Back to Journals » Clinical Ophthalmology » Volume 17
Phase 3, Randomized Study Comparing Intracameral Bimatoprost Implant 15 μg and Selective Laser Trabeculectomy in Patients with Open-Angle Glaucoma or Ocular Hypertension
Authors Christie WC, Basha MM, Ho Q, Kim K, Craven ER , Kolko M
Received 28 June 2023
Accepted for publication 27 September 2023
Published 12 October 2023 Volume 2023:17 Pages 3023—3036
DOI https://doi.org/10.2147/OPTH.S427976
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
William C Christie,1 Mahdi M Basha,2 Quoc Ho,3 Kimmie Kim,3 E Randy Craven,3 Miriam Kolko4,5
1Scott & Christie Eyecare Associates, Pittsburgh, PA, USA; 2Fraser Eye Care Center, Warren, MI, USA; 3Allergan, an AbbVie company, Irvine, CA, USA; 4Rigshospitalet, Copenhagen University Hospital, Glostrup, Denmark; 5University of Copenhagen, Copenhagen, Denmark
Correspondence: William C Christie, Scott & Christie Eyecare Associates, 105 Brandt Drive Suite 201, Cranberry Township, Pittsburgh, PA, 16066, USA, Tel +1 (724) 772-5420, Email [email protected]
Purpose: We evaluate the safety and intraocular pressure (IOP)-lowering effect of 15-μg bimatoprost implant (higher dose than the currently approved product) compared with selective laser trabeculoplasty (SLT) in patients with open-angle glaucoma or ocular hypertension.
Methods: Randomized, phase 3, 12-month, multicenter, paired-eye, patient- and efficacy evaluator–masked noninferiority study. Patients with inadequate IOP control were randomized to receive 360° SLT (day 1) or up to 3 administrations of 15-μg bimatoprost implant (day 4, weeks 16 and 32) in the primary eye and the alternative treatment in the contralateral eye. The primary endpoint was IOP change from baseline at weeks 4, 12, and 24.
Results: At weeks 4, 12, and 24, mean IOP change from baseline ranged from − 7.01 to − 6.65 mm Hg in implant-treated eyes (N=138) and − 6.45 to − 6.26 mm Hg in SLT-treated eyes (N=138). Differences in IOP change from baseline ranged from − 0.70 to − 0.25 mm Hg favoring implant; the upper limit of the 95% confidence interval of the difference (implant minus SLT) was < 1.0 mm Hg at all 3 visits. The probability of requiring no additional (rescue) IOP-lowering treatment in implant-treated versus SLT-treated eyes was 93.6% versus 86.5% at day 180 and 74.6% versus 77.1% at day 360. Corneal endothelial cell loss was more common in implant-treated eyes and typically occurred after repeated implant administration.
Conclusion: Bimatoprost implant 15 μg met prespecified criteria for statistical and clinical noninferiority to SLT in lowering IOP, and after 1, 2, or 3 administrations, demonstrated a duration of IOP lowering similar to SLT. Bimatoprost implant 15 μg was associated with corneal adverse events in some patients, especially after repeated administrations at a fixed interval, and has been discontinued from development. A lower dose strength of implant (bimatoprost implant 10 μg, Durysta) is US Food and Drug Administration–approved for single administration.
Keywords: clinical trial, drug delivery device, intracameral, paired eye
Introduction
Intraocular pressure (IOP)-lowering eye drops are the standard first-line treatment for open-angle glaucoma (OAG) and ocular hypertension (OHT).1,2 Topical IOP-lowering medications are widely available and generally safe,3,4 and the prostaglandin analog/prostamide (PGA) class of topical IOP-lowering medications, which is most efficacious, is capable of providing substantial (>30%) IOP lowering in patients with elevated IOP.5 However, the use of eye drops to lower IOP has shortcomings, including patient nonadherence to daily treatment,6,7 tolerability issues,3,4,8,9 and the need for multiple clinic visits for treatment monitoring.
Selective laser trabeculoplasty (SLT) is an effective IOP-lowering procedure that eliminates the need for patient adherence to daily treatment and has a good safety profile.10 Studies have shown that IOP lowering is similar with SLT and topical medication,11 and there are data supporting the use of SLT as first-line therapy in OAG and OHT.12–14 Nonetheless, SLT is mainly used as an adjunctive treatment in patients requiring additional IOP-lowering beyond that achieved with eye drops.12 It is commonly understood that it may take 1 to 2 months for the full effect of SLT on IOP to be achieved, and the IOP-lowering effect subsides over time, but the procedure effectively lowers IOP when repeated,15 and a second SLT treatment can be as successful as the initial procedure.10,16
Durysta® (Allergan, an AbbVie company, North Chicago, IL, USA) intracameral implant, consisting of bimatoprost 10 µg in a sustained-release drug delivery system, was approved for single administration by the US Food and Drug Administration in 2020, based on results after the initial implant administration in two 20-month, phase 3, registration trials (ARTEMIS 1 and 2), which used 3 implant administrations at fixed 16-week intervals.17,18 In the ARTEMIS studies, bimatoprost implant 10 µg demonstrated noninferiority to topical timolol in lowering IOP, and the effect on IOP was sustained in most patients for at least a year after the last implant administration.17,18 The incidence of corneal and ocular inflammatory adverse events was higher with the bimatoprost implant than with timolol.17,18 Because of potential corneal endothelial cell loss with repeat treatment, administration is limited to a single implant, without retreatment.
As part of the bimatoprost implant development program, a higher dose strength of the implant (containing 15 µg bimatoprost) was also evaluated for efficacy and safety in the ARTEMIS studies. The higher dose strength (15-µg bimatoprost) implant was evaluated in the present study, which used SLT as the comparator treatment. Bimatoprost implant 10 and 15 µg are both cylindrical implants that are administered intracamerally and settle in the inferior iridocorneal angle,17,19 but bimatoprost 15 µg is 50% longer than bimatoprost 10 µg, and the larger size of the 15-µg implant is associated with increased risk of corneal contact and corneal adverse events.17,18 After three administrations of the 15-µg implant in the ARTEMIS studies, at month 20 the mean loss in central corneal endothelial cell density (CECD) was approximately 22%–24%, and 12%–16% of patients had a ≥20% decrease in CECD from baseline in the study eye.17,18 Bimatoprost implant 15 µg was discontinued from development in 2018 because of a determination that corneal adverse events associated with repeat, fixed-interval administration of the 15-µg dose strength of the bimatoprost implant would not support a favorable benefit:risk consideration.
The objective of this study was to evaluate the IOP-lowering effect and safety of bimatoprost implant 15 µg compared with SLT in patients with OAG or OHT. During the course of the study, the number of administrations of the implant was reduced from 3 to 2, because analysis of data from a completed phase 1/2 study20 and an ongoing phase 3 study suggested that sustained IOP lowering could be achieved with fewer administrations. A later protocol amendment ended study enrollment and discontinued implant administrations to ongoing participants because of the decision to discontinue development of bimatoprost implant 15 µg.
Materials and Methods
Study Design and Adherence to Ethical Standards
This phase 3, multicenter (33 sites in 8 countries—Denmark, France, Poland, Russia, Singapore, Spain, Thailand, and the United States), randomized, patient- and efficacy evaluator–masked, paired-eye, 12-month noninferiority study evaluated the IOP-lowering effect and safety of bimatoprost implant 15 µg compared with SLT in patients with OAG or OHT. The study was conducted from February 24, 2016 to January 26, 2021 in accordance with the International Conference for Harmonisation guidelines, applicable regulations, and the Declaration of Helsinki. An Institutional Review Board or Independent Ethics Committee (listed in Supplementary Materials) approved the study for each clinical site. All patients provided written informed consent before screening. The study is registered at ClinicalTrials.gov with the identifier NCT02636946.
Study Population
Adult patients diagnosed in each eye with OAG or OHT that required IOP-lowering treatment were enrolled. Baseline IOP at 8
Randomization, Intervention, and Visit Schedule
For each enrolled patient, the eye with the higher IOP at baseline (or the right eye, if the IOP was the same in both eyes) was assigned as the primary eye. Primary eyes were randomized 1:1 to treatment with the bimatoprost implant or SLT; the randomization was stratified by baseline IOP in the primary eye (≤25 vs >25 mm Hg) and the difference in baseline IOP between the primary and contralateral eye (0–2 mm Hg vs 3–5 mm Hg). Contralateral eyes received the alternative study treatment (ie, if the primary eye received a bimatoprost implant, the contralateral eye received SLT and vice versa).
On day 1, the eye assigned to SLT received a 360° administration of SLT using standard procedure, and the contralateral eye received a sham procedure for masking. The sham procedure was performed using the same method, with the exception that the laser was not activated. Preparation for the SLT and sham procedures included instillation of apraclonidine or brimonidine and topical anesthetic drops; nonsteroidal anti-inflammatory drops were used for 3 days after the procedures.
The initial study protocol required three administrations of the bimatoprost implant in the implant-treated eye, on day 4, week 16, and week 32. At each implant administration visit, a sham procedure was administered to the contralateral, SLT-treated eye for masking. Eyes were prepared for intraocular injection using standard aseptic procedure. The bimatoprost implant was administered intracamerally using a single-use, prefilled applicator system as described previously.17 In the sham procedure, a needleless applicator was used to touch the cornea.
The study protocol was amended during the study to reduce the number of bimatoprost implant administrations per eye. An amendment in September 2018 discontinued the week 32 administration, changing the number of administrations to 2 (on day 4 and week 16) to allow a longer duration of efficacy follow-up after the second administration. A later amendment in March 2020 ended the enrollment of new participants into the study and prohibited any additional study treatments for ongoing participants, reflecting the decision to discontinue development of the 15-µg dose strength of the bimatoprost implant. Therefore, the eye treated with the bimatoprost implant could have received 1, 2, or 3 implant administrations per protocol in place at the time.
Use of nonstudy (rescue) IOP-lowering treatment in either eye was prohibited unless the investigator determined that it was necessary for the safety of the participant because of inadequate IOP control. Inadequate control of IOP was to be confirmed at a subsequent visit (scheduled or unscheduled visit). Each eye was evaluated on an individual basis when determining the need for nonstudy IOP-lowering treatment; initiation of nonstudy treatment in one eye did not automatically lead to initiation of treatment in the contralateral eye. Use of nonstudy IOP-lowering treatment with a known crossover effect on the contralateral eye was prohibited.
All study participants were followed for the duration of the study through the week 52 exit visit. The schedule of study visits included a minimum of 20 visits and 5 phone calls for participants who received all study treatments. This schedule included screening (up to 28 days with a period for washout of any previous IOP-lowering medication of up to 42 days for both eyes), a baseline visit (up to 3 days), the SLT and bimatoprost implant administration visits, safety visits at 1 day after each bimatoprost implant administration visit, phone calls for safety assessment 1 day after the SLT treatment visit and 3 days and 2 weeks after each bimatoprost implant administration visit, and follow-up study visits with efficacy and safety evaluations at weeks 4, 8, 12, 15, 20, 24, 28, 31, 36, 40, 44, 47, and 52/exit.
Outcome Measures
The primary efficacy measure was IOP. IOP measurements were taken at 8
The primary efficacy endpoint was the change in IOP from baseline at weeks 4, 12, and 24. Secondary efficacy outcome measures included the time from initial treatment to the first use of nonstudy (rescue) IOP-lowering treatment and the percentage of eyes achieving at least a 20% reduction in IOP from baseline at each post-baseline visit.
Analysis
Baseline characteristics of patients and eyes were evaluated in the intent-to-treat (ITT) population of all randomized patients. The primary efficacy analysis used a modified ITT (mITT) population, which excluded participants who were ineligible for a second bimatoprost implant administration because the final study protocol amendment had been implemented. Safety parameters were evaluated in participants and eyes that received at least one study treatment.
Change from baseline in IOP in SLT- and bimatoprost implant–treated eyes at weeks 4, 12, and 24 was analyzed using a mixed-effects model for repeated measures with covariates of treatment, visit, eye, baseline IOP, treatment-by-baseline, treatment-by-eye, treatment-by-visit, and visit-by-eye interaction. The model used an unstructured covariance matrix for study visits and a compound symmetry covariance matrix for the between-eye correlation. Statistical noninferiority of the bimatoprost implant to SLT would be declared if the upper limit of the 95% confidence interval (CI) of the least-squares mean (LSM) difference in IOP change from baseline (bimatoprost implant minus SLT) at weeks 4, 12, and 24 was ≤1.5 mm Hg at all 3 visits. Clinical noninferiority of the bimatoprost implant to SLT would be declared if the upper limit of the 95% CI of the difference was ≤1.0 mm Hg at 2 or all 3 visits. The analysis of IOP change from baseline excluded IOP measurements taken at any time after use of rescue IOP-lowering treatment.
The sample size calculation was based on paired-eye differences using a normal approximation with a 2-sided significance level of 0.05. Enrollment of approximately 160 patients was planned to provide 98% power to show statistical noninferiority and 90% power to show clinical noninferiority of the bimatoprost implant to SLT, assuming the same mean IOP change from baseline in the bimatoprost implant– and SLT-treated eyes, a standard deviation (SD) of the mean IOP change from baseline of 4 mm Hg in both groups, a between-eyes correlation coefficient in change from baseline IOP of 0.5, and a study discontinuation rate of 10%.
Results
A total of 144 patients were enrolled and randomized to primary eye treatment with SLT (n=72) or bimatoprost implant 15 µg (n=72), with the alternative study treatment assigned to the contralateral eye. The study participants were primarily White, with a mean age of 60 years (Table 1), and most eyes were phakic, diagnosed with OAG, and had a baseline IOP no higher than 25 mm Hg after washout of any previous IOP-lowering medication (Table 2). The majority of eyes (70.8%) required washout of a topical PGA, most commonly latanoprost. Almost all (n=142) of the study participants received at least one study treatment, and the safety population of eyes consisted of 141 eyes that received SLT and 141 eyes that received the bimatoprost implant (14 eyes received 1 implant, 94 eyes received 2 implants, and 33 eyes received 3 implants). Among eyes that received the bimatoprost implant, 141, 127, and 33 eyes received a first, second, and third bimatoprost implant administration, respectively. The mITT population consisted of 138 study participants who received 1 (n=11), 2 (n=94), or 3 (n=33) administrations of the bimatoprost implant in the implant-treated eye.
 |
Table 1 Baseline Demographics Overall and by Assigned Treatment in Primary Eye (ITT Population) |
 |
Table 2 Baseline Characteristics of Eyes (Primary and Contralateral) by Study Treatment (ITT Population) |
The study completion rate was high, and 135 of the 144 enrolled patients (93.8%) completed the study. Reasons for study discontinuation were ocular adverse event (n=4), lost to follow-up (n=2), protocol violation (n=2), and withdrawal of consent (n=1). One of the ocular adverse events leading to study discontinuation occurred prior to study treatment (the adverse event was not a TEAE).
IOP-Lowering Effect
Mean (SD) baseline IOP in the mITT population was 24.38 (2.49) mm Hg for bimatoprost implant−treated eyes (n=138) and 24.45 (2.75) mm Hg for SLT-treated eyes (n=138). Analysis of the primary endpoint showed consistently greater reductions in IOP from baseline in the implant-treated eyes compared with the SLT-treated eyes at weeks 4, 12, and 24; the LSM difference between groups ranged from −0.25 to −0.75 mm Hg, with the between-group difference statistically significant at week 4 only (Figure 1). The upper limit of the 95% CI of the between-group difference (bimatoprost implant minus SLT) in LSM change in IOP from baseline was <1.0 mm Hg at all 3 visits. Therefore, bimatoprost implant 15 μg met the prespecified criteria for both statistical and clinical noninferiority to SLT in the mITT population. Noninferiority of bimatoprost implant 15 μg to SLT was also confirmed in a sensitivity analysis using the ITT population.
Approximately one-quarter of bimatoprost implant–treated and SLT-treated eyes required nonstudy (rescue) IOP-lowering treatment during the study. In each case, the nonstudy IOP-lowering treatment was medication; no eye received laser or surgical rescue treatment. Nonstudy IOP-lowering medication was used in 38 of 144 eyes in the bimatoprost implant group (26.4%) and 34 of 144 eyes in the SLT group (23.6%). Kaplan–Meier analysis of time to first use of nonstudy IOP-lowering treatment after the initial study treatment (SLT on day 1 or bimatoprost implant on day 4) showed that the durability of IOP control after SLT was similar to the duration of IOP control after beginning bimatoprost implant treatment (Figure 2). At 120 days after first treatment, a time point when eyes in the bimatoprost implant group had still received only a single implant administration, the probability of not requiring rescue IOP-lowering treatment was 97.2% with the bimatoprost implant versus 91.5% with SLT. At 180 days, when most eyes in the bimatoprost implant group had received a second implant administration, the probability of not requiring rescue IOP-lowering treatment was 93.6% with the bimatoprost implant versus 86.5% with SLT. At 360 days, when most eyes in the bimatoprost implant group had received either 2 or 3 implant administrations, the probability of not requiring rescue IOP-lowering treatment was 74.6% with the bimatoprost implant versus 77.1% with SLT. None of the differences between treatment groups in probability of not requiring rescue were statistically significant. Among the 14 eyes that were treated with a single bimatoprost implant, 10 completed the study; 4 of those eyes had been rescued, and 6 had not received any rescue therapy.
 |
Figure 2 Kaplan−Meier analysis of time to first use of nonstudy (rescue) IOP-lowering treatment. Abbreviations: IOP, intraocular pressure; SLT, selective laser trabeculoplasty. |
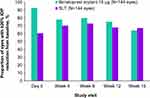
Responder rates were high with both study treatments. At follow-up study visits through week 15 (1 week before administration of a second implant, when the probability of having been rescued was <10%), the percentage of eyes achieving a ≥20% reduction in IOP from baseline ranged from 64.2% to 92.7% among bimatoprost implant–treated eyes and from 60.6% to 72.9% among SLT-treated eyes (Figure 3).
Safety
One or more TEAEs were reported for 81.0% (115/142) of study participants. Most TEAEs were ocular, and the incidence of ocular TEAEs was higher in the bimatoprost implant–treated eyes (70.2%, 99/141) than in the SLT-treated eyes (52.5%, 74/141). The incidence of treatment-related ocular TEAEs was also higher in the bimatoprost implant–treated eyes (52.5%, 74/141) than in the SLT-treated eyes (31.2%, 44/141). The only treatment-related non-ocular TEAE reported was headache, which was reported as related to the day 1 (SLT) treatment for 4.2% (6/142) of study participants. There were no deaths during the study.
Table 3 lists the most-reported ocular TEAEs. The most common ocular TEAE in both bimatoprost implant–treated and SLT-treated eyes was conjunctival hyperemia. Corneal TEAEs were reported in 19.9% (28/141) of bimatoprost implant–treated eyes compared with 4.3% (6/141) of SLT-treated eyes. The most frequent corneal TEAES were corneal endothelial cell loss and corneal edema. Corneal endothelial cell loss was infrequent in the bimatoprost implant–treated eyes after the first implant administration, but the incidence increased after the second and third implant administrations. Serious ocular TEAEs were reported for 6.3% (9/141) of the bimatoprost implant–treated eyes (5 corneal endothelial cell loss, 2 corneal edema, 1 cataract, 1 quadrantanopia), generally after the second or third implant administration. No serious ocular TEAEs were reported for the SLT-treated eyes. Anterior chamber inflammatory TEAEs, most commonly anterior chamber cell, were reported in 9.9% (14/141) of bimatoprost implant–treated eyes compared with 3.5% (5/141) of SLT-treated eyes. Iritis was reported in 3 (2.1%) implant-treated eyes, in each case after the second implant administration.
 |
Table 3 Incidence of Ocular TEAEs (Safety Population) |
Ocular TEAEs led to the early exit of three study participants. The ocular TEAEs leading to participant discontinuations (corneal edema, n=1; iritis, n=1; photophobia and lacrimation increased, n=1) all occurred in the bimatoprost implant–treated eye after the second implant administration. Eight of 141 bimatoprost implant–treated eyes (5.7%) required implant removal because of ocular TEAEs, most commonly corneal edema and corneal endothelial cell loss.
Specular microscopy findings showed greater loss in CECD in bimatoprost implant–treated eyes compared with SLT-treated eyes by week 40 (Table 4). During the study, 14.2% (20/141) of bimatoprost implant–treated eyes compared with 3.5% (5/141) of SLT-treated eyes demonstrated a ≥20% decrease in CECD from baseline. Consistent with TEAE reports of corneal endothelial cell loss, the mean decrease in CECD from baseline was larger in eyes that had received multiple implant administrations (Table 4). However, regardless of whether eyes had received 1, 2, or 3 bimatoprost implant administrations, the mean change in CECD from baseline at week 52 represented a <10% loss in CECD in implant-treated eyes (Table 4).
 |
Table 4 Corneal Endothelial Cell Density Findings on Specular Microscopy (Safety Population) |
On gonioscopic examination, the bimatoprost implant was often observed to swell after administration, then slowly decrease in size. By week 52, most of the implants administered on day 4 were reported to be ≤25% of the initial size or no longer visible. Overall, 22.7% (32/141) of study participants were reported to have bimatoprost implant contact the corneal endothelium in the implant-treated eye; most of these incidences occurred after the second implant administration. It is thought that corneal touch was more likely after repeated treatment because of accumulation of polymer in the angle, given the 16-week fixed dosing interval used in the study.
In other safety evaluations, biomicroscopy and ophthalmoscopy findings were more frequent in the bimatoprost implant–treated eyes because findings of conjunctival hyperemia (>1-grade increase from baseline) were reported for 23.4% (33/141) of implant-treated eyes compared with 6.4% (9/141) of SLT-treated eyes. Worsening of BCVA by more than 2 lines was reported for 9.9% (14/141) of bimatoprost implant–treated eyes and 4.3% (6/141) of SLT-treated eyes. There were no observed differences in cup/disc ratio between treatments, and there were no meaningful changes in central corneal thickness, with the mean change from baseline in central corneal thickness ranging from −4.5 to 2.9 μm in bimatoprost implant–treated eyes and 1.4 to 7.4 μm in SLT–treated eyes.
Discussion
This study evaluated a 15-µg bimatoprost implant, a higher dose than has been approved. The results showed a similar efficacy of the 15-µg bimatoprost implant and SLT in patients with OAG or OHT. In the analysis of the primary endpoint of change from baseline in IOP at weeks 4, 12, and 24, bimatoprost implant 15 µg met the prespecified criteria for statistical and clinical noninferiority to SLT. Furthermore, survival analysis demonstrated that the duration of IOP management without need for use of IOP-lowering eye drops was similar in bimatoprost implant–treated and SLT-treated eyes. SLT demonstrated a more favorable safety profile compared with the 15-µg bimatoprost implant. Serious ocular TEAEs were reported in 6.3% of implant-treated eyes versus no SLT-treated eyes, corneal TEAEs were reported in 19.9% of implant-treated eyes versus 4.3% of SLT-treated eyes, and anterior chamber inflammatory TEAEs were reported in 9.9% of implant-treated eyes versus 3.5% of SLT-treated eyes.
The marketed bimatoprost implant (bimatoprost implant 10 µg, Durysta) was approved for single administration based on the phase 3 ARTEMIS studies. Single administration of the 10-µg bimatoprost implant has been demonstrated to be both safe and effective in IOP lowering, whereas the 15-µg bimatoprost implant evaluated in this study was discontinued from development. In the ARTEMIS studies, the 10-µg bimatoprost implant provided mean IOP reductions ranging from 4.9 to 7.0 mm Hg up to 15 weeks after the initial administration, compared with mean IOP reductions of 6.0 to 6.3 mm Hg in eyes treated with timolol eye drops.21 Bimatoprost implant 10 and 15 µg both demonstrated noninferiority to topical timolol in IOP lowering.17,18 The mean IOP reduction and duration of IOP control without the use of IOP-lowering eye drops were not compared between the bimatoprost implant groups but generally appeared to be comparable with the 10-µg and 15-µg implants.17,18
Previous studies have demonstrated a long duration of IOP-lowering effect of the bimatoprost implant. In a phase 1/2 study, 23.8% (10/42) of eyes treated with the 10- or 15-µg bimatoprost implant required no additional IOP-lowering treatment up to 24 months after a single implant administration.20,21 Moreover, in the ARTEMIS studies, eyes treated with bimatoprost implant 10 or 15 µg had a >70% probability of requiring no additional IOP-lowering treatment for 1 year after their final implant administration.17,18 However, drug distribution studies using a canine model, analysis of drug concentrations in aqueous samples taken from patients who underwent implant removal, and in vitro drug release assays have suggested that intraocular bimatoprost concentrations decline to nondetectable levels by 3 to 4 months after administration of the bimatoprost implant.17 The extended duration of IOP lowering beyond the duration of intraocular drug bioavailability has been proposed to result from durable, matrix metalloproteinase (MMP)-mediated remodeling of aqueous outflow pathways. It was hypothesized that the high concentrations of bimatoprost achieved in target outflow tissues with the implant produce enhanced MMP upregulation, leading to more extensive and enduring tissue remodeling, and sustained IOP reduction.22 In support of this hypothesis, in human trabecular meshwork cell cultures, bimatoprost was shown to induce dramatic upregulation of MMP1 only at the high concentrations observed in bimatoprost implant–treated eyes.23
The safety profile of bimatoprost implant 15 µg observed in this study is consistent with findings in the phase 3 ARTEMIS studies.17,18 The majority of TEAEs were ocular, with higher incidence rates in the bimatoprost implant–treated eyes compared with the SLT-treated eyes. Some of the most common TEAEs observed in the implant-treated eyes, including conjunctival hyperemia, eye pain, conjunctival hemorrhage, and photophobia, typically occurred within 2 days after the implant administration procedure and were likely caused by the procedure preparation, which included povidone-iodine irrigation.
Corneal TEAEs including corneal endothelial cell loss and edema were safety concerns in the 15-µg bimatoprost implant–treated eyes. Corneal endothelial cells play an important role in maintaining the cornea in its natural state of relative dehydration,24 and extensive corneal endothelial cell loss results in corneal edema, corneal opacity, and reduced visual acuity.24 Corneal endothelial cell loss occurs during normal aging, with an estimated rate of CECD loss in adults of 0.6% per year.25 A 10% decrease in CECD may not be clinically meaningful or reliable,26 but larger losses in CECD can be of clinical concern. In this study, a ≥20% decrease in CECD from baseline was measured in 14.2% of eyes treated with bimatoprost implant 15 µg. Some eyes (3.5%) treated with SLT also had a ≥20% decrease in CECD from baseline. Worsening of BCVA by more than 2 lines was reported for 9.9% of the 15-µg bimatoprost implant–treated eyes compared with 4.3% of the SLT-treated eyes.
Among the 141 eyes treated with the 15-µg bimatoprost implant in this study, 8 (5.7%) required implant removal because of TEAEs. The implant removal procedure involves the use of an intraocular irrigating solution to flush the implant out of the eye through a keratome incision under sterile conditions.17 Corneal endothelial cell counts after study exit were not recorded in this study, but in the phase 3 ARTEMIS 1 study, in general, corneal TEAEs resolved and CECD stabilized after implant removal.17
Bimatoprost implant 15 µg was discontinued from development because the smaller 10-µg bimatoprost implant has a more favorable benefit-risk profile. The results of the present study are consistent with a greater risk of corneal adverse events with the 15-µg bimatoprost implant. In the present study, corneal endothelial cell loss was reported as a TEAE more frequently after multiple administrations of the 15-µg bimatoprost implant, but in three eyes, it was reported after the first (single) administration. Rare TEAEs of corneal endothelial cell loss were also reported after a single administration of the 15-µg bimatoprost implant in the ARTEMIS studies.17,18 In contrast, a single administration of bimatoprost implant 10 µg (the currently approved dose strength) was demonstrated to be safe in both ARTEMIS studies as well as in the phase 1/2 study.17,18,20 In all three studies, after a single administration of the 10-µg implant, there were no TEAE reports of corneal endothelial cell loss, corneal edema, or corneal touch, and no patient had a 20% or greater decrease in CECD from baseline.21
A limitation of this study is that the study design did not support evaluation of the duration of effect of a single administration of the bimatoprost implant because of the required re-administration at 16-week intervals. The number of implant administrations received varied among participants, with most receiving 2 implant administrations at a fixed 16-week dosing interval. Also, study enrollment was less than had been planned because the final study amendment ended patient enrollment. Nevertheless, the primary endpoint was met, and bimatoprost implant 15 µg demonstrated noninferiority to SLT in IOP lowering at 4, 12, and 24 weeks. Finally, the study did not use the 10-µg dose strength of the bimatoprost implant that is now approved for use (a single administration per eye) in the United States. A study comparing the approved 10-µg dose strength of the bimatoprost implant with SLT is currently in progress (NCT02507687), and the results are eagerly anticipated.
Conclusions
Bimatoprost implant 15 µg demonstrated statistical and clinical noninferiority to SLT in lowering IOP in patients with OAG or OHT. SLT demonstrated a more favorable safety profile than the 15-µg bimatoprost implant, with fewer corneal and inflammatory adverse events and no serious ocular adverse events reported in the SLT-treated eyes. The most important safety issue in the study was corneal endothelial cell loss, generally occurring after multiple implant administrations. The 15-µg dose strength of the bimatoprost implant was discontinued from development. However, single administration of bimatoprost implant 10 µg has been shown to be safe and efficacious, with a long duration of IOP-lowering effect, and single administration of bimatoprost implant 10 µg is currently approved for lowering IOP in patients with OAG and OHT. A study comparing the approved 10-µg bimatoprost implant with SLT (NCT02507687) is in progress.
Abbreviations
BCVA, best-corrected visual acuity; CECD, central endothelial cell density; CI, confidence interval; IOP, intraocular pressure; ITT, intent-to-treat; LSM, least-squares mean; mITT, modified intent-to-treat; MMP, matrix metalloproteinase; OAG, open-angle glaucoma; OHT, ocular hypertension; PGA, prostaglandin analog/prostamide; SD, standard deviation; SLT, selective laser trabeculoplasty; TEAE, treatment-emergent adverse event.
Data Sharing Statement
AbbVie is committed to responsible data sharing regarding the clinical trials we sponsor. This includes access to anonymized, individual, and trial-level data (analysis data sets), as well as other information (eg, protocols, clinical study reports, or analysis plans), as long as the trials are not part of an ongoing or planned regulatory submission. This includes requests for clinical trial data for unlicensed products and indications. These clinical trial data can be requested by any qualified researchers who engage in rigorous, independent, scientific research, and will be provided following review and approval of a research proposal, Statistical Analysis Plan (SAP), and execution of a Data Sharing Agreement (DSA). Data requests can be submitted at any time after approval in the US and Europe and after acceptance of this manuscript for publication. The data will be accessible for 12 months, with possible extensions considered. For more information on the process or to submit a request, visit the following link: https://www.abbvieclinicaltrials.com/hcp/data-sharing/.
Principal Investigators
Louis Alpern, MD; Mahdi Basha, MD; Lance Bergstrom, MD; James Branch, MD; Maria I. Canut, MD; William Christie, MD; Anastasios Costarides, MD; Frank Cotter, MD; Douglas Day, MD; Michael Depenbusch, MD; Alena Eremina, MD; John Galanis, MD; Julián García Feijoo, MD; Damien Goldberg, MD; Brennan Greene, MD; Linda Hansapinyo, MD; William Haynes, MD; Sebastian Heersink, MD; Bartłomiej Kałużny, MD; Miriam Kolko, MD; Benjamin Lambright, MD; Oleg Lebedev, MD; Christopher Lin, MD; Manchima Makornwattana, MD; Kundandeep Nagi, MD; Shamira Perera, MBBS, FRCOphth; Muriel Poli, MD; Cedric Schweitzer, MD; Pankajkumar Shah, MD; Scott Smetana, MD; Valerie Trubnik, MD; Gerald Walman, MD; Dominik Zalewski, MD
Acknowledgments
AbbVie and the authors thank the investigators and patients who participated in this study. Evidence Scientific Solutions, Inc (Philadelphia, PA, USA) provided medical writing assistance for the development of this publication. All authors had access to relevant data and participated in the drafting, review, and approval of this publication. No honoraria or payments were made for authorship.
Funding
This study was sponsored by Allergan (an AbbVie company), Irvine, CA, USA. Allergan/AbbVie participated in the design of the study, data management, data analysis, interpretation of the data, and preparation, review, and approval of the manuscript.
Disclosure
William C. Christie is a consultant for Allergan (an AbbVie company). Mahdi M. Basha has received research support from AbbVie, Alcon, Formosa Pharmaceuticals, Glaukos, Ivantis, Novartis, and Ocular Therapeutix, and is a speaker for AbbVie and Alcon. Quoc Ho, Kimmie Kim, and E. Randy Craven are employees of AbbVie Inc and may hold stock/stock options. Miriam Kolko is a speaker for AbbVie, Santen, Thea Laboratories, and Topcon. In addition, Miriam Kolko sits on advisory boards for AbbVie, Santen, and Thea Laboratories. The authors report no other conflicts of interest in this work.
References
1. Gedde SJ, Vinod K, Wright MM, et al. Primary Open-Angle Glaucoma Preferred Practice Pattern®. Ophthalmology. 2021;128(1):P71–P150.
2. Gedde SJ, Lind JT, Wright MM, et al. Primary Open-Angle Glaucoma Suspect Preferred Practice Pattern®. Ophthalmology. 2021;128(1):P151–P192. doi:10.1016/j.ophtha.2020.10.023
3. Schuman JS. Antiglaucoma medications: a review of safety and tolerability issues related to their use. Clin Ther. 2000;22(2):167–208. doi:10.1016/S0149-2918(00)88478-7
4. Mehran NA, Sinha S, Razeghinejad R. New glaucoma medications: latanoprostene bunod, netarsudil, and fixed combination netarsudil-latanoprost. Eye. 2020;34(1):72–88. doi:10.1038/s41433-019-0671-0
5. van der Valk R, Webers CA, Lumley T, Hendrikse F, Prins MH, Schouten JS. A network meta-analysis combined direct and indirect comparisons between glaucoma drugs to rank effectiveness in lowering intraocular pressure. J Clin Epidemiol. 2009;62(12):1279–1283. doi:10.1016/j.jclinepi.2008.04.012
6. Reardon G, Kotak S, Schwartz GF. Objective assessment of compliance and persistence among patients treated for glaucoma and ocular hypertension: a systematic review. Patient Prefer Adherence. 2011;5:441–463. doi:10.2147/PPA.S23780
7. Robin AL, Muir KW. Medication adherence in patients with ocular hypertension or glaucoma. Expert Rev Ophthalmol. 2019;14(4–5):199–210. doi:10.1080/17469899.2019.1635456
8. Alm A, Grierson I, Shields MB. Side effects associated with prostaglandin analog therapy. Surv Ophthalmol. 2008;53(Suppl 1):S93–105. doi:10.1016/j.survophthal.2008.08.004
9. Zhou X, Zhang X, Zhou D, Zhao Y, Duan X. A narrative review of ocular surface disease related to anti-glaucomatous medications. Ophthalmol Ther. 2022;11(5):1681–1704. doi:10.1007/s40123-022-00557-0
10. Garg A, Gazzard G. Selective laser trabeculoplasty: past, present, and future. Eye. 2018;32(5):863–876. doi:10.1038/eye.2017.273
11. Chi SC, Kang YN, Hwang DK, Liu CJ. Selective laser trabeculoplasty versus medication for open-angle glaucoma: systematic review and meta-analysis of randomised clinical trials. Br J Ophthalmol. 2020;104(11):1500–1507. doi:10.1136/bjophthalmol-2019-315613
12. Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Selective laser trabeculoplasty versus drops for newly diagnosed ocular hypertension and glaucoma: the LiGHT RCT. Health Technol Assess. 2019;23(31):1–102. doi:10.3310/hta23310
13. Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Laser in glaucoma and ocular hypertension (LiGHT) trial: six-year results of primary selective laser trabeculoplasty versus eye drops for the treatment of glaucoma and ocular hypertension. Ophthalmology. 2023;130(2):139–151. doi:10.1016/j.ophtha.2022.09.009
14. Ruiz-Lozano RE, Alamillo-Velazquez J, Ortiz-Morales G, et al. Selective laser trabeculoplasty is safe and effective in patients previously treated with prostaglandin analogs: an evidence-based review. Int Ophthalmol. 2023;43(2):677–695. doi:10.1007/s10792-022-02460-w
15. Jang HJ, Yu B, Hodge W, Malvankar-Mehta MS. Repeat selective laser trabeculoplasty for glaucoma patients: a systematic review and meta-analysis. J Curr Glaucoma Pract. 2021;15(3):117–124. doi:10.5005/jp-journals-10078-1302
16. Garg A, Vickerstaff V, Nathwani N, et al. Efficacy of repeat selective laser trabeculoplasty in medication-naive open-angle glaucoma and ocular hypertension during the LiGHT trial. Ophthalmology. 2020;127(4):467–476. doi:10.1016/j.ophtha.2019.10.023
17. Medeiros FA, Walters TR, Kolko M, et al. Phase 3, randomized, 20-month study of bimatoprost implant in open-angle glaucoma and ocular hypertension (ARTEMIS 1). Ophthalmology. 2020;127(12):1627–1641. doi:10.1016/j.ophtha.2020.06.018
18. Bacharach J, Tatham A, Ferguson G, et al. Phase 3, randomized, 20-month study of the efficacy and safety of bimatoprost implant in patients with open-angle glaucoma and ocular hypertension (ARTEMIS 2). Drugs. 2021;81(17):2017–2033. doi:10.1007/s40265-021-01624-9
19. Weinreb RN, Bacharach J, Brubaker JW, et al. Bimatoprost implant biodegradation in the phase 3, randomized, 20-month ARTEMIS studies. J Ocul Pharmacol Ther. 2023;39(1):55–62. doi:10.1089/jop.2022.0137
20. Craven ER, Walters T, Christie WC, et al. 24-Month phase I/II clinical trial of bimatoprost sustained-release implant (Bimatoprost SR) in glaucoma patients. Drugs. 2020;80(2):167–179. doi:10.1007/s40265-019-01248-0
21. Medeiros FA, Sheybani A, Shah MM, et al. Single administration of intracameral bimatoprost implant 10 µg in patients with open-angle glaucoma or ocular hypertension. Ophthalmol Ther. 2022;11(4):1517–1537. doi:10.1007/s40123-022-00527-6
22. Weinreb RN, Robinson MR, Dibas M, Stamer WD. Matrix metalloproteinases and glaucoma treatment. J Ocul Pharmacol Ther. 2020;36(4):208–228. doi:10.1089/jop.2019.0146
23. Stamer WD, Perkumas KM, Kang MH, Dibas M, Robinson MR, Rhee DJ. Proposed mechanism of long-term intraocular pressure lowering with the bimatoprost implant. Invest Ophthalmol Vis Sci. 2023;64(3):15. doi:10.1167/iovs.64.3.15
24. Schmedt T, Silva MM, Ziaei A, Jurkunas U. Molecular bases of corneal endothelial dystrophies. Exp Eye Res. 2012;95(1):24–34. doi:10.1016/j.exer.2011.08.002
25. Bourne WM, Nelson LR, Hodge DO. Central corneal endothelial cell changes over a ten-year period. Invest Ophthalmol Vis Sci. 1997;38(3):779–782.
26. McCarey BE, Edelhauser HF, Lynn MJ. Review of corneal endothelial specular microscopy for FDA clinical trials of refractive procedures, surgical devices, and new intraocular drugs and solutions. Cornea. 2008;27(1):1–16. doi:10.1097/ICO.0b013e31815892da
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.