Back to Journals » International Journal of General Medicine » Volume 16
Plecanatide Improves Symptoms of Irritable Bowel Syndrome with Constipation: Results of an Integrated Efficacy and Safety Analysis of Two Phase 3 Trials
Authors Brenner DM, Dorn SD, Fogel RP, Christie J, Laitman AP, Rosenberg J
Received 21 March 2023
Accepted for publication 7 August 2023
Published 25 August 2023 Volume 2023:16 Pages 3769—3777
DOI https://doi.org/10.2147/IJGM.S400431
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Hossam El-Din Shaaban
Darren M Brenner,1 Spencer D Dorn,2 Ronald P Fogel,3 Jennifer Christie,4 Adam P Laitman,5 Jonathan Rosenberg6
1Internal Medicine-Gastroenterology, Northwestern University-Feinberg School of Medicine, Chicago, IL, USA; 2Division of Gastroenterology and Hepatology, UNC School of Medicine, Chapel Hill, NC, USA; 3Digestive Health Center of Michigan, Chesterfield, MI, USA; 4Emory University School of Medicine, Atlanta, GA, USA; 5Salix Pharmaceuticals, Bridgewater, NJ, USA; 6GI Alliance of Illinois, Gurnee, IL, USA
Correspondence: Darren M Brenner, MD, FACG, AGAF, RFF, Northwestern Memorial Hospital/Arkes Family Pavilion, 676 N St Clair Street, Suite 1400, Chicago, IL, 60611, USA, Tel +1 312 695 8132, Fax +1 312 695 3999, Email [email protected]
Purpose: Patients with irritable bowel syndrome with constipation (IBS-C) experience abdominal pain with altered bowel movements. Plecanatide is indicated as IBS-C treatment in adults. This integrated analysis further characterizes plecanatide efficacy and safety in IBS-C.
Patients and Methods: Data pooled from 2 identically designed phase 3 trials included adults with IBS-C randomized to plecanatide 3 mg or 6 mg, or placebo once daily for 12 weeks. A daily diary recorded stool frequency/symptoms, with abdominal pain, bloating, cramping, discomfort, fullness, and straining intensity individually rated. Overall response (primary endpoint) was defined as ≥ 30% improvement from baseline in average worst abdominal pain severity and increase of ≥ 1 complete spontaneous bowel movement, during same week (composite), for ≥ 6 of 12 weeks. Secondary endpoints included sustained response (overall response, plus meeting weekly composite criteria during ≥ 2 of last 4 treatment weeks) and changes from baseline in individual symptoms. Safety assessments included adverse event monitoring.
Results: Overall, 2176 patients (74.0% female; mean [SD] age, 43.5 [14.1] years) were included in efficacy analyses (plecanatide 3 mg [n = 724], 6 mg [n = 723], placebo [n = 729]). A significantly greater percentage of patients achieved overall response with plecanatide 3 mg (25.6%) and 6 mg (26.7%) versus placebo (16.0%; both P < 0.001 vs placebo). A significantly greater percentage of patients were sustained responders with plecanatide 3 mg (24.3%) and 6 mg (25.6%) versus placebo (15.6%; both P < 0.001 vs placebo). Significant improvements from baseline in abdominal discomfort, abdominal fullness, abdominal pain, bloating, and cramping occurred as early as Week 1 (Week 2 for abdominal pain) with plecanatide and were maintained through Week 12 versus placebo. Diarrhea, the most common adverse event, occurred in 4.3% (3 mg), 4.0% (6 mg) and 1.0% (placebo) of patients, leading to study discontinuation in 1.2%, 1.4%, and 0 patients, respectively.
Conclusion: Plecanatide is safe and effective for treating global and individual IBS-C symptoms.
Keywords: abdominal pain, bloating, functional GI disorders, guanylate cyclase-C agonist, irritable bowel syndrome
Introduction
Irritable bowel syndrome (IBS) with constipation (IBS-C) is a prevalent disorder of gut–brain interaction characterized by recurrent abdominal pain associated with hard and/or infrequent bowel movements.1 Patients with IBS-C report that abdominal pain is bothersome and interferes with daily activities to a greater degree than for patients with other IBS subtypes.2 Furthermore, patients with IBS-C typically experience additional symptoms, including bloating, abdominal distension, and straining, which can be a challenge for health care providers to manage.1,3,4 Patients with IBS-C have reported impaired quality of life, reduced work productivity, and increased direct and indirect health care expenditures.5–8 Although prescription and over-the-counter treatments are available for the wide-ranging abdominal and bowel symptoms, including symptom intensity experienced by patients with IBS-C, approximately one-third of patients or less report utilizing these therapies.3,4,9
Plecanatide 3-mg tablet is a guanylate cyclase-C agonist approved for the treatment of adults with IBS-C or chronic idiopathic constipation.10 The efficacy and safety of plecanatide for the treatment of IBS-C in adults were demonstrated in two identical, randomized, double-blind, placebo-controlled, phase 3 clinical trials that showed overall response, abdominal, and bowel symptoms were significantly improved with plecanatide versus placebo.11 Patients also reported significantly greater treatment satisfaction with plecanatide compared with placebo.11 The aim of this integrated efficacy and safety analysis was to further examine the efficacy and safety of 2 dosages of plecanatide for the treatment of patients with IBS-C.
Materials and Methods
Patients and Study Design
Data were pooled from 2 identically designed, randomized, double-blind, placebo-controlled phase 3 clinical trials (ClinicalTrials.gov identifiers NCT02387359 and NCT02493452).11 Both the patient populations and study designs have been described previously.11 Briefly, adults aged 18 to 85 years with IBS-C (Rome III criteria) and body mass index of 18 to 40 kg/m2 were randomly assigned (1:1:1 allocation) to once-daily oral treatment with plecanatide 3 mg, plecanatide 6 mg, or placebo for 12 weeks. For patients who did not have a bowel movement for ≥72 hours, administration of bisacodyl 5 mg tablets, per prescribing information, was permitted as a laxative (rescue medication) for a maximum of 2 days in a given week.
The study protocols were approved by the institutional review boards (IRBs)/ethics committees of the participating centers and a central IRB (Schulman IRB, Cincinnati, OH). The trials were conducted in accordance with the International Conference for Harmonisation guidance for Good Clinical Practice and the ethical principles of the Declaration of Helsinki. All participants provided written informed consent prior to admission in the trials. As the data presented herein are from a pooled analysis of deidentified data previously collected under the original trial approvals, additional IRB approval was not obtained.
Assessments
Bowel movement frequency, completeness, and symptom intensity were recorded via a daily electronic diary. Abdominal pain, abdominal discomfort, abdominal fullness, bloating, cramping, and straining were individually rated daily using an 11-point scale (range, 0 [“no or none”] to 10 [“worst possible”]). A patient global assessment of abdominal pain, IBS symptoms, and IBS disease severity was also recorded at baseline and Week 12. These were determined by the following questions: “How would you rate your abdominal pain overall over the past 7 days?” (5-point scale of 2 [“significantly relieved”], 1 [“moderately relieved”], 0 [“unchanged”], −1 [“moderately worse”], −2 [“significantly worse”]); “How would you rate your IBS signs and symptoms overall over the past 7 days?” (5-point scale of 2 [“significantly relieved”], 1 [“moderately relieved”], 0 [“unchanged”], −1 [“moderately worse”], −2 [“significantly worse”]); and “How would you rate the severity of your IBS symptoms at their worst over the past 7 days?” (5-point scale of 1 [“none”], 2 [“mild”], 3 [“moderate”], 4 [“severe”], 5 [“very severe”]).
The primary efficacy endpoint for both trials was the percentage of patients with an overall response, defined as a composite of abdominal pain response (≥30% improvement from baseline in average worst abdominal pain severity) and stool frequency response (increase from baseline of ≥1 complete spontaneous bowel movement [CSBM]), during the same week, for ≥6 of 12 treatment weeks. A key secondary efficacy endpoint was the percentage of patients with sustained response (overall response, plus meeting weekly composite criteria during ≥2 of last 4 treatment weeks). Additional secondary efficacy endpoints included changes from baseline in abdominal pain, abdominal discomfort, abdominal fullness, bloating, and cramping during the overall 12-week treatment period, and by week. The mean change from baseline in spontaneous bowel movements (SBMs) and CSBMs was also determined. Safety assessments included monitoring the incidence and severity of adverse events (AEs) and changes in vital signs and clinical laboratory tests.
Statistical Analyses
Efficacy analyses were conducted in the intent-to-treat (ITT) population, which included all nonduplicative randomized patients who received ≥1 dose of study drug, and the safety population, which included all patients who received ≥1 dose of study drug (included duplicative patients who participated at ≥1 site or trial [n = 13]). P values for response rate comparisons were determined using the Cochran-Mantel-Haenszel test, stratified by gender. P values were calculated for least-squares mean (LSM) data using a linear mixed-effects model with fixed effects for gender (stratification variable), treatment, week, interaction of treatment and week, the corresponding baseline value, and a random intercept for patient, with the model taking into account repeated measurements for each patient. Safety was reported using descriptive statistics.
Results
A total of 2176 nonduplicative patients with IBS-C were included in the ITT population (plecanatide 3 mg [n = 724], plecanatide 6 mg [n = 723], and placebo [n = 729]), and 2182 patients were included in the safety population (including duplicative patients participating at ≥1 site or trial; plecanatide 3 mg [n = 726], plecanatide 6 mg [n = 726], and placebo [n = 730]). Baseline demographic and disease characteristics in the ITT population were similar among treatment groups (Table 1). Overall, approximately three-quarters of patients were female and white, and the mean age was 43.5 years. Mean baseline abdominal symptom scores were approximately 6.5 (Table 1), indicating moderate symptom intensity. A total of 1857 (85.3%) patients in the ITT population completed the trials.
 |
Table 1 Baseline Demographic and Disease Characteristics |
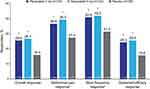
The percentage of overall responders (primary efficacy endpoint) was significantly greater with plecanatide 3 mg (25.6%) and plecanatide 6 mg (26.7%) compared with placebo (16.0%; P < 0.001 vs placebo for both Figure 1). For the individual components of overall response, a significantly greater percentage of patients treated with plecanatide 3 mg or 6 mg were abdominal pain and stool frequency responders for ≥6 of 12 treatment weeks compared with placebo (P < 0.001 vs placebo, all comparisons; Figure 1). Furthermore, a significantly greater percentage of patients in the plecanatide dose groups were sustained responders compared with placebo (P < 0.001 vs placebo for both Figure 1). Individual abdominal symptoms assessed by week showed significant differences in LSM change from baseline versus placebo for both plecanatide doses starting at Week 2 for abdominal pain (Figure 2A) and Week 1 for abdominal discomfort (Figure 2B), abdominal fullness (Figure 2C), bloating (Figure 2D), and cramping (Figure 2E) up to Week 12 (end of treatment period). As expected, improvements started to decline during the 2-week posttreatment period; however, differences favoring plecanatide (either or both doses) versus placebo were observed for most abdominal symptoms (Figures 2A–E).
Across the 12-week treatment period, significant improvements from baseline with plecanatide 3 mg and 6 mg were observed for bowel movement frequency, as well as SBMs/week and CSBMs/week (P < 0.001 vs placebo, all comparisons Table 2). Furthermore, LSM changes from baseline in patient global ratings of abdominal pain, IBS symptoms, and IBS disease severity were superior for both plecanatide doses versus placebo across the 12-week treatment period (P < 0.001 vs placebo, all comparisons Table 2).
 |
Table 2 Secondary Efficacy Outcomes Across 12 Weeks of Treatment |
Plecanatide 3 mg and 6 mg were generally well tolerated (Table 3). The most common reasons for discontinuation in the safety population (n = 2182) were withdrawal of consent (5.5%), loss to follow-up (3.6%), and ≥1 AE (1.6%). The most commonly reported AE with plecanatide treatment was diarrhea, occurring in 4.3% of patients treated with plecanatide 3 mg, and 4.0% of patients treated with plecanatide 6 mg, compared with 1.0% of patients treated with placebo (Table 3). Serious AEs were comparable among the 3 groups, occurring in 0.8% and 0.7% of patients receiving plecanatide 3 mg and 6 mg, respectively, and 0.8% of patients receiving placebo. The percentage of patients with an AE leading to treatment discontinuation was greater with plecanatide 3 mg and 6 mg than with placebo (2.5% and 2.2%, vs 0.4%), with discontinuation from the study due to the AE of diarrhea reported in 1.2%, 1.4%, and 0 patients, respectively.
 |
Table 3 Adverse Events (Safety Population) |
Discussion
Irritable bowel syndrome with constipation is characterized by recurrent abdominal pain with hard and/or infrequent bowel movements.1 Over 90% of patients with constipation utilize only over-the-counter agents to treat their constipation, and approximately two-thirds have never discussed their constipation with a health care provider.12 When patients seek health care for constipation, over-the-counter agents, exercise, and dietary changes are frequently recommended by providers for managing symptoms.13 However, it is important to note that the American College of Gastroenterology guideline for management of IBS recommends against the use of polyethylene glycol, which is approved by the US Food and Drug Administration (FDA) for constipation, given that clinical trials have demonstrated efficacy for bowel, but not sensory, symptoms in patients with IBS-C.14–16 Indeed, patients with IBS-C typically experience other abdominal symptoms in addition to abdominal pain and decreased stool frequency, and the level of intensity that patients experience with these symptoms varies.1,3,4 One such symptom is bloating, which has been reported to be more severe in patients with IBS with abdominal pain/discomfort versus patients without abdominal pain/discomfort.17 Thus, the rate of improvement in other IBS-C symptoms, timing for when the improvement may occur, and persistence of response are important considerations for patients and health care providers when choosing amongst therapies. Both plecanatide doses resulted in significant reductions in bloating, abdominal discomfort, abdominal fullness, and cramping by the end of Week 1 of treatment and in abdominal pain by Week 2; these findings had not been reported previously. Furthermore, significant increases in frequency of complete bowel movements were identified beginning at Week 1 compared with placebo, and this was maintained throughout all 12 weeks of treatment. These new results support symptom improvements beyond bowel movement frequency, and they provide valuable insight into how quickly patients with IBS-C may experience these benefits with plecanatide. These results also provide a better understanding of the overall patient experience with treatment (not previously reported), as patient global ratings of abdominal pain, IBS symptoms and IBS disease severity were improved with plecanatide compared with placebo. Plecanatide also exhibited a favorable safety profile with the most common AE of diarrhea, which occurred in a small percentage of patients in both plecanatide treatment groups (~4%). This is an important finding given that, in a survey of adults with IBS-C (n = 1311), 23% of patients reported diarrhea as the reason for being dissatisfied with treatment, and 41% of providers cited treatment-related diarrhea as a challenge for managing this patient population.13
The findings of these efficacy and safety analyses expand on previously reported trial data of plecanatide for the treatment of IBS-C,11 including characterization of weekly response to treatment. The current FDA-recommended dosage is plecanatide 3 mg once daily for the treatment of IBS-C.
Strengths of this integrated analysis include the large population of adults with IBS-C who were examined and the more extensive analysis of individual endpoints representing symptoms commonly experienced by patients with IBS-C. Limitations include the duration of treatment (12 weeks) and limited follow-up (2 weeks posttreatment). This minimized ability to interpret the duration of individual abdominal symptom benefits with plecanatide >2 weeks after treatment discontinuation, although it is not expected that this minimally absorbed therapeutic would continue to provide symptom benefits upon discontinuation. Although these analyses did not focus on specific subgroups of patients with IBS-C and/or patterns of response (eg, time to decrease of severity of specific symptoms, patients most/least likely to be responders for specific symptoms), the findings of these pooled analyses provide further, and more comprehensive, support for plecanatide being efficacious and safe in the treatment of the wide range of abdominal and bowel symptoms that patients with IBS-C may experience.
Conclusion
Plecanatide is safe and effective for the treatment of global and individual symptoms in adults with IBS-C.
Data Sharing Statement
Qualified researchers interested in obtaining access to trial data should submit a detailed research proposal and data access request to [email protected]. For more information, please see https://www.bauschhealth.com/ESG/access-to-clinical-study-data.
Ethical Considerations
The study protocols were approved by the institutional review boards/ethics committees of the participating centers and a central institutional review board (Schulman IRB, Cincinnati, OH). The trials were conducted in accordance with the International Conference for Harmonisation guidance for Good Clinical Practice and the ethical principles of the Declaration of Helsinki. All participants provided written informed consent prior to admission in the trials. As the data presented herein are from a pooled analysis of de-identified data previously collected under the original trial approvals, additional IRB approval was not obtained.
Acknowledgments
Technical editorial and medical writing assistance was provided, under direction of the authors, by Mary Beth Moncrief, PhD, and Sophie Bolick, PhD, Synchrony Medical Communications LLC, West Chester, PA. Funding for this assistance was provided by Salix Pharmaceuticals, Bridgewater, NJ.
Funding
The trials were supported by Synergy Pharmaceuticals, and the current analyses were supported by Salix Pharmaceuticals.
Disclosure
Darren M. Brenner is a consultant and speaker for Salix Pharmaceuticals and is supported in research by an unrestricted gift from the IDP Foundation. Jennifer Christie reports being an advisory board member for Evoke Pharma, Takeda Pharmaceuticals, USA, Inc., and Grail, LLC, as well as grants from Syneos Pharmaceuticals. Adam P. Laitman is an employee of Salix Pharmaceuticals. Jonathan Rosenberg reports serving on speakers bureaus for AbbVie (Allergan), Salix Pharmaceuticals, and Takeda Pharmaceuticals USA, Inc. The authors report no other conflicts of interest in this work.
References
1. Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150(6):1393–1407. doi:10.1053/j.gastro.2016.02.031
2. Shah ED, Almario CV, Spiegel BM, Chey WD. Presentation and characteristics of abdominal pain vary by irritable bowel syndrome subtype: results of a nationwide population-based study. Am J Gastroenterol. 2020;115(2):294–301. doi:10.14309/ajg.0000000000000502
3. Lacy BE, Cangemi D, Vazquez-Roque M. Management of chronic abdominal distension and bloating. Clin Gastroenterol Hepatol. 2021;19(2):219–231. doi:10.1016/j.cgh.2020.03.056
4. Taylor DCA, Abel JL, Martin C, et al. Comprehensive assessment of patients with irritable bowel syndrome with constipation and chronic idiopathic constipation using deterministically linked administrative claims and patient-reported data: the Chronic Constipation and IBS-C Treatment and Outcomes Real-World Research Platform (CONTOR). J Med Econ. 2020;23(10):1072–1083. doi:10.1080/13696998.2020.1799816
5. Ballou S, McMahon C, Lee HN, et al. Effects of irritable bowel syndrome on daily activities vary among subtypes based on results from the IBS in America survey. Clin Gastroenterol Hepatol. 2019;17(12):2471–2478. doi:10.1016/j.cgh.2019.08.016
6. Paré P, Gray J, Lam S, et al. Health-related quality of life, work productivity, and health care resource utilization of subjects with irritable bowel syndrome: baseline results from LOGIC (Longitudinal Outcomes Study of Gastrointestinal Symptoms in Canada), a naturalistic study. Clin Ther. 2006;28(10):1726–1735. doi:10.1016/j.clinthera.2006.10.010
7. Doshi JA, Cai Q, Buono JL, et al. Economic burden of irritable bowel syndrome with constipation: a retrospective analysis of health care costs in a commercially insured population. J Manag Care Pharm. 2014;20(4):382–390. doi:10.18553/jmcp.2014.20.4.382
8. Nellesen D, Yee K, Chawla A, Edelman Lewis B, Carson RT. A systematic review of the economic and humanistic burden of illness in irritable bowel syndrome and chronic constipation. J Manage Care Pharm. 2013;19(9):755–764. doi:10.18553/jmcp.2013.19.9.755
9. Brenner DM, Lacy BE, Ford AC, et al. Linaclotide reduced response time for irritable bowel syndrome with constipation symptoms: analysis of 4 randomized controlled trials. Am J Gastroenterol. 2023;118(5):872–879. doi:10.14309/ajg.0000000000002064
10. Salix Pharmaceuticals. Trulance tablets, for oral use [package insert]. Salix Pharmaceuticals, Bridgewater, NJ; 2021.
11. Brenner DM, Fogel R, Dorn SD, et al. Efficacy, safety, and tolerability of plecanatide in patients with irritable bowel syndrome with constipation: results of two phase 3 randomized clinical trials. Am J Gastroenterol. 2018;113(5):735–745. doi:10.1038/s41395-018-0026-7
12. Oh SJ, Fuller G, Patel D, et al. Chronic constipation in the United States: results from a population-based survey assessing healthcare seeking and use of pharmacotherapy. Am J Gastroenterol. 2020;115(6):895–905. doi:10.14309/ajg.0000000000000614
13. Quigley EMM, Horn J, Kissous-Hunt M, Crozier RA, Harris LA. Better understanding and recognition of the disconnects, experiences, and needs of patients with irritable bowel syndrome with constipation (BURDEN IBS-C) study: results of an online questionnaire. Adv Ther. 2018;35(7):967–980. doi:10.1007/s12325-018-0733-x
14. Lacy BE, Pimentel M, Brenner DM, et al. ACG clinical guideline: management of irritable bowel syndrome. Am J Gastroenterol. 2021;116(1):17–44. doi:10.14309/ajg.0000000000001036
15. Awad RA, Camacho S. A randomized, double-blind, placebo-controlled trial of polyethylene glycol effects on fasting and postprandial rectal sensitivity and symptoms in hypersensitive constipation-predominant irritable bowel syndrome. Colorectal Dis. 2010;12(11):1131–1138. doi:10.1111/j.1463-1318.2009.01990.x
16. Chapman RW, Stanghellini V, Geraint M, Halphen M. Randomized clinical trial: macrogol/PEG 3350 plus electrolytes for treatment of patients with constipation associated with irritable bowel syndrome. Am J Gastroenterol. 2013;108(9):1508–1515. doi:10.1038/ajg.2013.197
17. Oh JE, Chey WD, Spiegel B. Abdominal bloating in the US: results of a survey of 88,795 Americans examining prevalence and healthcare seeking. Clin Gastroenterol Hepatol. 2022;21:2370–2377. doi:10.1016/j.cgh.2022.10.031
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.