Back to Journals » Journal of Inflammation Research » Volume 16
Plasma and Peritoneal Fluid Annexin A2 Levels in Patients with Endometriosis
Authors Zygarowicz M , Kacperczyk-Bartnik J , Sierdzinski J, Wojtyla C, Pierzynski P, Manka G, Kiecka M, Spaczynski RZ, Piekarski P, Banaszewska B, Jakimiuk A, Issat T , Rokita W, Mlodawski J, Szubert M, Sieroszewski P, Raba G, Szczupak K, Kluz T, Kluza M, Lipa M, Warzecha D, Wielgos M, Koc-Zorawska E, Zorawski M, Laudanski P
Received 15 May 2023
Accepted for publication 6 September 2023
Published 7 December 2023 Volume 2023:16 Pages 5959—5969
DOI https://doi.org/10.2147/JIR.S421389
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Michal Zygarowicz,1,* Joanna Kacperczyk-Bartnik,2,3,* Janusz Sierdzinski,4 Cezary Wojtyla,5,6 Piotr Pierzynski,5,6 Grzegorz Manka,7 Mariusz Kiecka,7 Robert Z Spaczynski,8 Piotr Piekarski,9 Beata Banaszewska,10 Artur Jakimiuk,11,12 Tadeusz Issat,13 Wojciech Rokita14,15 ,† Jakub Mlodawski,14,15 Maria Szubert,3,16,17 Piotr Sieroszewski,16,18 Grzegorz Raba,19,20 Kamil Szczupak,19,20 Tomasz Kluz,21 Marek Kluza,21 Michal Lipa,3,22 Damian Warzecha,5,22 Miroslaw Wielgos,23,24 Ewa Koc-Zorawska,25,26 Marcin Zorawski,26,27 Piotr Laudanski5,6,28
1Students’ Scientific Group Affiliated to the Department of Obstetrics, Gynecology and Gynecological Oncology, Medical University of Warsaw, Warsaw, Poland; 2II Department of Obstetrics and Gynaecology, Medical University of Warsaw, Warsaw, Poland; 3Club 35. Polish Society of Gynecologists and Obstetricians, Wrocław, Poland; 4Department of Medical Informatics and Telemedicine, Medical University of Warsaw, Warsaw, Poland; 5OVIklinika Infertility Center, Warsaw, Poland; 6Women’s Health Research Institute, Calisia University, Kalisz, Poland; 7Angelius Provita Hospital, Katowice, Poland; 8Center for Gynecology, Obstetrics and Infertility Treatment Pastelova, Poznan, Poland; 9Division of Infertility and Reproductive Endocrinology, Department of Gynecology, Obstetrics and Gynecological Oncology, Poznan University of Medical Sciences, Poznan, Poland; 10Chair and Department of Laboratory Diagnostics, Poznan University of Medical Sciences, Poznan, Poland; 11Department of Obstetrics and Gynecology, Central Clinical Hospital of the Ministry of Interior, Warsaw, Poland; 12Center of Reproductive Health, Institute of Mother and Child in Warsaw, Warsaw, Poland; 13Department of Obstetrics and Gynecology, Institute of Mother and Child in Warsaw, Warsaw, Poland; 14Collegium Medicum Jan Kochanowski University in Kielce, Kielce, Poland; 15Clinic of Obstetrics and Gynecology, Provincial Combined Hospital in Kielce, Kielce, Poland; 16Department of Gynecology and Obstetrics Medical University of Lodz, Lodz, Poland; 17Department of Surgical Gynecology and Oncology, Medical University of Lodz, Lodz, Poland; 18Department of Fetal Medicine and Gynecology, Medical University of Lodz, Lodz, Poland; 19Clinic of Obstetrics and Gynecology, Provincial Hospital, Przemysl, Poland; 20Department of Obstetrics and Gynecology, University of Rzeszow, Rzeszow, Poland; 21Department of Gynecology, Gynecology Oncology and Obstetrics, Institute of Medical Sciences, Medical College of Rzeszow University, Rzeszow, Poland; 22Department of Obstetrics and Gynaecology, Warsaw Southern Hospital, Warsaw, Poland; 23Premium Medical, Warsaw, Poland; 24Faculty of Medicine, Lazarski University, Warsaw, Poland; 25II Department of Nephrology, Hypertension and Internal Medicine with Dialysis Unit, Medical University of Bialystok, Bialystok, Poland; 26The Academy of Applied Medical and Social Sciences, Elbląg, Poland; 27Department of Cardiology, Lipidology and Internal Medicine with Cardiac Intensive Care Unit, Medical University of Bialystok, Bialystok, Poland; 28Department of Obstetrics, Gynecology and Gynecological Oncology, Medical University of Warsaw, Warsaw, Poland
*These authors contributed equally to this work
†Professor Wojciech Rokita passed away on March 18, 2020
Correspondence: Piotr Laudanski, Department of Obstetrics, Gynecology and Gynecological Oncology, Medical University of Warsaw, Kondratowicza Street 8, Warsaw, 03-242, Poland, Tel +48 22 326 53 80, Email [email protected]
Introduction: Endometriosis is an inflammatory-related reproductive age disease characterized by the presence of endometrial cells outside the uterine cavity. Current laboratory practice does not provide specific markers for detecting and assessing the advancement of endometriosis in either plasma or peritoneal fluid. The severity of disease is assessed in stages from I to IV based on the results of laparoscopic inspection. The protein annexin A2 (ANXA2) has been reported to be associated with inflammatory processes.
Aim of the Study: The study aimed to investigate and compare ANXA2 protein concentration using the ELISA method in plasma and peritoneal fluid in a group of women with endometriosis compared to controls.
Materials and Methods: Biological material was collected during a multicenter, cross-sectional study, which was conducted at eight departments during elective laparoscopy from 53 women with and 40 women without endometriosis. Patients were divided by endometriosis stage and infertility status, and then compared with subgroups. Analysis included the Chi-square test for categorical variables, Mann–Whitney U-test and two-sided Wilcoxon rank-sum test for continuous variables.
Results: Women with endometriosis had significantly elevated plasma ANXA2 levels compared to women without endometriosis (mean concentrations 28.69 vs 19.61 ng/L, p=0.01). Differences in peritoneal fluid ANXA2 levels were statistically insignificant (mean concentrations of 23.7 vs 22.97 ng/L, p=0.06). Plasma concentrations in patients with stage III and IV endometriosis were significantly higher compared to controls (mean concentrations of 24.19 vs 19.71 ng/L, p=0.03). No such differences were observed in plasma when comparing stages I–II vs III–IV, and stages I–II vs controls (mean concentrations of 33.82 vs 24.19 ng/L, p=0.72 and 33.82 vs 19.71 ng/L, p=0.12, respectively). Comparison of samples from patients with or without infertility, primary or secondary infertility, endometriosis with or without infertility, and non-endometriosis with or without infertility showed no significant differences in the plasma nor in the peritoneal fluid concentrations.
Conclusion: ANXA2 is possibly involved in the pathogenesis of endometriosis, especially in advanced stages. Due to the limited group of tested samples, further studies are needed to confirm its role.
Keywords: annexin A2, endometriosis, infertility
Introduction
Endometriosis is a benign, chronic inflammatory disease characterized by the presence of endometrial tissue outside the uterus, most commonly in the pelvic peritoneum, the ovaries, and the rectovaginal septum.1 It affects about 10% of women in the general population of reproductive age, but among women suffering from infertility it affects about 50%.1–4 Endometriosis is most often manifested by chronic pelvic pain, infertility, dysmenorrhea and pain during sexual intercourse. The severity of the disease is assessed on a scale from I to IV, but the severity of symptoms varies considerably and does not always correlate with endometriosis stage.1–3
Endometriosis is an estrogen-dependent disease, which means that estrogen causes endometriosis cells to develop and survive, which then induces inflammation of the peritoneum. Chronic pro-inflammatory effects cause adhesions of intraperitoneal tissues, changes in the composition of the peritoneal fluid and, as a consequence, pain, infertility and difficulties maintaining pregnancy. Chronic inflammation creates conditions similar to those during the development of many cancers.5 The presence of endometriosis also increases the overall risk of developing malignancies, especially of the pelvis.6
The etiology of endometriosis is still not fully explained. There are numerous theories trying to illustrate this condition.4,7–13 Sampson’s theory is the most popular explanation for the pathogenesis and states that endometriosis is the result of retrograde menstruation, during which endometrial cells implant in the peritoneum.12 Moreover, the role of the immune response in endometriosis pathogenesis may be particularly extensive.14,15
As the gold standard, final diagnosis of endometriosis is based on histopathological examination of lesion samples.16 Unfortunately, this method is invasive and requires visible macroscopic lesions.
Non-specific clinical presentation causes delays in diagnosis, often exceeding 7 years.17,18 A great hope for the development of diagnostics is associated with research on endometriosis-specific biomarkers enabling detection of the disease at an early stage.19,20
Many potential biomarkers that may have an impact on pathogenesis of endometriosis are being studied, among which are metalloproteinases, growth factors, cytokines, chemokines, miRNAs and adhesion molecules.3,7–9,19,21
Annexin family proteins are known to be involved in the interaction of membrane structures that expose these proteins.22–25 Annexin A2 (ANXA2) has been shown to be specific to endometriosis several times in scientific publications, but final conclusions differ in terms of whether it is significantly increased in stages I–IV or only in stages III and IV.26,27 The divergent results show that further studies are needed involving larger groups of patients.
ANXA2 protein is also markedly increased in malignant diseases, including lung cancer, gastric cancer, pancreatic ductal adenocarcinoma, colorectal cancer, hepatocellular carcinoma, breast cancer, cervical cancer, endometrial cancer, ovarian cancer, renal cell carcinoma, high-grade prostate cancer, glioblastoma, multiple myeloma, acute lymphoblastic leukemia, and acute promyelocytic leukemia.28–32
In addition, ANXA2 is a protein markedly present in prostasomes (secretory vesicles of the prostate epithelium of men) and is part of seminal fluid.22 Prostasomes, together with spermatozoa, enter the uterine cavity, and then combine with spermatozoa in the fallopian tube, presumably to participate in the process of fertilization of the ovum.33 Other ANXA family proteins are known to function in a similar way to ANXA2.34 ANXA1 is also present in sperm (not only in prostasomes). Together with ANXA5, both are reported to participate in fertilization through local immunomodulatory effects on women’s lymphocytes.22,35 Prostasomes regulate sperm motility, capacitation and acrosomal reaction.33 ANXA2 is involved in actin remodeling, protein assembly, transcription, mRNA transport, and DNA replication and repair.36
The aim of this study was to examine ANXA2 protein levels in plasma and peritoneal fluid in a group of women with endometriosis compared to a control group. Secondary aims included analysis of ANXA2 levels in women at different endometriosis stages (I–IV) and in infertile patients.
Materials and Methods
Biological material was collected during a multicenter, cross-sectional study conducted in eight Obstetrics and Gynecology Departments in Poland between 2018 and 2019 (project number: 6/6/4/1/NPZ/2017/1210/13522, financed by the Polish Ministry of Health): Department of Obstetrics and Gynecology, Medical University of Warsaw; Angelius Provita Hospital, Katowice; Department of Gynecology, Division of Infertility and Reproductive Endocrinology, Obstetrics and Gynecological Oncology at Poznan University of Medical Sciences; Department of Obstetrics and Gynecology, Central Clinical Hospital of the Ministry of Interior in Warsaw; Clinic of Obstetrics and Gynecology, Provincial Combined Hospital, Kielce; Department of Surgical Gynecology and Oncology, Medical University of Lodz; Department of Gynecology and Obstetrics, Provincial Hospital, Przemyśl; and Department of Gynecology, Gynecology Oncology, and Obstetrics, Institute of Medical Sciences, Medical College of Rzeszow University.37
Patients qualified for elective laparoscopic procedures if they had non-malignant indications, such as: idiopathic infertility, chronic pelvic pain syndrome, ovarian cysts or suspected endometriosis. Infertility was defined as the inability to become pregnant during at least 12 months of regular unprotected intercourse in women under the age of 35 and at least 6 months in other women.38
Exclusion criteria were irregular menstruation (over 35 days or less than 25 days), age under 18 or over 40 years, hormonal therapy in the preceding 3 months before laparoscopy, malignant or suspected malignant disease, autoimmune disease, previous and/or current pelvic inflammatory disease, any previous pelvic surgery, uterine fibroids or polycystic ovaries.
The cycle phase was calculated based on previous menstruation dates and average length of menstrual cycle. In addition, the phases of the menstrual cycle in women with and without endometriosis were determined based on histological dating of eutopic endometrial samples collected simultaneously with pathological changes.
Each patient was evaluated based on the American Fertility Society revised classification of endometriosis, along with histological examination of the biopsies.39
All patients completed the clinical questionnaire of the World Endometriosis Research Foundation.40 Written informed consent was obtained from all patients. The study was approved by the Independent Ethics Committee of the Medical University of Warsaw (KB/223/2017).
Patients fasted 6 to 12 hours before surgery. Prior to the procedure and before anesthesia induction, blood samples were collected in 10 mL ethylenediaminetetraacetic acid tubes (Sarstedt) in order to assess ANXA2 plasma levels. Peritoneal fluid was aspirated with a Veress needle under direct visual control at the beginning of laparoscopy to avoid blood contamination. Each procedure was performed in accordance with the standard operating procedures of the Endometriosis Phenome and Biobanking Harmonization Project.41 The collection of biological material had no influence on the medical treatment of the patients and was completed in accordance with the Declaration of Helsinki. The aspirated peritoneal fluid was centrifuged in all centers at 1000 x g for 10 minutes at 4°C. The supernatant was transferred to a fresh 10 mL tube (Sarstedt). The same types of tube were used in all blood and peritoneal fluid collection centers. The time lapse between sample collection (both peritoneal fluid and plasma) and processing was under 45 minutes. All centers centrifuged blood samples at 2500 x g for 10 minutes at 4°C. All samples were stored at −80°C.
Based on the results of laparoscopic inspection, patients were assigned to the appropriate endometriosis stage subgroup (I–IV). Patients without visible endometriosis lesions were recruited to the control group. Later, we also divided the patients with endometriosis into two separate groups because of the similarities in disease activity between stages within the groups: (1) grade I or II endometriosis or (2) grade III or IV endometriosis. Information about endometriosis stage was not provided by participating centres in the case of three patients.
Double-antibody sandwich enzyme-linked immunosorbent assay (ELISA) was performed in order to assess levels of ANXA2 in collected plasma and peritoneal fluid samples. ELISA is a quantitative method that has been used for decades for detection and quantification of specific substances.42,43 It has also been widely performed in order to detect ANXA2 in human biological samples.20,44–46 Human ANXA2 ELISA kits (SunRedBio, Shanghai, China, catalogue number 201-12-1089) were used with a sensitivity of 0.135 ng/L and an assay range of 0.3–40 ng/L. Quantitative ANXA2 level analyses were financed by an internal grant from the Medical University of Warsaw (project number: 1W51/1/M/MB/N/21). Study protocol was approved by the Institutional Review Board at the Medical University of Warsaw (approval number: AKBE/245/2021).
Statistical analysis was performed with SAS v. 9.4 (SAS Institute, Cary, NC, USA) and Statistica v. 13.3 software (StatSoft Inc., Kraków, Poland). The groups were compared by Chi-square test for categorical variables. Mann–Whitney U-test and two-sided Wilcoxon rank-sum test were performed for continuous variables depending on the distribution of variables after testing for normal distribution using the Shapiro–Wilk test. Generation of a receiver-operating characteristics (ROC) curve and calculation of the area under the curve (AUC) and 95% confidence intervals (95% CI) were used to assess the predictive power of ANXA2 concentration in the plasma and peritoneal fluid. The level of statistical significance was set at p <0.05. Datasets are available and will be shared by the corresponding author upon request.
Results
Table 1 and Table 2 show the characteristics and results of Annexin A2 levels in the study and control groups (women with and without endometriosis). There was a significantly higher mean level of plasma (28.69 vs 19.61 ng/L) and higher median (12.31 vs 7.85 ng/L) ANXA2 concentrations in patients with endometriosis compared to patients without endometriosis (p=0.01). There was also a higher mean level of peritoneal fluid (23.7 vs 22.97 ng/L) and higher median (15.66 vs 9.42 ng/L) ANXA2 concentrations in patients with endometriosis compared to patients without endometriosis, but the differences were not statistically significant (p=0.06).
 |
Table 1 Group Characteristics and Annexin A2 Levels Detected in Plasma of Patients with and without Endometriosis |
 |
Table 2 Group Characteristics and Annexin A2 Levels Detected in Peritoneal Fluid of Patients with and without Endometriosis |
Table 3 presents the results of ANXA2 levels of patients at different endometriosis stages and women without endometriosis. There was a statistically significant higher mean level of plasma (24.19 vs 19.71 ng/L) and higher median (14.69 vs 7.91 ng/L) ANXA2 concentrations in patients at stage III and IV compared to patients without endometriosis (p=0.03). There was also a higher mean level of peritoneal fluid (26.64 vs 22.92 ng/L) and higher median (19.7 vs 9.65 ng/L) ANXA2 concentrations in patients at stages III and IV compared to patients without endometriosis; however, the differences were not statistically significant (p=0.07).
 |
Table 3 Comparison of Plasma and Peritoneal Fluid Annexin A2 Levels Depending on Endometriosis Stage |
Additional analyses, as shown in Table 4, examined the association between ANXA2 levels and infertility. A tendency towards a higher mean level of plasma (30.40 vs 18.45 ng/L) and median (12.06 vs 8.34 ng/L) ANXA2 levels were characteristic of a history of infertility, but no statistically significant differences regarding ANXA2 plasma levels were detected (p=0.12). A similar trend was noticed in the peritoneal fluid. We also observed a higher mean level of peritoneal fluid (25.61 vs 11.52 ng/L) and higher median (14.70 vs 8.69 ng/L) ANXA2 concentrations in patients with primary infertility compared to patients with secondary infertility, yet the differences were not significant (p=0.06).
 |
Table 4 Annexin A2 Levels Detected in Plasma and Peritoneal Fluid of Patients with and without Infertility |
Comparison of plasma and peritoneal fluid ANXA2 concentrations within the endometriosis group did not show any statistically significant differences between women with and without infertility issues (Table 4).
The discriminatory ability of ANXA2 concentrations in the plasma and in the peritoneal fluid in the total population analyzed were evaluated by ROC analysis. ROC curves are presented in Figure 1. The AUC value for ANXA2 plasma concentration was 0.654 (95% CI: 0.54–0.77, p=0.008). For ANXA2 concentrations in the peritoneal fluid, the AUC value was 0.622 (95% CI: 0.50–0.75, p=0.059). The diagnostic values of ANXA2 concentrations evaluation are summarized in Table 5. The overall model quality for the diagnosis of endometriosis exceeded 0.5 only for the ANXA2 plasma concentration and this was not achieved for ANXA2 concentration in the peritoneal fluid. The cutoff value of 6.941 ng/L in the plasma was associated with 83% sensitivity and 57.5% specificity.
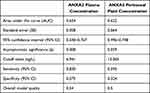 |
Table 5 Receiver-Operating Characteristics (ROC) Analysis and Diagnostic Value of ANXA2 Concentration in the Plasma and in Peritoneal Fluid of Women with Endometriosis and Control Women |
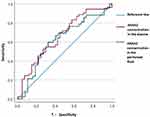 |
Figure 1 Receiver-operating characteristics (ROC) curves of ANXA2 concentration in the plasma and the peritoneal fluid of women with endometriosis and control women. |
Discussion
The main finding of our study was the higher level of ANXA2 plasma concentration detected in patients with endometriosis compared to women without endometriosis. There are several reports in the literature on elevated ANXA2 protein levels in women with endometriosis. Nazri et al examined the concentration of exosomes in the peritoneal fluid and the content of protein composition in isolated exosomes in a group of women with endometriosis compared to a control group.26 In their results, they ranked ANXA2 among five proteins significantly specific for endometriosis. The authors explained that ANXA2 serves as an activator of matrix metallopeptidase (MMP-9) of peritoneal macrophages and participates in the degradation of the extracellular matrix of the endometrial tissue which flows through retrograde menstruation. In addition, simultaneous damage to the extracellular matrix of the peritoneal layer of mesothelial cells by ANXA2-containing exosomes may allow implantation and development of ectopic endometrial lesions.47 The exact cellular source of the increased ANXA2 production is not clear, but the focus is on ectopic endometrial tissue. This idea is supported by a certain similarity between endometriosis and metastatic cancer, especially since the elevated level of ANXA2 protein is already known to be typically present in many cancers, including endometrial cancer.48–52 These authors also consider monocytes to be cells that secrete ANXA2 in exosomes. In the same study it was also stated that endometriosis in stages I and II may differ in its pathogenesis from that in stages III and IV, resulting in a difference in ANXA2 concentrations, and this may create the use of ANXA2 as a biomarker differentiating endometriosis stages. In another study, Kaya et al also showed significantly higher serum concentrations of ANXA2 in women at stage III and IV endometriosis compared with those at stage I and II and in the control group without endometriosis.27 Our study showed no significant differences between these groups in either plasma or peritoneal fluid; however, this could be caused by the sample size. We observed that plasma ANXA2 levels are significantly higher in patients at stage III–IV endometriosis compared with women without endometriosis. There was no similar observation for patients at stage I–II endometriosis in comparison to the control group (Table 3).
In a study by Sun et al, ANXA2 levels in ectopic (study group) and eutopic (control group) endometrial tissues were compared.53 The results are inconsistent with previously cited studies, as ANXA2 concentration was reduced in the study group. This may be due to the fact that the control group included mostly endometrial tissues from patients with grade II–III cervical intraepithelial neoplasia. Considering the numerous reports of elevated ANXA2 in cancer, this may be the reason for the increased ANXA2 in the control group in relation to the study group. Another explanation for this finding may be the fact that endometrial tissue is evaluated rather than peritoneal fluid or plasma, which can give contradictory results. Thus, the results of Sun et al only seem to confirm that the process of carcinogenesis promotes the expression of ANXA2 in tissues, including the endometrium, which was particularly demonstrated by Zou et al with the example of endometrial cancer.54
A different cross-sectional study, by Volpato et al, applied the Western blotting method to measure Annexin A1 expression in peritoneal samples of women with (n=22) and without (n=18) endometriosis.55 Annexin A1 was detected in both the study and control groups, but its expression was lower in women with endometriosis. The same study also evaluated cytokine expression in the peritoneal fluid using the ELISA method and observed that women with endometriosis were characterized by higher IL-6 concentration, but the IL-1β levels were comparable with the control group. The authors concluded that reduced inflammatory resolution mediators could cause development of inflammatory endurance and aggravation of endometriosis. Contradictory results were presented in a study by Li et al,56 which analyzed eutopic endometrium samples of 25 patients with endometriosis and 16 healthy women. Additionally, peritoneal fluid of ten women with endometriosis was examined. The authors observed Annexin A1 overexpression in both the eutopic endometrium and peritoneal fluid of endometriosis patients. Paula et al compared the expression of Annexin A1, mast cell proteases and formyl peptide receptor 1 (FPR1) in the ectopic endometrium of 18 women with eutopic endometrium and 10 women without endometriosis.57 Histology results of ectopic endometriotic lesions presented an undifferentiated glandular pattern with inflammatory cells and altered mast cell heterogeneity. This finding was also associated with elevated ANXA1 and FPR1 expression in the epithelial cells. It was concluded that simultaneous upregulation of mast cell chymase, ANXA1 and FPR1 is involved in development of ectopic endometriotic lesions.
Hsu et al demonstrated the positive effect of ANXA2 on motility and the angiogenic potential of endometrial stromal cells in vitro.58 The authors examined the function of ANXA2 present in small extracellular vesicles produced by ectopic endometrial tissue. Change in cell activity is caused by upregulation of the ERK/STAT3 pathway. As a result, ANXA2 creates heterotetramer with S100 A10 calcium-binding protein (S100A10), translocates to the cell surface, activates the plasminogen, ERK1/2, and degrades the extracellular matrix. This process is required for the initiation of cell migration, invasion, and angiogenesis. ANXA2 is present in small extracellular vesicles from ectopic endometrial stromal cells and is absent in those from eutopic endometrial stromal cells, which is consistent with the findings reported by Nazri et al.26 They concluded that retrograde menstrual tissue might be one of the sources of small extracellular vesicles within the peritoneal fluid and thus promotes the development of endometriotic lesions. However, our study showed that it is not so easy to detect the difference in the concentration of this protein in the peritoneal fluid using only ELISA without isolation of small extracellular vesicles. Our negative results regarding the lack of observation of significant differences in the concentration of ANXA2 in the peritoneal fluid between patients with and without endometriosis and between patients at different stages of endometriosis do not exclude the possibility of ANXA2 involvement in the pathogenesis of endometriosis. Kajdos et al performed flow cytometry and compared plasma and peritoneal fluid samples of patients with ovarian endometriosis (n=23) and teratoma (n=7) to evaluate the presence of extracellular microvesicles.59 The authors reported an association between endometriosis and a significantly higher plasma level of Annexin V-positive microvesicles.
It is also worth noting that large variations in ANXA2 values were observed in our relatively homogeneous group of patients. This suggests that multiple factors may be responsible for the levels of ANXA2 detected and questions the possibility of using ANXA2 concentration in peritoneal fluid as a biomarker. Zhou et al reported overexpression of ANXA2 in adenomyosis and described many cellular processes in which this protein is involved, including endocytosis, exocytosis, and cellular adhesion.60 ANXA2 can bind to membrane phospholipids in a Ca2-dependent manner, which provides a link between Ca2 signaling and membrane functions. It also forms networks on the cell surface, which organize membrane domains and membrane recruitment platforms for interacting proteins. This demonstrates multiple possible levels of ANXA2-mediated pathogenesis of endometriosis. Similar findings were reported in a study by Liu et al.20 Overexpression of ANXA2 was detected using the immunohistochemical method in both ectopic and eutopic endometrium tissues from 30 patients with adenomyosis compared to 15 patients with uterine fibroids. No statistically significant differences in ANXA2 levels were observed between eutopic and ectopic samples of patients with adenomyosis. Additionally, these authors observed a positive correlation between severity of dysmenorrhea and expression of ANXA2. Saher et al explored the expression of potential biomarkers for ovarian endometriomas.61 In this case-control study, the authors performed differential proteomic analysis of eutopic and ectopic tissue of six patients with ovarian endometriosis. As Annexin A5 is responsible for apoptosis inhibition, cell migration and invasion, the molecular analysis showed its overexpression in the ectopic ovarian endometriomas compared with the eutopic endometrial tissue.
One of the limitations of our study was the size of the study group, which may have resulted in insignificant results regarding the difference in ANXA2 concentrations in the peritoneal fluid of patients with and without endometriosis. In order to overcome this limitation, further cooperation and research by a multi-center working group on endometriosis is planned. The strength of the work is the analysis of ANXA2 concentrations in samples collected from the population of women diagnosed with endometriosis and infertility, as so far there are few published reports on this subject, and most of them focus on oncology.
Conclusions
Our study mainly showed significantly higher plasma levels of ANXA2 in women with endometriosis compared to the control group without endometriosis. Undoubtedly, this is a reason for further research on the ANXA2 protein in the context of its use as a biomarker of endometriosis, perhaps also in combination with other biomarkers to increase the sensitivity of the test. Accurate results according to stage of endometriosis showed that this protein was much more useful in detecting stages III and IV than I and II. The lack of statistically significant results in infertility comparisons directs further ANXA2 research more towards elucidating a role in the pathogenesis of endometriosis, but not infertility in general.
Abbreviations
ANXA2, Annexin A2; AUC, area under the curve; ELISA, enzyme-linked immunosorbent assay; FPR1, peptide receptor 1; ROC, receiver-operating characteristics.
Disclosure
Michal Zygarowicz, Dr Joanna Kacperczyk-Bartnik and Professor Piotr Laudanski report grant from the Medical University of Warsaw no. 1W51/1/M/MB/N/21 used for this study. Michal Zygarowicz also reports non-financial support from Medical University of Białystok. Professor Piotr Laudanski reports grant from the Polish Ministry of Health no. 6/6/4/1/NPZ/2017/1210/13522 and grant from the European Union’s Horizon 2020 Research and Innovation Program under the Marie Skłodowska-Curie grant no. 101008193 TRENDO during the conduction of the study. This study was conducted with the use of equipment purchased by Medical University of Białystok as part of the RPOWP 2007-2013 funding, Priority I, Axis 1.1, contract No. UDA- RPPD.01.01.00-20-001/15-00 dated 26.06.2015. The authors report no other conflicts of interest in this work.
References
1. Giudice LC, Kao LC. Endometriosis. Lancet. 2004;364(9447):1789–1799. doi:10.1016/S0140-6736(04)17403-5
2. Giudice LC. Clinical practice. Endometriosis. N Engl J Med. 2010;362(25):2389–2398. doi:10.1056/NEJMcp1000274
3. Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med. 2020;382(13):1244–1256. doi:10.1056/NEJMra1810764
4. Załęcka J, Pankiewicz K, Issat T, Laudański P. Molecular mechanisms underlying the association between endometriosis and ectopic pregnancy. Int J Mol Sci. 2022;23(7):3490. doi:10.3390/ijms23073490
5. Guo SW. Cancer-associated mutations in endometriosis: shedding light on the pathogenesis and pathophysiology. Hum Reprod Update. 2020;26(3):423–449. doi:10.1093/humupd/dmz047
6. Van Gorp T, Amant F, Neven P, Vergote I, Moerman P. Endometriosis and the development of malignant tumours of the pelvis. A review of literature. Best Pract Res Clin Obstet Gynaecol. 2004;18(2):349–371. doi:10.1016/j.bpobgyn.2003.03.001
7. Laudanski P, Charkiewicz R, Kuzmicki M, et al. Profiling of selected angiogenesis-related genes in proliferative eutopic endometrium of women with endometriosis. Eur J Obstet Gynecol Reprod Biol. 2014;172:85–92. doi:10.1016/j.ejogrb.2013.10.007
8. Laudanski P, Charkiewicz R, Tolwinska A, Szamatowicz J, Charkiewicz A, Niklinski J. Profiling of selected MicroRNAs in proliferative eutopic endometrium of women with ovarian endometriosis. Biomed Res Int. 2015;2015:760698. doi:10.1155/2015/760698
9. Laudanski P, Gorodkiewicz E, Ramotowska B, Charkiewicz R, Kuzmicki M, Szamatowicz J. Determination of cathepsins B, D and G concentration in eutopic proliferative endometrium of women with endometriosis by the surface plasmon resonance imaging (SPRI) technique. Eur J Obstet Gynecol Reprod Biol. 2013;169(1):80–83. doi:10.1016/j.ejogrb.2013.01.024
10. Laudański P, Szamatowicz J, Oniszczuk M. Profiling of peritoneal fluid of women with endometriosis by chemokine protein array. Adv Med Sci. 2006;51:148–152.
11. Laudanski P, Szamatowicz J, Ramel P. Matrix metalloproteinase-13 and membrane type-1 matrix metalloproteinase in peritoneal fluid of women with endometriosis. Gynecol Endocrinol. 2005;21(2):106–110. doi:10.1080/09513590500154043
12. Sourial S, Tempest N, Hapangama DK. Theories on the pathogenesis of endometriosis. Int J Reprod Med. 2014;2014:179515. doi:10.1155/2014/179515
13. Szamatowicz J, Laudański P, Tomaszewska I, Szamatowicz M. Chemokine growth-regulated-alpha: a possible role in the pathogenesis of endometriosis. Gynecol Endocrinol. 2002;16(2):137–141. doi:10.1080/gye.16.2.137.141
14. Karadadas E, Hortu I, Ak H, Ergenoglu AM, Karadadas N, Aydin HH. Evaluation of complement system proteins C3a, C5a and C6 in patients of endometriosis. Clin Biochem. 2020;81:15–19. doi:10.1016/j.clinbiochem.2020.04.005
15. ebovic DI, Mueller MD, Taylor RN, Lebovic DI. Immunobiology of endometriosis. Fertil Steril. 2001;75(1):1–10. doi:10.1016/S0015-0282(00)01630-7
16. Becker CM, Bokor A, Heikinheimo O, et al.; ESHRE Endometriosis Guideline Group. ESHRE guideline: endometriosis. Hum Reprod Open. 2022;2022(2):hoac009. doi:10.1093/hropen/hoac009.
17. Wróbel M, Wielgoś M, Laudański P. Diagnostic delay of endometriosis in adults and adolescence-current stage of knowledge. Adv Med Sci. 2022;67(1):148–153. doi:10.1016/j.advms.2022.02.003
18. Staal AH, van der Zanden M, Nap AW. Diagnostic Delay of Endometriosis in the Netherlands. Gynecol Obstet Invest. 2016;81(4):321–324. doi:10.1159/000441911
19. Nisenblat V, Bossuyt PM, Shaikh R, et al. Blood biomarkers for the non-invasive diagnosis of endometriosis. Cochrane Database Syst Rev. 2016;2016(5):CD012179. doi:10.1002/14651858.CD012179
20. Liu F, Liu L, Zheng J. Expression of annexin A2 in adenomyosis and dysmenorrhea. Arch Gynecol Obstet. 2019;300(3):711–716. doi:10.1007/s00404-019-05205-w
21. Goławski K, Soczewica R, Kacperczyk-Bartnik J, et al. The role of cadherin 12 (CDH12) in the peritoneal fluid among patients with endometriosis and endometriosis-related infertility. Int J Environ Res Public Health. 2022;19(18):11586. doi:10.3390/ijerph191811586
22. Munuce MJ, Marini PE, Teijeiro JM. Expression profile and distribution of Annexin A1, A2 and A5 in human semen. Andrologia. 2019;51(2):e13224. doi:10.1111/and.13224
23. Matos ALL, Kudruk S, Moratz J, et al. Membrane binding promotes annexin A2 oligomerization. Cells. 2020;9(5):1169. doi:10.3390/cells9051169
24. Tao M, Isas JM, Langen R. Annexin B12 trimer formation is governed by a network of protein-protein and protein-lipid interactions. Sci Rep. 2020;10(1):5301. doi:10.1038/s41598-020-62343-x
25. Liu L. Calcium-dependent self-association of annexin II: a possible implication in exocytosis. Cell Signal. 1999;11(5):317–324. doi:10.1016/S0898-6568(98)00047-3
26. Nazri HM, Imran M, Fischer R, et al. Characterization of exosomes in peritoneal fluid of endometriosis patients. Fertil Steril. 2020;113(2):364–373. doi:10.1016/j.fertnstert.2019.09.032
27. Kaya C, Alay I, Guraslan H, et al. The role of serum caspase 3 levels in prediction of endometriosis severity. Gynecol Obstet Invest. 2018;83(6):576–585. doi:10.1159/000489494
28. Chen CY, Lin YS, Chen CH, Chen YJ. Annexin A2-mediated cancer progression and therapeutic resistance in nasopharyngeal carcinoma. J Biomed Sci. 2018;25(1):30. doi:10.1186/s12929-018-0430-8
29. Huang Y, Jia M, Yang X, et al. Annexin A2: the diversity of pathological effects in tumorigenesis and immune response. Int J Cancer. 2022;151(4):497–509. doi:10.1002/ijc.34048
30. Li Z, Yu L, Hu B, et al. Advances in cancer treatment: a new therapeutic target, Annexin A2. J Cancer. 2021;12(12):3587–3596. doi:10.7150/jca.55173
31. Qiu LW, Liu YF, Cao XQ, et al. Annexin A2 promotion of hepatocellular carcinoma tumorigenesis via the immune microenvironment. World J Gastroenterol. 2020;26(18):2126–2137. doi:10.3748/wjg.v26.i18.2126
32. Sharma MC. Annexin A2 (ANX A2): an emerging biomarker and potential therapeutic target for aggressive cancers. Int J Cancer. 2019;144(9):2074–2081. doi:10.1002/ijc.31817
33. Aalberts M, Sostaric E, Wubbolts R, et al. Spermatozoa recruit prostasomes in response to capacitation induction. Biochim Biophys Acta. 2013;1834(11):2326–2335. doi:10.1016/j.bbapap.2012.08.008
34. Schloer S, Pajonczyk D, Rescher U. Annexins in translational research: hidden treasures to be found. Int J Mol Sci. 2018;19(6):1781. doi:10.3390/ijms19061781
35. Rand JH, Arslan AA, Wu XX, et al. Reduction of circulating annexin A5 levels and resistance to annexin A5 anticoagulant activity in women with recurrent spontaneous pregnancy losses. Am J Obstet Gynecol. 2006;194(1):182–188. doi:10.1016/j.ajog.2005.05.034
36. Ayala-Sanmartin J, Zibouche M, Illien F, Vincent M, Gallay J. Insight into the location and dynamics of the annexin A2 N-terminal domain during Ca2+-induced membrane bridging. Biochim Biophys Acta. 2008;1778(2):472–482. doi:10.1016/j.bbamem.2007.11.004
37. Laudański P, Rogalska G, Warzecha D, et al. Autoantibody screening of plasma and peritoneal fluid of patients with endometriosis. Hum Reprod. 2023;38(4):629–643. doi:10.1093/humrep/dead011
38. Practice Committee of the American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril. 2020;113(3):533–535. doi:10.1016/j.fertnstert.2019.11.025
39. Canis M, Donnez JG, Guzick DS, et al. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67(5):817–821. doi:10.1016/S0015-0282(97)81391-X
40. WERF EPHect Working Group, Vitonis AF, Vincent K, Rahmioglu N, et al. World Endometriosis Research Foundation Endometriosis Phenome and Biobanking Harmonization Project: II. Clinical Covariate Phenotype Data Collection Endometriosis Res Fertil Steril. 2014;102(5):1223–1232.
41. WERF EPHect Working Group, Rahmioglu N, Fassbender A, Vitonis AF, et al. World endometriosis research foundation endometriosis phenome and biobanking harmonization project: III. Fluid biospecimen collection, processing, and storage in endometriosis research. Fertil Steril. 2014;102(5):1233–1243. doi:10.1016/j.fertnstert.2014.07.1208.
42. Engvall E, Perlmann P. Enzyme-linked immunosorbent assay (ELISA). Quantitative assay of immunoglobulin G. Immunochemistry. 1971;8(9):871–874. doi:10.1016/0019-2791(71)90454-X
43. Van Weemen BK, Schuurs AH. Immunoassay using antigen-enzyme conjugates. FEBS Lett. 1971;15(3):232–236. doi:10.1016/0014-5793(71)80319-8
44. Karabulut M, Afsar CU, Serilmez M, Karabulut S. Circulating annexin A2 as a biomarker in patients with pancreatic cancer. J Cancer Res Ther. 2020;16(9):S110–S115. doi:10.4103/jcrt.JCRT_755_18
45. Liu LX, Wu YG, Zheng J. Increased annexin A2 and decreased β-catenin in adenomyosis contribute to adenomyosis-associated dysmenorrhea. Histol Histopathol. 2017;32(12):1333–1340. doi:10.14670/HH-11-906
46. Yang J, Yang F, Nie J, et al. Evaluation of annexin A2 as a novel diagnostic serum biomarker for lung cancer. Cancer Biomark. 2015;15(2):205–211. doi:10.3233/CBM-140455
47. Costa-Silva B, Aiello NM, Ocean AJ, et al. Pancreatic cancer exosomes initiate pre-metastatic niche formation in the liver. Nat Cell Biol. 2015;17(6):816–826. doi:10.1038/ncb3169
48. Alonso-Alconada L, Santacana M, Garcia-Sanz P, et al. Annexin-A2 as predictor biomarker of recurrent disease in endometrial cancer. Int J Cancer. 2015;136(8):1863–1873. doi:10.1002/ijc.29213
49. Hernández JE, González-Montiel A, Allos-Villalva JCC, et al. Prognostic molecular biomarkers in endometrial cancer: a review. J Cancer Res Ther. 2019;7(3):17–28. doi:10.14312/2052-4994.2019-3
50. Herrero C, Brea J, Pérez-Díaz A, et al. Modeling ANXA2-overexpressing circulating tumor cells homing and high throughput screening for metastasis impairment in endometrial carcinomas. Biomed Pharmacother. 2021;140:111744. doi:10.1016/j.biopha.2021.111744
51. Herrero C, de la Fuente A, Casas-Arozamena C, et al. Extracellular vesicles-based biomarkers represent a promising liquid biopsy in endometrial cancer. Cancers. 2019;11(12):2000. doi:10.3390/cancers11122000
52. Maxwell GL, Hood BL, Day R, et al. Proteomic analysis of stage I endometrial cancer tissue: identification of proteins associated with oxidative processes and inflammation. Gynecol Oncol. 2011;121(3):586–594. doi:10.1016/j.ygyno.2011.02.031
53. Sun D, Wang Y, Wang L, Guo X. MicroRNA-342 promotes the malignant-like phenotype of endometrial stromal cells via regulation of annexin A2. Anal Cell Pathol. 2021;2021:1328682. doi:10.1155/2021/1328682
54. Zou LB, Zhang RJ, Tan YJ, et al. Identification of estrogen response element in the aquaporin-2 gene that mediates estrogen-induced cell migration and invasion in human endometrial carcinoma. J Clin Endocrinol Metab. 2011;96(9):E1399–408. doi:10.1210/jc.2011-0426
55. Volpato LK, Horewicz VV, Bobinski F, Martins DF, Piovezan AP. Annexin A1, FPR2/ALX, and inflammatory cytokine expression in peritoneal endometriosis. J Reprod Immunol. 2018;129:30–35. doi:10.1016/j.jri.2018.08.002
56. Li CY, Lang JH, Liu HY, Zhou HM. Expression of Annexin-1 in patients with endometriosis. Chin Med J. 2008;121(10):927–931. doi:10.1097/00029330-200805020-00012
57. Paula R, Oliani AH, Vaz-Oliani DC, D’Ávila SC, Oliani SM, Gil CD. The intricate role of mast cell proteases and the annexin A1-FPR1 system in abdominal wall endometriosis. J Mol Histol. 2015;46(1):33–43. doi:10.1007/s10735-014-9595-y
58. Hsu CY, Hsieh TH, Lin HY, et al. Characterization and proteomic analysis of endometrial stromal cell-derived small extracellular vesicles. J Clin Endocrinol Metab. 2021;106(5):1516–1529. doi:10.1210/clinem/dgab045
59. Kajdos M, Szymanski J, Jerczynska H, Stetkiewicz T, Wilczynski JR. Microvesicles released from ectopic endometrial foci as a potential biomarker of endometriosis. Ginekol Pol. 2022. doi:10.5603/GP.a2022.0096
60. Zhou S, Yi T, Liu R, et al. Proteomics identification of annexin A2 as a key mediator in the metastasis and proangiogenesis of endometrial cells in human adenomyosis. Mol Cell Proteomics. 2012;11(7):
61. Sahar T, Nigam A, Anjum S, Waziri F, Jain SK, Wajid S. Differential expression of Lumican, Mimecan, Annexin A5 and Serotransferrin in ectopic and matched eutopic endometrium in ovarian endometriosis: a case-control study. Gynecol Endocrinol. 2021;37(1):56–60. doi:10.1080/09513590.2020.1824218
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
