Back to Journals » International Journal of General Medicine » Volume 15
PFAPA Syndrome: Clinical, Laboratory and Therapeutic Features in a Single-Centre Cohort
Authors Lazea C , Damian L , Vulturar R, Lazar C
Received 15 May 2022
Accepted for publication 26 July 2022
Published 29 August 2022 Volume 2022:15 Pages 6871—6880
DOI https://doi.org/10.2147/IJGM.S373942
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Cecilia Lazea,1 Laura Damian,2 Romana Vulturar,3 Calin Lazar1
1Department Pediatrics I, University of Medicine and Pharmacy “Iuliu Hatieganu”, Cluj-Napoca, Romania; 2Department of Rheumatology, County Emergency Clinical Hospital Cluj-Napoca, Centre for Rare Musculoskeletal Autoimmune and Autoinflammatory Diseases, Cluj-Napoca, Romania; 3Department of Molecular Sciences, University of Medicine and Pharmacy “Iuliu Hatieganu”, Cluj-Napoca, Romania
Correspondence: Cecilia Lazea, Department Pediatrics I, University of Medicine and Pharmacy “Iuliu Hatieganu”, 68, Motilor street, Cluj-Napoca, 400370, Romania, Email [email protected]; [email protected]
Objective: The aim of this study is to describe a group of Romanian children with periodic fever, aphthous stomatitis, pharyngitis and cervical adenitis (PFAPA) syndrome.
Materials: This consisted of 39 children diagnosed with PFAPA syndrome according to Thomas’ criteria (eight patients with an age at diagnosis < 1 year and 31 patients with an age at diagnosis > 1 year).
Methods: Retrospective analysis of the patients with PFAPA syndrome was focused on clinical features, laboratory findings and therapeutic methods. Comparison between the two groups divided by age at onset was also investigated.
Results: Median age at onset was 1.58 years, and median age at diagnosis was 2.97 years. The mean interval between episodes was 35.5 days and the mean duration per febrile episode was 4.1 days. The median diagnosis delay was 2.42 years. The patients presented pharyngitis (100%), adenitis (94.8%) and aphthous lesions (66.7%). The frequency of febrile attacks was higher in children with an age at diagnosis under 1 year (p = 0.0287). Younger age was associated with the presence of aphthae. The mean value of C-reactive protein (CRP) was 7.9mg/dl and the mean value of leucocytes was 14,839/mm3. In 95% of patients given oral corticosteroids, remission of symptoms was reported within 24 h. In three patients, tonsillectomy was performed with complete remission of the disease.
Conclusion: We present a cohort of children with PFAPA syndrome, with clinical and laboratory features similar to those described in the literature. Febrile attacks had a higher incidence in children with younger age at the onset of the disease. The patients had a favorable response to corticosteroids.
Keywords: PFAPA syndrome, periodic fever, child
Introduction
Periodic fever, aphthous stomatitis, pharyngitis and cervical adenitis (PFAPA) syndrome or Marshall syndrome are characterized by recurrent episodes of fever lasting for a few days with a recurrence at every 3–8 weeks, associated with at least one of three main signs: aphthous stomatitis, cervical adenitis and pharyngitis.1 The fever episodes have little or no response to common antipyretics. Patients are asymptomatic between episodes and their growth and development are normal.2–4 Other symptoms which can be present during fever attacks include headache, joint pain, myalgia, nausea, vomiting and abdominal pain. The onset is early, usually before school age, and usually lasts up to the age of 10–11 years, but there are some cases diagnosed in adults.5 It is a self-limited disease with no sequels, but the recurrent episodes of fever affect daily life of the whole family. Although PFAPA syndrome is the most common cause of recurrent fever in children, the real incidence of the disease is unknown because the diagnosis is rarely established, and the children are given repeated unnecessary antibiotics because of the common misdiagnosis as bacterial tonsillitis. In recent years, awareness among clinicians has increased the rate of diagnosis. Initially, PFAPA syndrome was considered a sporadic disease, but several case studies have reported familial clustering, suggesting a possible hereditary component.6,7 The genetic origin of PFAPA syndrome is a matter of debate, with several studies suggesting that inflammasome-related genes might be involved in this autoinflammatory syndrome.8–13 The pathogenesis is not known exactly, but a defect in the regulation of the inflammatory response by innate immune pathways and adaptive immune response are involved, as suggested by activation of Th1 of CD4+ cells.14 Studies on cytokines have revealed a significant increase of serum pro-inflammatory cytokine levels during the flares, a reduction of anti-inflammatory cytokine levels and a dysregulation of IL-1b monocyte production, which has a pivotal role.11,15,16 Interference with monomeric CRP’s anti-inflammatory effect activity and significant alteration of neutrophil functions have also been described.17
There are no diagnostic tests for PFAPA syndrome. The diagnosis is established on clinical criteria and on exclusion of other possible causes of recurrent fever in children. During febrile attacks, elevation of white blood cells, with preponderance of neutrophils and of acute phase reactants, are present. Usually, procalcitonin does not increase during fever attacks.8–11 Between attacks, all inflammatory parameters are normal. Current treatment of PFAPA includes corticosteroids in acute episodes and tonsillectomy, but there is not a consensus due to a lack of large clinical trials.18,19
The aim of this study was to describe the demographic, clinical and laboratory characteristics of a cohort of Romanian children diagnosed with PFAPA syndrome.
Materials and Methods
Study Design
This was a monocentric, retrospective, observational and analytical cohort study. We reviewed the medical records of the patients diagnosed with PFAPA in the last 8 years.
Study Population
From a group of 44 patients diagnosed in our centre with PFAPA syndrome, 39 patients met the criteria for inclusion in this study. Depending on age of onset of the symptoms, the patients were divided into two groups: group 1 – patients with age at onset below 1 year (8 patients) and group 2 – patients with age at onset above 1 year (31 patients).
Methods
Criteria for inclusion in the study were:
- diagnosis of PFAPA syndrome established according to Thomas’ criteria:2 regularly recurrent fever, absence of upper respiratory tract infection and at least one of the following clinical signs: pharyngitis, aphthous stomatitis or cervical adenitis
- completely asymptomatic intervals between febrile episodes
- normal growth and development
Exclusion criteria were:
- patients with proven recurrent respiratory or urinary tract infections
- patients with suspected hereditary periodic fever syndromes
- patients with cyclic neutropenia
The study protocol was as follows:
- medical interview: demographic data, medical history of patients and their families, characteristics of febrile episodes
- laboratory tests during febrile episodes before corticosteroid administration and during asymptomatic intervals (peripheral leukocyte counts, haemoglobin, thrombocytes, C-reactive protein, erythrocyte sedimentation rate, procalcitonin, immunoglobulins)
- viral studies (Epstein–Barr virus, cytomegalovirus)
- culture: throat, urine, blood
- treatment: Prednisone 0.5mg/kg/dose within up to 24 h from fever onset and/or tonsillectomy
- observing response to corticosteroids in the first 24 h after administration, the change in febrile episode periodicity after corticosteroid administration, and the efficacy of the tonsillectomy regarding the reappearance or persistence of febrile episodes
- 12 months of follow-up
Statistical Analysis
Statistical analyses were performed using the MedCalc® Statistical Software version 19.6 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2020).
Data were analysed using Student’s t-test for comparison of quantitative variables and the Chi-Square test for qualitative variables. A p value below 0.05 was considered significant and below 0.01 was considered highly significant.
Ethics Statement
Written informed consent was obtained from guardians of paediatric patients, and the study followed the ethical guidelines of the Declaration of Helsinki and the ethical standards of the national research committee. The study protocol was approved by the Medical Ethics Committee of the University of Medicine and Pharmacy Cluj-Napoca (110/2022).
Results
Group Characteristics
A total number of 39 patients with PFAPA syndrome were included in this study, of whom 22 (56.4%) were males.
Clinical Findings
Detailed clinical characteristics of the patients are presented in Table 1.
 |
Table 1 Clinical Characteristics of PFAPA Episodes |
The most frequent symptom was pharyngitis, which was present in all patients, followed by cervical adenopathy (94.8%) and aphthous stomatitis (66.7%). Associated symptoms were abdominal pain (23.1%), vomiting (10.2%), diarrhoea (7.7%), headache (5.1%) and arthralgia (5.1%) – (Figure 1). In 17.9% of patients, pharyngeal exudates were found. Twenty-five patients (64.1%) presented all three cardinal symptoms of the disease (fever, pharyngitis and aphthous lesions). Maintenance of normal findings in afebrile intervals was present in all patients.
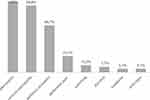 |
Figure 1 Clinical findings during PFAPA flares. |
The presence of aphthous lesions was associated with duration of fever (p = 0.0019) and maximal temperature (p = 0.0284). The age at onset was positively correlated with the median periodicity of episode occurrence (p = 0.0023). Comparative clinical data between group 1 (patients with age at onset below 1 year) and group 2 (patients with age at onset above 1 year) are presented in Table 2.
 |
Table 2 Clinical Characteristics of PFAPA Episodes Depending on Age at Onset |
A number of 12 patients (30.8%) presented comorbidities: six patients (15.4%) – allergy, two patients (5.1%) – febrile seizures, two patients (5.1%) – obesity, one patient (2.6%) –anaemia, one patient (2.6%) – pulmonary stenosis and one patient (2.6%) – hypercholesterolemia.
Family History
The family medical history of the patients revealed recurrent fever and pharyngitis (in first and second-degree relatives) in four patients (10.2%) and autoimmune diseases in five patients (12.8%).
Laboratory Findings
Findings of laboratory data during PFAPA flares and inter-episode periods are presented in Table 3.
 |
Table 3 Laboratory Findings During PFAPA Flares and Inter-Episode Periods |
Statistically significant differences between the acute phase and the inter-episode period were recorded for the value of leukocytes, neutrophils, monocytes, hemoglobin, thrombocytes, ESR and CRP. Procalcitonin had normal values in all children during flares. Test for anti-streptolysin antibody was negative in all children. All patients had normal values of immunoglobulins.
Treatment
Twenty-three patients (59%) received oral corticosteroids (Prednisone one dose 0.5mg/kg) during febrile episodes. In 95% of the patients, the fever disappeared within 24 h of administration. After corticosteroid administration, in 35% of cases the febrile flares appeared more frequently, in 52% of cases the frequency of occurrence has not changed and in 13% of cases the flares appeared less often. Three cases (7.7%) underwent tonsillectomy with complete resolution of symptoms.
Discussion
In the present study, we report the clinical and laboratory characteristics of 39 children diagnosed with PFAPA syndrome. Previously, only small studies of children with PFAPA syndrome have been published in Romania and to our knowledge this is the largest study cohort of such patients. PFAPA syndrome is the most frequent autoinflammatory disorder with an episodic nature and periodicity, due to the activation of innate immune pathways during flares, with unknown real incidence and incompletely elucidated pathogenesis. The diagnosis of this disease is based on clinical findings and an age of the onset earlier than 5 years of age is considered an important diagnostic criterion, although there are studies describing a later onset of the symptoms.20–26
Group Characteristics
In our cohort, the male-to-female ratio was 1.3:1, which aligns to other studies which have reported that incidence in males is higher than in females (range 53–71%).27–33
Clinical Findings
The median age of first manifestation in our group was 1.58 years, in line with data from the literature, which supports the onset of the disease before the age of 5 years. Median time between the onset of the disease and diagnosis was 2.4 years, longer than reported by most of other studies, but not unprecedented.37,38 This long duration between the onset of the diseases and diagnosis should raise awareness among healthcare professionals. The delay in the diagnosis of PFAPA is evidence of the tendency to underdiagnose this disease, and during this period, these children underwent repeated unnecessary antibiotic treatments (which can lead to complications) because the disease is commonly confounded with bacterial tonsillitis.29
The main role in the diagnosis of these children belongs to the family physicians and paediatricians who first examine these patients and to ENT specialists who require thorough knowledge of this disease.
Regarding the differences between the two groups divided by age at onset, in group 1 (age at onset <1 year) the diagnosis was established earlier than group 2 (age at onset >1 year), most likely because recurrent fever in infants (who do not yet attend the nursery and as a consequence are without a reliable source of recurrent respiratory infections) raises the suspicion of autoinflammatory disease; for this reason, these children are referred to paediatric, immunologic or rheumatologic consultation. Furthermore, a higher rate of publications regarding this disorder and greater familiarity with this disease have reduced the delay in diagnosis in recent years.
The mean duration of fever episodes (4.1 days) and the mean interval between flares (5 weeks) resembles those described by other studies.27,33,34,37,39 In our cohort, the younger the age at diagnosis, the shorter the asymptomatic interval between flares (27 days vs 38 days), another finding that has been reported by other studies.39,40 On the other hand, a comparison between the clinical presentation of paediatric and adult patients with PFAPA has found that the frequency of the flares was significantly higher in paediatric cases, while febrile attack duration was significantly longer in adults.22,41
The frequency of characteristic symptoms in our group showed higher incidence of cervical adenitis and aphthous stomatitis. An explanation of this finding may be that the diagnosis in our group was made using classical criteria. Recent publications have proposed simplified criteria consisted of regular fever episodes without any other explanation, even in the absence of pharyngitis, aphthous stomatitis or cervical adenitis, and also in children older than 5 years.42 An online survey for paediatric rheumatologists and infectious disease specialists assessing PFAPA diagnostic criteria has shown that signs of aphthous stomatitis, adenitis, or pharyngitis are not required as long as regular fever episodes with asymptomatic intervals between episodes and normal growth and development are present.43 Erythematous pharyngitis was present in all our patients and exudative pharyngitis in 18%. Other studies have reported exudative pharyngitis in 37.5–66%.20,38,39,44 The three major signs were all present in 67% of our patients, exceeding the incidence reported from other studies (27–53%), most likely because the diagnosis in our group was made using the classic criteria.29,32
A novel finding of this study was association of the aphthous lesions with duration of fever (p = 0.0019) and maximal temperature (p = 0.0284).
Other than main diagnostic features were present in 43.5% of patients and this finding suggests the variability of presentation of this disorder. This finding is confirmed by other studies (Table 3). Compared to other studies, we have found myalgia, arthralgia and headache in a smaller proportion of patients, supported by the smaller median age of our patients. A comprehensive comparison between paediatric and adult patients with PFAPA found that joint symptoms, myalgia, headache and rashes were more common in adults.3,41
The analysis of comorbidities revealed that the most frequently associated disease was allergy, in 15.4% of patients, in line with other studies which revealed an incidence between 18.3% and 39%.29,34
Family History
A family history of recurrent pharyngitis (in first or second-degree relatives) in our group was lower (10.2%) than in other studies which noted a higher incidence (range between 23% and 52%).31–35 A previous case–control study comparing the family history of PFAPA patients with healthy controls subjects found that first-degree relatives (parents and siblings) of patients with PFAPA syndrome have a higher prevalence of recurrent pharyngitis and aphthous stomatitis than relatives of control subjects, suggesting that these disorders could represent reduced penetrance phenotypes of PFAPA determined by an inherited genetic predisposition and/or common environmental exposure.35 These findings raise the possibility of the involvement of genetic factors in PFAPA syndrome etiopathogenesis. A genome-wide linkage study performed in seven families with PFAPA syndrome revealed the absence of a unique gene that was mutated in all the affected individuals, suggesting the absence of genetic homogeneity for this disorder.12 Another debated pathogenetic hypothesis originating in overlapping between the PFAPA syndrome and mild forms of autoinflammatory diseases was based on changes in inflammatory genes, but the frequencies of these variants are not different from those that are present in the general population. This suggests that the pathogenesis of this disorder could be multifactorial or polygenic in which an environmental trigger provokes inflammasome activation resulting in PFAPA flares.9,12,20,36
Laboratory Findings
No specific diagnostic tests for PFAPA are available, during flares, so the major problem of diagnosis is to differentiate between a PFAPA attack and an infectious febrile disease.
Elevation of inflammatory parameters and normal values of procalcitonin during flares was present in our group, and these findings are consistent with previously published data.39,40,45–48 Many studies have found that the level of procalcitonin during episodes of PFAPA is lower compared to bacterial infections, and this finding may be useful in distinguishing febrile episodes of PFAPA from bacterial infections in children.47–50
Complete blood cell counts during febrile episodes in our cohort revealed a raising of leucocyte, neutrophil and monocyte levels, as well as the reduction of thrombocytes. Eosinophils and lymphocytes had reduced values during the flares compared to the afebrile period, but the differences were not statistically significant. Oscillations in the concentration of blood cells during the afebrile and febrile phases have been described in other studies.40,41,45,46,51 A slight reduction of hemoglobin during febrile attacks compared to the afebrile period was observed in our cohort, concordant to other studies.28,40 These findings could be determined by the IL-1 production with a pivotal role in PFAPA pathogenesis, which has an effect on hematopoiesis, with increased myeloid cell production with concomitant decrease in lymphoid and erythrocyte cell production.52 Elevation of IL-1 level under acute inflammatory conditions promotes platelet release.53 On the other hand, megakaryocytes act as immune cells and promote systemic inflammation through microparticles rich in IL-1.54
Significant alterations of the neutrophil functions were demonstrated during febrile attacks, including increased intracellular oxygen radical production and apoptosis,55 and could be explained as an imbalance between the free radical production and the capacity of antioxidant defense mechanisms.56 Normal values of quantitative immunoglobulins have been reported by other studies.27,31,38 None of our patients had elevated levels of IgD, although other studies claimed that raised IgD levels may represent a non-specific epiphenomenon, which may accompany PFAPA syndrome and mevalonate kinase deficiency.38,57
Treatment
Corticosteroid administration (a single dose of Prednisone 0.5mg/kg at fever onset) was the most frequent therapeutic option in our group and resulted in rapid resolution of fever in 62% of patients and disappearance of fever within 24 hours in 95% of cases. Administration of oral corticosteroids did not, however, prevent subsequent episodes of fever and did not change the course of the disease.28 The response rate to a single dose of corticosteroid is different in numerous studies, varying between 63% and 84%. In 13% of patients receiving corticosteroids, the febrile recurrences occurred at longer intervals and in 35% of these the flairs appeared more often. In other studies, the percentage of patients whose duration between febrile attacks was shorter varied between 19 and 75%.27,29,38 Despite this inconvenient finding, the administration of corticosteroids can mitigate the consequences of flares and is preferred by the families of these patients for controlling febrile episodes in certain circumstances of social importance. Although PFAPA syndrome is considered a benign condition with spontaneous resolution, most often it is associated with a considerable burden for the child and the parents in their daily activities.58,59 Colchicine was not used in our study group, although other studies reported its efficiency.32,60,61
Tonsillectomy was performed in only 3 children with total remission of the symptoms. This was indicated in children with very frequent flares after the administration of corticosteroids and prolonged symptoms. In general, the parents of our patients were wary of the tonsillectomy proposal and this is an additional reason for the low number of tonsillectomies in our group. The role of tonsillectomy in PFAPA syndrome is controversial. The arguments for tonsillectomy are prevention of the recurrence of further episodes, reducing the severity of the clinical manifestations, and inducing complete remission. Tonsillectomy is advocated against by the spontaneous resolution of PFAPA syndrome and possible relapses after a period of remission, so this decision must be carefully evaluated considering the intensity and frequency of febrile episodes in each child. Therefore, tonsillectomy should be considered in cases of intolerance for or failure of the standard medical treatment.
Our study has several limitations. Firstly, this is a retrospective study which implies variability of the data presented in the medical records. Secondly, we did not perform genetic tests in order to rule out other identifiable causes of periodic fever. A third limitation is the short period of follow-up.
Conclusions
We conclude that although PFAPA syndrome was described more than 30 years ago, its diagnosis is difficult and very often delayed. PFAPA syndrome is a benign but troublesome disease. A single dose of corticosteroids is effective in controlling symptoms. Careful medical history, detailed analysis of the clinical features, asymptomatic intervals between flares, laboratory tests that exclude other conditions, and abortion of episodes after a single dose of corticosteroids could represent a simple algorithm of diagnosis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Marshall GS, Edwards KM, Butler J, Lawton AR. Syndrome of periodic fever, pharyngitis, and aphthous stomatitis. J Pediatr. 1987;110:43–46. doi:10.1016/s0022-3476(87)80285-8
2. Thomas KT, Feder HM, Lawton AR, Edwards KM. Periodic fever syndrome in children. J Pediatr. 1999;135:15–21. doi:10.1016/s0022-3476(99)70321-5
3. Padeh S, Stoffman N, Berkun Y. Periodic fever accompanied by aphthous stomatitis, pharyngitis and cervical adenitis syndrome (PFAPA syndrome) in adults. Isr Med Assoc J. 2008;10:358–360.
4. Cochard M, Clet J, Le L, et al. PFAPA syndrome is not a sporadic disease. Rheumatology. 2010;49:1984–1987. doi:10.1093/rheumatology/keq187
5. Cattalini M, Soliani M, Rigante D, et al. Basic characteristics of adults with periodic fever, aphthous stomatitis, pharyngitis and adenopathy syndrome in comparison with typical pediatric expression of the disease. Mediators Inflamm. 2015;2015:570418. doi:10.1155/2015/570418
6. Sampaio ICRM, Rodrigo MJ, Monteiro Marques JGDP. Two siblings with periodic fever, aphthous stomatitis, pharyngitis, adenitis (PFAPA) syndrome. Pediatr Infect Dis J. 2009;28(3):254–255. doi:10.1097/INF.0b013e31818c8ea5
7. Valenzuela P, Majerson D, Tapia JL, Talesnik E. Syndrome of periodic fever, aphthous stomatitis, pharyngitis and adenitis (PFAPA) in siblings. Clin Rheumatol. 2009;28:1235–1237. doi:10.1007/s10067-009-1222-z
8. Akelma AZ, Cizmeci MN, Kanburoglu MK, et al. Is PFAPA syndrome really a sporadic disorder or it is genetic? Med Hypotheses. 2013;81(2):279–281. doi:10.1016/j.mehy.2013.04.030
9. Dagan E, Gershoni-Baruch R, Khatib I, Mori A, Brik R. MEFV, TNF1rA, CARD15 and NLRP3 mutations in PFAPA. Rheumatol Int. 2010;30:633–636. doi:10.1007/s00296-009-1037-x
10. Berkun Y, Levy R, Hurwitz A, et al. The familial Mediterranean fever gene as a modifier of periodic fever, aphthous stomatitis, pharyngitis, and adenopathy syndrome. Semin Arthritis Rheum. 2011;40(5):467–472. doi:10.1016/j.semarthrit.2010.06.009
11. Kolly L, Busso N, von Scheven-Gete A, et al. Periodic fever, aphthous stomatitis, pharyngitis, cervical adenitis syndrome is linked to dysregulated monocyte IL-1β production. J Allergy Clin Immunol. 2013;131:1635–1643. doi:10.1016/j.jaci.2012.07.043
12. Di Gioia SA, Bedoni N, von Scheven-Gête A, et al. Analysis of the genetic basis of periodic fever with aphthous stomatitis, pharyngitis, and cervical adenitis (PFAPA) syndrome. Sci Rep. 2015;5:10200. doi:10.1038/srep10200
13. Cheung MS, Theodoropoulou K, Lugrin J, Martinon F, Busso N, Hofer M. Periodic fever with aphthous stomatitis, pharyngitis, and cervical adenitis syndrome is associated with a CARD8 variant unable to bind the NLRP3 inflammasome. J Immunol. 2017;198:2063–2069. doi:10.4049/jimmunol.1600760
14. Glomba-Kraszewska B, Matkowska-Kocjan A, Szenborn L. The pathogenesis of periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis syndrome: a review of current research. Mediators Inflamm. 2015;2015:563876. doi:10.1155/2015/563876
15. Stojanov S, Hoffmann F, Kéry A, et al. Cytokine profile in PFAPA syndrome suggests continuous inflammation and reduced anti-inflammatory response. Eur Cytokine Netw. 2006;17:90–97.
16. Stojanov S, Lapidus S, Chitkara P, et al. Periodic fever, aphthous stomatitis, pharyngitis, and adenitis (PFAPA) is a disorder of innate immunity and Th1 activation responsive to IL-1 blockade. Proc Natl Acad Sci USA. 2011;108:7148–7153. doi:10.1073/pnas.1103681108
17. Kraszewska-Głomba B, Myszka M, Krajewska M, Szenborn L. High prevalence of autoantibodies against monomeric C Reactive Protein (CRP) in children with PFAPA syndrome. J Med Biochem. 2018;37:507–509. doi:10.1515/jomb-2017-0066
18. Amarilyo G, Rothman D, Manthiram K, et al.; CARRA PFAPA Consensus Treatment Plan Workgroup. Consensus treatment plans for periodic fever, aphthous stomatitis, pharyngitis and adenitis syndrome (PFAPA): a framework to evaluate treatment responses from the childhood arthritis and rheumatology research alliance (CARRA) PFAPA work group. Pediatr Rheumatol Online J. 2020;18:31. doi:10.1186/s12969-020-00424-x
19. Vanoni F, Theodoropoulou K, Hofer M. PFAPA syndrome: a review on treatment and outcome. Pediatr Rheumatol Online J. 2016;14:38. doi:10.1186/s12969-016-0101-9
20. Gattorno M, Caorsi R, Meini A, et al. Differentiating PFAPA syndrome from monogenic periodic fevers. Pediatrics. 2009;124:e721–e728. doi:10.1542/peds.2009-0088
21. Vanoni F, Federici S, Antón J, et al.; for Eurofever and the Paediatric Rheumatology International Trials Organisation (PRINTO). An international delphi survey for the definition of the variables for the development of new classification criteria for periodic fever aphtous stomatitis pharingitis cervical adenitis (PFAPA). Pediatr Rheumatol Online J. 2018;16:27. doi:10.1186/s12969-018-0246-9
22. Cantarini L, Vitale A, Sicignano LL, et al. Diagnostic criteria for adult-onset Periodic Fever, Aphthous Stomatitis, Pharyngitis, and Cervical Adenitis (PFAPA) Syndrome. Front Immunol. 2017;8:1018. doi:10.3389/fimmu.2017.01018
23. Sicignano LL, Rigante D, Moccaldi B, et al. Children and adults with PFAPA syndrome: similarities and divergences in a real-life clinical setting. Adv Ther. 2021;38:1078–1093. doi:10.1007/s12325-020-01576-8
24. Marques DP, Rocha S, Manso M, Domingos R. Periodic fever with pharyngitis, aphthous stomatitis and cervical adenitis syndrome: a rare cause of fever in adults. Eur J Case Rep Intern Med. 2019;6:001041. doi:10.12890/2019_001041
25. Alam F, Hammoudeh M. An underlooked cause of Periodic Fever (PFAPA) in an adult patient with no response to tonsillectomy. Case Rep Rheumatol. 2018;2018:6580835. doi:10.1155/2018/6580835
26. Yamahara K, Egawa Y, Lee K, Nakashima N, Ikegami S. A case of Adult-Onset Periodic Fever, Aphthous Stomatitis, Pharyngitis, and Cervical Adenitis (PFAPA) syndrome responsive to tonsillectomy in Japan. Case Rep Otolaryngol. 2019;2019:1746180. doi:10.1155/2019/1746180
27. Feder HM, Salazar JC. A clinical review of 105 patients with PFAPA (a periodic fever syndrome). Acta Paediatr. 2010;99(2):178–184. doi:10.1111/j.1651-2227.2009.01554.x
28. Padeh S, Brezniak N, Zemer D, et al. Periodic fever, aphthous stomatitis, pharyngitis, and adenopathy syndrome: clinical characteristics and outcome. J Pediatr. 1999;135:98–101. doi:10.1016/s0022-3476(99)70335-5
29. Tasher D, Somekh E, Dalal I. PFAPA syndrome: new clinical aspects disclosed. Arch Dis Child. 2006;91:981–984. doi:10.1136/adc.2005.084731
30. Mehregan FF, Ziaee V, Ahmadinejad Z, Tahghighi F, Sabouni F, Moradinejad MH. Periodic Fever, Aphthous Stomatitis, Pharyngitis and Cervical Adenitis (PFAPA) syndrome in Iranian Children First Report of Iranian Periodic Fever and Autoinflammatory Registry (IPFAIR). Iran J Pediatr. 2014;24:598–602.
31. Perko D, Debeljak M, Toplak N, Avčin T. Clinical features and genetic background of the periodic fever syndrome with aphthous stomatitis, pharyngitis, and adenitis: a single center longitudinal study of 81 patients. Mediators Inflamm. 2015;2015:293417. doi:10.1155/2015/293417
32. Batu ED, Kara Eroğlu F, Tsoukas P, et al. Periodic fever, aphthosis, pharyngitis, and adenitis syndrome: analysis of patients from two geographic areas. Arthritis Care Res. 2016;68:1859–1865. doi:10.1002/acr.22901
33. Costagliola G, Maiorino G, Consolini R. Periodic Fever, Aphthous Stomatitis, Pharyngitis, and Cervical Adenitis Syndrome (PFAPA): a clinical challenge for primary care physicians and rheumatologists. Front Pediatr. 2019;7:277. doi:10.3389/fped.2019.00277
34. Wurster VM, Carlucci JG, Feder HM, Edwards KM. Long-term follow-up of children with periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis syndrome. J Pediatr. 2011;159:958–964. doi:10.1016/j.jpeds.2011.06.004
35. Manthiram K, Nesbitt E, Morgan T, Edwards KM. Family history in Periodic Fever, Aphthous Stomatitis, Pharyngitis, Adenitis (PFAPA) syndrome. Pediatrics. 2016;138:e20154572. doi:10.1542/peds.2015-4572
36. Asna Ashari K, Rezaei N. PFAPA (periodic fever, aphthous stomatitis, pharyngitis, and adenitis) syndrome: an overview of genetic background. Clin Rheumatol. 2021;40(11):4437–4444. doi:10.1007/s10067-021-05770-z
37. Sampaio I, Marques JG. Síndrome PFAPA (febre periódica, estomatite aftosa, faringite, adenite): análise retrospectiva de 21 casos [Periodic fever with aphthous stomatitis, pharyngitis and adenitis: report of 21 cases]. Acta Med Port. 2011;24:37–42. doi:10.20344/amp.345
38. Kyvsgaard N, Mikkelsen T, Korsholm J, Veirum JE, Herlin T. Periodic fever associated with aphthous stomatitis, pharyngitis and cervical adenitis. Dan Med J. 2012;59:A4452.
39. Hofer M, Pillet P, Cochard MM, et al. International periodic fever, aphthous stomatitis, pharyngitis, cervical adenitis syndrome cohort: description of distinct phenotypes in 301 patients. Rheumatology. 2014;53:1125–1129. doi:10.1093/rheumatology/ket460
40. Ibáñez Alcalde MLM, Caldevilla Asenjo L, Calvo Rey C, et al. Characteristics and disease course in a cohort of children with PFAPA syndrome in the community of Madrid, Spain. Reumatol Clin. 2019;15:355–359. doi:10.1016/j.reuma.2017.10.015
41. Rigante D, Vitale A, Natale MF, et al. A comprehensive comparison between pediatric and adult patients with periodic fever, aphthous stomatitis, pharyngitis, and cervical adenopathy (PFAPA) syndrome. Clin Rheumatol. 2017;36:463–468. doi:10.1007/s10067-016-3317-7
42. Renko M, Lantto U, Tapiainen T. Towards better diagnostic criteria for periodic fever, aphthous stomatitis, pharyngitis and adenitis syndrome. Acta Paediatr. 2019;108:1385–1392. doi:10.1111/apa.14792
43. Manthiram K, Li SC, Hausmann JS, et al.; Childhood Arthritis and Rheumatology Research Alliance (CARRA) PFAPA Subcommittee. Physicians’ perspectives on the diagnosis and management of periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis (PFAPA) syndrome. Rheumatol Int. 2017;37:883–889. doi:10.1007/s00296-017-3688-3
44. Król P, Böhm M, Sula V, et al. PFAPA syndrome: clinical characteristics and treatment outcomes in a large single-centre cohort. Clin Exp Rheumatol. 2013;31:980–987.
45. Førsvoll JA, Oymar K. C-reactive protein in the periodic fever, aphthous stomatitis, pharyngitis and cervical adenitis (PFAPA) syndrome. Acta Paediatr. 2007;96:1670–1673. doi:10.1111/j.1651-2227.2007.00499.x
46. Yazgan H, Keleş E, Yazgan Z, Gebeşçe A, Demirdöven M. C-reactive protein and procalcitonin during febril attacks in PFAPA syndrome. Int J Pediatr Otorhinolaryngol. 2012;76:1145–1147. doi:10.1016/j.ijporl.2012.04.022
47. Yoshihara T, Imamura T, Yokoi K, et al. Potential use of procalcitonin concentrations as a diagnostic marker of the PFAPA syndrome. Eur J Pediatr. 2007;166:621–622. doi:10.1007/s00431-006-0281-2
48. Kraszewska-Głomba B, Szymańska-Toczek Z, Szenborn L. Procalcitonin and C-reactive protein-based decision tree model for distinguishing PFAPA flares from acute infections. Bosn J Basic Med Sci. 2016;16:157–161. doi:10.17305/bjbms.2016.974
49. Lazea C, Manasia R, Lazăr C, Damian L. Procalcitonin, C-reactive protein and erythrocyte sedimentation rate in periodic fever, aphthous stomatitis, pharyngitis and cervical adenitis (PFAPA syndrome). Romanian J Rheumatol. 2016;25:136–139. doi:10.37897/RJR.2016.3.6
50. Førsvoll JA, Kristoffersen EK, Øymar K. Is there a role for procalcitonin in the evaluation of children with PFAPA syndrome? Ann Pediatr Rhematol. 2012;3:171–175. doi:10.5455/apr.092520121447
51. Brown KL, Wekell P, Osla V, et al. Profile of blood cells and inflammatory mediators in periodic fever, aphthous stomatitis, pharyngitis and adenitis (PFAPA) syndrome. BMC Pediatr. 2010;10:65. doi:10.1186/1471-2431-10-65
52. Pietras EM, Mirantes-Barbeito C, Fong S, et al. Chronic interleukin-1 exposure drives haematopoietic stem cells towards precocious myeloid differentiation at the expense of self-renewal. Nat Cell Biol. 2016;18:607–618. doi:10.1038/ncb3346
53. Haas S, Hansson J, Klimmeck D, et al. Inflammation-induced emergency megakaryopoiesis driven by hematopoietic stem cell-like megakaryocyte progenitors. Cell Stem Cell. 2015;17:422–434. doi:10.1016/j.stem.2015.07.007
54. Cunin P, Nigrovic PA. Megakaryocytes as immune cells. J Leukoc Biol. 2019;105:1111–1121. doi:10.1002/JLB.MR0718-261RR
55. Sundqvist M, Wekell P, Osla V, et al. Increased intracellular oxygen radical production in neutrophils during febrile episodes of periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis syndrome. Arthritis Rheum. 2013;65:2971–2983. doi:10.1002/art.38134
56. Matyas M, Hasmasanu MG, Zaharie G. Antioxidant capacity of preterm neonates assessed by hydrogen donor value. Medicina. 2019;55:720. doi:10.3390/medicina55110720
57. Kovacs L, Hlavatá A, Baldovič M, et al. Elevated immunoglobulin D levels in children with PFAPA syndrome. Neuro Endocrinol Lett. 2010;31:743–746.
58. Sparud-Lundin C, Berg S, Fasth A, Karlsson A, Wekell P. From uncertainty to gradually managing and awaiting recovery of a periodic condition- A qualitative study of parents´ experiences of PFAPA syndrome. BMC Pediatr. 2019;19:99. doi:10.1186/s12887-019-1458-y
59. Grimwood C, Kone-Paut I, Piram M, Rossi-Semerano L, Hentgen V. Health-related quality of life in children with PFAPA syndrome. Orphanet J Rare Dis. 2018;13(1):132. doi:10.1186/s13023-018-0878-3
60. Yıldız M, Haslak F, Adrovic A, et al. Periodic fever, aphthous stomatitis, pharyngitis, and adenitis syndrome: a single-center experience. Turk Arch Pediatr. 2022;57(1):46–52. doi:10.5152/TurkArchPediatr.2021.21229
61. Gunes M, Cekic S, Kilic SS. Is colchicine more effective to prevent periodic fever, aphthous stomatitis, pharyngitis and cervical adenitis episodes in Mediterranean fever gene variants? Pediatr Int. 2017;59(6):655–660. doi:10.1111/ped.13265
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
