Back to Journals » Infection and Drug Resistance » Volume 13
Phenotypic and Genotypic Assessment of Antibiotic Resistance of Staphylococcus aureus Bacteria Isolated from Retail Meat
Authors Torki Baghbaderani Z, Shakerian A, Rahimi E
Received 5 December 2019
Accepted for publication 27 March 2020
Published 7 May 2020 Volume 2020:13 Pages 1339—1349
DOI https://doi.org/10.2147/IDR.S241189
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Joachim Wink
Zeinab Torki Baghbaderani, Amir Shakerian, Ebrahim Rahimi
Department of Food Hygiene and Public Health, Shahrekord Branch, Islamic Azad University, Shahrekord, Iran
Correspondence: Amir Shakerian
Department of Food Hygiene and Public Health, Shahrekord Branch, Islamic Azad University, Shahrekord, Iran
Tel +98 38333361045
Fax +98 3833361031
Email [email protected]
Background: Resistant Staphylococcus aureus (S. aureus) bacteria are determined to be one of the main causes of foodborne diseases.
Purpose: This survey was done to assess the genotypic and phenotypic profiles of antibiotic resistance of S. aureus bacteria isolated from retail meat.
Methods: Four-hundred and eighty-five retail meat samples were collected and examined. S. aureus bacteria were identified using culture and biochemical tests. The phenotypic profile of antibiotic resistance was examined using the disk diffusion method. The genotypic pattern of antibiotic resistance was determined using the polymerase chain reaction.
Results: Forty-eight out of 485 (9.89%) raw retail meat samples were contaminated with S. aureus. Raw retail buffalo meat (16%) had the highest incidence of S. aureus, while raw camel meat (4%) had the lowest. S. aureus bacteria exhibited the uppermost incidence of resistance toward tetracycline (79.16%), penicillin (72.91%), gentamicin (60.41%), and doxycycline (41.666%). The incidence of resistance toward chloramphenicol (8.33%), levofloxacin (22.91%), rifampin (22.91%), and azithromycin (25%) was lower than other examined antibiotics. The most routinely detected antibiotic resistance genes were blaZ (58.33%), tetK (52.08%), aacA-D (33.33%), and ermA (27.08%). Cat1 (4.16%), rpoB (10.41%), msrA (12.50%), grlA (12.50%), linA (14.58%), and dfrA1 (16.66%) had the lower incidence rate.
Conclusion: Raw meat of animals may be sources of resistant S. aureus which pose a hygienic threat about the consumption of raw meat. Nevertheless, further investigations are essential to understand supplementary epidemiological features of S. aureus in retail meat.
Keywords: Staphylococcus aureus, incidence, antibiotic resistance pattern, antibiotic resistance genes, retail meat
Introduction
Meat is a nutrient foodstuff with highly beneficial effects on human health. It is a rich source of protein, fat, and some kinds of vitamins essential for a healthy life.1–5 Nevertheless, considering the low hygienic conditions of slaughterhouses, numerous outbreaks of foodborne diseases owing to the consumption of contaminated raw or undercooked meat have been reported in diverse parts of the world.1–5
Staphylococcus aureus (S. aureus), a Gram-positive and catalase-positive bacterium, is considered a substantial cause of foodborne diseases identified by a short incubation period, weakness, vomiting, nausea, abdominal cramps, and toxic shock syndrome.6 Raw or undercooked foodstuffs, particularly foods with animal origins, are determined as reservoirs of S. aureus.7
The bacterium has an emergence of resistance toward diverse kinds of antibiotic agents.8 Resistant S. aureus bacteria are responsible for about 100,000 cases of infectious diseases with about 20–30% mortality per annum in the United States.9 Resistant S. aureus bacteria caused more complicated diseases for a longer period of time.10 They are responsible for higher costs of control and treatment.10 Furthermore, a high incidence of resistance toward diverse kinds of antibiotics, particularly penicillins, cephalosporins, tetracyclines, aminoglycosides, macrolides, and fluoroquinolones, has been reported for S. aureus bacteria isolated from foods with animal origin.8,11
The phenotypic presence of antibiotic resistance of S. aureus bacteria is mostly associated with the presence of antibiotic resistance genes.12 A high presence of tetK and tetM, ermA and msrA, gyrA and grlA, blaZ, dfrA, rpoB, aacA-D, linA, and cat1 antibiotic resistance genes in the S. aureus bacteria caused the occurrence of resistance against tetracyclines, macrolides, fluoroquinolones, penicillins, folate inhibitors, ansamycins, aminoglycosides, lincosamides, and phenicols, respectively.12
Considering the high consumption rate of meat, the high importance of S. aureus, and unknown microbial and epidemiological aspects of the bacterium in raw meat samples, an existing survey was carried out to assess the incidence and the phenotypic and genotypic patterns of antibiotic resistance of S. aureus bacteria isolated from diverse kinds of raw retail meat samples.
Materials and Methods
Ethical Consideration
The survey was confirmed by the Ethical Council of Research of the Department of Food Hygiene, Shahrekord Branch, Islamic Azad University, Shahrekord, Iran.
Samples
From May to October 2018, a total of 485 numerous kinds of raw meat samples including camel (n=100), buffalo (n=100), sheep (n= 85), beef (n=100), and goat (n=100) were randomly collected from 65 different retail centers of Isfahan province, Iran. Samples (100 g, femur muscle) were directly transferred to the Food Hygiene Research Center. Transmission was carried out by cool boxes.
Isolation and Identification of S. aureus
Twenty-five grams of each collected meat sample were blended with 225 mL of buffered peptone water (Merck, Germany). At that time, solutions were homogenized using Stomacher (Interscience, Saint-Nom, France). Then, 5 mL of the achieved solution was transferred into 50 mL Trypticase Soy Broth (TSB; Merck, Germany) supplemented with 10% NaCl and 1% sodium pyruvate, and incubated for 18 h at 35 °C. Then, a loopful of the culture was transferred into Baird-Parker agar supplemented with egg yolk tellurite emulsion (Merck, Germany) and incubated at 37 °C for about 24 h.5,7 Black shiny colonies surrounded by 2 to 5-mm clear zones were further identified on the basis of Gram staining, hemolytic activity on sheep blood agar (Merck, Germany), catalase activity, coagulated test (rabbit plasma), oxidase test, glucose O/F test, resistance to bacitracin (0.04 U), mannitol fermentation on Mannitol salt agar (Merck, Germany), urease activity, nitrate reduction, phosphatase, deoxyribonuclease (DNase; Merck, Germany) test, Voges–Proskauer (Merck, Germany) test, and carbohydrate (xylose, sucrose, trehalose and maltose, fructose, lactose, mannose) fermentation tests.8,13
Phenotypic Assessment of Antibiotic Resistance
The phenotypic pattern of antibiotic resistance of S. aureus bacteria was investigated using the disk diffusion method on Mueller–Hinton agar (Merck, Germany).13 Principles of the Clinical Laboratory Standard Institute (CLSI) were used for this purpose.14 Diverse kinds of antibiotic agents including aminoglycosides (amikacin (30 µg/disk) and gentamicin (10 µg/disk)), fluoroquinolones (levofloxacin (5 µg/disk) and ciprofloxacin (5 µg/disk)), lincosamides (clindamycin (2 µg/disk)), macrolides (erythromycin (15 µg/disk) and azithromycin (15 µg/disk)), penicillins (penicillin (10 µg/disk)), tetracyclines (doxycycline (30 µg/disk) and tetracycline (30 µg/disk)), phenicols (chloramphenicol (30 µg/disk)), folate pathway inhibitors (trimethoprim–sulfamethoxazole (25 µg/disk)), and ansamycins (rifampin (5 µg/disk)) were used for this goal (Oxoid, UK). The method was completed using the protocol characterized previously.14 S. aureus (ATCC 43300 and ATCC 29213) was used as the quality control organism in antimicrobial susceptibility determination.
Genotypic Assessment of Antibiotic Resistance
S. aureus isolates were subcultured on TSB media (Merck, Germany) and further incubated for 48 h at 37 °C. Genomic DNA was extracted from the bacterial colonies using the DNA extraction kit (Thermo Fisher Scientific, St. Leon-Rot, Germany) according to the manufacturer’s instructions. The purity (A260/A280) and concentration of extracted DNA were then checked (NanoDrop; Thermo Scientific, Waltham, MA, USA). The quality of extracted DNA was assessed using electrophoresis of DNA on a 2% agarose gel stained with ethidium bromide (0.5 μg/mL) (Thermo Fisher Scientific, St. Leon-Rot, Germany).
Table 1 presents the polymerase chain reaction (PCR) protocol used for genotypic assessment of antibiotic resistance.15–21 A programmable DNA thermo-cycler (Eppendorf Mastercycler 5330; Eppendorf-Netheler-Hinz GmbH, Hamburg, Germany) was used in all PCRs. Amplified samples were analyzed by electrophoresis (120 V/208 mA) in 2.5% agarose gel. The gel was stained with 0.1% ethidium bromide (0.4 µg/mL). The UVI doc gel documentation system (Grade GB004; Jencons PLC, London, UK) was applied for analysis of images.
 |
Table 1 PCR Protocol Used for Genotypic Assessment of Antibiotic Resistance |
Statistical Analysis
Statistical analysis was done using SPSS 21.0 statistical software (SPSS Inc., Chicago, IL, USA). The chi-square test and Fisher’s exact two-tailed test were used to assess any significant relationship between the prevalence of S. aureus and the phenotypic and genotypic properties of antibiotic resistance. P value <0.05 was considered a statistically significant level.
Results
Table 2 shows the incidence of S. aureus in diverse kinds of raw retail meat samples. Forty-eight out of 485 (9.89%) raw retail meat samples were contaminated with S. aureus bacteria. Raw retail camel meat (4%) had the lowest incidence of S. aureus, while raw retail buffalo meat (16%) had the highest. A statistically significant difference was found between types of retail meat samples and incidence of S. aureus (P<0.05).
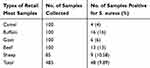 |
Table 2 Incidence of S. aureus in Diverse Kinds of Retail Meat Samples |
Table 3 shows the phenotypic profile of antibiotic resistance of S. aureus bacteria isolated from diverse kinds of retail meat samples. S. aureus bacteria disclosed the highest incidence of resistance toward tetracycline (79.16%), penicillin (72.91%), gentamicin (60.41%), and doxycycline (41.66%) antibiotic agents. Lower incidence of resistance was obtained toward chloramphenicol (8.33%), levofloxacin (22.91%), rifampin (22.91%), and azithromycin (25%) antibiotic agents. A statistically significant difference was found between types of raw retail meat samples and incidence of antibiotic resistance (P<0.05). Moreover, a statistically significant difference was found for the incidence of resistance between gentamicin and amikacin (P<0.05), azithromycin and erythromycin (P<0.05), tetracycline and doxycycline (P<0.05), and ciprofloxacin and levofloxacin (P<0.05) antibiotic agents.
 |
Table 3 Phenotypic Profile of Antibiotic Resistance of S. aureus Isolates Recovered from Diverse Kinds of Retail Meat Samples |
Table 4 shows the genotypic profile of antibiotic resistance of S. aureus bacteria isolated from diverse kinds of retail meat samples. BlaZ (58.33%), tetK (52.08%), aacA-D (33.33%), and ermA (27.08%) were the most commonly recognized antibiotic resistance genes amongst the S. aureus isolates. Incidences of cat1 (4.16%), rpoB (10.41%), msrA (12.50%), grlA (12.50%), linA (14.58%), and dfrA1 (16.66%) were lower than other detected antibiotic resistance genes. A statistically significant difference was found between types of raw retail meat samples and the incidence of antibiotic resistance genes (P<0.05). Furthermore, a statistically significant difference was found between the incidence of tetK and tetM (P<0.05), msrA and ermA (P<0.05), and gyrA and grlA (P<0.05) antibiotic resistance genes.
 |
Table 4 Genotypic Profile of Antibiotic Resistance of S. aureus Isolates Recovered from Diverse Kinds of Retail Meat Samples |
Discussion
S. aureus, a pathogen involved in severe gastrointestinal disorders and foodborne diseases, has an emergence of antibiotic resistance. Contaminated meat of animal species is considered one of the likely causes of transmission of antibiotic-resistant S. aureus to the human population.22
An existing survey addressed the incidence rate and phenotypic and genotypic profiles of antibiotic resistance of S. aureus bacteria recovered from raw beef, sheep, goat, camel, and buffalo retail meat samples. The incidence of S. aureus in the examined samples was 9.89%. The higher incidence rate was found in buffalo meat samples (16%), while the lower was found in camel meat samples (4%). This finding is possibly owing to the different diet of diverse animal species which may affect the incidence of bacteria. Furthermore, higher manipulation of buffalo carcasses by contaminated veterinarians through inspection in the slaughterhouse is another imperative risk factor for contamination. Moreover, the low number of camel slaughtering which can reduce the risk of cross-contamination may be another reason for the low incidence of S. aureus in camel retail meat. Foodstuff contamination with S. aureus may occur straight from infected food-producing animals (or their products such as meat) or may result from poor hygiene throughout production processes, or the retail and storage of food, since humans may also harbor microorganisms. Diverse surveys have been conducted in this field in Japan,23 Korea,24 Italy,25 and the Netherlands.26 The incidence of S. aureus bacteria in raw retail meat samples collected from Brazil,27 Turkey,28 Egypt,29 Germany,30 and Denmark31 was 21.72%, 30%, 40.80%, 71.50%, and 52.00%, respectively, which all were much higher than our findings. Additionally, the role of raw retail meat as a reservoir of S. aureus bacteria has been reported in surveys performed in Australia,32 the United Kingdom,33 and the United States.34 Hasanpour Dehkordi et al8 conveyed that the incidence of S. aureus bacteria in raw retail beef, sheep, goat, and camel meat samples was 16.00%, 24.00%, 20.40%, and 10.00%, respectively. Table 5 summarizes the isolation rate of S. aureus in different types of meat samples obtained from previous research.35–48
 |
Table 5 Summarizing the Isolation Rate of S. aureus in Different Types of Meat Samples Obtained from Previous Research |
The contamination rate of raw meat samples with S. aureus varies between diverse research studies. The difference in data advises that the time, season, place of sampling, method of sampling, types of samples, and even laboratory techniques applied in research may affect the outcomes of surveys. Moreover, different hygienic levels of butchers and retail centers may affect the incidence of bacteria in diverse investigations. Otherwise, the sample sizes, sample types, and geographic locations of research may be the reason for these differences. Compared to the results of other scientists, the comparatively low rate of S. aureus isolation was reported in our survey. This is expected because in fresh meat S. aureus is not a good competitor with normal microflora. The reasons for this finding are not clear, but since antibiotic prescription is higher than required, a lower incidence of S. aureus is possible.
Our survey also disclosed considerable incidence of resistance toward diverse groups of antibiotics, particularly aminoglycosides, fluoroquinolones, lincosamides, macrolides, penicillins, tetracyclines, phenicols, folate pathway inhibitors, and ansamycins, which was accompanied with the presence of aacA-D, gyrA and grlA, linA, msrA and ermA, blaZ, tetK and tetM, cat1, dfrA1, and rpoB antibiotic resistance genes, respectively. Thus, the phenotypic pattern of antibiotic resistance of S. aureus bacteria was confirmed by the genotypic profile. Furthermore, our outcomes disclosed that some S. aureus bacteria exhibited higher incidence of resistance toward antibiotics used for human beings which can indirectly signify their anthropogenic source. Reversely, some others exhibited higher incidence of resistance toward antibiotics used for animal beings which can indirectly demonstrate their animal origins. Similar resistance profiles of S. aureus bacteria isolated from dissimilar kinds of foodstuffs and clinical specimens have also been determined toward aminoglycosides,5,13,49-52 cephems,5,13,49–51 penicillins,5,13,49–51 macrolides,5,13,49–51 tetracyclines,5,13,49,50 fluoroquinolones,5,13,49–52 lincosamides,5,13,49–51 folate inhibitors,5,13,49–52 phenicols,5,13,49 and ansamycins5,13,49,50. Momtaz et al5 reported that the S. aureus strains with meat origins harbored the highest prevalence of resistance against tetracycline (97.50%), methicillin (75.60%), sulfamethoxazole (31.70%), trimethoprim (31.70%), streptomycin (31.70%), gentamicin (29.20%), enrofloxacin (28.00%), ampicillin (26.8%), chloramphenicol (20.70%), and cephalothin (17.00%) antibiotic agents. Hasanpour Dehkordi et al8 determined that S. aureus bacteria isolated from raw meat samples had a high incidence of resistance toward ampicillin (100%), ceftriaxone (80.00%), amoxicillin–clavulanic acid (50.00%), lincomycin (61.20%), tetracycline (55.00%), gatifloxacin (96.80%), minocycline (51.20%), cotrimoxazole (45.60%), clindamycin (54.30%), azithromycin (48.10%), erythromycin (37.50%), oxacillin (76.20%), and penicillin (100%) antibiotic agents. Fowoyo and Ogunbanwo53 disclosed that the S. aureus bacteria recovered from ready to eat foodstuffs exhibited a high incidence of resistance toward trimethoprim–sulfamethoxazole (74.90%), ampicillin (86.70%), cefotaxime (3.50%), amoxicillin–clavulanic acid (52.50%), ciprofloxacin (23.90%), oxacillin (35.70%), gentamicin (11.40%), erythromycin (15.70%), and ofloxacin (7.10%). The high incidence of resistance toward chloramphenicol (8.33%) may be due to its unlawful and unselective prescription especially in veterinary medicine. Akanbi et al54 reported that blaZ, mecA, rpoB, ermB, and tetM were the most commonly identified antibiotic resistance genes amongst the S. aureus bacteria recovered from food samples in South Africa. High distribution of mecA, gyrA, grlA, and cfr genes was also described in the S. aureus bacteria recovered from chicken meat in Egypt.55 Another Iranian survey56 disclosed that oxacillin-, gentamicin-, penicillin-, tetracycline-, and erythromycin-resistant S. aureus bacteria isolated from milk and dairy products harbored high incidence of blaZ, aacA-aphD, mecA, tetK and tetM, ermB, ermA, ermT, ermC, msrB, and msrA antibiotic resistance markers likewise to our survey. A similar phenotypic profile of antibiotic resistance was also reported from Iran57 and China.58 Differences in the opinion of medical and veterinary practitioners in antibiotic prescription, observation of ethics and rules in the use of antibiotics, availability or lack of antibiotics, and their prices are probable reasons for differences found in the incidence of resistance of S. aureus strains in numerous investigations. In a survey which was conducted by Bantawa et al,59 S. aureus bacteria isolated from buffalo, chicken, pork, and goat meat samples in eastern Nepal harbored a high incidence of resistance (10–100%) against amoxicillin, tetracycline, cefotaxime, and nalidixic acid.
Our findings also disclosed higher incidence of a phenotypic profile of resistance than a genotypic profile. For example, all of the penicillin-resistant S. aureus bacteria did not harbor blaZ antibiotic resistance genes. This matter also existed for other antibiotic agents and resistance genes. This finding may be owing to the fact that the presence of antibiotic resistance genes is one of the known procedures for the occurrence of antibiotic resistance in bacteria. On the other hand, several mechanisms have been identified to induce antibiotic resistance in bacteria including reduced permeability of bacteria to antibiotics, efflux antibiotic active pumps out of the bacterial cell, change in antibiotic target site, inactivation of antibiotics through hydrolysis or changes in their structure, occurrence of genetic mutations, and access of bacteria to the secondary metabolic pathways that compensate the antibiotic-inhibited reactions.
Conclusion
In conclusion, a high incidence of S. aureus in examined samples, particularly raw retail buffalo and beef meat samples, was accompanied with a high incidence of resistance toward diverse classes of antibiotic agents and also dissimilar antibiotic resistance genes. An existing survey is an initial report of the genotypic evaluation of antibiotic resistance of the S. aureus bacteria isolated from raw retail buffalo and camel meat samples. High incidence of resistance of S. aureus bacteria toward tetracycline, penicillin, gentamicin, and doxycycline antibiotic agents and also high frequency of blaZ, tetK, aacA-D, and ermA antibiotic resistance genes may pose an imperative menace regarding the role of raw or undercooked meat consumption on the transmission of antibiotic-resistant S. aureus. Incidence of resistance toward human-based and also animal-based antibiotics can indirectly show the origin of S. aureus isolates. It seems that tetracycline, penicillin, gentamicin, and doxycycline are not effective therapeutic agents in the cases of S. aureus foodborne diseases in Iran. Slaughterhouses can be severely contaminated with foodborne pathogens,46–49 so the maintenance of slaughter hygiene, regular microbiological monitoring of carcasses, implementation of good manufacturing practices, and a food safety system such as the HACCP system are essential to minimize the risk to the consumer. Additionally, appropriate cooking of raw meat before consumption, prevention from cross-contamination, and antibiotic prescription based on the outcomes of disk diffusion can diminish the risk of transmission of resistant S. aureus bacteria from meat to the human population. However, supplementary surveys are essential to determine more epidemiological features of the S. aureus bacteria in raw retail meat of animal species. Our research highlights the importance of controlling the antibiotic susceptibility of S. aureus in foodstuffs such as food-producing animals, retail foods, and even human beings, and this information could be used proactively to assist Iranian industries to progress better-quality food safety measures. Otherwise, on the basis of these observations, we recommend that attention should be paid by governments and individuals to prevent the further spread of antibiotic-resistant S. aureus.
Acknowledgments
The authors thank Prof. Mohsen Jafarian and Prof. Hassan Momtaz for their imperative provisions. An existing survey was monetarily buoyed by the Islamic Azad University, Shahrekord Branch, Shahrekord, Iran.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hemmatinezhad B, Khamesipour F, Mohammadi M, Safarpoor Dehkordi F, Mashak Z. Microbiological investigation of o‐serogroups, virulence factors and antimicrobial resistance properties of shiga toxin‐producing Escherichia coli isolated from ostrich, turkey and quail meats. J Food Saf. 2015;35(4):491–500. doi:10.1111/jfs.12199
2. Momtaz H, Davood Rahimian M, Safarpoor Dehkordi F. Identification and characterization of Yersinia enterocolitica isolated from raw chicken meat based on molecular and biological techniques. J App Poultry Res. 2013;22(1):137–145. doi:10.3382/japr.2012-00549
3. Momtaz H, Dehkordi FS, Rahimi E, Ezadi H, Arab R. Incidence of Shiga toxin-producing Escherichia coli serogroups in ruminant’s meat. Meat Sci. 2013;95(2):381–388. doi:10.1016/j.meatsci.2013.04.051
4. Rahimi E, Yazdanpour S, Dehkordi F. Detection of Toxoplasma gondii antibodies in various poultry meat samples using enzyme linked immuno sorbent assay and its confirmation by polymerase chain reaction. J Pure Appl Microbiol. 2014;8(1):421–427.
5. Momtaz H, Dehkordi FS, Rahimi E, Asgarifar A, Momeni M. Virulence genes and antimicrobial resistance profiles of Staphylococcus aureus isolated from chicken meat in Isfahan province, Iran. J App Poultry Res. 2013;22(4):913–921. doi:10.3382/japr.2012-00673
6. Wang L, Ruan S. Modeling nosocomial infections of methicillin-resistant Staphylococcus aureus with environment contamination. Sci Rep. 2017;7(1):580. doi:10.1038/s41598-017-00261-1
7. Fijałkowski K, Peitler D, Karakulska J. Staphylococci isolated from ready-to-eat meat–identification, antibiotic resistance and toxin gene profile. Int J Food Microbiol. 2016;238:113–120. doi:10.1016/j.ijfoodmicro.2016.09.001
8. Hasanpour Dehkordi A, Khaji L, Sakhaei Shahreza M, et al. One-year prevalence of antimicrobial susceptibility pattern of methicillin-resistant Staphylococcus aureus recovered from raw meat. Tropical Biomed. 2017;34(2):396–404.
9. Klevens RM, Morrison MA, Nadle J, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298(15):1763–1771. doi:10.1001/jama.298.15.1763
10. Li B, Webster TJ. Bacteria antibiotic resistance: new challenges and opportunities for implant‐associated orthopedic infections. J Orthopaed Res. 2018;36(1):22–32.
11. Madahi H, Rostami F, Rahimi E, Dehkordi FS. Prevalence of enterotoxigenic Staphylococcus aureus isolated from chicken nugget in Iran. Jundishapur J Microbiol. 2014;7(8). doi:10.5812/jjm.10237.
12. Abdolmaleki Z, Mashak Z, Dehkordi FS. Phenotypic and genotypic characterization of antibiotic resistance in the methicillin-resistant Staphylococcus aureus strains isolated from hospital cockroaches. Antimicrob Resist Infect Control. 2019;8(1):54. doi:10.1186/s13756-019-0505-7
13. Dehkordi FS, Gandomi H, Basti AA, Misaghi A, Rahimi E. Phenotypic and genotypic characterization of antibiotic resistance of methicillin-resistant Staphylococcus aureus isolated from hospital food. Antimicrob Resist Infect Control. 2017;6(1):104. doi:10.1186/s13756-017-0257-1
14. CLSI. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fifth Informational Supplement. CLSI document M100-S25. Wayne: Clinical and Laboratory Standards Institute;2015.
15. Lina G, Quaglia A, Reverdy M-E, Leclercq R, Vandenesch F, Etienne J. Distribution of genes encoding resistance to macrolides, lincosamides, and streptogramins among staphylococci. Antimicrob Agent Chemotherap. 1999;43(5):1062–1066. doi:10.1128/AAC.43.5.1062
16. Strommenger B, Kettlitz C, Werner G, Witte W. Multiplex PCR assay for simultaneous detection of nine clinically relevant antibiotic resistance genes in Staphylococcus aureus. J Clin Microbiol. 2003;41(9):4089–4094. doi:10.1128/JCM.41.9.4089-4094.2003
17. Baddour M, AbuElKheir M, Fatani A. Comparison of mecA polymerase chain reaction with phenotypic methods for the detection of methicillin-resistant Staphylococcus aureus. Curr Microbiol. 2007;55(6):473. doi:10.1007/s00284-007-9015-6
18. Van TTH, Chin J, Chapman T, Tran LT, Coloe PJ. Safety of raw meat and shellfish in Vietnam: an analysis of Escherichia coli isolations for antibiotic resistance and virulence genes. Int J Food Microbiol. 2008;124(3):217–223. doi:10.1016/j.ijfoodmicro.2008.03.029
19. Schmitz FJ, Köhrer K, Schering S, et al. The stability of grlA, grlB, gyrA, gyrB and norA mutations and MIC values of five fluoroquinolones in three different clonal populations of methicillin-resistant Staphylococcus aureus. Clin Microbiol Inf. 1999;5(5):287–290. doi:10.1111/j.1469-0691.1999.tb00143.x
20. Shittu AO, Okon K, Adesida S, et al. Antibiotic resistance and molecular epidemiology of Staphylococcus aureus in Nigeria. BMC Microbiol. 2011;11(1):92. doi:10.1186/1471-2180-11-92
21. Aboshkiwa M, Rowland G, Coleman G. Nucleotide sequence of the Staphylococcus aureus RNA polymerase rpoB gene and comparison of its predicted amino acid sequence with those of other bacteria. Biochim Biophys Acta. 1995;1262(1):73–78. doi:10.1016/0167-4781(95)00054-K
22. Fooladvand S, Sarmadian H, Habibi D, et al. High prevalence of methicillin resistant and enterotoxin gene-positive Staphylococcus aureus among nasally colonized food handlers in central Iran. European J Clin Microbiol Infect Dis. 2018;38(1):87–92.
23. Kitai S, Shimizu A, Kawano J, et al. Characterization of methicillin-resistant Staphylococcus aureus isolated from retail raw chicken meat in Japan. J Vet Med Sci. 2005;67(1):107–110. doi:10.1292/jvms.67.107
24. Kwon NH, Park KT, Jung WK, et al. Characteristics of methicillin resistant Staphylococcus aureus isolated from chicken meat and hospitalized dogs in Korea and their epidemiological relatedness. Vet Microbiol. 2006;117(2–4):304–312. doi:10.1016/j.vetmic.2006.05.006
25. Normanno G, Corrente M, La Salandra G, et al. Methicillin-resistant Staphylococcus aureus (MRSA) in foods of animal origin product in Italy. Int J Food Microbiol. 2007;117(2):219–222. doi:10.1016/j.ijfoodmicro.2007.04.006
26. De Boer E, Zwartkruis-Nahuis J, Wit B, et al. Prevalence of methicillin-resistant Staphylococcus aureus in meat. Int J Food Microbiol. 2009;134(1–2):52–56. doi:10.1016/j.ijfoodmicro.2008.12.007
27. Costa WLR, Ferreira J, Carvalho JS, Cerqueira ES, Oliveira LC, Almeida RC. Methicillin-resistant Staphylococcus aureus in raw meats and prepared foods in public hospitals in Salvador, Bahia, Brazil. J Food Sci. 2015;80(1):M147–M50. doi:10.1111/1750-3841.12723
28. Gundogan N, Citak S, Yucel N, Devren A. A note on the incidence and antibiotic resistance of Staphylococcus aureus isolated from meat and chicken samples. Meat Sci. 2005;69(4):807–810. doi:10.1016/j.meatsci.2004.10.011
29. Karmi M. Prevalence of methicillin-resistant Staphylococcus aureus in poultry meat in Qena, Egypt. Vet World. 2013;6(10):711–715. doi:10.14202/vetworld.2013.711-715
30. Richter A, Sting R, Popp C, et al. Prevalence of types of methicillin-resistant Staphylococcus aureus in turkey flocks and personnel attending the animals. Epidemiol Infect. 2012;140(12):2223–2232. doi:10.1017/S095026881200009X
31. Tang Y, Larsen J, Kjeldgaard J, Andersen PS, Skov R, Ingmer H. Methicillin-resistant and -susceptible Staphylococcus aureus from retail meat in Denmark. Int J Food Microbiol. 2017;249:72–76. doi:10.1016/j.ijfoodmicro.2017.03.001
32. Ou Q, Peng Y, Lin D, et al. A meta-analysis of the global prevalence rates of Staphylococcus aureus and methicillin-resistant S. aureus contamination of different raw meat products. J Food Protect. 2017;80(5):763–774. doi:10.4315/0362-028X.JFP-16-355
33. Fox A, Pichon B, Wilkinson H, et al. Detection and molecular characterization of Livestock‐Associated MRSA in raw meat on retail sale in North West England. Letters App Microbiol. 2017;64(3):239–245. doi:10.1111/lam.12709
34. Ge B, Mukherjee S, Hsu C-H, et al. MRSA and multidrug-resistant Staphylococcus aureus in U.S. retail meats, 2010–2011. Food Microbiol. 2017;62:289–297. doi:10.1016/j.fm.2016.10.029
35. Al-Amery K, Elhariri M, Elsayed A, et al. Vancomycin-resistant Staphylococcus aureus isolated from camel meat and slaughterhouse workers in Egypt. Antimicrob Resist Infect Control. 2019;8(1):129. doi:10.1186/s13756-019-0585-4
36. Beyene T, Hayishe H, Gizaw F, et al. Prevalence and antimicrobial resistance profile of Staphylococcus in dairy farms, abattoir and humans in Addis Ababa, Ethiopia. BMC Res Notes. 2017;10(1):171. doi:10.1186/s13104-017-2487-y
37. Kumar A, Kaushik P, Anjay PK, Kumar M. Prevalence of methicillin-resistant Staphylococcus aureus skin and nasal carriage isolates from bovines and its antibiogram. Vet World. 2017;10(6):593–597. doi:10.14202/vetworld.2017.593-597
38. Raji MA, Garaween G, Ehricht R, Monecke S, Shibl AM, Senok A. Genetic characterization of Staphylococcus aureus isolated from retail meat in Riyadh, Saudi Arabia. Front Microbiol. 2016;7:911. doi:10.3389/fmicb.2016.00911
39. El-Ghareeb WR, Almathen FS, Fayez MM, et al. Methicillin resistant Staphylococcus aureus (MRSA) in camel meat: prevalence and antibiotic susceptibility. Slov Vet Res. 2019;56(Suppl 22):249–256.
40. Bhargava K, Wang X, Donabedian S, Zervos M, da Rocha L, Zhang Y. Methicillin-resistant Staphylococcus aureus in retail meat, Detroit, Michigan, USA. Emerg Infect Dis. 2011;17(6):1135–1137. doi:10.3201/eid1706.101905
41. Gwida M, Zakaria A, El-Sherbiny H, Elkenany R, Elsayed M. Prevalence of Campylobacter, Enterococcus and Staphylococcus aureus in slaughtered camels. Vet Med. 2019;64(12):521–530. doi:10.17221/104/2019-VETMED
42. Mahfoozi A, Shirzad-Aski H, Kaboosi H, Ghaemi EA. Identification of the classical enterotoxin genes of Staphylococcus aureus in various foods by multiplex PCR assay. Iran J Vet Res. 2019;20(3):209–212.
43. Naas HT, Edarhoby RA, Garbaj AM, et al. Occurrence, characterization, and antibiogram of Staphylococcus aureus in meat, meat products, and some seafood from Libyan retail markets. Vet World. 2019;12(6):925–931. doi:10.14202/vetworld.2019.925-931
44. Rahimi E, Nonahal F, Salehi EA. Detection of classical enterotoxins of Staphylococcus aureus strains isolated from raw meat in Esfahan, Iran. Health Scope. 2013;2(2):95–98. doi:10.17795/jhealthscope-10651
45. Kitai S, Shimizu A, Kawano J, et al. Prevalence and characterization of Staphylococcus aureus and enterotoxigenic Staphylococcus aureus in retail raw chicken meat throughout Japan. J Vet Med Sci. 2005;67(3):269–274. doi:10.1292/jvms.67.269
46. Yusuf S, Kwaga JKP, Bello M, et al. Occurrence of methicillin-resistant Staphylococcus aureus in camels slaughtered at Kano abattoir, Kano, Nigeria. Int J Vet Sci. 2016;4(1–2):1–14.
47. Wu S, Huang J, Wu Q, et al. Staphylococcus aureus isolated from retail meat and meat products in China: incidence, antibiotic resistance and genetic diversity. Front Microbiol. 2018;9:2767. doi:10.3389/fmicb.2018.02767
48. Guven K, Mutlu MB, Gulbandilar A, Cakir P. Occurrence and characterization of Staphylococcus aureus isolated from meat and dairy products consumed in Turkey. J Food Saf. 2010;30(1):196–212. doi:10.1111/j.1745-4565.2009.00200.x
49. Paludi D, Vergara A, Festino AR, et al. Antimicrobial resistance pattern of methicillin-resistant Staphylococcus aureus in the food industry. J Bio Regulat Homeostat Agent. 2011;25(4):671.
50. Sallam KI, Abd-Elghany SM, Elhadidy M, Tamura T. Molecular characterization and antimicrobial resistance profile of methicillin-resistant Staphylococcus aureus in retail chicken. J Food Protect. 2015;78(10):1879–1884. doi:10.4315/0362-028X.JFP-15-150
51. Jackson CR, Davis JA, Barrett JB. Prevalence and characterization of methicillin-resistant Staphylococcus aureus isolates from retail meat and humans in Georgia. J Clin Microbiol. 2013;51(4):1199–1207. doi:10.1128/JCM.03166-12
52. Daka D, Yihdego D. Antibiotic-resistance Staphylococcus aureus isolated from cow’s milk in the Hawassa area, South Ethiopia. Ann Clinic Microbiol Antimicrob. 2012;11(1):26. doi:10.1186/1476-0711-11-26
53. Fowoyo P, Ogunbanwo S. Antimicrobial resistance in coagulase-negative staphylococci from Nigerian traditional fermented foods. Ann Clinic Microbiol Antimicrob. 2017;16(1):4. doi:10.1186/s12941-017-0181-5
54. Akanbi OE, Njom HA, Fri J, Otigbu AC, Clarke AM. Antimicrobial susceptibility of Staphylococcus aureus isolated from recreational waters and beach sand in Eastern Cape Province of South Africa. Int J Env Res Public Health. 2017;14(9):1001. doi:10.3390/ijerph14091001
55. Osman K, Badr J, Al-Maary KS, et al. Prevalence of the antibiotic resistance genes in coagulase-positive-and negative-staphylococcus in chicken meat retailed to consumers. Front Microbiol. 2016;7:1846. doi:10.3389/fmicb.2016.01846
56. Jamali H, Paydar M, Radmehr B, Ismail S, Dadrasnia A. Prevalence and antimicrobial resistance of Staphylococcus aureus isolated from raw milk and dairy products. Food Control. 2015;54:383–388. doi:10.1016/j.foodcont.2015.02.013
57. Shahraz F, Dadkhah H, Khaksar R, et al. Analysis of antibiotic resistance patterns and detection of mecA gene in Staphylococcus aureus isolated from packaged hamburger. Meat Sci. 2012;90(3):759–763. doi:10.1016/j.meatsci.2011.11.009
58. Rong D, Wu Q, Xu M, Zhang J, Yu S. Prevalence, virulence genes, antimicrobial susceptibility, and genetic diversity of Staphylococcus aureus from retail aquatic products in China. Front Microbiol. 2017;8:714. doi:10.3389/fmicb.2017.00714
59. Bantawa K, Sah SN, Subba Limbu D, Subba P, Ghimire A. Antibiotic resistance patterns of Staphylococcus aureus, Escherichia coli, Salmonella, Shigella and Vibrio isolated from chicken, pork, buffalo and goat meat in eastern Nepal. BMC Res Notes. 2019;12(1):766. doi:10.1186/s13104-019-4798-7
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
