organs. The proportion of patients with more than two metastatic sites was significantly greater in T790M-positive group than in T790M-negative group (P = 0.039). We divided all T790M-positive patients into two groups based on the status of concurrent EGFR mutation (19-del or L858R mutation). Patients with dual EGFR L858R and T790M mutations tended to display a higher incidence of multiple site metastases than those with single L858R mutation, although no statistical significance was found (P = 0.075). No difference in single metastatic site (brain, bone, lung) was observed between T790M-positive and T790M-negative cohorts.
Discussion
T790M mutation is not only a resistant mechanism but also a clinically significant biomarker following acquired resistance to EGFR-TKIs. Several reports have considered T790M as a favorable prognostic marker after acquired resistance.13,23–25 Researchers have explored the relationship between prognosis and de novo T790M mutation.25–30 However, these previous studies have been carried out with a relatively small number of cases; hence, the information provided is limited. In the present study, we comprehensively analyzed the clinicopathological and imageological characteristics and clinical outcomes in a larger cohort of patients with NSCLC, especially in patients with early-stage NSCLC harboring de novo T790M mutation and determined the correlation between pretreatment T790M mutation status and clinical outcomes.
Pretreatment T790M mutation was reported in 1.39% of the patients and coexisted with an EGFR-activating or uncommon mutation, consistent with the findings of previous studies.10,12,13 This observation suggests no selection bias in the study cohorts. Pretreatment EGFR T790M mutation was reported to be relatively frequent (95/106; 89.62%) in patients carrying concomitant sensitive EGFR mutations. As T790M mutation is weakly oncogenic by itself, its oncogenic potential is greatly enhanced in combination with another common EGFR-activating mutation such as L858R.11 Our data demonstrated that the frequency of de novo T790M mutation in patients with NSCLC harboring dual EGFR T790M and L858R mutations was almost 2.5 times higher (65 vs 26) than that in patients harboring dual EGFR T790M and 19-del mutations, consistent with the previous reports.23,27,31
Here we showed that the incidence of EML4-ALK mutation was significantly higher in T790M-positive group than in T790M-negative group, indicating that EML4-ALK mutation occurred more frequently in EGFR T790M-positive NSCLC patients. The combination of T790M and EML4-ALK mutations may synergistically enhance the oncogenic potential of both mutations. A recently published review article suggested that the coexistence of EML4-ALK and T790M mutations may serve as a mechanism of resistance to third-generation TKIs,32 paving a way for the development of dual ALK/EGFR inhibitors.33
Evaluation of clinicopathological characteristics revealed the absence of any association between pretreatment T790M mutation and the majority of the clinicopathological characteristics such as age, stage, tumor size, or tumor site, consistent with the previously reported results.34 We also found that the single T790M mutation was more frequent in females, non-smokers, and non-adenocarcinoma patients than in males, smokers, and adenocarcinoma patients. In combination with T790M mutation, the dual EGFR mutations such as single-activating EGFR mutation were more likely to be detected in lung adenocarcinoma than in non-adenocarcinoma.1,24,35,36
Imageological characteristics of T790M-positive and T790M-negative patients are yet incompletely established. We observed that T790M-positive patients presented marked lobulation and irregular shape. Given the limited number of patients with EGFR T790M mutation, we failed to establish imageological characteristics of patients with single T790M mutation that warrants further studies.
T790M mutation conferred additional transforming properties in combination with the common EGFR-activating mutations and significantly affected the RFS. In our study, the presence of de novo T790M mutation correlated with reduced RFS in patients with NSCLC in combination with an EGFR-activating mutation, indicating that EGFR T790M mutation may serve as a poor prognostic indicator for patients with EGFR-activating mutation in terms of RFS. The presence of de novo T790M mutation was associated with inferior RFS in patients with NSCLC that accepted adjuvant therapy after surgery.
The presence of T790M mutation also correlated with tumor metastatic capability. The proportion of patients with more than two metastatic sites was significantly higher in T790M-positive group than in T790M-negative group (P = 0.039). Patients with dual EGFR L858R and T790M mutations tended to exhibit a higher incidence of multiple site metastases than those with single L858R mutation, although no statistical significance was reported (P = 0.075).
The role of T790M mutation in lung cancer progression, especially before TKIs treatment, is still being debated. Yosuke Togashi et al demonstrated that the inhibition of β-catenin signal-mediated cancer stem cell-like properties resulted in an increase in the anticancer effects of irreversible EGFR-TKIs in EGFR-mutated NSCLC carrying T790M mutation.37 Thus, the stemness of cancer cells carrying dual EGFR-activating mutation and T790M mutation may contribute to the progression of disease. The activation of cell growth, proliferation, or apoptosis-related signaling pathways may also explain the worse RFS in patients with NSCLC harboring pretreatment concomitant EGFR T790M mutation. Co-targeting EGFR and signaling proteins, such as Src,38 Orphan receptor 1 (ROR1),39 and vascular endothelial cell growth factor (VEGF),40 showed a significant synergistic effect by overcoming or delaying the resistance to EGFR inhibitors in pre-clinical and clinical studies. It is unclear whether patients harboring pretreatment T790M mutation will benefit more from third-generation EGFR-TKIs than those without pretreatment T790M mutation. Several ongoing clinical trials may help researchers explore this important issue.41–44
Our study has several limitations. First, despite the inclusion of larger-scale data than previous studies, the results were produced from the patients at a single institution. Second, as this was a retrospective study, we failed to analyze non-tumor tissues to rule out the effects of germline T790M mutation. Third, the prevalence of pretreatment T790M mutation varied with analyses using different detection methods and ranged from 0.5% to 79%.25,28,45–47 The frequency of T790M mutation was 1.39%, consistent with the results of a study from another center in China.48 Different detection and sampling methods led to the differences in prevalence rates, owing to variations in sensitivity and specificity. We evaluated EGFR mutation status by ARMS. ARMS use specific primer that binds with a target sequence during the annealing step to enrich the sequence, which can achieve a higher specificity. EGFR T790M mutation is a somatic mutation, mutant cells are usually mixed with wild type cells; thus, the extracted DNA often has a large amount of wild type DNA, and so the detection of such somatic mutation needs higher specificity. Taken together, ARMS is one of the best options for T790M detection after balancing sensitivity and specificity.
Conclusion
The presence or absence of EGFR T790M mutation confers different disease characteristics and prognosis. We analyzed the clinicopathological characteristics of pretreated patients with NSCLC harboring de novo T790M mutations and determined the correlation between T790M mutation status and clinical outcomes. Our results indicate that the pretreatment T790M mutation tended to affect the imageological characteristics of NSCLC and that the presence of T790M mutation was associated with poor prognosis of patients with NSCLC.
Acknowledgment
We would like to acknowledge the funding support of National Natural Science Foundation of China (Grant No. 11675134, No. 11474345, No. 674043, No. 11874310 and No. 81572614).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350(21):2129–2139. doi:10.1056/NEJMoa040938
2. Rosell R, Moran T, Queralt C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med. 2009;361(10):958–967. doi:10.1056/NEJMoa0904554
3. Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non–small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362:2380–2388. doi:10.1056/NEJMoa0909530
4. Lecia V, Sequist BAW, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Clin Cancer Res. 2011;3:1169–1180.
5. Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res. 2013;19(8):2240–2247. doi:10.1158/1078-0432.CCR-12-2246
6. Arcila ME, Oxnard GR, Nafa K, et al. Rebiopsy of lung cancer patients with acquired resistance to EGFR inhibitors and enhanced detection of the T790M mutation using a locked nucleic acid-based assay. Clin Cancer Res. 2011;17(5):1169–1180. doi:10.1158/1078-0432.CCR-10-2277
7. Gainor JF, Shaw AT. Emerging paradigms in the development of resistance to tyrosine kinase inhibitors in lung cancer. J Clin Oncol. 2013;31(31):3987–3996. doi:10.1200/JCO.2012.45.2029
8. Chong CR, Janne PA. The quest to overcome resistance to EGFR-targeted therapies in cancer. Nat Med. 2013;19(11):1389–1400. doi:10.1038/nm.3388
9. Yu HA, Pao W. Targeted therapies: Afatinib–new therapy option for EGFR-mutant lung cancer. Nature Rev Clin Oncol. 2013;10(10):551–552. doi:10.1038/nrclinonc.2013.154
10. Wu JY, Yu CJ, Chang YC, Yang CH, Shih JY, Yang PC. Effectiveness of tyrosine kinase inhibitors on “uncommon” epidermal growth factor receptor mutations of unknown clinical significance in non-small cell lung cancer. Clin Cancer Res. 2011;17(11):3812–3821. doi:10.1158/1078-0432.CCR-10-3408
11. Gazdar A, Robinson L, Oliver D, et al. Hereditary lung cancer syndrome targets never smokers with germline EGFR gene T790M mutations. J Thorac Oncol. 2014;9(4):456–463. doi:10.1097/JTO.0000000000000130
12. Oxnard GR, Miller VA, Robson ME, et al. Screening for germline EGFR T790M mutations through lung cancer genotyping. J Thorac Oncol. 2012;7(6):1049–1052. doi:10.1097/JTO.0b013e318250ed9d
13. Yu HA, Arcila ME, Harlan Fleischut M, et al. Germline EGFR T790M mutation found in multiple members of a familial cohort. J Thorac Oncol. 2014;9(4):554–558. doi:10.1097/JTO.0000000000000052
14. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
15. Yang Z, Yang N, Ou Q, et al. Investigating novel resistance mechanisms to third-generation EGFR tyrosine kinase inhibitor osimertinib in non-small cell lung cancer patients. Clin Cancer Res. 2018;24(13):3097–3107. doi:10.1158/1078-0432.CCR-17-2310
16. Wang X, Gao Y, Wang B, et al. Analytic and clinical validation of an ultrasensitive, quantitative polymerase chain reaction assay for EGFR mutation analysis with circulating tumor DNA. Arch Pathol Lab Med. 2017;141(7):978–984. doi:10.5858/arpa.2016-0083-OA
17. Pan Y, Zhang Y, Li Y, et al. Prevalence, clinicopathologic characteristics, and molecular associations of EGFR exon 20 insertion mutations in East Asian patients with lung adenocarcinoma. Ann Surg Oncol. 2014;21(Suppl 4):S490–S496. doi:10.1245/s10434-013-3452-1
18. Firmino M, Angelo G, Morais H, Dantas MR, Valentim R. Computer-aided detection (CADe) and diagnosis (CADx) system for lung cancer with likelihood of malignancy. Biomed Eng Online. 2016;15:2. doi:10.1186/s12938-015-0120-7
19. Michael F, McNitt-Gray SGAI, Charles R, et al. The Lung Image Database Consortium (LIDC) data collection process for nodule detection and annotation. Acad Radiol. 2007;14:1464–1474. doi:10.1016/j.acra.2007.07.021
20. Jacobs C, van Rikxoort EM, Murphy K, Prokop M, Schaefer-Prokop CM, van Ginneken B. Computer-aided detection of pulmonary nodules: a comparative study using the public LIDC/IDRI database. Eur Radiol. 2016;26(7):2139–2147. doi:10.1007/s00330-015-4030-7
21. Gierada DS, Pinsky P, Nath H, Chiles C, Duan F, Aberle DR. Projected outcomes using different nodule sizes to define a positive CT lung cancer screening examination. J Natl Cancer Inst. 2014;106(11). doi:10.1093/jnci/dju061
22. Heuvelmans MA, Walter JE, Peters RB, et al. Relationship between nodule count and lung cancer probability in baseline CT lung cancer screening: the NELSON study. Lung Cancer. 2017;113:45–50. doi:10.1016/j.lungcan.2017.08.023
23. Chen LY, Molina-Vila MA, Ruan SY, et al. Coexistence of EGFR T790M mutation and common activating mutations in pretreatment non-small cell lung cancer: a systematic review and meta-analysis. Lung Cancer. 2016;94:46–53. doi:10.1016/j.lungcan.2016.01.019
24. Lee Y, Lee GK, Hwang JA, Yun T, Kim HT, Lee JS. Clinical likelihood of sporadic primary EGFR T790M mutation in EGFR-mutant lung cancer. Clin Lung Cancer. 2015;16(1):46–50. doi:10.1016/j.cllc.2014.09.002
25. Lee Y, Lee GK, Lee YS, et al. Clinical outcome according to the level of preexisting epidermal growth factor receptor T790M mutation in patients with lung cancer harboring sensitive epidermal growth factor receptor mutations. Cancer. 2014;120(14):2090–2098. doi:10.1002/cncr.28711
26. Costa C, Molina MA, Drozdowskyj A, et al. The impact of EGFR T790M mutations and BIM mRNA expression on outcome in patients with EGFR-mutant NSCLC treated with erlotinib or chemotherapy in the randomized phase III EURTAC trial. Clin Cancer Res. 2014;20(7):2001–2010. doi:10.1158/1078-0432.CCR-13-2233
27. Su KY, Chen HY, Li KC, et al. Pretreatment epidermal growth factor receptor (EGFR) T790M mutation predicts shorter EGFR tyrosine kinase inhibitor response duration in patients with non-small-cell lung cancer. J Clin Oncol. 2012;30(4):433–440. doi:10.1200/JCO.2011.38.3224
28. Fujita Y, Suda K, Fau-Kimura H, et al. Highly sensitive detection of EGFR T790M mutation using colony hybridization predicts favorable prognosis of patients with lung cancer harboring activating EGFR mutation. J Thorac Oncol. 2012;7(1556–1380(Electronic)):1640–1644. doi:10.1097/JTO.0b013e3182653d7f
29. Karachaliou N, Costa C, Gimenez-Capitan A, et al. BRCA1, LMO4, and CtIP mRNA expression in erlotinib-treated non-small-cell lung cancer patients with EGFR mutations. J Thorac Oncol. 2013;8(3):295–300. doi:10.1097/JTO.0b013e31827db621
30. Zhao J, Feng H-H, Zhao J-Y, et al. A sensitive and practical method to detect the T790M mutation in the epidermal growth factor receptor. Oncol Lett. 2016;11(4):2573–2579. doi:10.3892/ol.2016.4263
31. Wu Y-L, Zhou C, Hu C-P, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(2):213–222. doi:10.1016/S1470-2045(13)70604-1
32. Attili I, Karachaliou N, Conte P, Bonanno L, Rosell R. Therapeutic approaches for T790M mutation positive non-small-cell lung cancer. Expert Rev Anticancer Ther. 2018;18(10):1021–1030. doi:10.1080/14737140.2018.1508347
33. Jang J, Son JB, To C, et al. Discovery of a potent dual ALK and EGFR T790M inhibitor. Eur J Med Chem. 2017;136(1768):497–510. doi:10.1016/j.ejmech.2017.04.079
34. Oh JE, An CH, Yoo NJ, Lee SH. Detection of low-level EGFR T790M mutation in lung cancer tissues. Acta Pathol Microbiol Imm Scand. 2011;119(7):403–411. doi:10.1111/j.1600-0463.2011.02738.x
35. Rosell R, Moran T, Queralt C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med. 2009;361:958–967. doi:10.1056/NEJMoa0904554
36. Ciardiello F, Tortora G. EGFR antagonists in cancer treatment. N Engl J Med. 2008;358(11):1160–1174. doi:10.1056/NEJMra0707704
37. Togashi Y, Hayashi H, Terashima M, et al. Inhibition of beta-Catenin enhances the anticancer effect of irreversible EGFR-TKI in EGFR-mutated non-small-cell lung cancer with a T790M mutation. J Thorac Oncol. 2015;10(1):93–101. doi:10.1097/JTO.0000000000000353
38. Watanabe S, Yoshida T, Kawakami H, et al. T790M-selective EGFR-TKI combined with dasatinib as an optimal strategy for overcoming EGFR-TKI resistance in T790M-positive non-small cell lung cancer. Mol Cancer Ther. 2017;16(1538–8514 (Electronic)):2563–2571. doi:10.1158/1535-7163.MCT-17-0351
39. Karachaliou N, Gimenez-Capitan A, Drozdowskyj A, et al. ROR1 as a novel therapeutic target for EGFR-mutant non-small-cell lung cancer patients with the EGFR T790M mutation. Transl Lung Cancer Res. 2014;3(2218–6751 (Print)):122–130. doi:10.3978/j.issn.2218-6751.2014.03.02
40. Furugaki K, Fukumura J, Iwai T, et al. Impact of bevacizumab in combination with erlotinib on EGFR-mutated non-small cell lung cancer xenograft models with T790M mutation or MET amplification. Int J Cancer. 2016;138(4):1024–1032. doi:10.1002/ijc.29848
41. Remon J, Menis J, Hasan B, et al. The APPLE trial: feasibility and activity of AZD9291 (Osimertinib) treatment on positive plasma T790M in EGFR-mutant NSCLC patients. EORTC 1613. (1938-0690 (Electronic)).
42. Santarpia M, Liguori A, Karachaliou N, et al. Osimertinib in the treatment of non-small-cell lung cancer: design, development and place in therapy. Lung Cancer. 2017;8(1179):109–125. doi:10.2147/LCTT.S119644
43. Tan DS-W, Yang JC-H, Leighl NB, et al. Updated results of a phase 1 study of EGF816, a third-generation, mutant-selective EGFR tyrosine kinase inhibitor (TKI), in advanced non-small cell lung cancer (NSCLC) harboring T790M. J Clin Oncol. 2016;34(15_suppl):9044. doi:10.1200/JCO.2016.34.15_suppl.9044
44. Park K, Lee JS, Han JY, et al. 1300: efficacy and safety of BI 1482694 (HM61713), an EGFR mutant-specific inhibitor, in T790M-positive NSCLC at the recommended phase II dose. J Thor. 2016;11(4):S113. doi:10.1016/S1556-0864(16)30243-X
45. Hashida S, Soh J, Toyooka S, et al. Presence of the minor EGFR T790M mutation is associated with drug-sensitive EGFR mutations in lung adenocarcinoma patients. Oncol Rep. 2014;32(1791–2431 (Electronic)):145–152. doi:10.3892/or.2014.3197
46. Yang JC, Sequist LV, Geater SL, et al. Clinical activity of afatinib in patients with advanced non-small-cell lung cancer harbouring uncommon EGFR mutations: a combined post-hoc analysis of LUX-Lung 2, LUX-Lung 3, and LUX-Lung 6. Lancet Oncol. 2015;16(7):830–838. doi:10.1016/S1470-2045(15)00026-1
47. Li W, Qiu T, Guo L, et al. Primary and acquired EGFR T790M-mutant NSCLC patients identified by routine mutation testing show different characteristics but may both respond to osimertinib treatment. Cancer Lett. 2018;423(1872):9–15. doi:10.1016/j.canlet.2018.03.005
48. Wang S, Yan B, Zhang Y, et al. Different characteristics and survival in non-small cell lung cancer patients with primary and acquired EGFR T790M mutation. Int J Cancer. 2018;144:2880–2886.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



