Back to Journals » Neuropsychiatric Disease and Treatment » Volume 17
Phantom Limb Pain and Sensations in Chinese Malignant Tumor Amputees: A Retrospective Epidemiological Study
Authors Jiang S , Zheng K, Wang W, Pei Y, Qiu E, Zhu G
Received 30 December 2020
Accepted for publication 6 April 2021
Published 21 May 2021 Volume 2021:17 Pages 1579—1587
DOI https://doi.org/10.2147/NDT.S299771
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jun Chen
Shuang Jiang,1,2 Ke Zheng,3 Wei Wang,3 Yi Pei,3 Enduo Qiu,3 Gang Zhu1,4
1Department of Psychiatry, The First Affiliated Hospital of China Medical University, Shenyang, 110001, People’s Republic of China; 2Department of Pain Medicine (Psychology Clinic), Cancer Hospital of China Medical University, Liaoning Cancer Hospital & Institute, Shenyang, 110042, People’s Republic of China; 3Department of Bone and Soft Tissue Tumor Surgery, Cancer Hospital of China Medical University, Liaoning Cancer Hospital & Institute, Shenyang, 110042, People’s Republic of China; 4Central Laboratory, The First Affiliated Hospital of China Medical University, Shenyang, 110001, People’s Republic of China
Correspondence: Gang Zhu Tel/Fax +86-24-83282184
Email [email protected]
Objective: Phantom limb pain (PLP) was a common problem in malignant tumor amputees that can cause considerable suffering. The purposes of this study were to determine the incidence and factors associated with the occurrence of post-operation PLP, stump limb pain (SLP), and phantom limb sensations (PLS) in tumor amputees within the first month after surgery. Additionally, differences in phantom phenomena between upper and lower extremities were investigated.
Methods: In total, 162 amputees participated in this retrospective study who underwent malignant limb amputation between 2012 and 2019. Clinical characteristics were collected from medical records and reconfirmed by telephone interviews. A numerical rating scale (NRS) was used to quantitate phantom phenomena. We used analysis of variance and non-parametric statistics for categorical variables and ordinal variables separately.
Results: In the first month after malignant amputation, the incidence of PLP was 54.3%, that of PLS was 65.4%, and that of SLP was 32.7%. The duration of preoperative pain and amputation level was significantly different for the incidence of acute PLP. Further subgroup analysis of amputation level showed that patients whose amputation level was below the wrist and ankle joints had a significantly reduced incidence of PLP (p< 0.0083 in Bonferroni test). Binary logistics regression analysis determined that amputation level was the primary risk factor for the incidence of PLP. Factors related to the severity of postoperative PLP also included amputation level, preoperative pain, and amputation times. By comparing the differences between upper and lower limbs after amputation, we found that the incidence of PLS was higher after lower limb amputation, but there was no significant difference in the incidence of PLP and SLP. Preoperative experience of chemotherapy was not a risk factor for PLP.
Conclusion: Proximal amputation and long-term preoperative pain seemed to count more for PLP incidence. Further research may be required to individually determine factors associated with the occurrence and chronicity of phantom phenomena.
Keywords: phantom limb pain, phantom sensation, amputation level, preoperative pain
Introduction
Phantom limb pain (PLP) is a pain sensation from a removed extremity following amputation. The all-cause prevalence of PLP has been reported to be between 50% and 80%.1–3 Etiologies of PLP are often not categorized and have contrasted in previous studies due to sample size restrictions. In addition to infections, injuries, diabetes mellitus, and peripheral vascular diseases, malignant tumors of bones and soft tissues of the extremities are the most common causes of elective amputation for adults; however, to our knowledge, PLP in malignant amputees are rarely discussed.4 As preoperative diabetes is one of the risk factors for postoperative PLP,5 tumor amputation was also previously suspected to be a risk factor for PLP.1 This means that the prevalence of other etiologies cannot be extrapolated to that of malignant amputees. Therefore, it is necessary to carry out an independent and updated analysis on tumor amputees.
Due to different environmental settings during data collection (eg, rehabilitation hospitals, prosthetics adaptation centers, emergency of traumatological orthopedics), timelines after amputation often lack consistency. Kooijman et al discussed the difference between the incidence of PLP in the immediate postoperative period and 6 months after amputation, and presumed that time of data selection may have biased the estimates of PLP prevalence.6 Most studies have concluded that increased time since amputation may result in resolution of PLP.7,8 Therefore, we believe that it is necessary to separate the PLP discussion into the incidence stage and the development stage. In this study, we assumed the incidence stage of PLP to be 1 month after surgery, and then tried to explore correlations between pre-amputation factors and the incidence of postoperative phantom limb symptoms. The chronic PLP was not an aim of this research.
The detailed incidence and affecting factors on PLP after malignant amputation is especially insufficient in Chinese patients. The recent review appealed for data revision because the previous low prevalence rates recorded in developing countries may be associated with the stigmatization of phantom limb pain as a psychiatric illness.4 Previous researches also provide some risk factors for PLP, but factors associated with malignant tumor are rare. Malignant amputation is characterized by chronic preoperative pain from tumor invasion, strong psychological stress, specific pathological types with potential neurotropism, and latent neuropathic damage from preoperative chemotherapies. It is necessary to provide some data about these factors. Preoperative pain has been discussed as a risk factor for PLP5,9; however, detailed descriptions of preoperative pain are missing. Therefore, we performed a retrospective analysis to investigate the duration of preoperative suffering but not the severity and characteristics of the pain, since this information is always inaccurate after the event. The amputation level may be also a risk factor, which needs to be discussed in detailed level in upper and lower extremities. These risk factors were determined for two major central mechanism hypotheses of PLP (cortical reorganization and pain memory), which remain controversial.4,10–12 We believe meticulous epidemiological observations could provide more clues to reveal the phantom phenomena.
Methods
Participants
This research was based on the Declaration of Helsinki as the moral principle. Medical records of participants who had undergone limb amputation between May 2012 and June 30, 2019, were retrospectively reviewed upon approval from the local ethics committee of Cancer Hospital of China Medical University (NO. 20191165). All participants provided an informed consent form. The study cohort included 162 adult amputees (male: 94, female: 68) from 634 records in the database of the orthopedic ward.
All 634 records were pre-screened and excluded by the following criteria: Age <30 years, history of mental disorders, communication problems such as dementia, refusal to participate in the study, and comorbidities like diabetes mellitus. Amputees from metastatic or borderline tumor were excluded. Repeated records for chemotherapy or incomplete records were excluded. Two hundred and fifty-six complete records remained for further telephone-reconfirming. Subjective information about pain and informed consent in admission records are reconfirmed through the telephone interview, and the unconfirmed records were discarded (the patient died or seriously ill, lost contact, refused to participate, responded equivocally). Finally, 162 qualified records were obtained for analysis.
Pathological diagnoses of the amputees are listed in Table 1. Patients who received preoperative analgesics if necessary were not excluded, only the presence and duration of preoperative pain were recorded. Patients who underwent amputation of one or several fingers or toes were not excluded, but were categorized with subjects who underwent half palm or sole amputation in the “below the wrist or ankle” group.
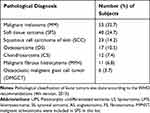 |
Table 1 Pathological Diagnoses of the Subjects |
Study Design and Data Definitions
The following items along with supplemental information were collected from hospital records and telephone follow-up interviews: age, sex, amputation frequency (single time or multiple times), amputation and dominant side (same or different), amputation level (4 levels as listed in Table 2), anesthesia method (general or local), pathological diagnosis, pain prior to amputation (present or absent), duration of preoperative pain, chemotherapies prior to operation (present or absent), stump limb pain (SLP, present or absent), phantom limb sensation (PLS), and PLP (present or absent), as well as average severity of PLS, PLP, and SLP during hospitalization (approximately 1 month after surgery). Epidural blockade and brachial plexus blockade were identified as local anesthesia in this study.
 |
Table 2 Kruskal–Wallis Test and Chi-Square Test for Level of Amputation and Phantom Phenomena |
In the first month after amputation, the patients always need stay in hospital for standard nursing and rehabilitation. The severity of pain and sensation were daily recorded in the nursing charts using a numerical rating scale (NRS). In the first 2 weeks after amputation, “Dezocine” was usually used as an analgesic agent for everyone. If dezocine could not offer enough analgesic effect, other analgesic agents would be administered for codes of ethics. The NRS scores before other agents used was called effective NRS. If other agents were used, NRS score cease to count. Effective NRS was used to account the average severity and then graded the score into three levels as mild (1–3), moderate (4–6), and severe (7–10). The brief three-level classification of NRS was designed to smooth the bias of subjective pain experience.
Due to the absence of standardized tools for assessing PLP, outcome measure was validated here by “Phantom phenomena questionnaire (PPQ)” from Prof. Cliff Richardson. Experienced interviewer explained what PLP, SLP, and non-painful PLS means and the differences among them, and interviewed the participants, reorganized the data by PPQ, and then grouped them for further analysis. Telephone interview only performed once as a manner to increase the credibility of data.
Statistical Analysis
Statistical analyses were performed using SPSS version 26 (IBM Corp., Armonk, NY, USA). Median and interquartile range was used to deal with outliers when the data not normally distributed. The univariate chi-squared test and continuity correction chi-square test were used to analyze associations between dichotomous variables. Shapiro–Wilk’s test, skewness, kurtosis was applied to evaluate normality for continuous variables. Student’s t-test or Mann–Whitney U-test were used for normal or non-normal distributed data, respectively. Continuous variables are expressed as mean ± standard deviation or median. Bonferroni analyses were also performed to compare the four amputation levels. Kruskal–Wallis tests were performed to detect differences between variables and severity of PLP and PLS. Levels of significance were set at p < 0.05. Bivariate regression analysis with candidate variables was performed to determine which preoperative risk factors could affect the incidence of PLP and PLS.
Results
Demographic and Clinical Characteristics of the Participants
Malignant melanoma (MM) and soft tissue sarcoma (SFS) are the most common etiologies of malignant amputations in adults. The average age of all subjects was 55.17±14.62 years (range: 30–88). Male amputees accounted for 58% of the participants. In total, 68 (42%) amputees had operations on the upper limb and 14 (9%) received multiple amputations due to disease deterioration. The dominant side was amputated in 84 (52%) cases. A total of 142 (88%) cases received general anesthesia for a wide range of lesions, lymph node dissection, or skin graft. There were 73 (45%) participants who experienced preoperative pain due to septic ulcers of the skin, swelling and distension of the tissue, or infectious complications. Preoperative chemotherapies were given to 24 (15%) patients (Table 3).
 |
Table 3 Background Information of Amputees and Chi-Square Test for Dichotomous Variables |
Incidence of PLP, SLP, and PLS, and Factors Associated with These Phenomena
Within the first month after amputation, the incidence of phantom pain was 54.3%, that of phantom sensations was 65.4%, and that of stump pain was 32.7% (Table 3). Amputees who experienced PLP did not differ significantly from those who did not experience PLP regarding age, sex, amputation times, amputation side, types of anesthesia, and perioperative chemotherapy; however, there were significant differences between the groups in the presence of preoperative pain (Table 3), especially pre-operative pain duration (Table 4). The risk factors associated with PLS were general anesthesia and the presence of preoperative pain. SLP seems to only be an occasional outcome of amputation. However, it should be noted that local anesthesia often implicates lower amputation levels or less metastases. For example, patients with local MM on toes or fingers always undergone lower-level amputation and tended to choose local anesthesia.
 |
Table 4 Student’s t-test and Mann–Whitney Rank Test for Continuous Variables |
We also focused on the levels of amputation and analyzed the different incidences of PLP between upper and lower extremities. It was found that the incidence of PLP and PLS were significantly related to amputation level (Table 2), while the occurrence of SLP was not. PLP and PLS are rare in distal limb amputees, especially in “below the wrist (BTW)” and “below the ankle (BTA)” groups according to the Bonferroni test (p<0.0083). Another finding was that there was no significant difference in the incidence of PLP, but a significant difference in the incidence of PLS between the upper and lower limbs, while lower limb amputees more likely to experience PLS.
When entering the two candidate factors into binary logistic regression analysis for PLP (Table 5), it was found that the effect of preoperative pain was no longer significant, but that amputation level (ie, below the ankle and below the wrist) was more likely to prevent PLP (BTW-OR:0.104, p=0.001; BTA-OR:0.152, p=0.010), suggesting that the level of amputation accounts more for PLP.
 |
Table 5 Binary Logistic Regression Analysis for PLP in Upper and Lower Extremities |
Relationship Between the Severity of Phantom Limb Pain and Other Factors
According to the Kruskal–Wallis test, amputation times, level of amputation, and preoperative pain were associated with the severity of PLP and PLS (Table 6). Sex, whether the amputation side is dominant, anesthesia method, and preoperative chemotherapy did not change the severity of PLP or PLS. Among the factors investigated, no one showed a significant statistical association with the severity of postoperative SLP.
 |
Table 6 Non-Parametric Test for the Difference Between Variables and Severity of PLP, SLP and PLS |
Discussion
We have noted that the prevalence of PLP varied considerably in different studies. Different definitions of risk factors, inclusion and exclusion criteria, and sample collection settings may have induced these varying results. The details of study design should be paid close attention when interpreting the results of different studies. Malignant tumors are one of the major three etiologies of amputation; however, these cases are rarely discussed separately from other etiologies despite having obviously unique pathological mechanisms and therapeutic strategies. Limakatso et al released the first meta-analysis of the prevalence of PLP and related risk factors in 2019. They concluded that, except for congenital limb insufficiency, the overall incidence of PLP in acquired amputees was between 50% and 85.6% among etiologically mixed samples.4 Yin et al reported in 2017 that the incidence of PLP in the Chinese population was 29%, but the main amputation cause was trauma (60.5%).13 Due to limited sample size, a few studies only discussed tumor amputation and reported that the prevalence of PLP in adult tumor amputation patients was between 41% and 60%,14,15 and that of youth and children was between 48% and 85.7%.16–19 The incidence of PLP in malignant amputees was 54.3% in this study. We did not exclude the toe or finger amputees, which might explain the relatively lower incidence. Here, we only retrospectively reviewed the incidence of PLP in the first month post-amputation and provide a reference for similar amputees. Our results suggested that there was no significant difference in the incidence of PLP and SLP between upper and lower limbs.
In addition to PLP, postoperative PLS was also investigated as necessary to differentiate pain and sensation. The incidence of PLS was 65.4% in this study, which was highly coordinated but higher than PLP. Studies on PLS are relatively rare. It is generally believed that PLS is a more common postoperative phantom phenomenon than PLP and a related factor of PLP. Casale et al reported that the incidence of PLS in the lower extremities was 90% at 6 months after amputation and 60% 1 year later.20 Kooijman et al reported that the incidence of PLS in only upper extremity amputation cases was 76%, which included patients with congenital limb loss. 6 A simple comparison seems to show that lower limb amputees have a higher PLS probability. No precedent for comparing phantom limb phenomena between upper and lower limbs in tumor amputees was found. During this study, the comparison of upper and lower limbs found that the overall incidence of PLS in lower limb amputees was significantly higher than that of upper limb amputees. However, this phenomenon and the underlying latent mechanisms still need to be confirmed by further studies.
The incidence of residual limb pain was relatively low, and no related factors were found. SLP seemed like an accidental phenomenon after surgery. For ethical considerations, patients were routinely administered dezocine via intravenous drip for analgesia within 1 week after surgery, which might cover SLP.
In this study, we investigated the risk factors of postoperative PLP, and amputation level was found to be the primary influencing factor. The incidence of PLP in patients with amputation below the wrist and ankle joints was significantly lower; however, PLP of the rest of the amputated proximal limbs was unaffected by amputation level. Previous studies have suggested that PLP is more likely to occur in proximal amputees than in distal amputees.21,22 Ahmed et al divided the amputation level into upper and lower sections with elbow and knee joint and reported that the prevalence of PLP was high in patients with proximal amputations.14 Kooijman et al suggested a trend for an association between amputation level and PLP.6 Subjects with amputations above the elbow experienced PLP more frequently than those with an amputation below the elbow, but this association did not reach the level of statistical significance. Other studies have shown mixed results. Kelle et al investigated the early period of amputation in mixed etiology samples and found that the VAS scores of PLP, which can be used as predictors of chronic PLP, were higher in amputees above the knee and below the ankle but the differences gradually disappeared over time.23 However, there are also negative results. Noguchi et al also classified the upper and lower extremity amputees into two groups and found no difference in PLP.5 It is unclear if the bias between results was from the partition of amputation level, so it is necessary to distinguish the correlation between amputation level and PLP by subdivision statistics. In this study, using a four-level classification system, we found that distal amputation, especially distal amputation below the wrist and ankle joint, was associated with a significantly reduced incidence of PLP. Proximal amputation may suggest a larger projection area of correspondingly affected cortex, but why proximal amputation was more likely to cause PLP than distal amputation will require further mechanistic studies.
Despite conflicting reports about the association between preoperative pain and PLP, more studies support that amputees with pain before amputation are more likely to develop PLP.24 Noguchi et al reported that insufficient analgesia for preoperative pain and diabetes mellitus can impact the development of PLP.5 Yin et al reported that preoperative pain is a risk factor for PLP.13 Larbig et al reported that preoperative pain and postoperative subacute pain are risk factors for predicting long-term chronic PLP and concluded that early intervention for pain is important for preventing chronic pain and interrupting the brain from learning pain memory.9 Ahmed et al found preoperative pain in 36.67% of the adult tumor amputees and a higher incidence of PLP and PLS in these patients.14 However, it should be noted that there have been studies of peripheral vascular diseases and tumor samples that reported preoperative pain had no effect on PLP.25,26 Hagberg et al concluded that preoperative pain in lower limb is related to PLP,27 while Kooijman et al believe that preoperative pain is unrelated to PLP after upper limb amputation.6 This suggests that preoperative pain in different parts of the limb may also affect the occurrence of PLP. One of the possible reasons for the controversy above is that most of the studies did not investigate suspicious preoperative pain in detail, such as the intensity of onset, frequency, characteristics, and total duration. Due to the limitations of retrospectively reviewing pain intensity, these data are very likely to be inaccurate. Therefore, in this study, only the duration of preoperative pain was collected as a factor, then preoperative pain, especially the duration of preoperative pain was believed to be a risk factor for the incidence of PLP. We also believe that it is necessary to fully collect information on preoperative pain, emotions, and other feelings before amputation in future studies.
Unlike other causes of amputation, preoperative chemotherapy is common in patients with tumor amputation and a unique potential factor that could influence PLP. With the application of neoadjuvant chemotherapy in the treatment of limb tumors, preoperative chemotherapy (PoC) and limb reservation have become more conventional. Available chemotherapy drugs (CHRx) such as methotrexate, platinum, and vincristine are susceptible to chemotherapy-related peripheral neuropathy (CIPN); meanwhile, the latent injury means the influence of the peripheral nerve may also account for part of mechanisms of PLP as discussed previously. Not only do the mechanistic intersections of PLP and CIPN make PoC suspicious, there are also supporting observations. Among pediatric amputees, 74% of those who had been exposed to CHRx before or during amputation experienced PLP, 44% of the patients who received CHRx after amputation experienced PLP, and only 12% of the patients who had never received CHRx have experienced PLP.18 Ahmed et al started a discussion on chemotherapy and PLP in adult cancer patients.28 In total, 33.8% of the subjects received chemotherapy and their risk of PLP and PLS was higher, their risk of SLP in the early stage was also higher. In contrast, Yin et al reported that radiotherapy and chemotherapy had nothing to do with the occurrence of PLP.13 We did not detect differences in PLP between the PoC group and the non-PoC group. Obviously, current discussion on PoC is insufficient and limited by the small sample, different time points of data collection, and different CHRx. We believe that chemotherapy should be discussed separately between the preoperative or postoperative stages when we discuss the occurrence of PLP.
This study did not find other factors significantly related to the occurrence of PLP. There have been studies suggesting that PLP is more likely to occur in patients who experienced general anesthesia28 and those who needed postoperative analgesia.13 Suffered subacute pain might be a risk factor for developing PLP. But Noguchi et al believe that the choice of anesthesia has nothing to do with postoperative PLP.5 We also did not detect a relationship between PLP and anesthesia. Additionally, psychosocial factors may also be related factors that lead to differences.29 Larbig et al reported that the severity of PLP 1 year after amputation was related to depression and anxiety.9 Emotional state may be a risk factor for chronic pain, but it is difficult to accurately collect emotional status in retrospective studies, so it was not discussed in this study.
We also found that amputation times, amputation level, and preoperative pain may be factors related to the severity of PLP. Sex, PoC, and amputation of the dominant limb did not lead to more severe pain. We concluded that occurrence and severity should be discussed separately. Our results were not much different from the existing epidemiological data and provide some data of current status of PLP in tumor amputees.
Limitations
The limitations of this study included (a) a small sample size relative to the large number of predictors in a retrospective single-center study; survivor bias could exist due to the low survival rates of malignant amputees; (b) the significant loss of effective data from the difficulty in following-up; although a smaller timescale was set to shorten the recall deviation, information bias is still inevitable; chemotherapy and other intervention guidelines may also have changed over the study period; (c) due to the lack of effective interview tools, the understanding and description of PLP could not be unified; previous studies designed specific questionnaires for their concerned traits, but there is no confirmed consensus in how to describe PLP; the experience of pain is highly subjective, and a unified scale to quantify PLP is currently absent; and (d) the incidence of PLP was discussed only within 1 month after surgery. This study did not include amputees with delayed PLP. Additionally, the entire course and severity of PLP were not fully described, so no complete picture of PLP is shown.
Conclusion
To the best of our knowledge, this is the first attempt to provide epidemiological evidence in Chinese malignant amputees. PLP should be discussed separately upon occurrence and development stages. The incidence and severity of phantom pain in malignant amputees were retrospectively analyzed. The time-length of preoperative pain was found to be related to the occurrence of postoperative phantom limb pain in the adult population. It remains necessary and worthy to set up a tool for consistency evaluations to allow future studies to measure the phantom phenomenon uniformly. Comprehensive descriptive data are required to provide more clues for future mechanistic research.
Acknowledgments
This project was supported by a grant from the Major Project of the Department of Science & Technology of Liaoning Province (2019JH8/10300019). We must express our strong gratitude to the Prof. Cliff Richardson (The University of Manchester) for the sharing of “Phantom phenomena questionnaire (PPQ)” and helping us use it correctly by email. This questionnaire was used to unify the description of phantom phenomena and to make the data Structured. We also appreciate the specific contribution of April Hsia in editing and Leif Li in data processing.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kavitha R, Joshua H. Phantom limb pain. J Palliat Med. 2010;13(10):1285–1286. doi:10.1089/jpm.2010.9775
2. Le Feuvre P, Aldington D. Know pain know gain: proposing a treatment approach for phantom limb pain. J R Army Med Corps. 2014;160:16–21. doi:10.1136/jramc-2013-000141
3. Allami M, Faraji E, Mohammadzadeh F, Soroush MR. Chronic musculoskeletal pain, phantom sensation, phantom and stump pain in veterans with unilateral below-knee amputation. Scand J Pain. 2019;aop:1–9. doi:10.1515/sjpain-2019-0045
4. Limakatso K, Bedwell GJ, Madden VJ, Parker R. The prevalence and risk factors for phantom limb pain in people with amputations: a systematic review and meta-analysis. PLoS One. 2020;15:e0240431. doi:10.1371/journal.pone.0240431
5. DeMoss P, Ramsey LH, Karlson CW. Phantom limb pain in pediatric oncology. Front Neurol. 2018;9:7–9. doi:10.3389/fneur.2018.00219
6. McCormick Z, Chang-Chien G, Marshall B, Huang M, Harden RN. Phantom limb pain: a systematic neuroanatomical-based review of pharmacologic treatment. Pain Med. 2014;15:292–305. doi:10.1111/pme.12283
7. Raffin E, Richard N, Giraux P, Reilly KT. Primary motor cortex changes after amputation correlate with phantom limb pain and the ability to move the phantom limb. Neuroimage. 2016;130:134–144. doi:10.1016/j.neuroimage.2016.01.063
8. Richardson C, Olleveant N, Crawford K, Kulkarni J. Exploring the role of cortical reorganization in postamputation phantom phenomena, including phantom limb pain in lower limb amputees: a cross-sectional study of the patterns of referral of sensations into the phantom. Pain Manag Nurs. 2018;19(6):599–607. doi:10.1016/j.pmn.2018.04.004
9. Kikkert S, Johansen-Berg H, Tracey I, Makin TR. Reaffirming the link between chronic phantom limb pain and maintained missing hand representation. Cortex. 2018;106:174–184. doi:10.1016/j.cortex.2018.05.013
10. Noguchi S, Saito J, Nakai K, Kitayama M, Hirota K. Factors affecting phantom limb pain in patients undergoing amputation: retrospective study. J Anesth. 2019;33(2):216–220. doi:10.1007/s00540-018-2599-0
11. Yin Y, Zhang L, Xiao H, et al. The pre-amputation pain and the postoperative deafferentation are the risk factors of phantom limb pain: a clinical survey in a sample of Chinese population. BMC Anesthesiol. 2017;17(1):1–6. doi:10.1186/s12871-017-0359-6
12. Ahmed A, Bhatnagar S, Mishra S, Khurana D, Joshi S, Ahmad S. Prevalence of phantom limb pain, stump pain, and phantom limb sensation among the amputated cancer patients in India: a prospective, observational study. Indian J Palliat Care. 2017;23(1):24–35. doi:10.4103/0973-1075.197944
13. Mishra S, Bhatnagar S, Gupta D, Diwedi A. Incidence and management of phantom limb pain according to World Health Organization analgesic ladder in amputees of malignant origin. Am J Hosp Palliat Med. 2008;24(6):455–462. doi:10.1177/1049909107304558
14. Burgoyne LL, Billups CA, Jirón JL, et al. Phantom limb pain in young cancer-related amputees: recent experience at St Jude children’s research hospital. Clin J Pain. 2012;28(3):222–225. doi:10.1097/AJP.0b013e318227ce7a
15. Anghelescu DL, Kelly CN, Steen BD, et al. Mirror therapy for phantom limb pain at a pediatric oncology institution. Rehabil Oncol. 2016;34(3):104–110. doi:10.1097/01.REO.0000000000000022
16. Smith J, Thompson JM. Phantom limb pain and chemotherapy in pediatric amputees. Mayo Clin Proc. 1995;70(4):357–364. doi:10.4065/70.4.357
17. Krane EJ, Heller LB. The prevalence of phantom sensation and pain in pediatric amputees. J Pain Symptom Manage. 1995;10(1):21–29. doi:10.1016/0885-3924(94)00062-P
18. Casale R, Alaa L, Mallick M, Ring H. Phantom limb related phenomena and their rehabilitation after lower limb amputation. Eur J Phys Rehabil Med. 2009;45:559–566.
19. Kooijman CM, Dijkstra PU, Geertzen JHB, Elzinga A, Van Der Schans CP. Phantom pain and phantom sensations in upper limb amputees: an epidemiological study. Pain. 2000;87(1):33–41. doi:10.1016/S0304-3959(00)00264-5
20. Gallagher P, Allen D, Maclachlan M. Phantom limb pain and residual limb pain following lower limb amputation: a descriptive analysis. Disabil Rehabil. 2001;23:522–530. doi:10.1080/09638280010029859
21. Dijkstra PU, Geertzen JHB, Stewart R, Van Der Schans CP. Phantom pain and risk factors: a multivariate analysis. J Pain Symptom Manage. 2002;24:578–585. doi:10.1016/S0885-3924(02)00538-9
22. Kelle B, Kozanoğlu E, Biçer ÖS, Tan İ. Association between phantom limb complex and the level of amputation in lower limb amputee. Acta Orthop Traumatol Turc. 2017;51(2):142–145. doi:10.1016/j.aott.2017.02.007
23. Hanley MA, Jensen MP, Smith DG, Ehde DM, Edwards WT, Robinson LR. Preamputation pain and acute pain predict chronic pain after lower extremity amputation. J Pain. 2007;8:102–109. doi:10.1016/j.jpain.2006.06.004
24. Larbig W, Andoh J, Huse E, et al. Pre- and postoperative predictors of phantom limb pain. Neurosci Lett. 2019;702:44–50. doi:10.1016/j.neulet.2018.11.044
25. Richardson C, Crawford K, Milnes K, Bouch E, Kulkarni JA. Clinical evaluation of postamputation phenomena including phantom limb pain after lower limb amputation in dysvascular patients. Pain Manag Nurs. 2015;16:561–569. doi:10.1016/j.pmn.2014.10.006
26. Wall R, Novotny-Joseph P, Macnamara TE. Does preamputation pain influence phantom limb pain in cancer patients? South Med J. 1985;78(1):34–36. doi:10.1097/00007611-198501000-00009
27. Hagberg K, Brånemark R. Consequences of non-vascular trans-femoral amputation: a survey of quality of life, prosthetic use and problems. Prosthet Orthot Int. 2001;25(3):186–194. doi:10.1080/03093640108726601
28. Lee BM, Singh Ghotra V, Karam JA, Hernandez M, Pratt G, Cata JP. Regional anesthesia/analgesia and the risk of cancer recurrence and mortality after prostatectomy: a meta-analysis. Pain Management. 2015;5:387–395. doi:10.2217/PMT.15.30
29. Luza LP, Ferreira EG, Minsky RC, Pires GKW, da Silva R. Psychosocial and physical adjustments and prosthesis satisfaction in amputees: a systematic review of observational studies. Disabil Rehabil Assist Technol. 2019:1–8. doi:10.1080/17483107.2019.1602853
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
