Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Peripheral Complement Factor-Based Biomarkers for Patients with First-Episode Schizophrenia
Authors Cao Y, Xu Y, Xia Q, Shan F, Liang J
Received 23 May 2023
Accepted for publication 20 June 2023
Published 23 June 2023 Volume 2023:19 Pages 1455—1462
DOI https://doi.org/10.2147/NDT.S420475
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Yin Cao,1– 4 Yayun Xu,5– 7 Qingrong Xia,1– 4 Feng Shan,1– 4 Jun Liang1– 4
1Affiliated Psychological Hospital of Anhui Medical University, Hefei, People’s Republic of China; 2Department of Pharmacy, Hefei Fourth People’s Hospital, Hefei, People’s Republic of China; 3Psychopharmacology Research Laboratory, Anhui Mental Health Center, Hefei, People’s Republic of China; 4Anhui Clinical Research Center for Mental Disorders, Hefei, People’s Republic of China; 5Department of Epidemiology and Biostatistics, School of Public Health, Anhui Medical University, Hefei, People’s Republic of China; 6Inflammation and Immune Mediated Diseases Laboratory of Anhui Province, Anhui Institute of Innovative Drugs, Anhui Medical University, Hefei, People’s Republic of China; 7The Key Laboratory of Anti-Inflammatory and Immune Medicines, Ministry of Education, Hefei, People’s Republic of China
Correspondence: Jun Liang, Department of Pharmacy, Hefei Fourth People’s Hospital, Affiliated Psychological Hospital of Anhui Medical University, Anhui Mental Health Center, 316 Huangshan Road, Hefei, 230000, People’s Republic of China, Email [email protected]
Objective: Schizophrenia (SCZ) is a severe, protracted neurological disorder that causes disruptive conduct in millions of individuals globally. Discovery of potential biomarkers in clinical settings would lead to the development of efficient diagnostic techniques and an awareness of the disease’s pathogenesis and prognosis. The aim of the present study was to discover and identify serum complement factor-based biomarkers in discriminating patients with first-episode SCZ from healthy controls.
Methods: Eighty-nine patients with first-episode SCZ and 89 healthy controls were included in this study. Psychiatric symptom severity of patients with SCZ was measured with the Brief Psychiatric Rating Scale-18 Item Version (BPRS) and the Scales for the Assessment of Negative/Positive Symptoms (SANS/SAPS). A total of 5 complement factors including complement component 1 (C1), C2, C3, C4, and 50% hemolytic complement (CH50) were measured using commercially available enzyme-linked immunosorbent assay (ELISA) kits. The levels of serum complement factors in the SCZ and control groups were compared, and the receiver operating characteristic (ROC) curve method was used to assess the diagnostic values of various complement factors for separating SCZ patients from healthy controls. Pearson’s correlation test was used to assess the relationships between serum complement factor concentrations and the psychiatric symptom severity.
Results: There was an increase in serum levels of C1, C2, C3, C4, and CH50 among patients with SCZ. Moreover, based on ROC curve analysis, the AUC value of a combined panel of C1, C2, C3, C4, and CH50 was 0.857 when used to discriminate patients with SCZ from healthy controls. Furthermore, serum C2, C3, and CH50 levels were positively correlated to the scores of SANS, SAPS, and BPRS in patients with SCZ, respectively.
Conclusion: These results suggested that circulating complement factors including C1, C2, C3, C4, and CH50 may have potential in discovering biomarkers for diagnosing first-episode SCZ.
Keywords: complement factors, biomarker, diagnosis, serum, schizophrenia
Introduction
Schizophrenia (SCZ), a serious psychiatric disorder, is one of the most incapacitating and expensive illnesses, with a prevalence of 1% worldwide.1 Indeed, SCZ is listed by the World Health Organization as one of the 10 most common causes of disability.2 Although numerous data suggest that hereditary and environmental variables interact in a complicated way to alter the etiology,3 the pathogenic processes behind SCZ are still unknown.4 Currently, there is no proven biomarker for the diagnosis and prognosis of SCZ; instead, the diagnosis is mostly based on subjective evaluations of clinical symptoms. The discovery of diagnostic biomarkers is crucial in general because insufficient or postponed treatment of mental disease in the first 2–3 years might result in increasing clinical symptoms and potentially additional consequences.5
According to several lines of evidence, dysregulation of the immune system played a crucial role in the emergence of SCZ.6 According to epidemiological studies, infection and autoimmune disorders have been linked to SCZ.7,8 Moreover, proinflammatory cytokines were found to be elevated in SCZ in numerous cross-sectional studies.9,10 Furthermore, antipsychotics such as clozapine have been shown to have immunomodulatory effects.11 Therefore, immune dysregulation may be a risk factor for SCZ.
The innate immune system’s complement system is essential for clearing an organism of germs and damaged cells, causing inflammation, and getting rid of invading foreign organisms.12 Recent evidence suggests that the complement system coordinates the balance of neural development processes.13 For instance, in Alzheimer’s disease, microglia caused neurotoxicity and pathological synapse loss through overactivation of the complement system.14 Due to the fact that the complement system directly participates in neurogenesis, synaptic pruning and cell death, all of which are related to SCZ, it is imperative to have a thorough understanding of the complement cascade in patients with SCZ. Complement component 1 (C1), C2, C3, and C4 have been reported to be the crucial role in promoting the solubility and clearance of immune complexes.15 Importantly, accumulating evidence suggests that dysregulation of C1, C2, C3, and C4 is among the risk factors for SCZ.16 Additionally, serum 50% hemolytic complement (CH50) activity is the most commonly used method of screening patient sera for functional activity of the classical complement pathway.17 Thus, whether these complement factors could serve as objective and reliable biological indicators for the diagnosis of SCZ was evaluated in the present study.
In the present study, we examined the serum levels of multiple complement factors including C1, C2, C3, C4, and CH50 in patients with first-episode SCZ, with the aim to discover and identify serum complement factor-based biomarkers that can be used for discriminating patients with first-episode SCZ from healthy controls.
Materials and Methods
Study Design and Participants
This study was conducted at Anhui Mental Health Center between July 2020 and March 2023. An experienced researcher used psychiatric interviews to screen 89 patients with SCZ following the guidelines of the structured clinical interview according to the Diagnostic and Statistical Manual for Psychiatric Disorders-Fifth Version (DSM-V). The following were the general requirements for inclusion: (1) being between the ages of 18 and 65; (2) fulfilling the SCZ diagnostic criteria given in the DSM-V; and (3) being first-episode drug-naive patients. The exclusion criteria were as follows: (1) diabetes, hyperlipidemia, cardiovascular disease, or other severe physical diseases; (2) additional mental disorders, alcoholism, or other substance abuse disorder. We also recruited 89 healthy controls at the same time, all of whom matched the patients in age, gender, and ethnicity in frequency. The ethics committee at Hefei Fourth People’s Hospital gave its approval to this procedure, which was carried out in accordance with the principles outlined in the Declaration of Helsinki. Informed consent was obtained from all the participants.
Clinical Assessment
The severity of psychiatric symptom was measured with the Brief Psychiatric Rating Scale-18 Item Version (BPRS) and the Scales for the Assessment of Negative/Positive Symptoms (SANS/SAPS). BPRS is an 18-item with each question rated on a 7-point Likert scale that is used to assess psychopathological variables. The Chinese version of BPRS has been shown to have good reliability and validity.18 A thorough assessment of negative SCZ symptoms is offered by the SANS, which consists of 24 questions that are grouped into five domains: flattened affect, alogia, avolition apathy, anhedonia/asociality, and attention.19 In contrast, the SAPS, which has 35 questions and is used to evaluate positive symptoms of SCZ; it is broken down into four categories: hallucinations, delusions, bizarre behavior, and positive formal thought disorder.19
Blood Sample Collection and Measurement of Serum Complement Factors
Blood samples were taken from the participants’ veins between 7:00 and 8:00 a.m. and immediately centrifuged at 1200 g for 10 minutes at 4 °C. Serum sample was extracted from the supernatant. All the samples were stored at −80 °C until detection. In addition, the time period during which the control samples were collected was as closely as possible matched to that of the SCZ group. A total of 5 serum complement factors including C1 (catalog number: JL53181), C2 (catalog number: JL29878), C3 (catalog number: JL10735), C4 (catalog number: JL10177), and CH50 (catalog number: JL10736) (Jianglai Bio, Shanghai, China) were measured using commercially available enzyme-linked immunosorbent assay (ELISA) kits according to manufacturer’s instructions.
Statistical Analysis
SPSS (version 17.0; IBM Corp., Armonk, NY, USA) was used to analyze the data. The data are expressed as mean ± standard deviation (SD), and the P value for statistical significance was set at 0.05. The normality of the distribution of continuous variables was measured by a one-sample Kolmogorov–Smirnov test. For continuous variables including age, BMI, and serum levels of complement factors, Student’s t-test was used to compare differences in variables between the two groups. A chi-square test was used to determine whether the groups differed in terms of gender. For correlation analyses, Pearson correlation tests were utilized. The area under the curve (AUC) of serum complement factors was examined for its ability to distinguish SCZ patients from healthy controls using receiver operating characteristic (ROC) curve analysis. G*Power (version 3.1.9.2, University of Kiel, Kiel, Germany) was used to calculate the post hoc power of a two-sample t-test with two groups due to the small sample size.
Results
Differences in Demographic and Clinical Characteristics of Participants
Participants’ demographic and clinical characteristics are summarized in Table 1. There was no statistically significant difference in age (t = −0.101, P = 0.920), gender (χ2 = 0.363, P = 0.547), or BMI (t = 0.344, P = 0.731) between patients with SCZ and healthy controls. The mean scores of BPRS, SANS, and SAPS were 35.74 ± 11.20, 40.77 ± 20.29, and 31.02 ± 13.38, respectively.
 |
Table 1 Comparison Between Control and SCZ Groups in Terms of Clinical Characteristics |
Comparative Analysis of Serum Complement Factors Between Patients with SCZ and Healthy Controls
Table 2 shows the serum complement factor levels of healthy controls and SCZ patients. Patients with SCZ had higher levels of C1, C2, C3, C4, and CH50 than controls (Table 2 and Figure 1; all P < 0.05). Post hoc power analyses showed that the power of the present study was sufficient (power > 0.80) for C1, C2, C3, C4 and CH50 (Table 2).
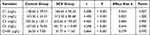 |
Table 2 Comparative Analysis of Serum Complement Factors Between Control and SCZ Groups |
Diagnostic Values of Different Complement Factors in Separating Patients with SCZ from Healthy Controls
ROC curve analysis was performed to evaluate the diagnostic value of different complement factors in separating patients with SCZ from healthy controls (Table 3 and Figure 2). The results showed that the AUC values of C1, C2, C3, C4, and CH50 were 0.630, 0694, 0.668, 0.656, and 0.636, respectively. When the cut-off point was 136.10 pg/mL for C1, the sensitivity and specificity of diagnosis reached 66.3% and 50.6%, respectively; when the cut-off point was 245.05 pg/mL for C2, the sensitivity and specificity of diagnosis reached 74.2% and 51.7%, respectively; when the cut-off point was 602.95 pg/mL for C3, the sensitivity and specificity of diagnosis reached 57.3% and 67.4%, respectively; when the cut-off point was 379.00 pg/mL for C4, the sensitivity and specificity of diagnosis reached 56.2% and 68.5%, respectively; when the cut-off point was 28.55 pg/mL for CH50, the sensitivity and specificity of diagnosis reached 58.4% and 61.8%, respectively. With a sensitivity of 79.8% and a specificity of 79.8%, a combined panel of C1, C2, C3, C4, and CH50 was able to differentiate patients with SCZ from healthy controls with a high accuracy (AUC = 0.857).
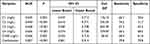 |
Table 3 Different Complement Factors and Their Ability to Discriminate Between Patients with SCZ and Healthy Volunteers Based on ROC Analysis |
Correlation Between Psychiatric Symptom Severity and the Levels of Serum Complement Factors in SCZ Group
Figure 3 shows the relationship between psychiatric symptom severity and the levels of serum complement factors in patients with SCZ. There was a positive relationship between BPRS scores and the levels of serum CH50 (r = 0.264, P = 0.015). In terms of SANS/SAPS, SANS scores were found to be positively correlated to the levels of serum C2 (r = 0.212, P = 0.047), and SAPS scores were found to be positively correlated to the levels of serum C3 (r = 0.236, P = 0.029).
 |
Figure 3 Correlation between psychiatric symptom severity and the levels of complement factors in SCZ group. ×: no significance. |
Discussion
This study compared the levels of 5 complement factors (including C1, C2, C3, C4, and CH50) in the serum of first-episode SCZ patients, with the aim of discovering and identifying biomarkers based on serum complement factors to distinguish between first-episode SCZ patients and healthy controls. There are three main findings of the present study. Firstly, patients with SCZ exhibited higher serum levels of C1, C2, C3, C4 and CH50. Secondly, ROC curve analysis showed that the AUC value of a combined panel of C1, C2, C3, C4, and CH50 was 0.857 in discriminating patients with SCZ from healthy controls. Thirdly, serum C2, C3, and CH50 levels were positively correlated to the scores of SANS, SAPS, and BPRS in patients with SCZ, respectively.
There is increasing evidence that inflammation markers play a role in the neuroprogression of SCZ and have potential in discovering biomarkers for psychotic illness. It has been reported that both NADPH oxidase 1 (the main source of physiological reactive oxygen species) and raftlin (the main lipid raft protein) showed very good diagnostic performance in discriminating patients with SCZ from healthy controls.20 Moreover, a recent meta-analysis showed that the blood levels of interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), soluble interleukin-2 receptor (sIL-2R), and interleukin-1 receptor antagonist (IL-1RA) were significantly increased in acutely ill patients with SCZ compared with controls.21 Similarly, a significant increase in serum levels of IL-6, IL-18, TNF-α, and sIL-2R in patients with SCZ were found compared with the control group.22 These findings suggest that inflammation markers may prove to be of clinical value for the diagnosis of SCZ.
The complement system is an inflammation activating part of the innate immune system.23 Several studies have focused on the state of complement system in SCZ patients. C3 and C4 play central roles in complement cascades.24 It has been reported that the C3 levels in peripheral blood of patients with SCZ were increased compared to healthy controls.24,25 In terms of C4, recent studies found that the plasma level of C4 is expanded in SCZ patients at the intense phase of disease and can be diminished by antipsychotic prescription.24,26 In the present study, the total hemolytic activity of the complement and the activities of individual complement components, C1, C2, C3, and C4, were assessed in the blood serum of 89 patients with SCZ and 89 healthy controls. Consistent to previous studies, our results also showed that the serum levels of C3 and C4 were higher in patients with SCZ compared to healthy controls. To the best of our knowledge, the results of the present study firstly found that patients with SCZ exhibited higher serum levels of C1, C2, and CH50. Taken together, these findings provide more data linking complement system to SCZ.
Several potential diagnostic biomarkers including malondialdehyde (MDA),27 prolidase activity,28 and G protein-coupled estrogen receptor29 for SCZ have been reported. To investigate the potential value of these aberrant complement factors as diagnostic biomarkers for SCZ, ROC analysis was performed and the AUC values of C1, C2, C3, C4, and CH50 were all <0.7. Considering that the AUC value in ROC analysis should be greater than 0.7 in order to have clinical value for screening,30 and combining multiple serum proteins as a single group can improve the sensitivity or specificity of a single biomarker,31 the diagnostic value for SCZ of a combined panel of C1, C2, C3, C4, and CH50 was evaluated in the present study. The results showed that this panel’s AUC increased to 0.857, indicating that it has significant potential as biomarkers for identifying SCZ patients.
BPRS, SANS, and SAPS are the most widely used interview scales for evaluation of the severity of psychiatric symptoms.32–34 Thus, the severity of psychiatric symptoms in patients with SCZ was evaluated by these scales in the present study. A few studies have explored the relationship between the severity of psychiatric symptoms and complement system in patients with SCZ. It has been shown that the C4/C3 ratio was significantly positively correlated with BPRS positive scores in patient with psychosis.35 Another study found that increases in C3 and C4 were associated with reductions in total PANSS psychopathology scores.36 In the present study, serum C2, C3, and CH50 levels were positively correlated to the scores of SANS, SAPS, and BPRS in patients with SCZ, respectively. The reasons for these relationships between the severity of psychiatric symptoms and complement system remain unclear. In light of the relatively small sample size and the single-center design of this study, further multicentric studies are needed to confirm these findings, and the specific mechanisms underlying these relationships require further investigation.
The current study has some limitations that need to be considered. First, there is a possibility of sampling bias in this study as a result of the small sample size and one-center design. Second, there is no causal relationship between psychiatric symptoms and the complement system in this cross-sectional study. Third, not all complement factors were analyzed due to constraints related to funding.
In conclusion, this study demonstrates that a combined panel of C1, C2, C3, C4, and CH50 may be useful as diagnostic biomarkers for identifying first-episode SCZ patients. To confirm these complement factors’ potential as novel SCZ biomarkers, multicentric studies are clearly required. To examine the causal relationship between complement factors and the severity of psychiatric symptoms, longitudinal studies are warranted.
Funding
This study was provided by the Research Fund Project of Anhui Medical University (Project No: 2021xkj113), Research Fund Project of Hefei Fourth People’s Hospital (Project No: HFSY202109), Hefei Seventh cycle Key Medical Specialty, and Anhui Province Medical and Health Key Specialty Construction Project.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kahn R, Sommer I, Murray R, et al. Schizophrenia. Nat Rev Dis Primers. 2015;1:15067. doi:10.1038/nrdp.2015.67
2. Murray C, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. doi:10.1016/S0140-6736(12)61689-4
3. Jauhar S, Johnstone M, McKenna P. Schizophrenia. Lancet. 2022;399:473–486. doi:10.1016/S0140-6736(21)01730-X
4. Ollà I, Pardiñas A, Parras A, et al. Pathogenic mis-splicing of CPEB4 in schizophrenia. Biol Psychiatry. 2023. doi:10.1016/j.biopsych.2023.03.010
5. McCutcheon R, Reis Marques T, Howes O. Schizophrenia-an overview. JAMA psychiatry. 2020;77:201–210. doi:10.1001/jamapsychiatry.2019.3360
6. van Kesteren C, Gremmels H, de Witte L, et al. Immune involvement in the pathogenesis of schizophrenia: a meta-analysis on postmortem brain studies. Transl Psychiatry. 2017;7:e1075. doi:10.1038/tp.2017.4
7. Khandaker G, Cousins L, Deakin J, Lennox B, Yolken R, Jones P. Inflammation and immunity in schizophrenia: implications for pathophysiology and treatment. Lancet Psychiatr. 2015;2:258–270. doi:10.1016/S2215-0366(14)00122-9
8. Khandaker G, Dantzer R. Is there a role for immune-to-brain communication in schizophrenia? Psychopharmacology. 2016;233:1559–1573. doi:10.1007/s00213-015-3975-1
9. Upthegrove R, Manzanares-Teson N, Barnes N. Cytokine function in medication-naive first episode psychosis: a systematic review and meta-analysis. Schizophr Res. 2014;155:101–108. doi:10.1016/j.schres.2014.03.005
10. Dickerson F, Stallings C, Origoni A, et al. Inflammatory markers in recent onset psychosis and chronic schizophrenia. Schizophr Bull. 2016;42:134–141. doi:10.1093/schbul/sbv108
11. Volk D. Role of microglia disturbances and immune-related marker abnormalities in cortical circuitry dysfunction in schizophrenia. Neurobiol Dis. 2017;99:58–65. doi:10.1016/j.nbd.2016.12.019
12. Ricklin D, Hajishengallis G, Yang K, Lambris J. Complement: a key system for immune surveillance and homeostasis. Nat Immunol. 2010;11:785–797. doi:10.1038/ni.1923
13. Schartz N, Tenner A. The good, the bad, and the opportunities of the complement system in neurodegenerative disease. J Neuroinflammation. 2020;17:354. doi:10.1186/s12974-020-02024-8
14. Heneka M, McManus R, Latz E. Inflammasome signalling in brain function and neurodegenerative disease. Nat Rev Neurosci. 2018;19:610–621. doi:10.1038/s41583-018-0055-7
15. Pouw R, Ricklin D. Tipping the balance: intricate roles of the complement system in disease and therapy. Semin Immunopathol. 2021;43:757–771. doi:10.1007/s00281-021-00892-7
16. Magdalon J, Mansur F, Teles E, et al. Complement system in brain architecture and neurodevelopmental disorders. Front Neurosci. 2020;14:23. doi:10.3389/fnins.2020.00023
17. Namatame C, Misu T, Takai Y, et al. CH50 as a putative biomarker of eculizumab treatment in neuromyelitis optica spectrum disorder. Heliyon. 2021;7:e05899. doi:10.1016/j.heliyon.2021.e05899
18. Guo W, Gu Y, Zhou J, Wang X, Sun Q. Characteristics and associated factors of violence in male patients with schizophrenia in China. Front Psychiatr. 2023;14:1106950. doi:10.3389/fpsyt.2023.1106950
19. Tibber M, Kirkbride J, Joyce E, et al. The component structure of the scales for the assessment of positive and negative symptoms in first-episode psychosis and its dependence on variations in analytic methods. Psychiatry Res. 2018;270:869–879. doi:10.1016/j.psychres.2018.10.046
20. Hurşitoğlu O, Kurutas E, Strawbridge R, Uygur O, Yildiz E, Reilly T. Serum NOX1 and raftlin as new potential biomarkers of interest in schizophrenia: a preliminary study. Neuropsychiatr Dis Treat. 2022;18:2519–2527. doi:10.2147/NDT.S385631
21. Goldsmith D, Rapaport M, Miller B. A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder and depression. Mol Psychiatry. 2016;21:1696–1709. doi:10.1038/mp.2016.3
22. Al-Hakeim H, Al-Rammahi D, Al-Dujaili A. IL-6, IL-18, sIL-2R, and TNFα proinflammatory markers in depression and schizophrenia patients who are free of overt inflammation. J Affect Disord. 2015;182:106–114. doi:10.1016/j.jad.2015.04.044
23. Carroll M. The complement system in regulation of adaptive immunity. Nat Immunol. 2004;5:981–986. doi:10.1038/ni1113
24. Chen Y, Zhao Z, Lin F, Wang L, Lin Z, Yue W. Associations between genotype and peripheral complement proteins in first-episode psychosis: evidences from C3 and C4. Front Genet. 2021;12:647246. doi:10.3389/fgene.2021.647246
25. Ali F, Abd El-Azeem E, Hamed M, Ali M, Abd Al-Kader N, Hassan E. Redox dysregulation, immuno-inflammatory alterations and genetic variants of BDNF and MMP-9 in schizophrenia: pathophysiological and phenotypic implications. Schizophr Res. 2017;188:98–109. doi:10.1016/j.schres.2017.01.016
26. Su J, Feng X, Chen K, Fang Z, Zhang H. Plasma complement component 4 alterations in patients with schizophrenia before and after antipsychotic treatment. Asian J Psychiatr. 2022;73:103110. doi:10.1016/j.ajp.2022.103110
27. Hurşitoğlu O, Orhan F, Kurutaş E, Doğaner A, Durmuş H, Kopar H. Diagnostic performance of increased malondialdehyde level and oxidative stress in patients with schizophrenia. Noro psikiyatri arsivi. 2021;58:184–188. doi:10.29399/npa.27372
28. Güneş M, Bulut M, Demir S, et al. Diagnostic performance of increased prolidase activity in schizophrenia. Neurosci Lett. 2016;613:36–40. doi:10.1016/j.neulet.2015.12.036
29. Hursitoglu O, Orhan FO, Kurutas EB, Doganer A, Durmus HT, Bozkusc O. Evaluation serum levels of g protein-coupled estrogen receptor and its diagnostic value in patients with schizophrenia. Memory. 2020;33:34.
30. Swets J. Measuring the accuracy of diagnostic systems. Science. 1988;240:1285–1293. doi:10.1126/science.3287615
31. Luo P, Yin P, Hua R, et al. A Large-scale, multicenter serum metabolite biomarker identification study for the early detection of hepatocellular carcinoma. Hepatology. 2018;67:662–675. doi:10.1002/hep.29561
32. Thakkar K, Schall J, Logan G, Park S. Response inhibition and response monitoring in a saccadic double-step task in schizophrenia. Brain Cogn. 2015;95:90–98. doi:10.1016/j.bandc.2015.01.007
33. Zhao Y, Ma T, Zhang L, Ran X, Zhang R, Ku Y. Atypically larger variability of resource allocation accounts for visual working memory deficits in schizophrenia. PLoS Comput Biol. 2021;17:e1009544. doi:10.1371/journal.pcbi.1009544
34. Lottman K, Gawne T, Kraguljac N, Killen J, Reid M, Lahti A. Examining resting-state functional connectivity in first-episode schizophrenia with 7T fMRI and MEG. NeuroImage Clin. 2019;24:101959. doi:10.1016/j.nicl.2019.101959
35. Laskaris L, Zalesky A, Weickert C, et al. Investigation of peripheral complement factors across stages of psychosis. Schizophr Res. 2019;204:30–37. doi:10.1016/j.schres.2018.11.035
36. Li H, Zhang Q, Li N, et al. Plasma levels of Th17-related cytokines and complement C3 correlated with aggressive behavior in patients with schizophrenia. Psychiatry Res. 2016;246:700–706. doi:10.1016/j.psychres.2016.10.061
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


