Back to Journals » Infection and Drug Resistance » Volume 16
Pediatric Gastrointestinal Basidiobolomycosis: A Retrospective Study from Jazan Province, Saudi Arabia
Authors Ghazwani SM, Arishi HM, Dhayhi NS, Shami MO , Gosadi IM, Rajab M, Badedi M , Mobarki M, Alhazmi AH
Received 1 May 2023
Accepted for publication 11 July 2023
Published 18 July 2023 Volume 2023:16 Pages 4667—4676
DOI https://doi.org/10.2147/IDR.S416213
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Salman M Ghazwani,1,2 Haidar M Arishi,3 Nabil S Dhayhi,3 Mohammed O Shami,4 Ibrahim M Gosadi,5 Moutaz Rajab,2,6 Mohammed Badedi,7 Mousa Mobarki,8 Abdulaziz H Alhazmi9
1Department of Surgery, Faculty of Medicine, Jazan University, Jazan, 45142, Saudi Arabia; 2Department of Pediatric Surgery, King Fahad Central Hospital, Jazan, 82666, Saudi Arabia; 3Pediatric Infectious Diseases Unit, King Fahad Central Hospital, Jazan, 82666, Saudi Arabia; 4Faculty of Medicine, Jazan University, Jazan, 45142, Saudi Arabia; 5Department of Family and Community Medicine, Faculty of Medicine, Jazan University, Jazan, 45142, Saudi Arabia; 6Department of General Surgery, Pediatric Surgery Unit, Faculty of Medicine, Cairo University, Cairo, 4240310, Egypt; 7Administration of Research and Studies, Jazan Health Affairs, Jazan, 82611, Saudi Arabia; 8Department of Pathology, Faculty of Medicine, Jazan University, Jazan, 45142, Saudi Arabia; 9Department of Microbiology and Parasitology, Faculty of Medicine, Jazan University, Jazan, 45142, Saudi Arabia
Correspondence: Abdulaziz H Alhazmi, Department of Microbiology and Parasitology, Faculty of Medicine, Jazan University, Jazan, 45142, Saudi Arabia, Tel +966-7-3295000, Email [email protected]
Introduction: Basidiobolomycosis is a rare fungal infection caused by Basidiobolus ranarum, and its incidence is poorly understood due to its rarity. Gastrointestinal Basidiobolomycosis (GIB) is an uncommon presentation with limited reports in Saudi Arabia. This retrospective study aims to describe risk factors, clinical findings, diagnosis, and management of GIB in the pediatric population.
Methods: We conducted a retrospective analysis of all pediatric patients diagnosed with GIB at a tertiary hospital between 2010 and 2022. Patients were identified based on their diagnosis of GIB. A self-administered questionnaire was distributed to assess risk factors associated with GIB.
Results: We analyzed 25 cases of pediatric GIB, with approximately half of the cases (56%) occurring during the COVID-19 pandemic. The mean age of affected patients was 6.6 years, with a male predominance (60%, n=15). About 100% of parents acknowledged gecko existence in their residence, and their children were exposed to insect bites. Poor appetite was reported in all patients, and high counts of eosinophils and erythrocyte sedimentation rate were observed. Thrombocytosis was present in approximately 90% of patients, and 87% had anemia. Abdominal computerized tomography scans and ultrasound-guided biopsies were the most used diagnostic tools, with cases being diagnosed based on histopathological findings and confirmed via fungal culture.
Conclusion: Our study provides valuable information on the potential risk factors, clinical features, diagnosis, and management of pediatric GIB in the Jazan region. The observed increase in cases during the COVID-19 pandemic highlights the need for continued surveillance and research to understand better the epidemiology and associated risk factors with this rare fungal infection. These findings emphasize the need for heightened awareness, early detection, and effective prevention strategies to mitigate the impact of pediatric GIB.
Keywords: gastrointestinal basidiobolomycosis, fungal infection, abdominal mass, voriconazole, Jazan, Saudi Arabia
Introduction
Gastrointestinal Basidiobolomycosis (GIB) is an infection caused by Basidiobolus ranarum, which is environmental saprophytic fungi found worldwide in soil, decaying organic matter, and the gastrointestinal tracts of amphibians, fish, reptiles, and insectivorous bats.1 This fungus belongs to the order Entomophthorales of the class Zygomycetes. Basidiobolomycosis, characterized by chronic subcutaneous induration affecting the limbs, trunk, and buttocks, is found mainly in the tropical areas of South America, Africa, and Asia.2,3 There is a dearth of reports about Basidiobolomycosis epidemiology in our region, and, like other fungal infections, cases spiked during the COVID-19 pandemic.4–8
Minor trauma, local inoculation, and insect bites appear to be the predominant modes of transmission; however, it is rare for Basidiobolus spp. to be found in the human gut.4,5 Thus, GIB seems to be transmitted through ingesting food contaminated with excreta from frogs, lizards, decayed animals, or plants.4 The first presumed case of pediatric GIB was reported in 1964 in a six-year-old Nigerian boy. Since then, especially in the past three decades, well-documented cases have been reported from different regions around the globe.5–9 The clinical outcome of pediatric GIB depends on the severity of the disease, the degree of surrounding tissue involvement, and the presence of complications at the time of diagnosis.5 The GIB is often challenging to identify, and clinical diagnosis is usually not evident as it could go underdiagnosed or misdiagnosed with cancers or other diseases such as Crohn’s.7,8
The diagnosis of GIB in pediatric patients with abdominal masses needs a high index of suspicion, and specific protocols should be adapted for accurate diagnosis and better management of such cases. In this retrospective study, we aimed to describe our experience with diagnosing GIB pediatric cases and report risk factors, clinical presentations, and management in the Jazan region. Further, we aimed to discuss the effects of the COVID-19 pandemic on the epidemiology of GIB.
Materials and Methodology
Study Design and Participants
This observational retrospective study analyzed data of pediatric patients diagnosed and treated for GIB at a tertiary healthcare referral center in the Jazan region. The relevant clinical data were extracted from the hospital’s electronic medical records specifically the reviewed medical records of the patients between March 2010 and March 2022. The study population included all patients in the pediatric age group of 1 to 14 years of age that were presented to our center with the diagnosis of GIB during the specified study period. Patients younger than one year and older than 14 years were excluded. The effects of the COVID-19 pandemic on the epidemiology of GIB were also examined in this study as data were analyzed to determine the incidence of GIB before and during the COVID-19 pandemic. Further, a questionnaire that included questions about the risk factors of GIB was distributed to the patients’ guardians. The answers were collected using an online form to ease the data collection.
Data Collection Sheet
Data collection sheets and questionnaires were developed to facilitate clinical data extraction and risk factor assessment. The data collection sheet and the questionnaire were created by a panel of consultants in pediatric surgery, infectious disease, pathology, and microbiology to ensure a comprehensive clinical assessment of the diagnosed cases. The panel of consultants reviewed medical literature to determine extracted data and risk factors to be assessed. The extracted data were related to the patient’s age at the time of admission, gender, geographic information, and clinical history before admission. The initial clinical presentations and clinical examinations were documented. Reports of histopathological, radiological, and laboratory tests, including microbiology, were collected. Surgical interventions and management were likewise obtained from the files. In addition, the patients’ follow-ups were also evaluated regarding the fungal infection localization, and the duration of medical management for each patient were recorded. The questionnaire included the guardian’s demographic data, such as sex, education, family income, and whether the patients lived in a village, mountainous area, or city. Risk factors were assessed by asking the patients’ guardians direct yes-or-no questions.
Data Analysis
Data cleaning and coding were done using Microsoft Excel software. Data analysis used frequencies and proportions to summarize the study’s findings. Frequencies and ratios of each symptom, sign, or laboratory finding were utilized to investigate the most common clinical presentation among the diagnosed cases.
Ethical Consideration
The study was conducted per the ethical standards of the local ethical committee and approved by the Jazan Health Ethics Committee (approval number 2160, dated 18th of August 2021). This study relied on routinely collected clinical data and self-reported data from relevant patients or guardians. The study was conducted following the ethical guidelines of the Helsinki Declaration and the local guidelines of the National Committee of Bioethics in Saudi Arabia.
Results
From all the examined files, 25 patients met the inclusion criteria. The mean age of diagnosed patients was 6.6 years. Most of the patients were male, with a 60% proportion (n=15). Most patients (n=11, 44%) came from the Al-Ardhah Governate in Tihamah coastal plain (Figure 1).
 |
Figure 1 Distribution of GIB cases by governance in Jazan, Saudi Arabia. |
Table 1 presents the distribution of demographic variables among the participants enrolled in the study. Regarding education, all patients’ guardians (100%, n=25) had less than a university education. When considering the participants’ family monthly income in Saudi Riyal, 76% (n=19) reported earning less than 5000 Riyal, while 24% (n=6) reported an income between 5000 and 10,000 Riyal. Regarding residency, most participants (92%, n=23) lived in village and mountain areas, while only 8% (n=2) resided in urban areas.
 |
Table 1 Demographic Variables, Clinical Presentations and Laboratory Findings of Children Diagnosed with Gastrointestinal Basidiobolomycosis in the Jazan Region, Saudi Arabia Between 2010 and 2022 |
The distribution of the most identified clinical presentation of the diagnosed cases is summarized in Table 1. The most identified symptoms were poor, or loss of, appetite, abdominal tenderness, abdominal masses, weight loss, and abdominal pain.
Table 2 presents the risk factors identified by directly questioning patients’ guardians. About 44% (n=11) reported that their children played in swamps, and 24% (n=6) of participants said having noticed their child eating dirt or other inedible materials. Regarding livestock at home, 80% (n=20) of respondents confirmed raising livestock, and 84% (n=21) of participants reported their children being exposed to or walking among organic compost piles. Regarding walking barefoot among organic manure, 84% (n=21) of respondents answered affirmatively, and 100% of the participants reported the presence of geckos in their place of residence or where their children frequently play. About 80% (n=20) of respondents reported the presence of frogs, and 48% (n=12) of participants reported the presence of bats. A vast majority, 96% (n=24), confirmed the abundance of amphibians and reptiles, and all participants reported that their children were exposed to insect bites on the skin or face.
 |
Table 2 Risk Factors That Associated with Pediatric GIB as Reported by Patients’ Guardians |
Regarding the blood investigations, all patients had an elevated eosinophilic count, and high erythrocyte sedimentation rate (ESR), followed by thrombocytosis and anemia. The abdominal ultrasound (US) was the initial modality for most patients to investigate the abdominal mass. The investigation was then completed and assessed using the abdominal computerized tomography (CT) scan to evaluate the anatomical involvement and extension around the mass (Figure 2). The ileocecal region was the most affected part, with thickened bowel loops in around 80% of patients. For most patients, the diagnosis was confirmed by a Basidiobolus ranarum fungal culture and through histopathology via surgery, US-guided biopsy, and colonoscopy (Figures 3–5). Most surgically resected masses showed hard, ulcerating, fungating, and brown-yellow color (Figure 4). Figure 6 shows the distribution of cases during the studied period between 2010 and 2022, with the highest number of cases (n=8) during the period of the COVID-19 pandemic, ie, between 2020 and 2022.
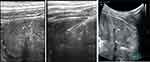 |
Figure 3 Ultrasound showing guided biopsy for histopathological study. Biopsy is taking from the mass (white arrows). |
 |
Figure 6 Cases distribution (n=25) between 2012 and 2022. |
Discussion
Basidiobolomycosis is a potentially lethal fungal infection, and patients with GIB are misdiagnosed with other illnesses, such as inflammatory bowel diseases and gastrointestinal cancer.7–10 Saudi Arabia is one of the regions that reported different case reports of GIB.5,7,8 Further, the Jazan region is no exception as it is recently experienced a surge in GIB cases in the past two years, ie, 2021 and 2022 (Figure 6). This rise in the cases indicated the importance of conducting this study to determine the epidemiology of this condition in our region in the last few years and to clarify the most appropriate approach for diagnosis and management to lower morbidity and mortality, improve recovery, and shorten hospital stays.
In this study, we assessed risk factors and retrospectively studied data related to clinical presentations, diagnosis, management, and outcome of pediatric GIB in a tertiary hospital in the Jazan region. It is noticeable that the incidence of GIB has increased during the COVID-19 pandemic, which is in line with other observations that reported a rise in fungal infection cases during the COVID-19 pandemic.6 It was suggested that patients with immunocompromised status are at a higher risk of developing fungal infections when infected with SARS-CoV-2.2 Further, the COVID-19 pandemic has negatively affected the management of invasive fungal infections in many regions around the globe.11 However, what could explain the rise in pediatric GIB cases during the COVID-19 pandemic remains unanswered. One possible explanation is the referral system of healthcare that has been ameliorated in Saudi Arabia during the pandemic, which allowed better diagnosis and documentation and faster management of such cases, compared to the period before the pandemic, where cases might stay undiagnosed or misdiagnosed.12 In this study, we could not conclude if these cases were diagnosed with COVID-19, and the effect of SARS-CoV-2 on the GIB course remained to be elucidated. However, it is known that GIB could be a fatal condition.13,14 Moreover, at the initial presentation, it could be clinically indolent, and patients may be presented with fever and abdominal pain that mimic other diseases and typically delay the diagnosis or lead to misdiagnosis.7,8 Therefore, with such a surge in the cases, a high level of suspicion is required to prevent delayed diagnosis as it is known that intra-abdominal Basidiobolomycosis complications are severe and include, but are not limited to, bowel perforations and fistula formations and consequently death.13–15
To better characterize the clinic-demographic findings of GIB, we found that most of our patients are male (60%) and live in villages or mountainous areas (92%). This finding is consistent with previous studies that have reported a male predominance in GIB cases,10 primarily due to known behavioral differences between males and females in our region. Plus, patients residing in villages or mountainous areas recorded a higher prevalence of 92%. This finding agrees with other10 and could be explained by the specific environmental conditions that favor the growth and transmission of the basidiobolus fungus. Among other reported risk factors, the presence of geckos in the participant’s place of residence or where their children frequently play was reported by 100% of the participants. Geckos have been identified as carriers of basidiobolus species,4 and their presence in proximity to children may increase the chances of exposure to the pathogen. Further, exposure to insect bites on the skin or face has been reported by 100% of the patients, as insects can serve as a mode of transmission for various pathogens, including fungi.3
Regarding the most common clinical presentations in our cohort, we found poor appetite and abdominal tenderness (100%), palpable abdominal masses (88%), weight loss (80%), and abdominal pain (76%). These findings agreed with what Shreef et al reported, in which they conducted a systematic review of all cases of pediatric GIB in Saudi Arabia and said that abdominal pain (94.4%) was the most common presentation, followed by constipation (83.3%) and abdominal mass (77.8%).15 However, unlike our finding, only 22% of cases reported fever.15 The higher portion of patients with fever (56%) in this cohort may be due to the more significant number of patients we included.
Regarding the laboratory investigations, the most common observations were elevated eosinophilic count, high ESR, thrombocytosis, and anemia. Thus, obtaining the proper history of the patient with a particular focus on the differential blood count could direct the medical team to the correct diagnosis. Eosinophils are the most evident cells in the white blood cell differential count in all GIB patients, linked to fungal-related illnesses, including broncho-pulmonary mycosis.16 In most cases, an increase in eosinophils count is expected, which cannot be explained by a history of acute or chronic immunological complaints, such as autoimmune diseases, allergies, asthma, or eczema.16 The evidence concerning elevated eosinophil levels among cases diagnosed with GIB is well established.5,7,8,10 Therefore, agreed with others, this study acknowledged that elevated eosinophil levels are present in all cases of pediatric GIB. Thrombocytosis has been found in 88% of our cases, and most of our knowledge about the roles of platelets during invasive fungal infections emerged from mucormycosis cases.17–19 However, platelet activation during GIB has not been studied, and further evaluation of its interaction with basidiobolomycosis is required.
Surgical intervention by resecting the mass was historically the preferred method of treatment.20,21 However, this treatment option is known to be associated with postoperative complications, notably anaphylactic shock, sepsis, delayed healing, and fungal dissemination.20,21 Thus, developing a high level of clinical suspicion is necessary for faster management. Since then, we have shifted from surgical to medical management to treat GIB. Further, imaging techniques such as US and CT scans helped delineate the origin of the mass, the local infiltration, and present complications. Most of the included cases were reported as abdominal masses in the colon, small bowel intestine, and, less commonly, the liver. However, the definitive diagnosis for most cases followed a histopathological examination of the tissue and was confirmed by a fungal culture.22 In our laboratory, Sabouraud agar is the primary medium used to isolate suspected fungal infections, such as Basidiobolus ranarum, and the medium is incubated for three days in 25 to 30c.22
Despite the absence of guidelines for Basidiobolomycosis treatment,23–25 cases we encountered were successfully managed with voriconazole as an antifungal treatment. As reported by others (Table 3),7,8,14,23–25 our experience with this drug was satisfactory as all patients had recovered after one year of this treatment, except for one patient who had an invasive liver fungal infection that was successfully treated with prolongation of treatment for other six months. When GIB is clinically suspected and early treatment is initiated, full recovery from this illness is possible. Engaging pediatricians, pathologists, and surgeons, in this case, the discussion is recommended to obtain better clinical outcomes for pediatric GIB.
 |
Table 3 Published Case Reports About Pediatric GIB in Saudi Arabia |
This study is one of the few studies in the region about Basidiobolomycosis and comes with many limitations. It is an observational retrospective study, and this methodology has its known limitations. Moreover, despite the efforts to collect related clinical information, we could not acquire or analyze further clinical data, microbiology characterizations, or antifungal susceptibility tests. However, with several recorded cases in the current study or as previously reported (Table 3),10 Jazan region requires special attention, and increased awareness of GIB among medical professionals is mandatory. Future studies should cover other potential risk factors of GIB in the Jazan region. Furthermore, we strongly encourage conducting national studies and obtaining further measures to investigate GIB during the COVID-19 pandemic. Plus, the cost-effectiveness impact of this disease should also be studied regarding hospital stays and the duration of antifungal medications. Moreover, preventive measures for this disease should be applied in the Jazan region, especially in Alardah, as it is highly affected by this disease.
Conclusions
In this retrospective study, a surge in basidiobolomycosis cases during the COVID-19 pandemic has been reported, and this is maybe due to the effective referral system developed as a response to the COVID-19 pandemic. A robust index of suspicion of GIB is required if the patient is presented with palpable abdominal mass and eosinophilia, especially for patients at higher risk. The role of surgery in GIB cases seems limited to only establishing the diagnosis in unplanned cases and handling complications. Early diagnosis and initiation of antifungal treatment in the diagnosed cases could improve the prognosis. Health awareness programs of GIB in pediatrics are required, and further studies on the impact of the pandemic and the potential risk factors are deemed essential in highly prevalent regions, such as the Jazan region.
Data Sharing Statement
The data presented in this study are available on request from the corresponding author.
Institutional Review Board Statement
This study was conducted per the ethical standards of the local ethical committee and ethically approved by the Jazan Health Ethics Committee (approval number 2160).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
We would like to thank King Fahd Central Hospital-Jazan and all supporting medical teams for their help in facilitating this research project and the patients’ guardians for being collaborative to responded to our questions about the risk factors.
Funding
This research received no external funding.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Okafor JI, Testrake D, Mushinsky HR, Yangco BG. A Basidiobolus sp. and its association with reptiles and amphibians in southern Florida. Sabouraudia. 1984;22(1):47–51. doi:10.1080/00362178485380081
2. Bittencourt AL, Londero AT, Araujo MS, Mendonca N, Bastos JL. Occurrence of subcutaneous zygomycosis caused by Basidiobolus haptosporus in Brazil. Mycopathologia. 1979;68(2):101–104. doi:10.1007/BF00441089
3. Maiti PK, Bose R, Bandyopadhyay S, Bhattacharya S, Dey JB, Ray A. Entomophthoromycosis in South Bengal (Eastern India): a 9 years study. Indian J Pathol Microbiol. 2004;47(2):295–297.
4. Sujatha S, Sheeladevi C, Khyriem AB, Parija SC, Thappa DM. Subcutaneous zygomycosis caused by Basidiobolus ranarum: a case report. Indian J Med Microbiol. 2003;21(3):205–206. doi:10.1016/S0255-0857(21)03076-0
5. Vikram HR, Smilack JD, Leighton JA, Crowell MD, De Petris G. Emergence of gastrointestinal Basidiobolomycosis in the United States, with a review of worldwide cases. Clin Infect Dis. 2012;54(12):1685–1691. doi:10.1093/cid/cis250
6. Dam P, Cardoso MH, Mandal S, et al. Surge of mucormycosis during the COVID-19 pandemic. Travel Med Infect Dis. 2023;52:102557. doi:10.1016/j.tmaid.2023.102557
7. Almoosa Z, Alsuhaibani M, AlDandan S, Alshahrani D. Pediatric gastrointestinal basidiobolomycosis mimicking malignancy. Med Mycol Case Rep. 2017;18:31–33. doi:10.1016/j.mmcr.2017.08.002
8. AlSaleem K, Al-Mehaidib A, Banemai M, bin-Hussain I, Faqih M, Al Mehmadi A. Gastrointestinal basidiobolomycosis: mimicking Crohns disease case report and review of the literature. Ann Saudi Med. 2013;33(5):500–504. doi:10.5144/0256-4947.2013.500
9. Edington GM. Phycomycosis in Ibadan, Western Nigeria: two postmortem reports. Trans R Soc Trop Med Hyg. 1964;58(3):242–245. doi:10.1016/0035-9203(64)90036-7
10. Al Haq AM, Rasheedi A, FarsiM A, et al. Gastrointestinal basidiobolomycosis in pediatric patients: a diagnostic dilemma and management challenge. Int J Pediatr Adolesc Med. 2021;8(4):212–220. doi:10.1016/j.ijpam.2020.05.003
11. Ibe C, Gonzalez A. The impact of COVID-19 pandemic on invasive fungal infections in Africa: what have we learned? PLoS Negl Trop Dis. 2022;16(8):e0010720. doi:10.1371/journal.pntd.0010720
12. Alabbasi KH, Kruger E, Tennant M. Strengthening Saudi Arabia’s primary health care through an e-referral system: a case study. Clin Pract. 2022;12(3):374–382. doi:10.3390/clinpract12030042
13. El-Shabrawi MH, Kamal NM. Gastrointestinal Basidiobolomycosis in children: an overlooked emerging infection? J Med Microbiol. 2011;60(Pt 7):871–880. doi:10.1099/jmm.0.028670-0
14. Al Asmi MM, Faqeehi HY, Alshahrani DA, et al. A case of pediatric gastrointestinal basidiobolomycosis mimicking Crohn’s disease, A review of pediatric literature. Saudi Med J. 2013;34(10):1068–1072.
15. Shreef K, Saleem M, Saeedd MA, Eissa M. Gastrointestinal basidiobolomycosis: an emerging, and a confusing, disease in children (a multicenter experience). Eur J Pediatr Surg. 2018;28(2):194–199. doi:10.1055/s-0037-1598104
16. Figueiredo RT, Neves JS. Eosinophils in fungal diseases: an overview. J Leukoc Biol. 2018;104(1):49–60. doi:10.1002/JLB.4MR1117-473R
17. Mohammadi R, Chaharsoghi MA, Khorvash F, et al. An unusual case of gastrointestinal Basidiobolomycosis mimicking colon cancer; literature and review. J Mycol Med. 2019;29(1):75–79. doi:10.1016/j.mycmed.2018.11.004
18. Speth C, Rambach G, Lass-Flörl C. Platelet immunology in fungal infections. Thromb Haemost. 2014;112(4):632–639. doi:10.1160/TH14-01-0074
19. García-Carnero LC, Mora-Montes HM. Mucormycosis and COVID-19-associated mucormycosis: insights of a deadly but neglected mycosis. J Fungi. 2022;8(5):445. doi:10.3390/jof8050445
20. El-Shabrawi MH, Kamal NM, Jouini R, Al-Harbi A, Voigt K, Al-Malki T. Gastrointestinal Basidiobolomycosis: an emerging fungal infection causing bowel perforation in a child. J Med Microbiol. 2011;60(Pt 9):1395–1402. doi:10.1099/jmm.0.031575-0
21. Zavasky D, Samowitz W, Loftus T, Segal H, Carroll K. Gastrointestinal zygomycotic infection caused by Basidiobolus ranarum: case report and review. Clin Infect Dis. 1999;28(5):1244–1248. doi:10.1086/514781
22. Zabolinejad N, Naseri A, Davoudi Y, Joudi M, Aelami MH. Colonic Basidiobolomycosis in a child: report of a culture-proven case. Int J Infect Dis. 2014;22:41–43. doi:10.1016/j.ijid.2013.11.016
23. Al-Hatmi AMS, Balkhair A, Al-Busaidi I, et al. Gastrointestinal Basidiobolomycosis in Oman: a series of seven cases. Med Mycol Case Rep. 2019;24:38–41. doi:10.1016/j.mmcr.2019.01.004
24. Abduh MS, Aldaqal SM, Almaghrabi J, Aljiffry MM, Elbadrawy HA, Alsahafi MA. A very rare basidiobolomycosis case presented with cecal perforation and concomitant hepatic involvement in an elderly male patient: a case study. Int J Environ Res Public Health. 2022;19(6):3412. doi:10.3390/ijerph19063412
25. Albaradi BA, Babiker AMI, Al-Qahtani HS. Successful treatment of gastrointestinal basidiobolomycosis with voriconazole without surgical intervention. J Trop Pediatr. 2014;60(6):476–479. doi:10.1093/tropej/fmu047
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



