Back to Journals » Open Access Emergency Medicine » Volume 14
Perception and Satisfaction of Patients’ Relatives Regarding Emergency Medical Service Response Times: A Cross-Sectional Study
Authors Huabbangyang T , Sangketchon C, Piewthamai K, Saengmanee K, Ruangchai K, Bunkhamsaen N, Keawjanrit P, Tonsawan R
Received 27 January 2022
Accepted for publication 6 April 2022
Published 13 April 2022 Volume 2022:14 Pages 155—163
DOI https://doi.org/10.2147/OAEM.S360114
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Hans-Christoph Pape
Thongpitak Huabbangyang,1 Chunlanee Sangketchon,1 Kritsadavadee Piewthamai,2 Kamthorn Saengmanee,2 Kanuangwan Ruangchai,2 Nantiya Bunkhamsaen,2 Pornchita Keawjanrit,2 Ruthaichanok Tonsawan2
1Department of Disaster and Emergency Medical Operation, Faculty of Science and Health Technology, Navamindradhiraj University, Bangkok, Thailand; 2Faculty of Medicine, Vajira Hospital, Navamindradhiraj University, Bangkok, Thailand
Correspondence: Chunlanee Sangketchon, Tel +66 22443878, Email [email protected]
Purpose: Delays in emergency medical service (EMS) directly affect life-threatening emergencies. Delays also indirectly affect the perception and satisfaction of patients and their relatives, which are important qualitative EMS indicators.
Patients and Methods: For this cross-sectional study, data was collected from May 1 to July 31, 2021, through questionnaires developed by the authors. The study sample consisted of relatives of EMS patients. The primary objective was the perceived EMS response time, which was compared to the actual EMS response time. The secondary objective was the relatives’ perceptions and feelings regarding the waiting time.
Results: During study period, the sample was 165 relatives of patients managed by EMS. The mean perceived EMS response time of 18.28 ± 8.10 min was significantly longer than the mean actual response time of 14.44 ± 4.86 min (p < 0.001). The positive correlation between the perceived and actual times was low but statistically significant (p < 0.001) with a correlation coefficient of 0.315 (95% CI 0.170– 0.446). The overall satisfaction level was high (, standard deviation 0.63). The mean perceived EMS response time compares with the high-to-highest satisfaction levels of relatives was significantly lower than the mean perceived EMS response time compares with the lowest-to-middle satisfaction levels of relatives (17.83 ± 8.05 and 22.50 ± 7.47 min, respectively; p = 0.028).
Conclusion: The perceived EMS response time was longer than the actual response time, with a low correlation. However, the relatives’ overall satisfaction level was high.
Keywords: emergency ambulance, satisfaction level, perception, response times
Introduction
The duration of waiting times in public healthcare are important for health services and improving them should be considered as part of improving the public health system.1 Waiting times also play a role in both patients’ and relatives’ satisfaction with public health services.2 Healthcare institutes responsible for emergency medical services (EMS) have indicated that response times constitute a standard index of EMS performance measures and should be routinely evaluated.3 The satisfaction of patients and their relatives is an essential element in improving EMS. EMS operating times are primarily thought of when considering prompt responses to life-threatening emergencies, but we suggest that they also indirectly affect the feelings and satisfaction of patients and their relatives for non-time critical emergencies. Previous studies of emergency departments demonstrated that 41% of patients expressed high satisfaction levels regarding wait times, with a mean expected waiting time of 94.85 min, while the actual waiting time was 78 min.2 For the previous study in emergency department, Netherland, three factors affecting waiting in emergency department, including information before treatment, pain and perception of severity level, were problem associated with perceived waiting time at the emergency department.4
Surveyed patients and relatives were unable to accurately estimate the actual waiting times in emergency departments. Although less than one-fourth of the respondents estimated waiting times longer than the actual times, almost half estimated the time as too long.5 Only a few prehospital studies focused on wait times and patient satisfaction,6,7 probably due to the numerous limitations of EMS, especially when life-threatening emergencies are involved. One previous study indicated that the estimated response times were longer than the actual times. And the study revealed the estimated time on scene and the time to definitive care were shorter than the actual times.8 Eisen et al hypothesized that stressful situations decrease the perception of time for emergency medical operation units. Emergency medical responders usually perceived the response time as slower than the actual time. However, the estimated time may be perceived differently for each individual, depending on the amount of caffeine, emotional state, personality, experience with medical emergencies, clinical factors related to the emergency, and experience asking for help in stressful situations. Psychology can distort the perception of ambulance response times.9 Improving EMS effectiveness requires accelerating the emergency response, including screening emergency life-threatening situations and improving the abilities and capacity of emergency medical dispatchers and dispatch centers.10
The present study aimed to compare the perceived EMS response times to the actual EMS response times and evaluate the perception and satisfaction level of relatives regarding wait times. The result of the present study can be used to improve service quality regarding response times, relatives’ perception of ambulance wait times, and service quality assurance to maximize patients’ and relatives’ satisfaction with ambulance wait times.
Materials and Methods
Study Design and Setting
For this cross-sectional study, data was collected from May 1 to July 31, 2021. The study sample consisted of relatives of EMS patients treated by the Bangkok EMS Dispatch Center (Erawan Center) and the Surgico Medical Ambulance and Rescue Team (S.M.A.R.T.), Division of Emergency Medical Service and Disaster, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Thailand. S.M.A.R.T is the zone 1 leader (from a total of 9) for Erawan Center, Bangkok, and receives calls and dispatches operation units for zone leaders in the responsible areas of Bangkok. The Thailand emergency medical triage protocols use code for patients’ classification and prioritization and ambulance provision in emergency responses. S.M.A.R.T is responsible for around 50 square kilometers, including 6 public and private hospitals and more than 500,000 people. The operation team from S.M.A.R.T. includes paramedics, emergency medical technicians, emergency nurse practitioners, and emergency physicians. However, the night shift includes only paramedics and EMTs under an online medical director. EMS is provided free of charge in Thailand and consists of advanced, intermediate, basic, and first responder teams. Vans and motorcycles are employed as EMS vehicles.
Eligibility Criteria
Inclusion criteria were relatives of the EMS patients aged >18 years serviced by either Bangkok EMS Dispatch Center (Erawan Center) and S.M.A.R.T. Division of Emergency Medical Service and Disaster, Faculty of Medicine Vajira Hospital, Navamindradhiraj University. The team leader evaluated the scene to ensure that interviewing relatives did not interfere with the on-site emergency procedures. During the interview, the relatives’ readiness to help and the lack of a family crisis, such as losing a family member, were determined. The exclusion criteria were non-cooperation and incomplete data.
Sample Size Determination
Target population in the study were the relatives of patients serviced by EMS of S.M.A.R.T. unit. The study period was during 1 May - 31 July 2021. The primary objective was a comparison between perceived EMS response times and actual EMS response times. The sample size was estimated using the mean estimation11 and standard deviation (SD) as described by Harvey et al,8 who reported mean perceived and actual EMS response times of 12.36 and 9.12 min, respectively. Satthing et al reported a SD of 7.187.12 We calculated an initial sample size of at least 130. To compensate for non-responders, we added 20% to the sample size, according to the formula13 “nnew = 130/(1−0.2),” resulting in a new sample size of 162.5. Therefore, the final sample size was set at 165.
Operational Definitions
The perceived EMS response time was defined as the time elapsed from the emergency call to the EMS arrival on the scene, as estimated by the relatives. The actual response time was the time elapsed from the team’s activation to arrival on the scene. The response code was derived from the team’s confirmation of the patients’ symptoms at the scene. The relatives were defined as the patient’s next of kin. The relatives’ satisfaction regarding the waiting time was measured using the 5-point Likert scale (mean scores of 4.50–5.00, 3.50–4.49, 2.50–3.49, 1.50–2.49, and 1.00–1.49 indicated highest, high, medium, low, and lowest satisfaction, respectively).14
Data Collection Tools, Procedures, and Quality Control
The questionnaire included 3 sections: 1) the S.M.A.R.T./emergency ambulance data, which was recorded by the paramedic team leader and included the response time and response code; 2) the personal data of the patient’s relatives, including gender, age, ambulance service history, relationship, and perceived waiting time; and 3) five questions concerning satisfaction with the wait time using a closed questionnaire with a Likert rating scale (1–5, where 5 represented the highest and 1 represented the lowest satisfaction14) that allowed for only one answer. The questionnaire was examined using a content validity index15 by three emergency physicians who were also emergency medical directors. The validity index was 1 for all questionnaires. The third section was validated and tested by 30 relatives of patients treated by S.M.A.R.T., Division of Emergency Medical Service and Disaster, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Thailand, one month before the actual data collection. The reliability index, which was assessed using Cronbach’s alpha, was 0.875 (high). The questionnaire is shown in Table S1.
Data Processing and Analysis
Statistical analyses were conducted using IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA). Means and SD describe the parametric and non-parametric continuous data, and numbers and percentages describe the categorical data. Differences were analyzed using Student’s t-test or the Mann–Whitney U-test. To analyze the relationship, we employed either Pearson’s correlation coefficient or Spearman correlation. The correlation was analyzed via a Bland-Altman analysis and reported with a limit of agreement and a 95% confidence interval. A p-value of less than 0.05 was considered statistically significant.
Ethics Approval and Consent to Participate
This study was approved by the Institutional Review Board of the Faculty of Medicine Vajira Hospital, Navamindradhiraj University (COA. No. 063/2564). Candidates unwilling to participate in the survey were excluded. Research assistants obtained written informed consent from patients’ relatives. If relatives were unpleasant or unwilling to answer the questionnaires, the process was terminated immediately. To preserve patient rights, answering relatives were evaluated by the team leader of the emergency operation unit to assure that the situation was not an obstacle to performing the emergency operation and confirm relatives’ readiness to participate. This study complied with the Declaration of Helsinki.
Results
Of the 165 participants included in the analysis, 60% were female. The mean age was 47.21 ± 15.18 years, and 53.3% of the participants had an ambulance call history. Most of the participants were children of the patients (44.2%) (Table 1).
 |
Table 1 Participant Characteristics |
Perceived and Actual EMS Response Times
The mean perceived EMS response time of 18.28 ± 8.10 min was significantly longer than the mean actual response time of 14.44 ± 4.86 min, with a mean difference of 3.85 ± 8.02 min (p < 0.001) (Table 2). The agreement limit of the correlation between the perceived and actual EMS response time was −12.20–19.90 min (Figure 1). The positive correlation was low but statistically significant (p < 0.001), and the correlation coefficient was 0.315 (95% CI 0.1700.446) (Table 3 and Figure 2).
 |
Table 2 Comparison Between Mean Perceived and Actual EMS Response Times |
 |
Table 3 Correlation Between the Perceived and Actual EMS Response Times |
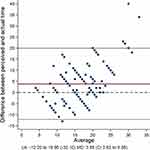 |
Figure 1 Bland-Altman plot of the difference between the perceived and actual EMS response times. Abbreviations: CI, confidence interval; EMS, emergency medical services. |
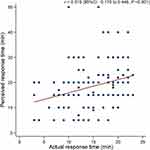 |
Figure 2 Scatter plot of the relationship between the perceived and actual emergency medical service response times. |
Relatives’ Satisfaction Level Regarding Wait Times
The overall satisfaction level was high ( , SD 0.63), and satisfaction with the level of convenience and speed was high (
, SD 0.63), and satisfaction with the level of convenience and speed was high ( , SD 0.86). Satisfaction with the initial instructions and waiting time information was high (
, SD 0.86). Satisfaction with the initial instructions and waiting time information was high ( , SD 0.92). Satisfaction with the continuous coordination from the dispatch center and ambulance was the highest (
, SD 0.92). Satisfaction with the continuous coordination from the dispatch center and ambulance was the highest ( , SD 0.79). Satisfaction with the appropriateness of the evaluation for providing urgent ambulance service was high (
, SD 0.79). Satisfaction with the appropriateness of the evaluation for providing urgent ambulance service was high ( , SD 0.85). The feeling of neglect was the lowest (
, SD 0.85). The feeling of neglect was the lowest ( , SD 0.92) (Table 4).
, SD 0.92) (Table 4).
 |
Table 4 Relatives’ Satisfaction Regarding Waiting Times |
Perceived EMS Response Time and Satisfaction Level
The mean actual EMS response time compares with the high-to-highest satisfaction levels of relatives was not significant as same as the mean actual EMS response time compare with the lowest-to-middle satisfaction levels of relatives (14.42 ± 4.89 and 14.63 ± 4.73 min, respectively; p = 0.871). The mean perceived EMS response time compares with the high-to-highest satisfaction levels of relatives was significantly lower than the mean perceived EMS response time compares with the lowest-to-middle satisfaction levels of relatives (17.83 ± 8.05 and 22.50 ± 7.47 min, respectively; p = 0.028). The mean differences in the actual response times and the perceived response times compare with the high-to-highest satisfaction levels of relatives were significantly lower than the mean differences in the actual response times and the perceived response times compare with the lowest-to-middle satisfaction levels of relatives (3.42 ± 7.96 and 7.88 ± 7.68 min, respectively; p = 0.034) (Table 5).
 |
Table 5 Comparison Between the Mean Perceived EMS Response Time and Satisfaction Level |
Discussion
In this study, the perceived EMS response times were longer than the actual EMS response times. The mean perceived emergency ambulance response time and mean actual response times were comparable to those of a previous study.8 Estimated response times of patients were usually longer than the actual response times.16 This discrepancy in actual and perceived response times may be due to the retrospective estimation of time elapsed from the first emergency call to EMS arrival, combined with the increased anxiety while waiting for EMS. The further research is needed to explore the reasons behind this discrepancy; however, research from psychology suggests increased anxiety may be a reason etc.
Shorter response times are significantly related to increased survival rates for victims of traffic accidents,17 and longer response times logically lead to significantly higher mortality rates.18 Our latest study found that response times of less than 8 minutes were associated with success in on scene prehospital cardiopulmonary resuscitation,19 which conflicted with a previous study by Blackwell et al that reported no relationship between response times and death or critical procedural interventions.20
A study on emergency departments found that 41% of patients had high levels of satisfaction regarding wait times, which was consistent with our study.2 The overall satisfaction level in our study was high ( , SD 0.63), possibly because the EMS team leaders asked relatives for their address and medical history and periodically contacted them to report the ambulance’s location. This action was regularly done in our area, not only in the study. The future challenge is to continue to improve the overall satisfaction as much as possible. A previous study demonstrated the association of emotional perception, experience, and satisfaction of patients, relatives, and families with distorted perception during medical emergencies.9 The authors propose that future research should focus on the relationship between patients’ and relatives’ experiences and satisfaction with ambulance calls and the perception of ambulance response times. These results can guide strategic EMS improvements to maximize patient and relative benefits and satisfaction leading to improved perception of actual response times.
, SD 0.63), possibly because the EMS team leaders asked relatives for their address and medical history and periodically contacted them to report the ambulance’s location. This action was regularly done in our area, not only in the study. The future challenge is to continue to improve the overall satisfaction as much as possible. A previous study demonstrated the association of emotional perception, experience, and satisfaction of patients, relatives, and families with distorted perception during medical emergencies.9 The authors propose that future research should focus on the relationship between patients’ and relatives’ experiences and satisfaction with ambulance calls and the perception of ambulance response times. These results can guide strategic EMS improvements to maximize patient and relative benefits and satisfaction leading to improved perception of actual response times.
Study Strengths and Limitations
The strength of this study is the use of this information to improve service quality, including response times and relatives’ feelings about waiting for the ambulance, and maximize patient and relative satisfaction. Our study had several limitations. First, although the patients should have been the study participants, this was not possible in the context of EMS. Patients are in critical and life-threatening conditions and cannot provide essential information for the questionnaire. Due to ethical issue, thus, data were collected from relatives. Moreover, most individuals who make emergency calls are relatives of the patients or bystanders. Second, this was a single-centered study. Therefore, the findings cannot be generalized. A future multicenter study is needed. Third, the third wave of the COVID-19 pandemic contributed to EMS operational delays. Shortages in healthcare personnel and emergency ambulances developed due to the number of COVID-19 patients and the time spent preparing the team, donning personal protective equipment, and interviewing the patients’ relatives regarding the COVID-19 contact history. The EMS teams should be prepared for emergencies in the COVID-19 pandemic, and the findings of this study could be applied to improve the monitoring and coordination with relatives for more successful outcomes. Relatives should not be neglected and conflicts between relatives and emergency department staff should be avoided to improve EMS. Fourth, In the present study, the data from questionnaire was collected by a research assistant which might lead to a lot of biases to relatives’ questionnaire answering, they might be afraid of an EMS staff or a research assistant. The last important limitation was that none of the patients’ relatives looked at watches. Every relative estimated the time. Therefore, unsurprisingly, the relatives’ perceived ambulance response time poorly correlated with the actual ambulance response time.
Conclusion
The perceived EMS response times were longer than the actual times, with a low correlation. However, the relatives’ overall satisfaction level was high.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
The present study was supported by the Navamindradhiraj University Research Fund for publishing costs. The authors are grateful to the paramedics, Surgico Medical Ambulance and Rescue Team (S.M.A.R.T.), the Division of Emergency Medical Service and Disaster, Faculty of Medicine Vajira Hospital, Navamindradhiraj University for the data collection. The authors would also like to thank Chunlanee Sangketchon MD, Chief of the Department of Disaster and Emergency Medical Operation, Faculty of Science and Health Technology, Navamindradhiraj University for assisting and facilitating the research and Aniwat Berpan MD. for acting as an English consultant for this study.
Author Contributions
All authors made a significant contribution to the study conception, design, execution, acquisition of data, analysis or interpretation of data, or in all these areas. All authors took part in drafting, revising, or critically reviewing the article. All authors gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
The research was funded by Navamindradhiraj University.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bursch B, Beezy J, Shaw R. Emergency department satisfaction: what matters most? Ann Emerg Med. 1993;22:586–591. doi:10.1016/S0196-0644(05)81947-X
2. Spechbach H, Rochat J, Gaspoz JM, Lovis C, Ehrler F. Patients’ time perception in the waiting room of an ambulatory emergency unit: a cross-sectional study. BMC Emerg Med. 2019;41:1–10.
3. Cabral ELS, Castro WRS, Florentino DRM, et al. Response time in the emergency services systematic review. Acta Cir Bras. 2008;33:1110–1121.
4. Bos N, van Stel H, Schrijvers A, Sturms L. Waiting in the accident and emergency department: exploring problematic experiences. South Med J. 2015;108:613–620. doi:10.14423/SMJ.0000000000000350
5. Thompson DA, Yarnold PR, Adams SL, Spacone AB. How accurate are waiting time perception of patients in the emergency department? Ann Emerg Med. 1996;28:652–656. doi:10.1016/S0196-0644(96)70089-6
6. Jaklič TK, Kovač J, Maletič M, Bunc KT. Analysis of patient satisfaction with emergency medical services. Open Med. 2018;13:493–502. doi:10.1515/med-2018-0073
7. Suriyawongpaisal P, Tansirisithikul R, Srithamrongsawat S. An assessment on Thai emergency medical services performance: the patient perspective. J Med Assoc Thai. 2012;95:111–118.
8. Harvey AL, Gerard WC, Rice GF, Finch H. Actual vs perceived ems response time. Prehosp Emerg Care. 2009;3:11–14. doi:10.1080/10903129908958898
9. Eisen LA. Time perception is distorted during responses to medical emergencies. Med Hypotheses. 2009;72:626–628. doi:10.1016/j.mehy.2009.01.007
10. Shah CH, Ismail IM, Mohsin SS. Ambulance response time and emergency medical dispatcher program: a study in Kelantan, Malaysia. Southeast Asian J Trop Med Public Health. 2008;39:1150–1154.
11. Daniel WW, Wayne WD. Biostatistics: a Foundation for Analysis in the Health Sciences. Wiley; 1987: 5.
12. Satthing P, Penpoint P, Phakrob N. Emergency operation timing of emergency operation unit at Jainad Narendra hospital [internet]; 2017 [
13. Pitisuttithum P, Picheansunthorn C. Textbook of Clinical Research.
14. Best JW, Kahn JV. Research in Education.
15. Polit DF, Beck CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health. 2006;29:489–497. doi:10.1002/nur.20147
16. Sultan M, Abebe Y, Tsadik AW, Ababa A, Yesus AG, Mould-Millman NK. Trends and barriers of emergency medical service use in Addis Ababa; Ethiopia. BMC Emerg Med. 2019;19:28. doi:10.1186/s12873-019-0242-5
17. Mahama MN, Kenu E, Bandoh DA, Zakariah AN. Emergency response time and pre-hospital trauma survival rate of the national ambulance service, Greater Accra (January - December 2014). BMC Emerg Med. 2018;18:33. doi:10.1186/s12873-018-0184-3
18. Blackwell TH, Kaufman JS. Response time effectiveness: comparison of response time and survival in an urban emergency medical services system. Acad Emerg Med. 2002;9:288–295. doi:10.1197/aemj.9.4.288
19. Huabbangyang T, Soion T, Promdee A, et al. Factors associated with successful resuscitation during out-of-hospital cardiac arrest performed by Surgico Medical Ambulance and Rescue Team (S.M.A.R.T), division of emergency medical service and disaster, Faculty of Medicine Vajira Hospital, Navamindrad. J Med Assoc Thai. 2021;104:1488–1496.
20. Blackwell TH, Kline JA, Willis JJ, Hicks GM. Lack of association between prehospital response times and patient outcomes. Prehosp Emerg Care. 2009;13:444–450. doi:10.1080/10903120902935363
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
