Back to Journals » Journal of Pain Research » Volume 17
Perspective on Intradiscal Therapies for Lumbar Discogenic Pain: State of the Science, Knowledge Gaps, and Imperatives for Clinical Adoption
Authors Lorio MP, Tate JL, Myers TJ, Block JE , Beall DP
Received 20 September 2023
Accepted for publication 7 March 2024
Published 18 March 2024 Volume 2024:17 Pages 1171—1182
DOI https://doi.org/10.2147/JPR.S441180
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Krishnan Chakravarthy
Morgan P Lorio,1 Jordan Lee Tate,2 Thomas J Myers,3 Jon E Block,4 Douglas P Beall5
1Advanced Orthopedics, Altamonte Springs, FL, USA; 2Southern Pain and Spine Associates, Jasper, GA, USA; 3Paradigm Health System, Slidell, LA, USA; 4Private Practice, San Francisco, CA, USA; 5Comprehensive Specialty Care, Edmond, OK, USA
Correspondence: Jon E Block, Private Practice, 2210 Jackson Street, Ste. 401, San Francisco, CA, 94115, USA, Tel +1(415) 775-7947, Email [email protected]
Abstract: Specific clinical diagnostic criteria have established a consensus for defining patients with lumbar discogenic pain. However, if conservative medical management fails, these patients have few treatment options short of surgery involving discectomy often coupled with fusion or arthroplasty. There is a rapidly-emerging research effort to fill this treatment gap with intradiscal therapies that can be delivered minimally-invasively via fluoroscopically guided injection without altering the normal anatomy of the affected vertebral motion segment. Viable candidate products to date have included mesenchymal stromal cells, platelet-rich plasma, nucleus pulposus structural allograft, and other cell-based compositions. The objective of these products is to repair, supplement, and restore the damaged intervertebral disc as well as retard further degeneration. In doing so, the intervention is meant to eliminate the source of discogenic pain and avoid surgery. Methodologically rigorous studies are rare, however, and based on the best clinical evidence, the safety as well as the magnitude and duration of clinical efficacy remain difficult to estimate. Further, we summarize the US Food and Drug Administration’s (FDA) guidance regarding the interpretation of the minimal manipulation and homologous use criteria, which is central to designating these products as a tissue or as a drug/device/biologic. We also provide perspectives on the core evidence and knowledge gaps associated with intradiscal therapies, propose imperatives for evaluating effectiveness of these treatments and highlight several new technologies on the horizon.
Keywords: degenerative, disc, intradiscal, autologous, allogeneic, injection, regenerative, discogenic, pain
Introduction
Significant advancements in the pathoanatomical characterization of the degenerative processes of the intervertebral disc have been instrumental in establishing and refining clinical diagnostic criteria specific to patients with lumbar discogenic pain.1–3 Although diagnosis can be difficult, salient features of physical examination have been defined to include axial midline low back pain, sitting intolerance, pain with flexion, positive provocation with sustained hip flexion, absence of motor/sensor/reflex change, and positive discography with or without non-radicular/non-sciatic referred leg pain in a sclerotomal distribution.2,4
In a recently published quantitative evaluation of the global burden of disease, the Institute for Health Metrics and Evaluation (IHME) reported that out of 395 diseases, injuries, and impairments, low back pain was the leading cause of years lived with disability (YLD), responsible for approximately 64 million YLDs or 7.4% of total global YLDs in 2019.1 Estimates suggest that as many as 40% of patients exhibiting persistently severe low back pain have diagnostic signs and symptoms of discogenic origin including imaging evidence of internal disc disruption and other findings associated with annular tearing.5,6
If discogenic low back pain becomes chronic and refractory to conservative medical management, there are few therapeutic options short of surgical discectomy often coupled with total disc arthroplasty or instrumented interbody spine fusion. These options, such as utilizing cell-based and biomaterial engineering therapies to modify the physiology and possibly restore the structure of the degenerated intervertebral disc, may serve to fill the extensive treatment gap between conservative management and traditional spine surgery. Therapeutic candidates including mesenchymal stromal cells (MSCs), platelet-rich plasma (PRP), nucleus pulposus (NP) tissue, and related cell-based agents have been proposed and can be delivered minimally-invasively under fluoroscopic guidance via a needle-based approach.7–15 Both autologous products and their allogeneic analogs have been studied for relief of discogenic pain.14,15 The underlying mechanism of action can involve the differentiation of chondrogenic precursor cells into viable regenerated disc tissue as with the injection of MSCs or the direct implantation of native disc material as with allogeneic NP. Products have ranged from autologous bone marrow aspirate containing a cocktail of pluripotent cell types to various derivatives including commercial formulations with proprietary manufacturing methods.
The overriding challenge for these intradiscal agents to impart a restorative effect lies in the very nature of the intervertebral disc itself. As a result of its distinctly complex developmental origin and tissue composition, the mature intervertebral disc is essentially avascular, aneural, and alymphatic in nature, creating a hostile microenvironment for regeneration to occur and flourish.16–18 Consequently, for an injectable cell product to provide tangible and durable clinical benefit, it will need to embody some or preferably all of a variety of pro-regenerative characteristics to maximize the likelihood of efficacy.19 These characteristics include, but are not limited to, (1) engrafting with a capacity to survive for an adequate period of time to directly contribute to matrix production, (2) having the potential to generate robust paracrine signaling to induce an anabolic switch in native cells to alter their behavior from degeneration to regeneration, (3) support the recruitment of regenerative cell types or otherwise limit the migration of fibrotic/catabolic cells into the disc, and (4) provide intradiscal structural and mechanical support that supplements volume loss and facilitates re-hydration.20
This commentary provides a perspective on the state of the science of intradiscal therapies aimed at ameliorating discogenic low back pain. We address the salient regulatory hurdles as well as the core evidence, knowledge gaps, and imperatives necessary to establish clinical utility.
Regulatory Considerations
As noted, the chemical composition and cellular components proposed for intradiscal therapies have run the gamut from amalgamations of pluripotent cell types to highly specific single-cell formulations focused on a precise differentiation pathway. This range of therapeutic strategy is, in large part, a function of the degree of post-procurement cell and tissue processing. In fact, the amount and type of manipulation of the tissues and cells dictates the commensurate regulatory pathway in the US for intradiscal injectables ranging from minimally-manipulated material regulated as a “tissue” solely under section 361 of the Public Health Service (PHS) Act, and regulations in Title 21 Code of Federal Regulations (CFR) Part 1271, to more highly manipulated material regulated as a drug, device, or biological product regulated under the Federal Food, Drug, and Cosmetic (FD&C) Act and/or section 351 of the PHS Act.21 These distinct regulatory pathways have profoundly different ramifications with respect to establishing product mechanisms of action, performance characteristics, utility, commercial claims, and reimbursement status.
From a US regulatory standpoint, the Food and Drug Administration (FDA) classifies injectable intradiscal therapies collectively as human cells, tissues, and cellular and tissue-based products (HCT/Ps) and has issued specific guidance with respect to the pathway for determining appropriate regulatory oversight.21 The FDA provides guidance documents for the interpretation of minimal manipulation and homologous use criteria and definitions of related key terms, which are central to product classification.
FDA has defined HCT/Ps as “human cells or tissues that are intended for implantation, transplantation, infusion, or transfer into a human recipient”.21 If an HCT/P fails to meet the criteria below and does not qualify for any of the stated exceptions, the HCT/P will be classified as either a drug, device, or biological product and applicable regulations and premarket review and clearance will be required.
An HCT/P is regulated solely under section 361 of the Public Health Service (PHS) Act and Title 21 Code of Federal Regulations (CFR) Part 1271 if it meets all of the following criteria:
For cells or nonstructural tissues, FDA defines minimal manipulation as “processing that does not alter the relevant biological characteristics of cells or tissues”.21 The properties that contribute to the cell or tissue’s basic physiological function are considered relevant biological characteristics. For structural tissues, FDA defines minimal manipulation as”processing that does not alter the original relevant characteristics of the tissue relating to the tissue's utility for reconstruction, repair, or replacment”.
Classification of intradiscal injectables that have undergone minimal manipulation must also correspond with FDA’s definition of homologous use. Specifically, homologous use is defined as the
repair, reconstruction, replacement, or supplementation of a recipient’s cells or tissues with an HCT/P that performs the same basic function or functions in the recipient as in the donor.21
It should be noted that even though autologous bone marrow is a source of hematopoietic progenitor cells, it has distinct regulatory considerations. Minimally manipulated bone marrow for homologous use and not combined with another article (with certain exceptions) is not considered an HCT/P. However, bone marrow that is more than minimally manipulated, intended by the manufacturer for a non-homologous use, or combined with another article with limited exceptions, meets the definition of an HCT/P and is subject to the regulations in 21 CFR Part 1271.
For intradiscal therapies proposed to address lumbar discogenic pain that are in product development, are being tested currently in clinical research trials, or are already commercially available, this regulatory framework has broad implications for indications-for-use and clinical adoption. From one perspective, it may be advantageous to secure classification purely as a “tissue” with minimal manipulation and restricted to homologous use, thereby avoiding FDA oversight and regulatory reporting requirements. Mineralized structural bone allografts supplied by certified bone banks fall into this category, for example, and have a long history of clinical use.
However, cost and effort considerations aside, it may be more valuable to obtain a so-called “regulatory patent” in the form of a biologics license application (BLA) or a premarket approval (PMA) from FDA. This pathway to market provides the benefits of capturing regulated clinical trial data including comparative effectiveness findings that are mandatory in supporting downstream publication dossiers that are necessary for obtaining reimbursement from third party payers and driving clinical adoption. That said, aside from tissue or cellular products that have a long history of homologous use and have been “grandfathered” into the medical delivery system via tissue banks, it is likely that any newly introduced intradiscal therapeutic products will have difficulty meeting FDA’s minimal manipulation clause and, therefore, will be subject to regulations exclusively under 21 CFR Part 1271. Indeed, the processing steps undertaken to inactivate or remove adventitious agents and attenuate antigenic response from an allogeneic tissue or cell source would most likely exceed the threshold for minimal manipulation.
Core Evidence
There have been a large number of pilot investigations of the clinical effectiveness of intradiscal cell-based therapies.7,13 While the findings of most reports suggest a positive treatment effect, their applicability is highly restricted due to extremely low sample sizes (ie, <10 cases) often generated by a single investigator from a single center. These important limitations are further compounded by lack of standardization of the intervention and variable reporting of relevant outcomes such as pain severity and functional improvement. These methodological shortcomings are likely reflective of what might be expected at the advent of any new family of therapeutic interventions, particularly in an unregulated setting. More rarely, there have been reports of initially promising cell-based intradiscal injectables that have failed to induce a durable treatment effect, with the subsequent cessation of trials due to futility.12,22–24
We have summarized below the core evidence for MSCs, PRPs, and NPs drawn from the most methodologically rigorous studies and meta-analyses.
Mesenchymal Stromal Cells
There have been two pivotal trials of the utility of MSCs for treatment of discogenic low back pain.12 Noriega et al25,26 conducted a randomized sham-controlled trial of allogeneic MSCs in 24 patients with over 3 years for post-injection follow-up. The sham consisted of infiltration of the paravertebral musculature with an anesthetic agent. Significant differences were noted between study groups in back pain and functional improvement throughout the follow-up period in favor of MSC treatment. In fact, sham-treated patients continued to demonstrate progressive degradation in all outcomes including structural disc degeneration with increasing Pfirrmann grades on MRI over baseline. In contrast, MSC-treated patients maintained the improved Pfirrmann grades achieved during the initial year after injection.25 This sham-controlled trial included important methodological safeguards such as treatment allocation concealment as well as blinding of patients and assessors to treatment assignment, resulting in a perfect Jadad score of 5. These features minimize both selection and ascertainment bias known to enhance treatment effects inherent in open-label trials.27,28 The authors reported no serious procedure-related adverse events.
In a larger multi-center trial of 100 patients conducted under an FDA investigational new drug (IND) application, Amirdelfan et al29 evaluated the efficacy of allogeneic precursor MSCs in a hyaluronic acid carrier with 3 years of post-injection follow-up. There were two control groups consisting of the hyaluronic acid carrier alone and saline. The proportion of subjects achieving minimally important change (eg, ≥30% for pain VAS) and clinically significant change (eg, ≥50% for pain VAS) composite endpoints was statistically superior for MSC-treated patients compared with controls at multiple follow-up intervals. However, there were no significant differences in structural parameters of disc degeneration using Pfirrmann grades across the study groups. The authors reported two treatment-emergent adverse events that were potentially related to the MSC treatment: one case of severe back pain and one case of implantation site infection.
Platelet-Rich Plasma
Clinical benefits associated with PRP have been modest for discogenic pain with an aggregate success rate for ≥50% back pain reduction of approximately 55% (95% CI: 40–70%) at 6 months follow-up as estimated in a meta-analysis by Schneider et al.13 These mixed efficacy findings were confirmed in additional meta-analyses conducted by Peng et al and Muthu et al9,10 No structural improvements on MRI were noted in any of these systematic reviews, and methodological quality of the included studies was generally weak. These meta-analyses reported no serious procedure-related adverse events associated with intradiscal PRP treatment.
Nucleus Pulposus
To date, the largest study of intradiscal therapies was a multi-center trial involving 218 subjects randomly allocated to receive a single injection of a proprietary allogeneic cellular NP formulation, saline, or non-surgical management.30,31 This study was known as the Viable Allograft Supplemented Disc Regeneration in the Treatment of Patients with Low Back Pain With or Without Disc Herniation (VAST) Trial. At the one-year primary endpoint, there were 54% and 53% improvements in back pain severity and ODI, respectively, after NP treatment. Patients who crossed-over to NP injection from non-surgical management experienced consistently larger improvements: 65% and 64% for pain and ODI. A subsequent post hoc analysis restricted to patients ≤ 42 years of age also demonstrated a statistically significant benefit of NP.32 It should be noted that there was a discernible treatment effect associated with saline injection in this study. This phenomenon has previously been identified in randomized trials of hyaluronic acid injections in the management of knee pain.33–35 It was concluded that saline conveys a beneficial effect over and above that normally prescribed to placebo and, thus, should be considered an “active” control. The authors reported that there were 11 (3.5%) instances of serious procedure-related adverse events in 141 NP-treated patients but none were persistently symptomatic.
Knowledge Gaps
Table 1 summarizes the key knowledge gaps in our understanding of the role and potential benefit of intradiscal therapies in the treatment of discogenic low back pain. We have identified five major areas that would benefit from greater specification, definition, and characterization including, (1) product composition and chemistry, (2) patient-reported outcome measures, (3) mechanism(s) of action, (4) delivery mode, and (5) imaging evaluation.
 |
Table 1 Knowledge Gaps in Characterizing Intradiscal Therapies for Disc Degeneration |
Product composition standardization is vital to manufacture a biochemically consistent commercial product that elicits a uniform cellular and clinical response in the recipient. Numerous MSC formulations tested to date, for example, have been comprised of heterogeneous populations of multipotent progenitor cells derived from a variety of tissues including bone marrow, adipose tissue, peripheral blood, or umbilical cord.11,12 This source procurement variation has been linked to differences in potency and differentiation inclinations.36–38 It is therefore imperative to ascertain which MSC formulation has the most robust capacity for post-injection survival as MSCs subjected to intervertebral disc environmental factors have been associated with a substantial reduction in proliferation and chondrogenic potency.39 This is due, in part, to the immature nature of the MSCs following transplantation and potential migration or leakage out of the intervertebral disc. The latter outcome could potentially give rise to undesired differentiation and tissue formation such as osteophyte formation.40 These issues form a knowledge gap that requires further research.
Formulations of allogeneic NP cells also contain a heterogeneous cell population of native cells residing in the NP including highly differentiated rounded NP cells and undifferentiated progenitor cells. However, unlike MSCs, NP cells are endemic to the intervertebral disc, rendering them likely more adaptive to survival within this inhospitable microenvironment.41 Since NP transplant is directly homologous (ie, disc tissue to disc tissue), product standardization may focus more on donor selection and procurement procedures.
Finally, it is important to characterize the role of carriers and scaffolds such as hydrogels used as delivery vehicles for cell- and tissue-based treatments to support intradiscal cell viability.42 The role of potential biomaterial scaffolds in cell survival, proliferation, and tissue regeneration is currently unknown, necessitating a more thorough investigation.
With respect to the standardization of patient-reported outcomes, we recommend a small, but well-validated, battery of outcome measures that include, at a minimum, low back pain severity, which is the cardinal discogenic symptom as well as corresponding referred leg pain severity, if present. The degree of functional impairment should also be evaluated preferably using the Oswestry Disability Index (ODI). These two outcome measures represent the core instruments for reporting clinical effectiveness findings for study populations. Although not mandatory, it is suggested that a quality-of-life metric be included, such as the SF-12 or the EQ-5D, to support subsequent cost-utility analyses.
While our understanding of pathological disc degeneration is extensive, investigation of the mechanism of action for intradiscal therapies to manage discogenic pain has been limited and, thus, treatment protocols remain correspondingly empiric. As noted previously, cell-based treatments may possess multiple characteristics that impart a beneficial effect via biochemical and/or structural pathways that can be identified preliminarily via animal models.19 However, it is crucial to confirm the mechanism of action for each product in humans to account for their unique spinal anatomy, where orthograde posture and obligate bipedalism are antecedent to disc degeneration itself and may compromise product durability.43,44
To date, studies of intradiscal restorative therapies have employed a single bolus injection technique. It is not clear whether this method maximizes efficacy or whether periodic and fractional treatment might afford a greater degree and duration of disc restoration and symptom amelioration. As an example, we currently have limited knowledge of alternative delivery protocols using exact-dosing injection regimens at multiple sites and different locations within the intervertebral disc.
Finally, pre- and post-procedure imaging protocols should be established and standardized to include MRI evaluation of disc structure as well as distinctions among the NP, annulus fibrosus, and disc height/volume based on the grading system and algorithm devised by Pfirrmann et al.45 Additionally, novel functional MRI techniques that allow the evaluation of early disc degeneration based on shifts in proteoglycan content, for example,46 might be useful in the assessment of progression of disc degeneration, and have potential applications in clinical trials to evaluate the efficacy of intradiscal therapies.47 Additionally, the presence and severity of other imaging markers such as vacuum phenomenon, bone marrow, and endplate abnormalities (eg, Modic changes), and disc calcification are important parameters to capture. Finally, provocative or anesthetic discography with concurrent CT scanning is mandatory at baseline to determine the location and extent of avulsions in the fibers of the annulus fibrosus in the form of radial and/or concentric tears and fissures, which are the hallmark of internal disc disruption and help to define patients with discogenic pain.2,48
Imperatives & Future Directions
Clinical Imperatives
Table 2 outlines the most salient clinical imperatives in the reporting of findings associated with intradiscal therapies for lumbar discogenic pain. These recommendations are based, in large part, on foundational research on injectable agents and minimally invasive surgeries used in the treatment of knee osteoarthritis pain.49
 |
Table 2 Clinical Imperatives in the Evaluation of Intradiscal Therapies |
Standardized study endpoints should employ responder rates based on previously specified thresholds and include not only the minimal clinically important difference (MCID) but also, the patient acceptable symptomatic state (PASS), and the substantial clinical benefit (SCB).50 Although frequently absent from published reports of intradiscal therapies, threshold scores are patient-level metrics and must be reported as the percentage of patients who meet or exceed the threshold. A frequently encountered error is presenting whether the mean change score for the study group meets the threshold or not.
By expanding the presentation of patient-reported outcomes beyond traditional reporting, PASS provides the opportunity to address whether patients are satisfied with the intervention and whether they have derived a substantial benefit.49 Indeed, MCID represents only the smallest difference in an outcome that the patient perceives as beneficial. It has become increasingly important, particularly for subjective symptoms such as pain, activity limitations, and participation restrictions, that feeling well rather than feeling better is what matters most to the patient.51
We recommend the inclusion of PASS in outcome reporting, which is a recent concept defined as the highest symptom level below which patients feel well. Only below this threshold is the improvement considered relevant.52 PASS can be presented as responder rates and used as a clinically applicable target for treatment efficacy by clinicians.53 Patients report a major improvement only when they perceive their health state as satisfactory, that is, when they achieve PASS.51,54
SCB represents a stricter-criteria for success than MCID in an attempt to better capture patient satisfaction. For discogenic low back pain or referred leg pain, the validated MCID reflects a ≥ 30% improvement over baseline,55 the SCB is ≥40–50% improvement,56–59 and the PASS threshold is 30–40 mm (100 mm VAS scale) in chronic orthopedic conditions.53 Considering that MCID and SCB responder rate calculations are based on percentage improvements over baseline, we recommend that data capture for pain scores utilizes continuous values as obtained using a VAS instrument. We do not recommend using a numeric pain rating scale (NPRS) as the categorical data do not lend themselves to accurate responder rate estimates when using percentage-based thresholds.
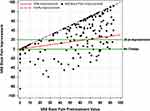
Use of responder rates for primary endpoint analysis, as opposed to showing mean improvements, has been criticized as discarding important individual data regarding the variability in the magnitude of success (or failure). Consequently, we recommend that responder rates also be displayed graphically as a scatterplot of pre-treatment values (x-axis) versus degree of improvement (y-axis) for each outcome (Figure 1). As such, patient success status is computed based on the degree of improvement achieved at follow-up over baseline, and overall responder rate findings can be assessed as to their sensitivity to a fixed success threshold (ie, ≥20 mm VAS) or a variable percentage threshold (ie, ≥30%). Figure 1 illustrates an example of a scatter plot of individual back pain VAS change scores and their distribution around fixed and variable responder rate thresholds.
Future Directions
Based on the rapidly-growing body of evidence on intradiscal therapies, future opportunities for the field appear promising with several new technologies in the product development pipeline ranging from simple to complex. One such candidate undergoing FDA trials is an autologous stem cell product (BRTX-100) where stem cells are harvested directly from the patient and then cultured in hypoxic conditions and re-injected directly into the affected intervertebral disc.
A 404 patient randomized controlled Phase III trial completed as a follow-up to the previously published trial by Amirdelfan et al29 evaluated allogeneic MSCs (Rexlemestrocel-L) in patients with chronic low back pain with patients equally randomized to either a single intradiscal injection of 6 million MSCs with or without a hyaluronic acid (HA) carrier to a saline control. They found a significant improvement in pain in the subjects injected with MSCs plus the HA carrier through 24 months compared with the saline control group with the greatest degree of improvement occurring in patients with a duration of chronic low back pain of less than 68 months. Despite this significant reduction in pain, the primary endpoint of a composite responder analysis of pain and functional improvement did not reach statistical significance at 2 years. Due to this shortfall, an additional Phase III trial is planned comparing an injection of MSCs plus HA to a saline sham procedure.
A Phase I–II trial of an injectable discogenic cellular agent (Rebonuputemcel) showed that with an injection of 9 million cells plus an HA carrier, it resulted in significantly less back pain, greater functional improvement, and better quality of life through the 78-week follow-up. A Phase III trial evaluating the higher effective dose of rebonuputemcel plus HA versus either sham or non-surgical management is planned to begin sometime in early 2024.
The use of allogeneic fibrin injected into the damaged region of the annulus may offer the least complex intradiscal approach to managing discogenic pain (Discseel® Procedure).60 Fibrin, a naturally-occurring protein involved in blood clotting, has a long history of clinical utilization as a tissue sealant or glue. As such, the material is injected intradiscally to provide a physical barrier to catabolic agents and neoinnervation within the interstices of the torn annular fibers. Despite a previous randomized controlled trial including 260 subjects comparing annular injections of fibrin to intradiscal injections of saline where the fibrin sealant did not outperform saline and the data were never published, there are new efforts to identify annular tearing via an annulogram prior to the annular injection of allogeneic fibrin.
There has also been a preliminary evaluation of intradiscal injection of a seven amino acid peptide that has a dual mode of action that modulates TGF-β1 and restores homeostasis in the disc by balancing toward anabolic extracellular matrix regeneration. The TGF-β1 modulation also downregulates IL-6 and nerve growth factor leading to a reduction in back pain. Following a promising Phase IIa trial that showed statistically significant improvements in pain and function through week 24, the Phase IIb trial failed to show significant differences but did show a much greater response for the two highest doses. These doses are currently being tested in a multicenter double-blind, randomized sham-controlled trial (the MODEL trial) comparing the active treatment (SB-01) versus a sham procedure and the results of this trial will likely be available in early 2025.
Early feasibility findings in 20 subjects treated by disc injection with a polymer composite hydrogel (PVA/PEG/PVP/barium sulfate; Hydrafil) showed significant improvements in back pain severity and function through 6 months of follow-up.61 The hydrogel is introduced as a liquid to augment the NP tissue, extend into annular tears, and reinforce the annulus fibrosis. Further clinical study is warranted.
Finally, a novel electroceutical procedure (Discure System) employs a multi-electrode catheter connected to an implantable pulse generator to provide direct intradiscal electrical stimulation in an attempt to increase the osmotic gradient within the degenerated intervertebral disc. Initial pre-clinical evidence using a porcine model demonstrated downregulation of pain markers and proinflammatory factors within damaged discs and exhibited distinct morphological changes histologically and on MRI of extensive annular and nucleus pulposus regeneration.62
Interpretation & Conclusions
Intradiscal therapies have shown great promise in the treatment of lumbar discogenic pain. The primary objective of these interventions is to repair, rejuvenate, and restore the damaged intervertebral disc and, in doing so, eliminate the source of the discogenic pain. That said, disc degeneration is an almost ubiquitous finding with aging in the human spine and the same aberrant biomechanical forces that caused the initial damage still exist. This dilemma poses several important research questions. How long can the effects of a regenerative therapy stave off the inevitable degeneration? Can a re-damaged disc be treated again? Does disc regeneration also slow the progression of arthritic degeneration in adjacent areas of the motion segment, particularly the facet joints?
Due to the methodological shortcomings (ie, small sample sizes, etc.) associated with many of the reports of intradiscal therapies, there has been a clarion call for additional randomized controlled trials (preferably sham-controlled).8,14,15,63 Indeed, the lack of high-grade clinical evidence from trials with a prospective randomized, double-blinded study design is often cited as a primary reason for rejecting proposed therapy advances in orthopedic surgery.64 While we would not argue that randomized sham-controlled trials provide the highest level of clinical evidence, we do not believe that they are necessary to infer safety and effectiveness.65,66 Although percutaneous interventions may be easier to sham than other spinal surgical procedures, we submit that sham-controlled trials are most valuable for interventions where devices are genuinely new and claim to offer measurable therapeutic benefits. When this is not the case, as with many commercially available products that already have regulatory clearance, randomized controlled trials may be inappropriate and wasteful.64 In fact, the majority of randomized interventional trials (~75%) designed to guide clinical practice possess pitfalls that have compromised their ability to do so.67
The expanding use of “big data”, including information gleaned from electronic health records, large observational cohorts, and patient registries, presents unique opportunities to conduct large-scale studies with many of the benefits of randomized trials but without the inherent difficulties.68
In closing, the interest in the development of effective methods to treat intervertebral disc degeneration is genuine and the enthusiasm around the compendium of core evidence generated to date is warranted. However, until further clinical results become available, we believe it is prudent to maintain cautious skepticism about the viability of these products to provide sustained and durable efficacy in the harsh intradiscal microenvironment. As stated herein, we propose a more thorough and comprehensive analysis and standardized presentation of clinical findings, which would measurably assist in validating the clinical utility of these promising interventions.
Data Sharing Statement
Requests for data sharing can be made by contacting the corresponding author. Individual participant data that underlie the results reported in this article will be made available (after deidentification) from 9 to 36 months after article publication. Data sharing will be limited to investigators whose proposed use of the data has been approved by an independent review committee identified for this purpose.
Acknowledgments
We appreciate the scientific review of the text by Timothy Ganey, Ph.D. Financial support for this work was provided by Vivex Biologics (Miami, FL, USA).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
JT reports grants and/or personal fees from Vivex, Mainstay, Abbott, Saluda, and Curonix, during the conduct of the study. JB is an independent advisor to Vivex Biologics and was remunerated for assistance in manuscript development. DPB is a consultant to Mesoblast, DiscGenics, Spine Biorestorative, Orthoson, and Vivex, has received research funding from Mesoblast, Discgenics, Spine Biorestorative, and Vivex, and is on the scientific advisory board of Orthoson, Vivex, and Mesoblast. The authors report no other conflicts of interest in this work.
References
1. Fine N, Lively S, Seguin CA, Perruccio AV, Kapoor M, Rampersaud R. Intervertebral disc degeneration and osteoarthritis: a common molecular disease spectrum. Nat Rev Rheumatol. 2023;19(3):136–152. doi:10.1038/s41584-022-00888-z
2. Lorio MP, Beall DP, Calodney AK, Lewandrowski KU, Block JE, Mekhail N. Defining the patient with lumbar discogenic pain: real-world implications for diagnosis and effective clinical management. J Pers Med. 2023;13(5):821. doi:10.3390/jpm13050821
3. Bogduk N. Degenerative joint disease of the spine. Radiol Clin North Am. 2012;50(4):613–628. doi:10.1016/j.rcl.2012.04.012
4. Bogduk N. On the definitions and physiology of back pain, referred pain, and radicular pain. Pain. 2009;147(1–3):17–19. doi:10.1016/j.pain.2009.08.020
5. Manchikanti L, Singh V, Pampati V, et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4(4):308–316. doi:10.36076/ppj.2001/4/308
6. Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine. 1995;20(17):1878–1883. doi:10.1097/00007632-199509000-00007
7. Her YF, Kubrova E, Martinez Alvarez GA, D’Souza RS. The analgesic efficacy of intradiscal injection of bone marrow aspirate concentrate and culture-expanded bone marrow mesenchymal stromal cells in discogenic pain: a systematic review. J Pain Res. 2022;15:3299–3318. doi:10.2147/JPR.S373345
8. Hickman TT, Rathan-Kumar S, Peck SH. Development, pathogenesis, and regeneration of the intervertebral disc: current and future insights spanning traditional to omics methods. Front Cell Dev Biol. 2022;10:841831. doi:10.3389/fcell.2022.841831
9. Muthu S, Jeyaraman M, Chellamuthu G, Jeyaraman N, Jain R, Khanna M. Does the intradiscal injection of platelet rich plasma have any beneficial role in the management of lumbar disc disease? Global Spine J. 2022;12(3):503–514. doi:10.1177/2192568221998367
10. Peng B, Xu B, Wu W, Du L, Zhang T, Zhang J. Efficacy of intradiscal injection of platelet-rich plasma in the treatment of discogenic low back pain: a single-arm meta-analysis. Medicine. 2023;102(10):e33112. doi:10.1097/MD.0000000000033112
11. Sakai D, Andersson GB. Stem cell therapy for intervertebral disc regeneration: obstacles and solutions. Nat Rev Rheumatol. 2015;11(4):243–256. doi:10.1038/nrrheum.2015.13
12. Sakai D, Schol J, Watanabe M. Clinical development of regenerative medicine targeted for intervertebral disc disease. Medicina. 2022;58(2):267. doi:10.3390/medicina58020267
13. Schneider BJ, Hunt C, Conger A, et al. The effectiveness of intradiscal biologic treatments for discogenic low back pain: a systematic review. Spine J. 2022;22(2):226–237. doi:10.1016/j.spinee.2021.07.015
14. Schol J, Sakai D. Comprehensive narrative review on the analysis of outcomes from cell transplantation clinical trials for discogenic low back pain. N Am Spine Soc J. 2023;13:100195. doi:10.1016/j.xnsj.2022.100195
15. Xie B, Chen S, Xu Y, et al. Clinical efficacy and safety of human mesenchymal stem cell therapy for degenerative disc disease: a systematic review and meta-analysis of randomized controlled trials. Stem Cells Int. 2021;2021:9149315. doi:10.1155/2021/9149315
16. Johnson WE, Caterson B, Eisenstein SM, Hynds DL, Snow DM, Roberts S. Human intervertebral disc aggrecan inhibits nerve growth in vitro. Arthritis Rheum. 2002;46(10):2658–2664. doi:10.1002/art.10585
17. Johnson WE, Caterson B, Eisenstein SM, Roberts S. Human intervertebral disc aggrecan inhibits endothelial cell adhesion and cell migration in vitro. Spine. 2005;30(10):1139–1147. doi:10.1097/01.brs.0000162624.95262.73
18. Kepler CK, Ponnappan RK, Tannoury CA, Risbud MV, Anderson DG. The molecular basis of intervertebral disc degeneration. Spine J. 2013;13(3):318–330. doi:10.1016/j.spinee.2012.12.003
19. Alini M, Diwan AD, Erwin WM, Little CB, Melrose J. An update on animal models of intervertebral disc degeneration and low back pain: exploring the potential of artificial intelligence to improve research analysis and development of prospective therapeutics. JOR Spine. 2023;6(1):e1230. doi:10.1002/jsp2.1230
20. Setton LA, Chen J. Mechanobiology of the intervertebral disc and relevance to disc degeneration. J Bone Joint Surg Am. 2006;88(Suppl 2):52–57. doi:10.2106/JBJS.F.00001
21. Food and Drug Administration. Regulatory Considerations for Human Cells, Tissues, and Cellular and Tissue-Based Products: Minimal Manipulation and Homologous Use. Guidance for industry and Food and Drug Administration staff; 2020.
22. Coric D, Pettine K, Sumich A, Boltes MO. Prospective study of disc repair with allogeneic chondrocytes presented at the 2012 Joint Spine Section Meeting. J Neurosurg Spine. 2013;18(1):85–95. doi:10.3171/2012.10.SPINE12512
23. Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, et al. Lumbar Intradiskal Platelet-Rich Plasma (PRP) injections: a prospective, double-blind, randomized controlled study. PM R. 2016;8(1):1–10; quiz 10. doi:10.1016/j.pmrj.2015.08.010
24. Zielinski MA, Evans NE, Bae H, et al. Safety and Efficacy of platelet rich plasma for treatment of lumbar discogenic pain: a prospective, multicenter, randomized, double-blind study. Pain Physician. 2022;25(1):29–34.
25. Noriega DC, Ardura F, Hernandez-Ramajo R, et al. Treatment of degenerative disc disease with allogeneic mesenchymal stem cells: long-term follow-up results. Transplantation. 2021;105(2):e25–e27. doi:10.1097/TP.0000000000003471
26. Noriega DC, Ardura F, Hernandez-Ramajo R, et al. Intervertebral disc repair by allogeneic mesenchymal bone marrow cells: a randomized controlled trial. Transplantation. 2017;101(8):1945–1951. doi:10.1097/TP.0000000000001484
27. Schulz KF, Chalmers I, Altman DG. The landscape and lexicon of blinding in randomized trials. Ann Intern Med. 2002;136(3):254–259. doi:10.7326/0003-4819-136-3-200202050-00022
28. Schulz KF, Grimes DA. Blinding in randomised trials: hiding who got what. Lancet. 2002;359(9307):696–700. doi:10.1016/S0140-6736(02)07816-9
29. Amirdelfan K, Bae H, McJunkin T, et al. Allogeneic mesenchymal precursor cells treatment for chronic low back pain associated with degenerative disc disease: a prospective randomized, placebo-controlled 36-month study of safety and efficacy. Spine J. 2021;21(2):212–230. doi:10.1016/j.spinee.2020.10.004
30. Beall DP, Davis T, DePalma MJ, et al. Viable Disc tissue allograft supplementation; one- and two-level treatment of degenerated intervertebral discs in patients with chronic discogenic low back pain: one year results of the vast randomized controlled trial. Pain Physician. 2021;24(6):465–477.
31. Beall DP, Wilson GL, Bishop R, Tally W. VAST clinical trial: safely supplementing tissue lost to degenerative disc disease. Int J Spine Surg. 2020;14(2):239–253. doi:10.14444/7033
32. Hunter CW, Guyer R, Froimson M, DePalma MJ. Effect of age on outcomes after allogeneic disc tissue supplementation in patients with chronic discogenic low back pain in the VAST trial. Pain Manag. 2022;12(3):301–311. doi:10.2217/pmt-2021-0078
33. Altman RD, Devji T, Bhandari M, Fierlinger A, Niazi F, Christensen R. Clinical benefit of intra-articular saline as a comparator in clinical trials of knee osteoarthritis treatments: a systematic review and meta-analysis of randomized trials. Semin Arthritis Rheum. 2016;46(2):151–159. doi:10.1016/j.semarthrit.2016.04.003
34. Bar-Or D, Rael LT, Brody EN. Use of saline as a placebo in intra-articular injections in osteoarthritis: potential contributions to nociceptive pain relief. Open Rheumatol J. 2017;11(1):16–22. doi:10.2174/1874312901711010016
35. Saltzman BM, Leroux T, Meyer MA, et al. The therapeutic effect of intra-articular normal saline injections for knee osteoarthritis: a meta-analysis of evidence level 1 studies. Am J Sports Med. 2017;45(11):2647–2653. doi:10.1177/0363546516680607
36. Fabre H, Ducret M, Degoul O, et al. Characterization of different sources of human MSCs expanded in serum-free conditions with quantification of chondrogenic induction in 3D. Stem Cells Int. 2019;2019:2186728. doi:10.1155/2019/2186728
37. Mohamed-Ahmed S, Fristad I, Lie SA, et al. Adipose-derived and bone marrow mesenchymal stem cells: a donor-matched comparison. Stem Cell Res Ther. 2018;9(1):168. doi:10.1186/s13287-018-0914-1
38. Williams RJ, Tryfonidou MA, Snuggs JW, Le Maitre CL. Cell sources proposed for nucleus pulposus regeneration. JOR Spine. 2021;4(4):e1175. doi:10.1002/jsp2.1175
39. Gay MH, Mehrkens A, Rittmann M, et al. Nose to back: compatibility of nasal chondrocytes with environmental conditions mimicking a degenerated intervertebral disc. Eur Cell Mater. 2019;37:214–232. doi:10.22203/eCM.v037a13
40. Vadala G, Sowa G, Hubert M, Gilbertson LG, Denaro V, Kang JD. Mesenchymal stem cells injection in degenerated intervertebral disc: cell leakage may induce osteophyte formation. J Tissue Eng Regen Med. 2012;6(5):348–355. doi:10.1002/term.433
41. Risbud MV, Schipani E, Shapiro IM. Hypoxic regulation of nucleus pulposus cell survival: from niche to notch. Am J Pathol. 2010;176(4):1577–1583. doi:10.2353/ajpath.2010.090734
42. Colella F, Garcia JP, Sorbona M, et al. Drug delivery in intervertebral disc degeneration and osteoarthritis: selecting the optimal platform for the delivery of disease-modifying agents. J Control Release. 2020;328:985–999. doi:10.1016/j.jconrel.2020.08.041
43. Filler AG. Emergence and optimization of upright posture among hominiform hominoids and the evolutionary pathophysiology of back pain. Neurosurg Focus. 2007;23(1):1–6. doi:10.3171/FOC-07/07/E4
44. Pennisi E. Evolutionary biology. The burdens of being a biped. Science. 2012;336(6084):974. doi:10.1126/science.336.6084.974
45. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26(17):1873–1878. doi:10.1097/00007632-200109010-00011
46. Lotz JC, Haughton V, Boden SD, et al. New treatments and imaging strategies in degenerative disease of the intervertebral disks. Radiology. 2012;264(1):6–19. doi:10.1148/radiol.12110339
47. Kushchayev SV, Glushko T, Jarraya M, et al. ABCs of the degenerative spine. Insights Imaging. 2018;9(2):253–274. doi:10.1007/s13244-017-0584-z
48. International Spine Intervention Society. Lumbar disc stimulation (Provocation Discography). In: Bogduk N, editor. Practice Guidelines for Spinal Diagnostic and Treatment Procedures.
49. Rossi MJ, Brand JC, Lubowitz JH. Minimally Clinically Important Difference (MCID) is a low bar. Arthroscopy. 2023;39(2):139–141. doi:10.1016/j.arthro.2022.11.001
50. Adindu EK, Singh D, Geck M, Stokes J, Truumees E. Minimal clinically important difference and patient-acceptable symptom state in orthopaedic spine surgery: a review. JBJS Rev. 2023;11(4). doi:10.2106/JBJS.RVW.22.00200
51. Tubach F, Dougados M, Falissard B, Baron G, Logeart I, Ravaud P. Feeling good rather than feeling better matters more to patients. Arthritis Rheum. 2006;55(4):526–530. doi:10.1002/art.22110
52. Pham T, Tubach F. Patient acceptable symptomatic state (PASS). Joint Bone Spine. 2009;76(4):321–323. doi:10.1016/j.jbspin.2009.03.008
53. Daste C, Abdoul H, Foissac F, et al. Patient acceptable symptom state for patient-reported outcomes in people with non-specific chronic low back pain. Ann Phys Rehabil Med. 2022;65(1):101451. doi:10.1016/j.rehab.2020.10.005
54. Tubach F, Ravaud P, Martin-Mola E, et al. Minimum clinically important improvement and patient acceptable symptom state in pain and function in rheumatoid arthritis, ankylosing spondylitis, chronic back pain, hand osteoarthritis, and Hip and knee osteoarthritis: results from a prospective multinational study. Arthritis Care Res. 2012;64(11):1699–1707.
55. Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain. Towards international consensus regarding minimal important change. Spine. 2008;33(1):90–94. doi:10.1097/BRS.0b013e31815e3a10
56. Glassman SD, Copay AG, Berven SH, Polly DW, Subach BR, Carreon LY. Defining substantial clinical benefit following lumbar spine arthrodesis. J Bone Joint Surg Am. 2008;90(9):1839–1847. doi:10.2106/JBJS.G.01095
57. Power JD, Perruccio AV, Canizares M, et al. Determining minimal clinically important difference estimates following surgery for degenerative conditions of the lumbar spine: analysis of the Canadian Spine Outcomes and Research Network (CSORN) registry. Spine J. 2023;23(9):1323–1333. doi:10.1016/j.spinee.2023.05.001
58. Solberg T, Johnsen LG, Nygaard OP, Grotle M. Can we define success criteria for lumbar disc surgery?: estimates for a substantial amount of improvement in core outcome measures. Acta Orthop. 2013;84(2):196–201. doi:10.3109/17453674.2013.786634
59. Werner DAT, Grotle M, Gulati S, et al. Criteria for failure and worsening after surgery for lumbar disc herniation: a multicenter observational study based on data from the Norwegian Registry for Spine Surgery. Eur Spine J. 2017;26(10):2650–2659. doi:10.1007/s00586-017-5185-5
60. Yin W, Pauza K, Olan WJ, Doerzbacher JF, Thorne KJ. Intradiscal injection of fibrin sealant for the treatment of symptomatic lumbar internal disc disruption: results of a prospective multicenter pilot study with 24-month follow-up. Pain Med. 2014;15(1):16–31. doi:10.1111/pme.12249
61. Beall DP, Amirdelfan K, Nunley PD, Phillips TR, Imaz Navarro LC, Spath A. Hydrogel augmentation of the lumbar intervertebral disc: an early feasibility study of a treatment for discogenic low back pain. J Vasc Interv Radiol. 2024;35(1):51–58 e51. doi:10.1016/j.jvir.2023.09.018
62. Kanan M, Eby O, Kelkar A, et al. Electrical stimulation-mediated tissue healing in porcine intervertebral disc under mechanically dynamic organ culture conditions. Spine. 2022;47(10):764–772. doi:10.1097/BRS.0000000000004331
63. Vadala G, Ambrosio L, Russo F, Papalia R, Denaro V. Stem Cells and intervertebral disc regeneration overview-what they can and can’t do. Int J Spine Surg. 2021;15(s1):40–53. doi:10.14444/8054
64. Paez A, Rovers M, Hutchison K, et al. Beyond the RCT: when are randomized trials unnecessary for new therapeutic devices, and what should we do instead? Ann Surg. 2022;275(2):324–331. doi:10.1097/SLA.0000000000005053
65. Abraham I, Lewandrowski KU, Elfar JC, et al. Randomized clinical trials and observational tribulations: providing clinical evidence for personalized surgical pain management care models. J Pers Med. 2023;13(7):1044. doi:10.3390/jpm13071044
66. Lewandrowski KU, Leon JF, Dowling A, et al. Breaking through the glass ceiling effect of high-grade clinical evidence creation in orthopaedics & trauma. Revista Colombiana de Ortopedia y Traumatología. 2022;36(4):215–228. doi:10.1016/j.rccot.2022.10.003
67. Hutchinson N, Moyer H, Zarin DA, Kimmelman J. The proportion of randomized controlled trials that inform clinical practice. Elife. 2022;2:11.
68. Fanaroff AC, Califf RM, Harrington RA, et al. Randomized trials versus common sense and clinical observation: JACC review topic of the week. J Am Coll Cardiol. 2020;76(5):580–589. doi:10.1016/j.jacc.2020.05.069
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.