Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Persistent Respiratory Failure and Re-Admission in Patients with Chronic Obstructive Pulmonary Disease Following Hospitalization for COVID-19
Authors Figueira‐Gonçalves JM, García-Bello MÁ, Ramallo‐Fariña Y, Méndez R, Latorre Campos A, González-Jiménez P, Peces-Barba G, Molina-Molina M, España PP, García E, Domínguez-Pazos SJ, García Clemente M, Panadero C , de la Rosa-Carrillo D , Sibila O, Martínez-Pitarch MD, Toledo-Pons N , López-Ramirez C, Almonte-Batista W , Macías-Paredes A, Badenes-Bonet D, Pérez-Rodas EN, Lázaro J, Quirós Fernández S, Cordovilla R , Cano-Pumarega I , Torres A, Menendez R
Received 2 July 2023
Accepted for publication 30 October 2023
Published 7 November 2023 Volume 2023:18 Pages 2473—2481
DOI https://doi.org/10.2147/COPD.S428316
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Juan Marco Figueira‐Gonçalves,1,2 Miguel Ángel García-Bello,3,4 Yolanda Ramallo‐Fariña,3– 5 Raúl Méndez,6– 9 Ana Latorre Campos,6,7 Paula González-Jiménez,6,7,9 Germán Peces-Barba,10 María Molina-Molina,11 Pedro Pablo España,12 Estela García,13 Santiago de Jorge Domínguez-Pazos,14 Marta García Clemente,15 Carolina Panadero,16 David de la Rosa-Carrillo,17 Oriol Sibila,18 María Dolores Martínez-Pitarch,19 Nuria Toledo-Pons,20 Cecilia López-Ramirez,21 Wanda Almonte-Batista,22 Abigail Macías-Paredes,23 Diana Badenes-Bonet,24 Eli Nancy Pérez-Rodas,25 Javier Lázaro,26 Sarai Quirós Fernández,27 Rosa Cordovilla,28 Irene Cano-Pumarega,8,29 Antoni Torres,8,18 Rosario Menendez6– 9 On behalf of RECOVID
1Pneumology and Thoracic Surgery Service, Unit for Patients with Highly Complex COPD, University Hospital Nuestra Señora de Candelaria, Santa Cruz de Tenerife, Spain; 2University Institute of Tropical Disease and Public Health of the Canary Islands, University of La Laguna, Santa Cruz de Tenerife, Spain; 3Evaluation Unit (SESCS), Canary Islands Health Research Institute Foundation (FIISC), Tenerife, Spain; 4Network for Research on Chronicity, Primary Care, and Health Promotion (RICAPPS), Tenerife, Spain; 5Health Services Research on Chronic Patients Network (REDISSEC), Madrid, Spain; 6Pneumology Department, Hospital Universitario y Politécnico La Fe, Valencia, Spain; 7Respiratory InFections, Instituto de Investigación Sanitaria La Fe (IISLAFE), Valencia, Spain; 8CIBER de Enfermedades Respiratorias (CIBERES), Instituto de Salud Carlos III, Madrid, Spain; 9Medicine Department, University of Valencia, Valencia, Spain; 10Pulmonology Department, Hospital Fundación Jiménez Díaz, Madrid, Spain; 11ILD Unit, Respiratory Department, Hospital de Bellvitge, Hospitalet de Llobregat, Spain; 12Respiratory Service, Hospital de Galdakao-Usansolo, Galdakao, Spain; 13Respiratory Service, Hospital de Cabueñes, Gijón, Spain; 14Respiratory Service, Hospital Universitario de A Coruña, A Coruña, Spain; 15Respiratory Service, Hospital Universitario Central de Asturias, Oviedo, Spain; 16Respiratory Service, Hospital de Getafe, Getafe, Spain; 17Respiratory Service, Hospital de la Santa Creu i Sant Pau, Barcelona, Spain; 18Respiratory Service, Hospital Clínic, Barcelona, Spain; 19Respiratory Service, Hospital Lluís Alcanyís, Játiva, Spain; 20Respiratory Service, Hospital Son Espases, Palma, Spain; 21Medical Surgical Unit of Respiratory Diseases, Hospital Virgen del Rocío, Sevilla, Spain; 22Respiratory Service, Hospital de Albacete, Albacete, Spain; 23Respiratory Service, Hospital de Sant Jaume, Calella, Spain; 24Respiratory Service, Hospital del Mar, Barcelona, Spain; 25Respiratory Service, Hospital Municipal de Badalona, Badalona, Spain; 26Respiratory Service, Hospital Royo Villanova, Zaragoza, Spain; 27Respiratory Service, Hospital Basurto, Bilbao, Spain; 28Respiratory Service, Hospital de Salamanca, Salamanca, Spain; 29Respiratory Service, Hospital Universitario Ramón y Cajal (IRYCIS), Madrid, Spain
Correspondence: Juan Marco Figueira‐Gonçalves, Pneumology and Thoracic Surgery Service, University Hospital Nuestra Señora de Candelaria, Santa Cruz de Tenerife, Spain, Tel +34654959246, Email [email protected]
Background: Chronic obstructive pulmonary disease (COPD) has been associated with worse clinical evolution/survival during a hospitalization for SARS-CoV2 (COVID-19). The objective of this study was to learn the situation of these patients at discharge as well as the risk of re-admission/mortality in the following 12 months.
Methods: We carried out a subanalysis of the RECOVID registry. A multicenter, observational study that retrospectively collected data on severe acute COVID-19 episodes and follow-up visits for up to a year in survivors. The data collection protocol includes general demographic data, smoking, comorbidities, pharmacological treatment, infection severity, complications during hospitalization and required treatment. At discharge, resting oxygen saturation (SpO2), dyspnea according to the mMRC (modified Medical Research Council) scale and long-term oxygen therapy prescription were recorded. The follow-up database included the clinical management visits at 6 and 12 months, where re-admission and mortality were recorded.
Results: A total of 2047 patients were included (5.6% had a COPD diagnosis). At discharge, patients with COPD had greater dyspnea and a greater need for prescription home oxygen. After adjusting for age, sex and Charlson comorbidity index, patients with COPD had a greater risk of hospital re-admission due to respiratory causes (HR 2.57 [1.35– 4.89], p = 0.004), with no significant differences in survival.
Conclusion: Patients with COPD who overcome a serious SARS-CoV2 infection show a worse clinical situation at discharge and a greater risk of re-admission for respiratory causes.
Keywords: chronic obstructive pulmonary disease, COPD, COVID-19, coronavirus disease 2019, RECOVID, Spanish COVID-19 registry, SARS-CoV2, severe acute respiratory syndrome coronavirus 2, SEPAR, respiratory failure
Introduction
The disease caused by the SARS-CoV2 virus (COVID-19) has had a major impact worldwide due to its high morbidity and mortality. Advanced age, active smoking and the presence of comorbidities like chronic obstructive pulmonary disease (COPD) have been associated with worse clinical evolution or survival.1–7 The up-regulation of the angiotensin converting enzyme-2 (ACE-2) receptor, impaired innate and adaptive immune responses and demonstrated delayed clearance of respiratory viruses in these patients are some of the proposed mechanisms.7 Together, these factors may facilitate the propagation of SARS-CoV-2 in the lungs of patients with COPD, leading to rapid clinical deterioration and progression to severe COVID-19.7 Furthermore, COPD itself can act as a risk factor for re-admission and worse survival following hospitalization for COVID-19.8–10 However, limited studies have been conducted specifically in this population. The objective of this study was to learn the situation of patients with COPD at discharge as well as the risk of re-admission and mortality following hospitalization for SARS-CoV2 infection.
Methods
For the study, we carried out a subanalysis of the RECOVID (Spanish Registry for Hospitalized COVID-19) registry at 49 Spanish hospitals with patients hospitalized in 2020 (March–November) with a confirmed SARS-CoV2 infection using SARS-CoV2 RT-PCR.11 Briefly, it is a multicenter, observational study that retrospectively collected data on acute COVID-19 episodes and follow-up visits for up to a year in survivors. Patients with COVID-19 registered in the pneumology service of each participating center (stratum) were identified. To achieve a more representative cohort of patients, including different geographical areas, each center recruited groups of 50 randomly selected patients before entering the data. Only three hospitals recruited consecutive patients. The study was approved by both the Ethics Committee (Comité Ètic d’Investigació Clínica, Hospital San Pau, Barcelona) on 29 April 2020 and by the local committees of the participating centers. An electronic database was created and stored on the XOLOMON web platform to gather anonymized data in accordance with regulation (EU) 2016/679 of the European Parliament and of the Council, of 27 April 2016, and Spanish Organic Law 3/2018. The data collection protocol includes general demographic data, smoking, comorbidities, pharmacological treatment, infection severity, complications during hospitalization and required treatment. At discharge, resting oxygen saturation (SpO2), dyspnea according to the mMRC (modified Medical Research Council) scale and long-term oxygen therapy prescription were recorded. The follow-up database comprised clinical check-up visit data at 6 and 12 months, including information related to symptoms, analytical variables and complementary explorations, where re-admission and mortality were recorded. The study used a data monitor to review inconsistencies and missing data and prepare follow-up questions for each hospital. To deem each case valid, a minimum of 70% of completed data regarding the fundamental variables was necessary. After being evaluated by the ethics committee, informed consent was not required to carry out this study.
For the statistical analysis of qualitative variables, frequencies (and percentage) were calculated, while average and standard deviation were used for quantitative variables. Follow-up time was summarized using the median and maximum. Charlson index values were compared using independent mean contrast. The association between qualitative variables and the presence of COPD was evaluated using the chi-square test of independence. To compare the survival curves for the post-discharge death and re-admission variables, the Kaplan-Meier Log rank test was used. A Cox regression analysis was carried out to evaluate the impact of COPD on mortality and re-admission, after adjusting for age, sex and Charlson index, and before verifying the risk proportionality assumption. To analyze the risk of re-admission due to respiratory causes, the analysis was also adjusted for current smoking or pack-year index. All analyses were carried out with R software, version 4.2.1.12
Results
2047 patients were included (March–November 2020), of which 115 (5.6%) had been diagnosed with COPD. The characteristics of both groups are described in Table 1. Patients with COPD were older, had a greater smoking history and a greater comorbidity burden compared to patients without COPD. At discharge, patients with COPD had greater dyspnea, a lower baseline SpO2 and a greater need for prescription home oxygen (13.1% vs 5.3%, p = 0.007).
 |
Table 1 Baseline Characteristics of Patients Included in the Study |
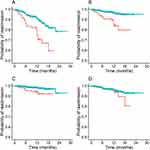
The average length of follow-up was 379 days (378 days for the patient cohort without COPD and 382 for the COPD cohort). A total of 191 patients (8.5%) had to be re-hospitalized (164 (8.5%) in the non-COPD group and 27 (23.5%) in the COPD group, p < 0.001). Compared to patients without COPD, patients with COPD showed a greater need to be re-admitted for any cause (χ² = 29.9, df = 1, p < 0.001, Figure 1A), for respiratory causes (χ² = 33.7, df = 1, p < 0.001, Figure 1B) and for cardiovascular causes (χ² = 10, df = 1, p = 0.001, Figure 1C), without finding any differences with respect to re-admission for other causes (χ² = 1, df = 1, p = 0.30, Figure 1D). In the Cox multivariate analysis adjusted for age, sex and Charlson comorbidity index, patients with COPD were found to have a greater risk of hospital re-admission for respiratory causes (HR 2.57 [1.35–4.89], p = 0.004). This high risk remained after adjusting for current smoking or pack-year index (HR 2.48 [1.28–4.8], p = 0.007 and HR 4.2 [1.8–9.8], p = 0.001, respectively). The risk of re-admission for any cause, for cardiovascular causes or other causes was not statistically significant (HR 1.48 [0.95–2.32], p = 0.084; HR 1.5 [0.55–4.0], p = 0.443 and HR 0.84 [0.36–1.96], p = 0.69, respectively) after adjusting for age, sex and Charlson comorbidity index.
Seventy patients passed away during follow-up. In the 12 months following discharge, 8.5% of patients with COPD and 2.7% of patients without COPD had passed away (p < 0.001). Although the group of patients with COPD showed worse survival compared to patients without COPD in the crude analysis (χ² = 10.5, df = 1, p = 0.001), in the multivariate analysis adjusted for sex, age and Charlson index, the impact of COPD on survival was not significant (HR 0.89 [0.41–1.93], p = 0.76).
Discussion
Our study has two relevant conclusions: 1) patients with COPD who overcome severe SARS-CoV2 infection have a worse clinical situation at discharge; 2) patients with COPD have a greater risk of re-admission, especially for respiratory causes. Studies conducted in the early stages of the COVID-19 pandemic showed that patients with COPD were hospitalized with a worse clinical situation, had high comorbidity (especially cardiovascular) and worse survival.13 Our study identifies hospitalized patients with COPD that overcome viral infection as a more vulnerable group and, consequently, at greater risk of suffering worse evolution after discharge. The baseline situation of patients with COPD, the severity of the process, prolonged stay, the treatment used, the presence of comorbidities, and SARS-CoV2 variant are some of the factors that will influence a patient’s situation when the infection resolves.1–6,14 Furthermore, COPD exacerbation due to SARS-COV2 seems to have a worse prognosis compared to other exacerbations not related to this virus. Hyams et al14 compared outcomes of patients hospitalized with SARS-CoV-2 infective exacerbation vs non-SARS-CoV-2 infective exacerbation and found that SARS-CoV-2 exacerbation was associated with worse outcomes than for those admitted with non-SARS-CoV2 infective exacerbation, with a 55% and 26% and 35% increased risk of positive pressure support, hospitalization length and 30-day mortality, respectively, when controlling for potential confounders such as age, chronic medical conditions and vaccination status.
The rate of re-admission in the 12 months following hospitalization for COVID-19 is estimated to be ≈ 10%,15,16 being higher in the elderly and in subjects with multiple comorbidities like COPD or cardiovascular disease.8–10 In our study, the probability of re-admission for patients with COPD was almost triple that of patients without COPD (24.1% versus 8.6). The presence of cardiovascular comorbidities combined with advanced age along with the respiratory disease itself could have a synergistic effect that would negatively affect these patients’ evolution. With respect to causes of re-admission, a meta-analysis by Akbari et al8 found respiratory and cardiac complications to be the main causes (48% and 14%, respectively): respiratory sepsis, COVID-19, pneumonia and the presence of pulmonary thromboembolism were the main diagnoses,10,16,17 situations in which patients with COPD are especially vulnerable.18–20 In our study, mortality at one year in patients with COPD was higher than patients without COPD, a result that coincides with previous studies.21 However, variability in the percentage of deaths in different studies may be a reflection of the heterogeneity of the populations analyzed, the inclusion criteria used, the follow-up policies or the level of severity at hospitalization.15 Data obtained from large databases such as Medicare shows that, in patients who were discharged alive from a COVID-19 related hospital admission (between March 2020 and August 2022), the risk of post-discharge death was nearly two-fold compared to the influenza virus, with most of the difference occurring within 30 days of discharge. These findings emphasize the need for patients who overcome a severe SARS-CoV2 infection to be monitored closely after discharge.22
Among the strengths of this study, we can highlight the large sample size and its multicentric nature. To our knowledge, this is the first study to analyze the evolution of patients with COPD following hospitalization for COVID-19. The limitations are those inherent to retrospective registries, with different diagnostic and follow-up protocols at the different hospitals. It is possible that the pandemic caused difficulties in out-patient follow-up,23 which could influence the high rate of re-admission in these patients with a more precarious clinical situation at discharge. In addition, our study was carried out at a time when vaccination against the SARS-COV2 virus had not yet been implemented. Current evidence suggesting that outcomes have improved over time for patients with COPD hospitalized with SARS-CoV-2 based on circulating and dominant variants, vaccination rates, healthcare pressure and COVID-19 treatments is varied.14,22,24–28 Taking into account these aspects, more studies will be required to confirm our results in the current health situation, especially with regard to these patients’ evolution after hospital discharge, evaluating the clinical impact of new dominant SARS-CoV2 variants, treatments and vaccination on this group of patients.
In conclusion, patients with COPD who have overcome severe SARS-CoV2 infection have a high risk of re-admission, especially re-admission related to respiratory causes, and show greater clinical deterioration at discharge, requiring oxygen for persistent respiratory distress, which could point to the need to create specific follow-up plans in this specific patient group.
Ethics and Consent Statements
The study was approved by both the Ethics Committee (Comité Ètic d’Investigació Clínica, Hospital San Pau, Barcelona) on 29 April 2020 and by the local committees of the participating centers. The study did not require informed consent.
List of RECOVID Principal Investigators
Clínica Asunción. Itxaso Sayago Reza.
Complejo Hospitalario Univ. de Albacete. Wanda Almonte Batista.
Complejo Hospitalario Univ. de Navarra. Laura Moreno Galarraga.
Hospital Clínic. Oriol Sibila Vidal.
Hospital Clínico San Carlos. Juan Luis Rodríguez Hermosa. Gianna Vargas Centanaro.
Hospital Clínico Univ. de Valladolid. Blanca de Vega Sánchez. Eduardo Solís García. Ester Rodríguez Florez. María José Chourio Estaba.
Hospital de Bellvitge. María Molina Molina. Jaume Bordas.
Hospital de Torrecárdenas. María Estela González Castro.
Hospital del Mar. Diana Badenes Bonet. Marisol Domínguez Álvarez.
Hospital Dos de Maig. Pérez-Rodas Eli-N (currently working at Hospital Municipal de Badalona, Barcelona). Alejandra Marín Arguedas.
Hospital Dr. José Molina Orosa. Berta Román Bernal.
Hospital General de Segovia. Graciliano Estrada Trigueros.
Hospital Gral. Univ. de Castellón. Selene Cuenca Peris. Margarita Martín Royo. Miguel Torres García.
Hospital Gral. Univ. de Ciudad Real. José Portillo Sánchez.
Hospital Gral. Univ. Santa Lucía. Francisca Lerenas Bernal. María Salome Ros Braquehais.
Hospital la Mancha Centro. José Alfonso García Guerra.
Hospital Lluis Alcanyís. María Dolores Martínez Pitarch. Iván Arroyo Fernández.
Hospital Ntra. Sra. de Sonsoles. Virginia Guevara Velázquez.
Hospital Plató. Pilar Martínez Olondris.
Hospital público de Monforte de Lemos. Marco Francisco Pereyra Barrionuevo.
Hospital Royo Villanova. Javier Lázaro Sierra. Paloma Clavería.
Hospital San Juan de Dios de Tenerife. Aurelio Luis Wangüemert Pérez. José Joel Ruiz Lacambra. Noelia Fernández Ramos. Sara Guanche Dorta.
Hospital Sant Jaume de Calella. Abigail Macias Paredes.
Hospital Santa Creu i Sant Pau. David de la Rosa Carrillo. Esther Palones Femenia. Inés Podzamczer Valls. Patricia Peñacoba Toribio.
Hospital de Jérez. Pilar Muñoz Zara.
Hospital Univ. 12 de octubre. Rocío García García.
Hospital Univ. A Coruña. María del Mar Marrube Fernández. Laura Villar Aguilar. Santiago de Jorge Domínguez Pazos. Tara Pereiro Brea. Angélica Consuegra-Vanegas
Hospital Univ. Central de Asturias. Ana Pando-Sandoval. Marta María García Clemente.
Hospital Univ. de Cabueñes. Amelia Alzueta Álvarez. Estela García Coya. Elizabeth de Freitas González.
Hospital Univ. de Galdakao-Usansolo. Pedro Pablo España Yandiola. Ane Uranga.
Hospital Univ. de Getafe. Beatriz Raboso Moreno. Carolina Panadero. Araceli Abad. Irene Cano (currently working at Hospital Universitario Ramón y Cajal (IRYCIS), Madrid, Spain).
Hospital Univ. Fundación Alcorcón. Iria Pérez Orbis.
Hospital Univ. Fundación Jiménez Díaz. German Peces-Barba, Carolina Gotera Rivera. Celia Ruiz Pérez.
Hospital Univ. i Politècnic La Fe. Rosario Menéndez Villanueva. Raúl Méndez. Ana Latorre, Paula González.
Hospital Univ. Infanta Sofía. Teresa Ramírez Prieto. Miguel Ángel Salvador Maya.
Hospital Univ. La Princesa. Claudia Valenzuela.
Hospital Univ. Marqués de Valdecilla. José M. Cifrián Martínez.
Hospital Univ. Ntra. Sra. Candelaria. Juan Marco Figueira Gonçalves. Adrián Baeza Ruiz. Andrea Expósito Marrero. Nikita Gurbani.
Hospital Univ. Puerta de Hierro. Rosa Malo de Molna Ruiz
Hospital Univ. Sagrat Cor. Marina Galdeano Lozano.
Hospital Univ. San Agustín. Manuel Villanueva Montes.
Hospital Univ. Son Espases. Nuria Toledo Pons. Luisa Ramón Clar.
Hospital Univ. Torrejón. Alba Esperanza Barrios.
Hospital Univ. Virgen del Rocío. Pilar Cejudo Ramos. Cecilia López Ramírez. Mirella Gaboli.
Hospital Univ. Virgen Macarena. Virginia Almadana Pacheco.
Hospital Univ. Arnau de Vilanova. Ferran Eduard Barbé Illa. Anna Clara.
Hospital Virgen de la Luz. Nuria Gutiérrez González.
Hospital Virgen de la Victoria. Eva Cabrera César.
Acknowledgments
Miriam Ovejero (SEPAR), Rafael Santana (data manager). SEPAR has contributed administrative personnel for logistical support, as well as a methodology and research platform. SEPAR’s integrated respiratory infection research program.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
A non-conditional grant from Gebro Pharma Laboratories, which did not participate in the design, data collection, statistical analysis or writing of the article. Sociedad Española de Neumología y Cirugía Torácica (SEPAR): 1078/2020 and 1290/2022. Raúl Méndez is the recipient of a Juan Rodés grant, supported by the Instituto de Salud Carlos III (ISCIII [JR21/00051]).
Disclosure
Dr Pedro Pablo España reports personal fees from Glaxo, grants from Pfizer, outside the submitted work. Drs Nuria Toledo-Pons reports personal fees from GSK, Chiesi; non-financial support from FAES and Sanofi, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021;21(1):855. doi:10.1186/s12879-021-06536-3
2. Posso M, Comas M, Román M, et al. Comorbidities and mortality in patients with COVID-19 aged 6. years and older in a university hospital in Spain. Arch Bronconeumol. 2020;56(11):756–758. doi:10.1016/j.arbres.2020.06.012
3. Golpe R, Blanco N, Castro-an ̃ón O, et al. Factors associated to hospital admission in a care protocol in COVID-19. Arch Bronconeumol. 2020;56(10):676–677. doi:10.1016/j.arbres.2020.05.038
4. Zhang JJ, Dong X, Liu GH, Gao YD. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin Rev Allergy Immunol. 2022;19:1–18.
5. Tazerji SS, Shahabinejad F, Tokasi M, et al. Global data analysis and risk factors associated with morbidity and mortality of COVID-19. Gene Rep. 2022;26:101505. doi:10.1016/j.genrep.2022.101505
6. Graziani D, Soriano JB, Del Rio-Bermudez C, et al. Characteristics and Prognosis of COVID-19 in Patients with COPD. J Clin Med. 2020;9(10):3259. doi:10.3390/jcm9103259
7. Gerayeli FV, Milne S, Cheung C, et al. COPD and the risk of poor outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2021;33:100789. doi:10.1016/j.eclinm.2021.100789
8. Akbari A, Fathabadi A, Razmi M, et al. Characteristics, risk factors, and outcomes associated with readmission in COVID-19 patients: a systematic review and meta-analysis. Am J Emerg Med. 2022;52:166–173. doi:10.1016/j.ajem.2021.12.012
9. Lavery AM, Preston LE, Ko JY, et al. Characteristics of Hospitalized COVID-19 Patients Discharged and Experiencing Same-Hospital Readmission - United States, March-August 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1695–1699. doi:10.15585/mmwr.mm6945e2
10. Ramos-Martínez A, Parra-Ramírez LM, Morrás I, et al. Frequency, risk factors, and outcomes of hospital readmissions of COVID-19 patients. Sci Rep. 2021;11(1):13733. doi:10.1038/s41598-021-93076-0
11. Menéndez R, Méndez R, Latorre A, et al. Residual pulmonary infiltrates, symptoms and diffusion impairment at 1-year after severe COVID-19 infection have different associated factors. J Intern Med. 2023;294:69–82. doi:10.1111/joim.13642
12. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2022. Available from: https://www.R-project.org/.
13. Gómez Antúnez M, Muiño Míguez A, Bendala Estrada AD, et al.; SEMI-COVID-19 Network. Clinical Characteristics and Prognosis of COPD Patients Hospitalized with SARS-CoV-2. Int J Chronic Obstructive Pulmonary Dis. 2021;15:3433–3445. doi:10.2147/COPD.S276692
14. Hyams C, Qian G, Nava G, et al. Impact of SARS-CoV-2 infective exacerbation of chronic obstructive pulmonary disease on clinical outcomes in a prospective cohort study of hospitalised adults. J R Soc Med;2023. 1410768231184162. doi:10.1177/01410768231184162
15. Ramzi ZS. Hospital readmissions and post-discharge all-cause mortality in COVID-19 recovered patients; A systematic review and meta-analysis. Am J Emerg Med. 2022;51:267–279. doi:10.1016/j.ajem.2021.10.059
16. Freire MP, Oliveira MS, Magri MMC, et al. Frequency and factors associated with hospital readmission after COVID-19 hospitalization: the importance of post-COVID diarrhea. Clinics. 2022;77:100061. doi:10.1016/j.clinsp.2022.100061
17. Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC. Readmission and Death After Initial Hospital Discharge Among Patients With COVID-19 in a Large Multihospital System. JAMA. 2021;325(3):304–306. doi:10.1001/jama.2020.21465
18. Inghammar M, Engstrom G, Ljungberg B, Lofdahl CG, Roth A, Egesten A. Increased incidence of invasive bacterial disease in chronic obstructive pulmonary disease compared to the general population—A population based cohort study. BMC Infect Dis. 2014;14:163–170. doi:10.1186/1471-2334-14-163
19. Lin SH, Perng DW, Chen CP, et al. Increased risk of community-acquired pneumonia in COPD patients with comorbid cardiovascular disease. Int J Chron Obstruct Pulmon Dis. 2016;11:3051–3058. doi:10.2147/COPD.S115137
20. Ambrosetti M, Ageno W, Spanevello A, Salerno M, Pedretti RF. Prevalence and prevention of venous thromboembolism in patients with acute exacerbations of COPD. Thromb Res. 2003;112(4):203–207. doi:10.1016/j.thromres.2003.12.003
21. Novelli L, Raimondi F, Carioli G, et al. One-year mortality in COVID-19 is associated with patients’ comorbidities rather than pneumonia severity. Respir Med Res. 2022;83:100976. doi:10.1016/j.resmer.2022.100976
22. Oseran AS, Song Y, Xu J, et al. Long term risk of death and readmission after hospital admission with covid-19 among older adults: retrospective cohort study. BMJ. 2023;
23. Fernández Villar A, Golpe Gómez R, González Montaos A, et al. The impact of the SARS-CoV-2 pandemic on the demographic, clinical and social profiles of patients admitted to the Pneumology Department for a COPD exacerbation. PLoS One. 2023;18(9):e0290156. doi:10.1371/journal.pone.0290156
24. Fedeli U, Casotto V, Barbiellini Amidei C, Vianello A, Guarnieri G. COPD-Related Mortality before and after Mass COVID-19 Vaccination in Northern Italy. Vaccines. 2023;11(8):1392. doi:10.3390/vaccines11081392
25. Hyams C, Challen R, Marlow R, et al. Severity of Omicron (B.1.1.529) and Delta (B.1.617.2) SARS-CoV-2 infection among hospitalised adults: a prospective cohort study in Bristol. United Kingdom Lancet Reg Health Eur. 2023;25:100556. doi:10.1016/j.lanepe.2022.100556
26. Van Goethem N, Chung PYJ, Meurisse M, et al. Clinical severity of SARS-CoV-2 Omicron variant compared with delta among hospitalized COVID-19 patients in Belgium during autumn and winter season 2021–2022. Viruses. 2022;14(6):1297. doi:10.3390/v14061297
27. Gómez-Antúnez M, Muiño-Míguez A, Bacete-Cebrián M, et al. Patients with COPD hospitalized due to COVID-19 in Spain: a comparison between the first and second wave. Rev Clin Esp. 2023;223(5):298–309. doi:10.1016/j.rce.2023.02.003
28. Lin L, Liu Y, Tang X, He D. The disease severity and clinical outcomes of the SARS-CoV-2 variants of concern. Front Public Health. 2021;9:775224. doi:10.3389/fpubh.2021.775224
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.