Back to Journals » Advances in Medical Education and Practice » Volume 8
Physician perspectives on education, training, and implementation of complementary and alternative medicine
Authors Patel SJ , Kemper KJ, Kitzmiller JP
Received 1 April 2017
Accepted for publication 19 May 2017
Published 25 July 2017 Volume 2017:8 Pages 499—503
DOI https://doi.org/10.2147/AMEP.S138572
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Sejal J Patel,1 Kathi J Kemper,2 Joseph P Kitzmiller3
1College of Public Health, The Ohio State University, 2Center for Integrative Health and Wellness, The Ohio State Wexner University Medical Center, 3Department of Biological Chemistry and Pharmacology, College of Medicine, The Ohio State University, Columbus, OH, USA
Abstract: Over recent decades, the demand for complementary and alternative medicine (CAM) has continued to rise in the US. Like the practice of traditional Western medicine, CAM is associated with not only significant health benefits but also significant risks. Unlike traditional Western medicine, however, much of CAM use is less regulated and often occurs unbeknownst to a patient’s medical doctor. The use of herbals, dietary supplements, and over-the-counter (OTC) medications can result in adverse effects, and many significant interactions can occur when their use is combined with allopathic medications. Even the more peripheral CAM practices (eg, acupuncture, massage, yoga, and Reiki) have associated risk (eg, adverse effects or worsening of physical injury and conditions). There is, however, impetus for change: both patients and physicians favor increasing physician knowledge of CAM and the synergistic implementation of CAM into routine clinical practice. Although improvement has been achieved from contemporary physician educational efforts, recently published results from patient and physician surveys strongly indicate that additional effort to increase physician knowledge of CAM is needed. Utilizing a 37-item survey and convenience-sampling methodology, we collected detailed information from 114 physicians, fellows, and residents from the Ohio State University Medical Center regarding impediments to increasing physician knowledge of CAM and its implementation in routine clinical practice. The aggregate results of our survey data showed that most physicians 1) desired to increase their knowledge of CAM, 2) believed that less than half of their patients were spontaneously reporting their use of CAM therapies, 3) were not aware of available evidence-based resources on CAM, 4) preferred case-based lectures for learning about CAM, and 5) reported insufficient time during patient encounters as the primary barrier for increasing the implementation of CAM in routine clinical practice.
Keywords: attitudes, integrative medicine, survey, holistic medicine, clinical practice
A Letter to the Editor has been received and published for this article.
Introduction
Nearly half of the adult patients in the US use complementary and alternative medicine (CAM) therapies to treat medical conditions or to improve their overall well-being, and current trends suggest that interest is growing.1–4 Despite this, ~80% do not discuss their CAM use with their physician.5–7 Lack of physician–patient communication regarding CAM can be tremendously problematic, resulting in forgone opportunities to discuss potential interactions between pharmaceuticals and CAM therapies, misattribution of therapeutic benefits or side effects, and a reduced capacity of physicians to function in a truly integrative capacity.5,7–9 Patient perception that physicians lack interest in CAM has commonly been cited as a reason for patients’ nondisclosure, and limited education and training regarding CAM likely contributes to limited physician–patient dialogue regarding CAM.1,6,10–13 Although leaders of the medical community have called on physicians to routinely include dialogue about CAM in their patient encounters (eg, reconciliation of all medications, including dietary supplements such as vitamins, minerals, and herbal products, is required at each patient encounter per the Joint Commission for the Accreditation for Hospitals [JCAHO]) and a growing number of academic medical centers in the US have renewed efforts to bolster training and education of CAM, evidence of their impact remains scant.1,9,13–16
At The Ohio State University Medical Center (OSUMC), traditional (lectures, workshops, and conferences) and contemporary (online databases and interactive websites) modes of education have been developed to educate physicians, medical staff, and trainees about CAM.9 An undergraduate Minor in Integrative Health program was established in OSU’s College of Medicine in 2006; a Medical Student Interest Group in Integrative Medicine was launched in 2012; an elective in Integrative Medicine for residents of Family Medicine and a special collection of integrative medicine resources in the University’s Health Sciences Library were made available starting in 2013; and online training in mind–body skills, as well as herbs and dietary supplements, has been available since 2014.9 Most of the CAM education and training initiatives, however, have been provided on an elective basis, and the subsequent benefits remain unknown. The physician survey we developed for this short report was designed to collect detailed information from physicians regarding their perspectives on education, training, and implementation of CAM. Resulting observations may play a vital role in informing curriculum development and evaluation efforts at our medical center and elsewhere.
Methods
For this study, we developed an online anonymous survey designed to collect detailed information from attending, fellow, and resident physicians at the OSUMC regarding their attitudes on CAM, their patient–physician dialogue regarding CAM, and their perceived impediments to increasing their knowledge of CAM and implementing it in their routine clinical practice. The 37-item survey and the recruitment and analysis protocols were approved by the institutional review board (IRB) at the Ohio State University (OSU). For purposes of the survey, CAM was defined similar to the definition used by the National Health Interview Survey: dietary supplements (vitamins, minerals, probiotics, herbs, and combinations of these products), acupuncture, massage, homeopathy, meditation, hypnosis, biofeedback, yoga, or systems, such as Traditional Chinese Medicine, shamanism, and Ayurvedic medicine (not including prayer, physical therapy, or therapies provided by psychologists, dietitians, and social workers).5
Recruitment of a convenience sample was achieved during May 2015 and February 2016 via broadly distributed flyer and leaflet advertisements, and email invitations were routinely sent to OSUMC physicians, fellows, and residents. Participants provided informed consent to participate by clicking on a link (“Take Me to the Survey”) embedded in the survey invitation email. As approved by the OSU IRB, the link was clearly labeled to indicate that informed consent to participate was acknowledged by clicking the link. Survey participants were provided a US$20 Amazon gift card to compensate them for their time (estimated to be 10–15 minutes). Secondary to the limited financial support for this project, the survey was concluded after 114 physicians participated. Their survey responses were collected and deidentified using Research Electronic Data Capture (REDCap), a secure web-based application for building and managing online surveys and databases.17 The counts and percentages for each survey item were determined and tabulated.
Results
Examination of the aggregate demographic data (Table 1) showed that most physician participants were <50 years of age, most were Caucasian, most practiced medicine as a specialist (eg, emergency medicine, cardiology, dermatology, internal medicine, neurology, pulmonary and critical care medicine, psychiatry, and surgical specialties), and about half were male.
  | Table 1 Demographics of physician survey participants |
Examination of the aggregate survey responses regarding physician–patient dialogue and patient use of CAM (Table 2) found disparity between the perceived frequency of CAM use and the perceived frequency of patients’ reporting of their CAM use. The highest percentage (42%) of physicians believed that 20%–40% of their patients use some form of CAM therapy, while the highest percentage (67%) of physicians believed that <20% of their patients spontaneously reported their CAM use without prompting or direct questioning. Furthermore, disparity between the perceived importance and the reported occurrence of physicians querying about CAM use was also found. Although the majority of physicians acknowledged (56% agreed and 31% strongly agreed) that physicians should routinely ask their patients about CAM use, the highest percentage of physicians (42%) responded that they directly ask patients about their use of CAM in only 0%–20% of their routine visits.
  | Table 2 Survey items regarding physician–patient dialogue and patient use of CAM Note: Values presented as n (%). Abbreviation: CAM, complementary and alternative medicine. |
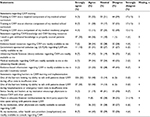
Several observations were made from the aggregate analyses of survey responses regarding CAM training, learning resources, and perceived barriers (Table 3). Accordingly, 25% reported that “CAM was required” and 35% reported “elective learning about CAM” during medical school, and only 15% reported having learned about CAM during residency training. Fewer than half were familiar with evidence-based resources on CAM in the medical journals they routinely consulted, on the Internet, or in the textbook resources available at our medical center’s health sciences library. In addition to lack of training and limited awareness of CAM resources, physicians reported several additional barriers to talking with their patients about CAM. More than 80% perceived that insufficient time was a barrier, and only 8% reported that lack of third party reimbursement was problematic. Other perceived barriers included lack of availability of physicians and nonphysicians for CAM consultation. Furthermore, 33% disagreed that other physicians at their institution were available to consult regarding CAM, and 24% disagreed that other health care providers (nonphysicians) at their institution were readily available to consult regarding CAM. Only 22% physicians reported that senior faculty and administrative leaders encouraged CAM physician–patient dialogue, and significant numbers had positive preferences for case-based lectures (58%), experiential workshops (55%), and case-based interactive online curricula or webinars (48%) for increasing their knowledge of CAM.
Although most physicians (87%) acknowledged that CAM use is common among their patients and that querying patients about CAM is important, many (42%) reported that they inquire about CAM use at <20% of their patient encounters. This highlights the need for strategies aimed at increasing and improving patient–physician dialogue and reconciliation of CAM therapies.
Physician perspectives reflecting a need for increased knowledge of CAM have been reported,1 and the majority of physicians in this study favored increasing their knowledge of CAM. We also observed a stark disconnect regarding physician’s familiarity with the evidenced-based CAM resources readily available to them. Some degree of unfamiliarity was expected, but the severity of the disconnect uncovered in our analysis was substantial. This highlights another significant impetus for change and another opportunity for interventions focused on increasing awareness of CAM and increasing the awareness and utilization of CAM knowledge and learning resources. As Internet-based resources and case-based interactive learning were preferred by the physicians in this study, they should be strongly emphasized in future CAM education and training efforts.
The relatively low number of participants in this study was a limitation. As the awarded budget allowed for only 114 participants, the use of convenience sampling methodology was necessitated. As the conditions of random sampling were not feasible, bias may have been introduced in that physicians who chose to participate may have had different experiences, interests, or attitudes regarding CAM compared to those who chose not to seek participation. Furthermore, our findings may be limited in that thousands of physicians are employed at the OSUMC and we surveyed only 114. Although convenience sampling has significant limitations (eg, biases and lower generalizability), the survey data collected in this study provide important insights that can inform future studies as well as CAM education and training efforts. Future studies should aim to utilize random sampling and include a larger sample size. Participants’ current level of practice (resident, fellow, or attending) was not acquired in our survey. This represents an important limitation of our report as survey responses may likely have been related to the participant’s temporal proximity to medical school or postgraduate training.
As increased efforts focused on the inclusion of CAM education and training in medical school, residency, and physician continuing medical education programs are warranted, support from institutions (eg, academic medical centers and hospitals), governing bodies (eg, US Food and Drug Administration [FDA]), and leading professional organizations (eg, American Medical Association) is also paramount. Along with examining whether the role (resident, fellow, or attending) or number of years out of training has any influence, designs of future studies should examine also whether physicians’ specialty or whether their practice as part of an interdisciplinary team has influence on their perspectives of CAM.
Conclusion
Patient demand for the inclusion of medicine and integrative medicine approaches to health care that are more precise is increasing in the US and other developed countries, resulting in increased need for CAM education, training, and resources for physicians and other health care providers. Physicians acknowledge the importance of acquiring knowledge and training of CAM, and this short report provides meaningful insight regarding physician perspectives on education, training, and implementation of CAM.
Acknowledgments
The authors thank the physicians who participated in this survey. They also thank The Center for Integrative Health and Wellness at The Ohio State University Medical Center for providing a research award to fund implementation of the physician survey.
Disclosure
The authors report no conflicts of interest in this work.
References
Maha N, Shaw A. Academic doctors’ views of complementary and alternative medicine (CAM) and its role within the NHS: an exploratory qualitative study. BMC Complement Altern Med. 2007;7:17. | ||
Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Report. 2015;(79):1–16. | ||
Nahin RL, Barnes PM, Stussman BJ, Bloom B. Costs of complementary and alternative medicine (CAM) and frequency of visits to CAM practitioners: United States, 2007. Natl Health Stat Report. 2009;(18):1–14. | ||
Kemper KJ, Vohra S, Walls R; Task Force on Complementary and Alternative Medicine; Provisional Section on Complementary, Holistic, and Integrative Medicine. American Academy of Pediatrics. The use of complementary and alternative medicine in pediatrics. Pediatrics. 2008;122(6):1374–1386. | ||
Chao MT, Wade C, Kronenberg F. Disclosure of complementary and alternative medicine to conventional medical providers: variation by race/ethnicity and type of CAM. J Natl Med Assoc. 2008;100(11):1341–1349. | ||
Davis EL, Oh B, Butow PN, Mullan BA, Clarke S. Cancer patient disclosure and patient-doctor communication of complementary and alternative medicine use: a systematic review. Oncologist. 2012;17(11):1475–1481. | ||
Robinson A, McGrail MR. Disclosure of CAM use to medical practitioners: a review of qualitative and quantitative studies. Complement Ther Med. 2004;12(2–3):90–98. | ||
McCune JS, Hatfield AJ, Blackburn AA, Leith PO, Livingston RB, Ellis GK. Potential of chemotherapy-herb interactions in adult cancer patients. Support Care Cancer. 2004;12(6):454–462. | ||
The Ohio State University Medical Center [webpage on the Internet]. Integrative Medicine Education. Available from: https://wexnermedical.osu.edu/integrative-complementary-medicine/education. Accessed April 1, 2017. | ||
Sidora-Arcoleo K, Yoos HL, Kitzman H, McMullen A, Anson E. Don’t ask, don’t tell: parental nondisclosure of complementary and alternative medicine and over-the-counter medication use in children’s asthma management. J Pediatr Health Care. 2008;22(4):221–229. | ||
Tasaki K, Maskarinec G, Shumay DM, Tatsumura Y, Kakai H. Communication between physicians and cancer patients about complementary and alternative medicine: exploring patients’ perspectives. Psychooncology. 2002;11(3):212–220. | ||
Owen D, Lewith GT. Teaching integrated care: CAM familiarization courses. Med J Aust. 2004;181(5):276–278. | ||
The Joint Commission [homepage on the Internet]. Using medication reconciliation to prevent errors. Available from: http://www.ihi.org/resources/Pages/Publications/UsingmedicationreconciliationtopreventerrorsJCAHOSentinelEventAlert35.aspx. Accessed July 4, 2017. | ||
Karpa K. Development and implementation of an herbal and natural product elective in undergraduate medical education. BMC Complement Altern Med. 2012;12:57. | ||
Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1423. | ||
Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301. | ||
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.