Back to Journals » Infection and Drug Resistance » Volume 16
Platelet-to-White Blood Cell Ratio as a Predictor of Mortality in Patients with Severe COVID-19 Pneumonia: A Retrospective Cohort Study
Authors Thungthienthong M, Vattanavanit V
Received 28 November 2022
Accepted for publication 18 January 2023
Published 24 January 2023 Volume 2023:16 Pages 445—455
DOI https://doi.org/10.2147/IDR.S398731
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Metus Thungthienthong,1 Veerapong Vattanavanit2
1Division of Internal Medicine, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand; 2Critical Care Medicine Unit, Division of Internal Medicine, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand
Correspondence: Veerapong Vattanavanit, Critical Care Medicine Unit, Division of Internal Medicine, Faculty of Medicine, Prince of Songkla University, 15 Kanjanavanich Road, Hat Yai, Songkhla, 90110, Thailand, Tel +66848456228, Fax +6674429385, Email [email protected]
Purpose: Complete blood count (CBC) parameters are widely used as predictors of Coronavirus disease 2019 (COVID-19) severity. However, the clinical significance of these markers in severe COVID-19 pneumonia remains unclear. This study aimed to investigate the role of CBC parameters in predicting mortality in patients with severe COVID-19 pneumonia.
Patients and Methods: We conducted a retrospective study at a tertiary care center in southern Thailand. Between January 2020 and December 2021, adult patients who had been diagnosed with severe COVID-19 pneumonia were enrolled. Demographic and clinical data, including CBC data on admission, were analyzed and compared between survivors and non-survivors.
Results: A total of 215 patients with severe COVID-19 pneumonia were enrolled. The in-hospital mortality was 29.3%. Non-survivors had a significantly lower platelet-to-white blood cell ratio (PWR) than survivors (15.8 vs 29.0, p < 0.001). PWR had the best accuracy in predicting in-hospital mortality, with an area under the curve (AUC) of the receiver operating characteristic curve of 0.801, followed by the CURB-65 of 0.789.
Conclusion: PWR appears to be a simple independent predictor of mortality in patients with severe COVID-19 pneumonia.
Keywords: white blood cell, platelet, mortality, COVID-19, pneumonia
Plain Language Summary
Patients with severe COVID-19 pneumonia require intensive respiratory support and have higher mortality. Hence, determining the factors predicting the outcomes of these patients is essential. CBC parameters are being used as predictors of COVID-19 severity. Therefore, this study investigated the role of CBC parameters in predicting mortality in patients with severe COVID-19 pneumonia. In our study, PWR was found to be a simple independent predictor of mortality in patients with severe COVID-19 pneumonia, which will help in better management of these patients.
Introduction
The coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is spreading rapidly throughout the world.1,2 Although most infected patients are asymptomatic, in some cases, they can develop severe pneumonia requiring intensive respiratory support.3 One study in Thailand found that 51% of patients developed COVID-19 pneumonia and 27% developed severe pneumonia.4 The mortality rate of severe pneumonia is higher than that of the mild form.5–7 Early triage and appropriate prognostic predictors are crucial for the management of these patients.
In addition to the respiratory tract, COVID-19 affects other organ systems. The hematologic system usually changes during the COVID-19 infection. The virus affects the hematopoietic and/or coagulation systems, deranging the complete blood count (CBC) and coagulation test results.8
CBC is a simple marker used routinely in the diagnostic laboratory. Previous studies have attempted to determine CBC parameters for predicting COVID-19 severity and mortality.9 However, the clinical significance of these markers in severe COVID-19 remains unclear. Compared to patients with non-severe diseases and survivors, patients with severe and fatal diseases have considerably higher white blood cell (WBC) counts and lower lymphocyte and platelet counts.9 However, most studies were conducted in China, and limited data are available on severe pneumonia patients.8 This study aimed to investigate the role of WBC, platelet, and other complete blood count parameters in predicting mortality in patients with severe COVID-19 pneumonia.
Materials and Methods
Study Population and Design
A retrospective study was conducted in a tertiary university teaching hospital in Thailand. Between January 2020 and December 2021, we reviewed all patients with severe COVID-19 pneumonia who were hospitalized in the COVID-19 wards. Our COVID-19 wards contain 20 beds and involve full-time board-certified intensivists or pulmonologists. The study was approved by the Human Ethics Committee of the Faculty of Medicine, Prince of Songkla University (EC number: 64–544-14-1). Owing to the retrospective nature of the study the necessity for obtaining informed consent was waived.
The study included all patients over the age of 18 who had laboratory-confirmed SARS-CoV-2 infection and severe pneumonia during admission. Patients who had insufficient CBC count data or had any hematologic illnesses were not included in this study.
Data Collection
Clinical and epidemiological information on the patients was obtained from their medical records. Age, sex, body mass index, COVID-19 vaccination, comorbidities, illness severity score, risk scores including CURB-65, National Early Warning Score 2 (NEWS 2), COVID-GRAM, and 4C mortality score, respiratory support, diagnosis of acute respiratory distress syndrome (ARDS), CBC parameters at the time of admission, treatment, and in-hospital mortality were included in the data. CBC counts were estimated using an automated hematological analyzer (XT-1800i, Sysmex Corporation, Japan).
SARS-CoV-2 infection was confirmed using reverse-transcriptase polymerase chain reaction (RT-PCR). Samples were collected using combined nasopharyngeal swabs and analyzed in the central laboratory of our hospital.
Severe pneumonia was defined as the presence of clinical signs of pneumonia (fever, cough, and dyspnea) and signs of severe respiratory distress, defined as accessory muscle use, inability to complete full sentences while speaking due to shortness of breath, respiratory rate > 30 breaths per minute, or SpO2 < 90% on room air. Chest imaging (radiography, computed tomography [CT] scan, ultrasound) may assist in the diagnosis, identification, or exclusion of pulmonary complications.10
ARDS was identified according to the Berlin definition: onset within 1 week, bilateral lung opacities, no evidence of cardiac failure-related hydrostatic edema, and a PaO2/FiO2 ratio < 300 mmHg with positive end-expiratory pressure (PEEP) ≥ 5 cm H2O.11
Illness severity was assessed using the Acute Physiology and Chronic Health Evaluation II (APACHE II) variables.12 After 24 hours of hospital admission, the highest and lowest values for each of the APACHE II variables were recorded.
CURB-65 score comprises 5 variables; i) confusion, ii) a respiratory rate ≥ 30 breaths per minute, a iii) blood urea nitrogen level greater than 7 mmol/L, iv) a systolic blood pressure < 90 mm Hg or a diastolic blood pressure ≤ 60 mm Hg, and v) age ≥ 65 years.13
NEW 2 measured physiologic parameters at the hospital admission including respiratory rate, oxygen saturation, need for supplemental oxygen, body temperature, blood pressure, heart rate and level of consciousness.14
COVID-GRAM was calculated from 10 variables at the hospital admission including X-ray abnormality, age, hemoptysis, dyspnea, unconsciousness, number of comorbidities, cancer history, neutrophil-to-lymphocyte ratio, lactate dehydrogenase, and direct bilirubin.15
The 4C mortality score was calculated from 8 variables at the hospital admission including age, sex at birth, number of comorbidities, respiratory rate, peripheral oxygen saturation on room air, Glasgow coma scale score, urea, and C-reactive protein.16
The neutrophil count was divided by the lymphocyte count to get the neutrophil-to-lymphocyte ratio (NLR). By dividing the platelet count by the white blood cell count, the platelet-to-white blood ratio (PWR) was obtained.
Statistical Analyses
The optimum sample size for diagnostic research was calculated.17 According to our estimates, severe COVID-19 pneumonia has an in-hospital mortality rate of 30%, and a sample size of 88 would have 80% power to distinguish a difference of 10% from the assumed value of 80% for specificity with 95% confidence.
Using the Shapiro–Wilk test, the data were checked for normality. Percentages are used to convey categorical data. The median was used to summarize continuous data, along with the interquartile range (IQR). To compare continuous variables and proportions between groups, Mann–Whitney U-tests, Fisher’s exact probability tests, and Chi-square tests were applied, respectively.
After the variables’ associations with mortality were assessed using univariable logistic regression (p < 0.2), the variables were then included in a multivariable logistic regression model. Before modeling, the collinearity between variables was eliminated. To find significant independent variables impacting mortality, odds ratios (ORs) and 95% confidence intervals (CIs) were employed.
Receiver operating characteristic (ROC) analyses were performed to determine the predictive power of CBC parameters. The Youden test was performed to determine the optimal cutoff for predicting mortality. The cumulative survival was compared using the Kaplan–Meier survival analysis. Two-tailed P values less than 0.05 were regarded as statistically significant. STATA version 16 (StataCorp, College Station, TX, USA) was used to perform all statistical analyses.
Results
Baseline Characteristics
The study included 215 of the 466 patients who were admitted to the COVID cohort wards between January 2020 and December 2021. The patients were divided into two 2 groups: survivors and non-survivors. A total of 152 patients (70.7%) were survivors and 63 patients (29.3%) were non-survivors (Figure 1).
 |
Figure 1 Patient recruitment. Showing flow of patients within the study. |
The baseline characteristics are presented in Table 1. The non-survival group was older but had a lower BMI than the survival group. Our patients were vaccinated (15.9% in the non-survival group and 27% in the survival group). The non-survival group had a higher median severity score (APACHE II) than the survival group (22 vs 16, p < 0.001).
 |
Table 1 Baseline Characteristics of Survivors Vs Non-Survivors |
The incidence of ARDS was higher in the non-survival groups than that in the survival group (85.7% vs 44.1%, p < 0.001). They needed more mechanical ventilator support during hospitalization than the survival group (90.5% vs 44.1%, p < 0.001).
The non-survival group showed significantly higher total WBC and neutrophil counts, and significantly lower lymphocyte and platelet counts than the survival group at the time of admission. The NLR was significantly higher in the non-survival group than in the survival group (23.5 vs 9.4, p < 0.001), whereas the PWR was significantly lower in the non-survival group than in the survival group (15.8 vs 29.0, p < 0.001). The other baseline characteristics are shown in Supplementary File 1.
Association of CBC Parameters and in-Hospital Mortality
The relationship between the CBC and in-hospital mortality is presented in Table 2. Univariable logistic regression analysis showed that the variables WBC, neutrophil, platelet, and red blood cell counts, red cell distribution width (RDW), PWR, and NLR were associated with mortality. Next, the multivariable logistic regression adjusted for severity score (APACHE II) included all the aforementioned univariable analytic factors with statistical significance. Only WBC count, neutrophil count, platelet count, PWR, and NLR were significantly associated with in-hospital mortality.
 |
Table 2 Univariable and Multivariable Analyses for in-Hospital Mortality |
We examined the optimum cutoff values determined by ROC analysis with an area under the curve (AUC). The optimal cutoff values for PWR, NLR, neutrophil count, white blood cell count, platelet count, and risk scores including CURB-65, NEWS 2, COVID-GRAM, and 4C mortality score are shown in Table 3. Among these CBC parameters, PWR occupied the largest area with an AUC of 0.801, followed by the CURB-65 score with an AUC of 0.789, while the smallest area belonged to platelet count (AUC of 0.366). The ROC curve of PWR is shown in Figure 2, and a comparison of the ROC curves for four risk scores is shown in Figure 3.
 |
Table 3 Sensitivity and Specificity of Blood Markers by the Cutoff |
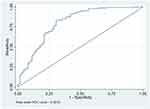 |
Figure 2 ROC curves for PWR. The area under the receiver operating characteristic curves to discriminate in-hospital mortality for PWR. |
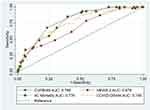 |
Figure 3 ROC curves for risk score comparisons. The area under the receiver operating characteristic curves for four risk scores: CURB-65, NEWS 2, COVID-GRAM, and the 4C mortality score. |
Additionally, the variation trend of the survival rate between the low PWR (< 20.34) and high PWR (≥ 20.34) groups was compared using the Kaplan–Meier survival analysis. The results showed a significant decline in the cumulative survival rate (p < 0.001) in those with low PWR (Figure 4).
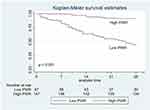 |
Figure 4 Survival analysis. Kaplan–Meier survival estimates, according to PWR. p values were calculated using the Log rank test. |
Discussion
This study investigated the prognostic value of the CBC parameters for in-hospital mortality in patients with severe COVID-19 pneumonia. Our results showed that WBC count, neutrophil count, platelet count, PWR, and NLR were significantly associated with in-hospital mortality. The PWR had the highest mortality predictor, followed by the CURB-65.
In patients with severe COVID-19 infection, leukocyte and neutrophil counts were considerably higher and gradually increased compared to those with non-severe infection.18,19 Higher total WBC counts were associated with mortality in COVID-19 as reported by Zhu et al20 Similar findings from our study indicated that increased neutrophils were the primary cause of the increase in WBCs since declining trends in lymphocyte numbers were observed. This activation mechanism can be explained by the hyperinflammatory state and cytokine storm.21 In addition to the bloodstream, the lung tissue has also been associated to an increase in neutrophils.22 The abnormal immune response of the lungs in patients with severe disease is a result of increased infiltration of immature neutrophils.
Lymphopenia was observed in patients with severe COVID-19. Terpos et al discovered that lymphopenia was higher in severe COVID-19.8 Moreover, the same result was reported in a meta-analysis by Danwang et al23 According to a meta-analysis of lymphocyte counts in COVID-19, patients with severe disease had a considerable decrease in the number of CD4+ T cells, CD8+ T cells, B cells, natural killer cells, and total lymphocytes compared to those with mild disease.24 The virus may directly infect lymphocytes or it may do so indirectly through inflammatory cytokines that cause lymphocyte apoptosis or suppress lymphocyte proliferation.8,21
Thrombocytopenia is associated with the development of severe disease and mortality in COVID-19 patients. Our study showed a lower platelet count in non-survivors and associated mortality. The mechanisms of thrombocytopenia in severe COVID-19 are attributed to infected bone marrow, suppression of bone marrow function by hyperinflammation, and increased platelet activation and subsequent consumption due to tissue damage.21 Liu et al reported that patients who had thrombocytopenia at admission were associated with mortality three times higher than those without thrombocytopenia.25 A meta-analysis by Danwang et al also found that severe COVID-19 patients had lower platelet counts.23
Systemic inflammatory markers represented as hematological ratios, such as NLR, PWR, and lymphocyte-to-monocyte ratio, were previously investigated as possible indicators of COVID-19 severity. In a study by Aly et al NLR had the highest severity predictor (AUC 0.838, sensitivity 71.38%, specificity 87.03%) with a cutoff value of 3.5 to predict severity in COVID-19.26 Kilercik et al revealed that NLR > 4.4 had the most predictive ability for COVID-19 severity (AUC 0.776, 95% CI: 0.744–0.807).27 NLR was also the best prognostic tool for predicting the progressive severity of COVID-19, as reported by Liu et al28 and Lian et al29 It is crucial to emphasize that the majority of research on NLR is retrospective. In prospective research published by Yildiz et al, an NLR value of 5.94 accurately predicted in-hospital mortality in patients hospitalized with COVID-19 pneumonia (AUC 0.665, sensitivity 62%, specificity 64%).30 When compared with other risk scores such as CURB-65, COVID-GRAM, NEWS 2, and 4C mortality score, the best predictor of mortality was the 4C mortality score (AUC 0.80), followed by the NLR on admission (AUC 0.76).31
In contrast, our results revealed that PWR was a better predictor of mortality than NLR. WBC and platelet counts independently predicted mortality. Therefore, the combined hematological ratio resulted in greater performance in mortality prediction. In our cohort, all patients were diagnosed with severe pneumonia. Previous studies revealed that patients with severe COVID-19 infection and hypoxemia were more likely to have thrombocytopenia25 and leukocytosis.20 Therefore, a lower PWR was associated with higher mortality. In our results, NLR showed lower predictor performance than WPR. The dynamic changes of neutrophils and lymphocytes were dependent on disease stages and severity.32,33 The single measurement NLR at the emergency department did not independently associate with COVID-19 mortality in a previous study, but the delta NLR did.34 The utility of PWR was proposed under other conditions. Weng et al found that a PWR of < 20 is a reliable marker of infection on postoperative splenectomy day 5.35 In patients with HBV-associated decompensated cirrhosis, Zhang et al demonstrated that a low PWR may be a predictor of a poor prognosis.36
Besides PWR, CURB-65 was a good mortality predictor in our cohort. CURB-65 is a simple tool comprising 4 clinical parameters and only 1 laboratory parameter, which originated from a community-acquired pneumonia study. CURB-65 served as a useful COVID-19 mortality predictor in previous studies.37,38 Bradley et al38 reported that CURB-65 could predict in-hospital death in COVID-19 pneumonia patients with an AUC of 0.79, which was the same as our results (AUC of 0.789). Other risk scores showed fair mortality predictor performance in our cohort since it originated from a heterogeneous population. COVID-GRAM was developed to predict the occurrence of critical illness in hospitalized COVID patients with mild severity.15 The 4C mortality score was developed from COVID-19 UK patients admitted to the hospital at least 4 weeks before final data extraction.16 The NEWS 2 score was generated as an early warning score in non-COVID patients. The mortality in COVID-GRAM and 4C mortality score cohorts was 3.2% and 32.2%, respectively.
To the best of our knowledge, this is the first study to report the prognostic value of the PWR in severe COVID-19 pneumonia patients. This new hematological ratio may provide valuable information for assessing disease severity. More intensive care should be considered in patients with a high PWR. To validate these results, further studies are required.
Our study has several limitations. Firstly, the patients were retrospectively enrolled from a single center; therefore, selection bias may exist. Secondly, we did not evaluate all confounders that might affect hematologic parameters and in-hospital mortality. Although we excluded patients with hematologic malignancies, we did not consider all potential factors that influence platelet and white blood cell counts, such as medication, renal function and liver function. We attempted to document possible treatment effects on mortality; however, some interventions such as nutrition therapy and uncontrolled antibiotics usage between groups or unmeasured covariates may serve as potential confounding factors. Thirdly, we focused on CBC at admission, and the dynamic changes in CBC during treatment were not estimated. There was considerable heterogeneity in the time of blood sample collection, even though it was performed as soon as patients were admitted to COVID wards.
Conclusion
PWR may serve as a simple, independent predictor of mortality in patients with severe COVID-19 pneumonia. PWR can promote the identification of patients who need critical care during admission. Thus, our study will contribute to improving patient management for those who have severe COVID-19 pneumonia.
Abbreviations
Complete blood count (CBC), coronavirus disease 2019 (COVID-19), platelet-to-white blood cell ratio (PWR), area under the curve (AUC), severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), white blood cell (WBC), National Early Warning Score 2 (NEWS 2), acute respiratory distress syndrome (ARDS), reverse-transcriptase polymerase chain reaction (RT-PCR), positive end-expiratory pressure (PEEP), Acute Physiology and Chronic Health Evaluation II (APACHE II), neutrophil-to-lymphocyte ratio (NLR), interquartile range (IQR), odds ratios (ORs), confidence intervals (CIs), Receiver operating characteristic (ROC), red cell distribution width (RDW), area under the curve (AUC), Division of Digital Innovation and Data Analytics (DIDA).
Ethics Approval and Consent to Participate
This research was authorized by the Human Ethics Committee, Faculty of Medicine, Prince of Songkla University, and was carried out in line with the Declaration of Helsinki (REC 64-544-14-1). Since this study was retrospective and all data were anonymized, the Ethics Committee waived obtaining informed consent.
Acknowledgments
We thank the officers of the Division of Digital Innovation and Data Analytics (DIDA), Faculty of Medicine, Prince of Songkhla University, for their timely response to our request for information.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The Faculty of Medicine, Prince of Songkla University provided research funding to support this study (grant number:64-544-14-1).
Disclosure
The authors declare that they have no competing interests for this work.
References
1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi:10.1056/NEJMoa2001017
2. Mo P, Xing Y, Xiao Y, et al. Clinical characteristics of refractory coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2021;73(11):e4208–e4213. doi:10.1093/cid/ciaa270
3. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
4. Srichatrapimuk S, Jayanama K, Kirdlarp S, et al. Predictors of pneumonia and severe pneumonia in patients with coronavirus disease 2019 at a tertiary-care hospital, Thailand. Southeast Asian J Trop Med Public Health. 2020;51(4):507–517.
5. Mahendra M, Nuchin A, Kumar R, Shreedhar S, Mahesh PA. Predictors of mortality in patients with severe COVID-19 pneumonia - A retrospective study. Adv Respir Med. 2021;89(2):135–144. doi:10.5603/ARM.a2021.0036
6. Mas-Ubillus G, Ortiz PJ, Huaringa-Marcelo J, et al. High mortality among hospitalized adult patients with COVID-19 pneumonia in Peru: a single centre retrospective cohort study. PLoS One. 2022;17(3):e0265089. doi:10.1371/journal.pone.0265089
7. Brandão Neto RA, Marchini JF, Marino LO, et al. Mortality and other outcomes of patients with coronavirus disease pneumonia admitted to the emergency department: a prospective observational Brazilian study. PLoS One. 2021;16(1):e0244532.
8. Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. Hematological findings and complications of COVID-19. Am J Hematol. 2020;95(7):834–847.
9. Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med. 2020;58(7):1021–1028. doi:10.1515/cclm-2020-0369
10. World Health Organization. COVID-19 Clinical management: living guidance; 2021. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1.
11. Ranieri VM, Rubenfeld GD, Thompson BT; The ARDS Definition Task Force. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–2533. doi:10.1001/jama.2012.5669
12. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. doi:10.1097/00003246-198510000-00009
13. Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–382. doi:10.1136/thorax.58.5.377
14. Royal College of Physicians. National early warning score (NEWS) 2; 2017. Available from: https://www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2.
15. Liang W, Liang H, Ou L, et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med. 2020;180(8):1081–1089. doi:10.1001/jamainternmed.2020.2033
16. Knight SR, Ho A, Pius R, et al. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: development and validation of the 4C mortality score. BMJ. 2020;370:m3339. doi:10.1136/bmj.m3339
17. Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6(1):14–17.
18. Yamada T, Wakabayashi M, Yamaji T, et al. Value of leukocytosis and elevated C-reactive protein in predicting severe coronavirus 2019 (COVID-19): a systematic review and meta-analysis. Clin Chim Acta. 2020;509:235–243. doi:10.1016/j.cca.2020.06.008
19. Zhang L, Huang B, Xia H, et al. Retrospective analysis of clinical features in 134 coronavirus disease 2019 cases. Epidemiol Infect. 2020;148:e199. doi:10.1017/S0950268820002010
20. Zhu B, Feng X, Jiang C, et al. Correlation between white blood cell count at admission and mortality in COVID-19 patients: a retrospective study. BMC Infect Dis. 2021;21(1):574. doi:10.1186/s12879-021-06277-3
21. Palladino M. Complete blood count alterations in COVID-19 patients: a narrative review. Biochem Med. 2021;31(3):030501. doi:10.11613/BM.2021.030501
22. Buja LM, Wolf DA, Zhao B, et al. The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): report of 3 autopsies from Houston, Texas, and review of autopsy findings from other United States cities. Cardiovasc Pathol. 2020;48:107233. doi:10.1016/j.carpath.2020.107233
23. Danwang C, Endomba FT, Nkeck JR, Wouna DLA, Robert A, Noubiap JJ. A meta-analysis of potential biomarkers associated with severity of coronavirus disease 2019 (COVID-19). Biomark Res. 2020;8(1):37. doi:10.1186/s40364-020-00217-0
24. Huang W, Berube J, McNamara M, et al. Lymphocyte subset counts in COVID-19 patients: a meta-analysis. Cytometry A. 2020;97(8):772–776. doi:10.1002/cyto.a.24172
25. Liu Y, Sun W, Guo Y, et al. Association between platelet parameters and mortality in coronavirus disease 2019: retrospective cohort study. Platelets. 2020;31(4):490–496. doi:10.1080/09537104.2020.1754383
26. Aly MM, Meshref TS, Abdelhameid MA, et al. Can hematological ratios predict outcome of COVID-19 patients? A multicentric study. J Blood Med. 2021;12:505–515. doi:10.2147/JBM.S316681
27. Kilercik M, Demirelce Ö, Serdar MA, Mikailova P, Serteser M. A new haematocytometric index: predicting severity and mortality risk value in COVID-19 patients. PLoS One. 2021;16(8):e0254073. doi:10.1371/journal.pone.0254073
28. Liu J, Liu Y, Xiang P, et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med. 2020;18(1):206. doi:10.1186/s12967-020-02374-0
29. Lian J, Jin C, Hao S, et al. High neutrophil-to-lymphocyte ratio associated with progression to critical illness in older patients with COVID-19: a multicenter retrospective study. Aging. 2020;12(14):13849–13859. doi:10.18632/aging.103582
30. Yildiz H, Castanares-Zapatero D, Pierman G, et al. Validation of neutrophil-to-lymphocyte ratio cut-off value associated with high in-hospital mortality in COVID-19 patients. Int J Gen Med. 2021;14:5111–5117. doi:10.2147/IJGM.S326666
31. Yildiz H, Castanares-Zapatero D, Hannesse C, Vandermeersch D, Pothen L, Jc Y. Prospective validation and comparison of COVID-GRAM, NEWS2, 4C mortality score, CURB-65 for the prediction of critical illness in COVID-19 patients. Infect Dis. 2021;53(8):640–642. doi:10.1080/23744235.2021.1896777
32. Fu J, Kong J, Wang W, et al. The clinical implication of dynamic neutrophil to lymphocyte ratio and D-dimer in COVID-19: a retrospective study in Suzhou China. Thromb Res. 2020;192:3–8. doi:10.1016/j.thromres.2020.05.006
33. Ye W, Chen G, Li X, et al. Dynamic changes of D-dimer and neutrophil-lymphocyte count ratio as prognostic biomarkers in COVID-19. Respir Res. 2020;21(1):169. doi:10.1186/s12931-020-01428-7
34. Abensur Vuillaume L, Le Borgne P, Alamé K, et al. Neutrophil-to-lymphocyte ratio and early variation of NLR to predict in-hospital mortality and severity in ED Patients with SARS-CoV-2 infection. J Clin Med. 2021;10(12):2563. doi:10.3390/jcm10122563
35. Weng J, Brown CV, Rhee P, et al. White blood cell and platelet counts can be used to differentiate between infection and the normal response after splenectomy for trauma: prospective validation. J Trauma. 2005;59(5):1076–1080. doi:10.1097/01.ta.0000189001.00670.d2
36. Zhang J, Qiu Y, He X, Mao W, Han Z. Platelet-to-white blood cell ratio: a novel and promising prognostic marker for HBV-associated decompensated cirrhosis. J Clin Lab Anal. 2020;34(12):e23556. doi:10.1002/jcla.23556
37. Guo J, Zhou B, Zhu M, et al. CURB-65 may serve as a useful prognostic marker in COVID-19 patients within Wuhan, China: a retrospective cohort study. Epidemiol Infect. 2020;148:e241. doi:10.1017/S0950268820002368
38. Bradley J, Sbaih N, Chandler TR, Furmanek S, Ramirez JA, Cavallazzi R. Pneumonia severity index and CURB-65 score are good predictors of mortality in hospitalized patients with SARS-CoV-2 community-acquired pneumonia. Chest. 2022;161(4):927–936. doi:10.1016/j.chest.2021.10.031
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
