Back to Journals » Patient Preference and Adherence » Volume 17
Perception and Willingness to Use Telepharmacy Among the General Population in Jordan
Authors Abu-Farha R , Alzoubi KH , Abu Assab M , Awwad O, Gharaibeh L , Mukattash TL , Halboup AM
Received 1 July 2023
Accepted for publication 18 August 2023
Published 25 August 2023 Volume 2023:17 Pages 2131—2140
DOI https://doi.org/10.2147/PPA.S428470
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Rana Abu-Farha,1 Karem H Alzoubi,2,3 Mohammad Abu Assab,4 Oriana Awwad,5 Lobna Gharaibeh,6 Tareq L Mukattash,3 Abdulsalam M Halboup7,8
1Clinical Pharmacy and Therapeutics Department, Faculty of Pharmacy, Applied Science Private University, Amman, Jordan; 2Department of Pharmacy Practice and Pharmacotherapeutics, University of Sharjah, Sharjah, United Arab Emirates; 3Department of Clinical Pharmacy, Faculty of Pharmacy, Jordan University of Science and Technology, Irbid, Jordan; 4Department of Clinical Pharmacy, Faculty of Pharmacy, Zarqa University, Zarqa, Jordan; 5Department Biopharmaceutics and Clinical Pharmacy, Faculty of Pharmacy, The University of Jordan, Amman, Jordan; 6Pharmacological and Diagnostic Research Center, Faculty of Pharmacy, Al-Ahliyya Amman University, Amman, Jordan; 7Department of Clinical Pharmacy and Pharmacy Practice, University of Science and Technology, Sana’a, Yemen; 8Discipline of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia
Correspondence: Abdulsalam M Halboup, Department of Clinical Pharmacy and Pharmacy Practice, University of Science and Technology, P.O.Box 13064, Sana’a, Yemen, Tel +967774960247, Email [email protected]
Objective: This research aimed to explore how telepharmacy is perceived, whether it would be willingly used by the overall population in Jordan, and the associated socioeconomic disparities that might affect its acceptance.
Methods: This is a survey-based cross-sectional study involving the general public of Jordan. The study took place in various Jordanian cities from May 2nd to June 1st, 2023. Using Google forms, the questionnaire was shared through various social media channels (such as Facebook and WhatsApp).
Results: The questionnaire received responses from 800 participants. The data showed that a sizable portion of the Jordanian population were unaware of telepharmacy (n= 343, 42.9%), and a majority had never utilized it (n= 131, 16.4%). The participants viewed the main advantage of telepharmacy as minimizing unnecessary trips to pharmacies (n= 668, 83.5%) and reducing travel time and expenses (n= 632, 79.0%). However, the primary concern was the mental effort required to use this service (n= 465, 58.1%). Of the respondents, 61.3% (n= 490) indicated a willingness to adopt telepharmacy services in the future. Regression analysis indicated that men were more likely to use this service compared to women (OR= 1.947, p< 0.001), and people living in northern and southern Jordan exhibited a greater willingness compared to those inhabiting the central region (OR= 2.168, p< 0.001).
Conclusion: The results reveal a positive attitude towards and a significant readiness to embrace telepharmacy among the Jordanian population. However, for broader acceptance and utilization, apprehensions regarding the service need to be addressed. Doing so could improve access to pharmaceutical care, particularly for patients living in far-flung areas of Jordan.
Keywords: telepharmacy, public, perception, willingness, Jordan
Introduction
Telehealth is the provision of medical services and health care remotely, using information technology and communication tools.1 Several are the fields of telehealth, with telepharmacy referring to the use of telecommunication to deliver patients’ pharmaceutical care.2 This virtual approach of healthcare provision can be particularly useful among patients living in rural areas, where appropriate pharmaceutical care services are not available, or when such service cannot be provided in-person.3
After the spread of COVID-19, the use of telepharmacy increased significantly to account for the lack of in-person consultation, as a way to provide optimal management to patients requiring pharmaceutical care during the pandemic.4–6 As a result, the traditional way to provide pharmacotherapy care has been combined with information technology solutions that were quickly integrated in the pharmacy practice framework, opening the opportunity to embrace related trainings into the pharmacy curricula.4,5,7
Advantages of telepharmacy include the reduction of treatment-related problems, increase adherence to medication, reduce adverse drug events and improve medication use outcomes thus enhancing the quality of pharmacy services provided to patients.8,9 It has been also showed to reduce hospital admissions during the pandemic, diminish burden on hospitals, and save time to patients and staff.4,10,11 Telepharmacy allows for a personalized interaction between the patient and the pharmacist to include patient-care services such as counseling, assessment of medication adherence, as well as comprehensive medication review.2,8,12
Jordan, a developing Middle Eastern country, had a population of around 10.2 million in 2020, with an average age of 22.8 and a slightly higher male-to-female ratio. The majority are Arab Muslims, and the literacy rate was 98% in 2015.13 In Jordan, the provision of pharmaceutical care is very satisfactory among the Jordanian community although pharmacies still adopt the conventional system to provide pharmaceutical care services, with only a few instances of limited consultations through social media.14 No telepharmacy has been ever implemented with a number of scientific reports addressing the need for such services.15,16 In order to implement it and optimize its use, efforts are needed providing pharmacists and the community with the appropriate knowledge and digital health to assure a good, equitable and ethical access to this technology.17 An important step to start with is understanding the perception/willingness of Jordanians toward the use of telepharmacy and investigating the sociodemographic characteristics that can mostly impact it.
In a recent study conducted in Jordan, pharmacists expressed a positive attitude to the implementation of telepharmacy.18 On the same line, Jordanians showed to have favorable perceptions towards telemedicine.19 Nonetheless, no information is available regarding the use of telepharmacy among Jordanians. This study thus aimed to investigate the perception and willingness to use telepharmacy among the general population in Jordan as well as to investigate the socioeconomic disparities in patient use of telepharmacy.
Materials and Methods
Study Design, Setting, and Sampling Method
This was a survey-based cross-sectional study conducted among the general Jordanian public. Participants were recruited from different Jordanian cities between May 2nd, 2023, and June First, 2023. Inclusion criteria was any Jordanian aged 18 years or above currently living in Jordan. The study questionnaire was uploaded to the Google form platform. A convenient sampling method was utilized through snowball effect and distribution of the online questionnaire via different social media platforms (Facebook and WhatsApp). A trained research assistant provided participants with a link to fill the form and a cover letter at the beginning of the questionnaire explained to the participants the goals of the study and guaranteed the anonymity of the participants. Each participant was also requested to invite others from their network to participate. The research assistant conducted regular follow-ups during data collection to ensure representation from various settings and entities within Jordanian society.
Development of the Survey
The initial draft of the study questionnaire was developed following extensive literature review of previous studies that evaluated public and healthcare providers’ knowledge, perceptions, and readiness towards the implementation of telepharmacy and telemedicine services.19–21 Following that, four independent experts conducted content and face validation, reviewed the initial draft of the questionnaire, and appropriate modifications were made accordingly.
The questionnaire’s final version (Supplementary File) contained seven sections. The first section comprised the sociodemographic characteristics of the participants. The second part included closed-ended questions to evaluate public awareness of telepharmacy services. The third and fourth parts evaluated the perceived benefits and concerns by the public related to the implementation of telepharmacy. The last part assessed the willingness of the public to use telepharmacy services. A Likert scale of five points that ranged between strongly agree (5) to strongly disagree (1) was employed to evaluate public perceived benefits and concerns (sections three and four).
Prior to distributing the survey, a preliminary assessment was conducted with a group of ten individuals. These participants were asked to assess the organization, comprehensibility, and length of the survey, as well as to provide their overall feedback. The results from the pilot testing were excluded from the eventual data analysis. Following pilot testing, Cronbach alpha values of 0.900, and 0.867 were reported for sections three and four, respectively, indicating that the internal consistency of the questionnaire items was acceptable.22
Sample Size Calculation
The sample size was determined based on the requirement of logistic regression analysis as per the recommendation of Fidell’s and Tabachnick.23 Based on their recommendations; 5–20 subjects are needed for each independent predictor. Using the upper limit, which is 20 subjects per predictor and having 10 predictors, the minimum sample size required was estimated at 200 subjects.
Ethical Approval
The Institutional Review Board (IRB) of the Private Applied Sciences University, Jordan, approved the study’s protocol (Approval number: 2023-PHA-23). Prior to filing out the study questionnaire, all participants provided their electronic consent of participation. The questionnaire includes a statement for volunteer participation, and participants confirmed their consent by selecting the “agree to participate” option before proceeding to the study questions. The current study was done following the Declaration of Helsinki of the World Medical Association.
Statistical Analysis
The Excel sheet obtained from Google Forms was downloaded and then exported to the Statistical Package for Social Science (SPSS) version 22 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were presented as frequency and percentage of qualitative variables and median and interquartile range (IQR) for quantitative variables. Normality was tested via the Shapiro–Wilk test. The P ≤ 0.05 indicated non-normal distribution.
Logistic regression analysis was carried out for possible predictors of the participants’ willingness to use telepharmacy services. Simple logistic regression was conducted to identify variables with P-value less than 0.250 which were then included in subsequent multiple logistic regression analysis. Before carrying out multiple logistic regression, absence of multicollinearity among variables was checked (Pearson correlation coefficient between any two variables should be less than 0.9). Internal consistency of the questionnaire was confirmed, Cronbach alpha value was more than 0.70.22 P-value ≤ 0.05 was considered statistically significant.
Results
A total of 800 participants responded and filled the questionnaire, most of them were women (n= 517, 64.6%). Participants had a median age of 33.0 years (IQR= 20.0), and almost two-thirds of the participants had an education higher than high school (n= 578, 72.3%). Over half of the participants had low monthly income (lower than 400 JOD) (n= 469, 58.6%), and around 39% had a biomedical-related degree (n= 313, 39.1%). Among the study participants, 19.3% reported to have chronic diseases (n= 154), and many of them are frequent visitors of the pharmacy with 2 or more visits per month (n= 346, 45.5%). The general characteristics of the participants are shown in Table 1.
 |
Table 1 Sociodemographic Characteristics of the Study Participants (N= 800) |
Telepharmacy is a new concept in Jordan, this explains the fact that 42.9% of participants (n= 343) have never heard of telepharmacy, and the percentage of those who used telepharmacy is even lower (n= 131, 16.4%), Figure 1.
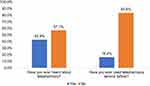 |
Figure 1 Participant’s awareness and previous use of telepharmacy services (n= 800). |
Telepharmacy can help provide convenience and easier access to pharmaceutical services. The public acknowledged these benefits of telepharmacy, the most important was decreasing unnecessary visits to pharmacies (n= 668, 83.5%), followed by the reduction in travel time and costs (n= 632, 79.0%), protection of patients in pandemics (n= 631, 78.9%), and saving the waiting time problem in most pharmacies (n= 621, 77.6%). More details about participants’ perceived benefits of telepharmacy are presented in Table 2.
 |
Table 2 Participants’ Perceived Benefits of Telepharmacy (N= 800) |
The concerns on the use of telepharmacy that the participants revealed (Table 3) were the mental effort it required (n= 465, 58.1%), subsequent communication and medication errors that could happen when drug orders and pharmaceutical care services are not delivered in person (n= 464, 58.0%). In general, half of the study population still did not perceive the suggested concerns as problematic.
 |
Table 3 Participants’ Perceived Concerns About Telepharmacy (N= 800) |
Among the study participants, 61.3% (n= 490) reported that they are willing to use telepharmacy services in the future, the remaining participants were either hesitant (n= 224, 28.0%) or unwilling (n= 86, 10.8%) to use the services. When the participants who were willing to use the service were introduced to the different services that can be obtained through telepharmacy, most of them were willing to benefit from remote patient counseling (n= 444, 90.6%). Home medication review was another telepharmacy activity that many participants were willing to use (n= 431, 88.0%). Although remote medication dispensing (n= 389, 79.4%) had lower public acceptance, all other activities received over 80% approval, highlighting strong overall telepharmacy acceptance as shown in Figure 2.
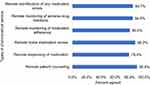 |
Figure 2 Types of pharmaceutical services participants willing to us (n= 490). |
Finally, logistic regression analysis was performed to assess predictors affecting participants’ willingness to use telepharmacy service (Table 4), and results showed that males were more willing to use the service than females (OR= 1.947, p<0.001). Moreover, participants living in the north and south of Jordan were more willing to use the service compared to those living in the center of Jordan (OR= 2.168, p<0.001). The logistic regression model had an acceptable fit, χ2 (8)= 13.350, p= 0.100 (Hosmer–Lemeshow goodness-of-fit). The model explained 8.4% (Nagelkerke R2) of participants’ willingness to use telepharmacy service and correctly classified 65.1% of cases.
 |
Table 4 Assessment of Factors Associated with Participants’ Willingness to Use Telepharmacy Service |
Discussion
This study came to investigate the perception and willingness to use telepharmacy among the general population in Jordan and the related socioeconomic disparities to using this service, as such understanding is crucial to comprehend the acceptance, introduction, and optimization of telepharmacy.
The study showed that an appreciable percentage of the Jordanian population had never heard about telepharmacy, and most of them never used it. These findings are expected as telepharmacy is one of the eHealth services not yet implemented in Jordan. Nevertheless, the study revealed that Jordanians have favorable views regarding the potential benefits of telepharmacy, particularly effort and time savings. These positive views are consistent with studies on telepharmacy24,25 and telemedicine in general.19,26 Likewise, aligning with other studies on telepharmacy,27,28 the study showed that protecting patients during pandemics and convenience to patients living in remote areas are other vital perceived benefits in favor of telepharmacy.
Furthermore, the study revealed that Jordanian populations are willing to utilize telepharmacy, with strong motives for this service acceptance and adoption, providing them convenience and accessibility to multiple remote pharmaceutical care and medication-related services relevant to their health issues. In particular, remote patient counseling, remote home medication review, and remote identification of medication errors. Similar results have been reported in various contexts, indicating the patients’ desire to use telepharmacy services.29,30
Identifying sociodemographic predictors of the willingness to telepharmacy service utilization has important implications for its implementation in the country. Among the ten predictors investigated in this study, the findings from the logistic regression analysis conducted revealed a significant impact of gender, as well as geographic location, on the willingness of the Jordanians to use telepharmacy. Explicitly, males were significantly more willing to use telepharmacy than females, and participants residing in remote areas (in the north and south) of Jordan were significantly more willing to use the service than those in the central region.
Previous research on gender differences in telehealth and telepharmacy use has shown conflicting results, with some studies suggesting that women are more accepting, others proposing that men are more accepting, and others showing no difference in the utilization level.31–34 Various factors, such as differences in eHealth literacy, health-seeking habits, attitudes toward technology, and convenience preferences, may impact this gender disparity.35 Further research is required to understand the underlying causes of these gender differences in Jordanians’ telepharmacy usage willingness and to provide focused interventions that address potential hurdles unique to each gender.
The greater willingness to use telepharmacy seen in the north and south areas of Jordan reflects a more robust understanding of the potential benefits offered by telepharmacy in addressing accessibility difficulties among rural area residents. This finding is consistent with other studies showing that telemedicine and telepharmacy could be crucial in bridging healthcare disparities in distant places.36,37
Although the study’s regression model explained variance of participants’ willingness to use telepharmacy is relatively low (8.4%), its classification accuracy of (65.1%) entails that it can help identify individuals who are more likely to be willing to use telepharmacy services (Nagelkerke R2). Of note, willingness to use telepharmacy is a multifactorial behavior that can be influenced by various individual, cultural, and contextual factors.37,38 In this regard, future research is immanent to identify the other predictors beyond those included in the study and adequately capture the numerous aspects impacting willingness to use telepharmacy in Jordan.
Although Jordanians in this study showed a positive perception and high willingness to use telepharmacy, successfully implementing this service requires addressing their concerns about adopting telepharmacy. This study revealed the most commonly identified Jordanians’ perceived worries related to the acceptance and adoption of telepharmacy, including the mental effort needed, possible communication and medication errors, and the inability to build professional relationships with pharmacists with virtual interactions during the service delivery. These concerns about using telepharmacy are varied from those reported by the study that investigated the adoption and usage of telemedicine among Jordanians, concluding that privacy, medical errors, and capacity for accurate diagnosis were the most prevalent.19 This variability can be attributed to the specific nature and context of telepharmacy compared to telemedicine and the subsequent differences in both studies’ questionnaire designs.
In light of the study findings, the potential perceived benefits and the high willingness to use telepharmacy among the general population in Jordan, besides identifying gender and geographical location as predictors of their willingness to use the service, provide vital initiatives for telepharmacy implementation in Jordan. Furthermore, mitigation of the identified public concerns regarding telepharmacy acceptance and adoption is necessary to pave the way for this service use and optimization. Collaboration between policymakers, healthcare professionals, and technical telepharmacy providers is essential to build the capacity for telepharmacy adoption in Jordan. Successful implementation relies on addressing these challenges while leveraging the advantages of remote healthcare services.
The study has a few limitations, as the convenient sampling design limits the generalizability of the study results. While the applied logistic regression analysis provided valuable insights, the analysis did not include other potential influencing factors such as eHealth literacy, health-seeking habits, and attitudes toward technology among the Jordanian population. Despite these few limitations, the study is the first to assess the use of telepharmacy and investigate the socioeconomic disparities related to willingness to use the service among Jordanians. Additionally, it identified their worries that may pose potential barriers to telepharmacy adoption.
Conclusion
The findings of this study demonstrate a positive perception and high willingness to use telepharmacy among the general population in Jordan. However, to ensure widespread acceptance and adoption of telepharmacy, concerns related to the mental effort needed, possible communication and medication errors, and the inability to build professional relationships with pharmacists due to the lack of physical interaction during telepharmacy delivery should be mitigated. By doing so, telepharmacy can potentially enhance access to pharmaceutical care services, especially for patients residing in distant areas of Jordan, offering convenience and cost saving. Subsequent research should address study limitations and incorporate a wide range of influential factors for a comprehensive understanding of telepharmacy adoption among the general population in Jordan.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Telemedicine: opportunities and developments in member states. Report on the second global survey on eHealth. World Health Organization; 2010.
2. Alexander E, Butler CD, Darr A, et al. ASHP statement on telepharmacy. Am J Health Syst Pharm. 2017;74(9):e236–e41. doi:10.2146/ajhp170039
3. Chambers B, Fleming C, Packer A, Botha L, Hawthorn G, Nott S. Virtual clinical pharmacy services: a model of care to improve medication safety in rural and remote Australian health services. Am J Health Syst Pharm. 2022;79(16):1376–1384. doi:10.1093/ajhp/zxac082
4. Mohamed Ibrahim O, Ibrahim RM, Abdel-Qader DH, Al Meslamani AZ, Al Mazrouei N. Evaluation of telepharmacy services in light of COVID-19. Telemed e-Health. 2021;27(6):649–656. doi:10.1089/tmj.2020.0283
5. Khoshnam‐Rad N, Gholamzadeh M, Gharabaghi MA, Amini S. Rapid implementation of telepharmacy service to improve patient-centric care and multidisciplinary collaboration across hospitals in a COVID era: a cross-sectional qualitative study. Health Sci Rep. 2022;5(6):e851. doi:10.1002/hsr2.851
6. Jirjees F, Odeh M, Aloum L, Kharaba Z, Alzoubi KH, Al-Obaidi HJ. The rise of telepharmacy services during the COVID-19 pandemic: a comprehensive assessment of services in the United Arab Emirates. Pharm Pract. 2022;20(2):1–11. doi:10.18549/PharmPract.2022.2.2634
7. Dickinson D. Please take a seat in the virtual waiting room: telepharmacy education in the pharmacy curriculum. Curr Pharm Teach Learn. 2022;14(2):127–129. doi:10.1016/j.cptl.2021.11.034
8. Hanjani LS, Caffery LJ, Freeman CR, Peeters G, Peel NM. A scoping review of the use and impact of telehealth medication reviews. Res Social Adm Pharm. 2020;16(8):1140–1153. doi:10.1016/j.sapharm.2019.12.014
9. Baldoni S, Amenta F, Ricci G. Telepharmacy services: present status and future perspectives: a review. Medicina. 2019;55(7):327. doi:10.3390/medicina55070327
10. Hefti E, Wei B, Engelen K. Access to Telepharmacy services may reduce hospital admissions in outpatient populations during the COVID-19 pandemic. Telemed e-Health. 2022;28(9):1324–1331. doi:10.1089/tmj.2021.0420
11. Gil-Candel M, Solana-Altabella A, Vicente-Escrig E, et al. Developing a telepharmacy programme with home medication dispensing and informed delivery in a tertiary hospital: description of the model and analysis of the results. Eur J Hosp Pharm. 2023;30(2):107–112. doi:10.1136/ejhpharm-2021-003194
12. Miller MJ, Kane-Gill SL. Pandemic stimulates a variety of telepharmacy applications: considerations for implementation, sustainability, and future directions. Am J Health Syst Pharm. 2022;79(11):918–920. doi:10.1093/ajhp/zxac100
13. Al-Hassan S. Education and parenting in Jordan. School systems, parent behavior, and academic achievement. Int Perspect. 2019;2019:55–65.
14. Abu-Farha R, Alzoubi KH, Alkhawaldeh R, Awwad O, Mukattash T, Alefishat E. Public satisfaction with community pharmacists roles as healthcare providers: a cross-sectional study from Jordan. J Res Pharm Pract. 2023;14(1):42–48.
15. Saifan AR, Alarabyat IA, Alrimawi I, Al-Nsair N. Utilizing telehealth intervention to support patients with cardiovascular diseases in Jordan: a qualitative study. J Appl Nurs Res. 2022;68:151641. doi:10.1016/j.apnr.2022.151641
16. Obeidat AZ, El-Salem K A National Telemedicine Program in the Kingdom of Jordan–Editorial. Elsevier; 2021:145–149.
17. Darrat I, Tam S, Boulis M, Williams AM. Socioeconomic disparities in patient use of telehealth during the coronavirus disease 2019 surge. JAMA Otolaryngol Head Neck Surg. 2021;147(3):287–295. doi:10.1001/jamaoto.2020.5161
18. Muflih SM, Al‐Azzam S, Abuhammad S, Jaradat SK, Karasneh R, Shawaqfeh MS. Pharmacists’ experience, competence and perception of telepharmacy technology in response to COVID‐19. Int J Clin Pract. 2021;75(7):e14209. doi:10.1111/ijcp.14209
19. Murshidi R, Hammouri M, Taha H, et al. Knowledge, attitudes, and perceptions of Jordanians towards the adopting and utilization of telemedicine: a national cross-sectional study. JMIR Hum Factors. 2022;9:e41499. doi:10.2196/41499
20. Elnaem MH, Akkawi ME, Al-Shami AK, Elkalmi R. Telepharmacy knowledge, perceptions, and readiness among future Malaysian pharmacists amid the COVID-19 pandemic. Indian J Pharm Educ Res. 2022;56(1):9–16. doi:10.5530/ijper.56.1.2
21. Muhammad K, Baraka MA, Shah SS, et al. Exploring the perception and readiness of Pharmacists towards telepharmacy implementation; a cross sectional analysis. PeerJ. 2022;10:e13296. doi:10.7717/peerj.13296
22. Taber KS. The use of cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018;48(6):1273–1296. doi:10.1007/s11165-016-9602-2
23. Tabachnick BG, Fidell LS. Using Multivariate Statistic.
24. Moulaei K, Shanbehzadeh M, Bahaadinbeigy K, Kazemi-Arpanahi H. Survey of the patients’ perspectives and preferences in adopting telepharmacy versus in-person visits to the pharmacy: a feasibility study during the COVID-19 pandemic. BMC Med Inform Decis Mak. 2022;22(1):99. doi:10.1186/s12911-022-01834-5
25. Matsumoto Y, Kizaki H, Ikeda Y, et al. Telepharmacy in mountainous depopulated areas of Japan: an exploratory interview study of patients’ perspectives. Drug Discov Ther. 2021;15(6):337–340. doi:10.5582/ddt.2021.01102
26. Manzoor M, Maziz MNH, Subrimanyan V, et al. Attitudes towards and the confidence in acceptance of telemedicine among the people in Sabah, Malaysia. Int J Health Sci. 2022;2022:2376–2386.
27. Li H, Zheng S, Li D, et al. The establishment and practice of pharmacy care service based on Internet social media: telemedicine in response to the COVID-19 pandemic. Front Pharmacol. 2021;12:707442. doi:10.3389/fphar.2021.707442
28. Dat TV, Tu VL, Quan NK, et al. Telepharmacy: a systematic review of field application, benefits, limitations, and applicability during the COVID-19 pandemic. Telemed e-Health. 2023;29(2):209–221. doi:10.1089/tmj.2021.0575
29. Pathak S, Blanchard CM, Moreton E, Urick BY. A systematic review of the effect of telepharmacy services in the community pharmacy setting on care quality and patient safety. J Health Care Poor Underserved. 2021;32(2):737–750. doi:10.1353/hpu.2021.0102
30. Escalona Y, Espiritu JC, Natividad D, Tambuli K, Rampak S. A Review of Telepharmacy in Asia. Int J Res Publ Rev. 2022;2582:7421.
31. Alnajrani RH, Alnajrani NR, Aldakheel FS, et al. An assessment of the knowledge, perception, and willingness to use telepharmacy services among the general public in the Kingdom of Saudi Arabia. Cureus. 2022;14(11). doi:10.7759/cureus.31769
32. Tjiptoatmadja NN, Alfian SD. Knowledge, perception, and willingness to use telepharmacy among the general population in Indonesia. Front Public Health. 2022;2022:10.
33. Nduka SO, Nwaodu MA, Nduka IJ. Telepharmacy services in a developing country: Nigerian community pharmacists’ and patients’ perspectives on the clinical benefits, cost, and challenges. Telemed e-Health. 2022;29:1238–1251. doi:10.1089/tmj.2022.0385
34. Schmitz A, Díaz-Martín AM, Guillén MJY. Modifying UTAUT2 for a cross-country comparison of telemedicine adoption. Comput Human Behav. 2022;130:107183. doi:10.1016/j.chb.2022.107183
35. Reiners F, Sturm J, Bouw LJW, Wouters EJM. Sociodemographic factors influencing the use of eHealth in people with chronic diseases. Int J Environ Res Public Health. 2019;16(4):645. doi:10.3390/ijerph16040645
36. Pathak S, Haynes M, Qato DM, Urick BY. Peer reviewed: telepharmacy and quality of medication use in rural areas, 2013–2019. Prev Chronic Dis. 2020;2020:17.
37. Karnvar AS, Kashikar VS, Dhole SN. A review on telepharmacy services. Ijpra. 2020;5(2):619–623.
38. Mishra PP, Mohapatra S. A progress review on current state of affairs on telepharmacy and telemedicine service. High Technol Lett. 2022;28(12):409–431.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
