Back to Journals » International Journal of General Medicine » Volume 16
Patterns of Medical Admissions and Predictors of Mortality in Ayder Comprehensive Specialized Hospital, Northern Ethiopia: A Prospective Observational Study
Authors Hailu A , Gidey K , Ebrahim MM , Berhane Y, Gebrehawaria T , Hailemariam T, Negash A, Mesele H , Desta T, Tsegay H, Alemayohu MA , Bayray A
Received 4 November 2022
Accepted for publication 9 January 2023
Published 21 January 2023 Volume 2023:16 Pages 243—257
DOI https://doi.org/10.2147/IJGM.S385578
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Abraha Hailu,1 Kibreab Gidey,1 Mohamedawel Mohamedniguss Ebrahim,2 Yonas Berhane,1 Teklay Gebrehawaria,1 Tesfay Hailemariam,1 Atakelti Negash,1 Habtamu Mesele,1 Tekleab Desta,1 Haylsh Tsegay,1 Mulubirhan Assefa Alemayohu,3 Alemayehu Bayray3
1Department of Internal Medicine, School of Medicine, Mekelle University - College of Health Sciences, Mekelle, Tigray, Ethiopia; 2Department of Biostatistics, School of Public Health, Mekelle University - College of Health Sciences, Mekelle, Tigray, Ethiopia; 3Department of Epidemiology, School of Public Health, Mekelle University - College of Health Sciences, Mekelle, Tigray, Ethiopia
Correspondence: Abraha Hailu Weldegerima, Department of Internal Medicine, Cardiology Unit, Mekelle University College of Health Sciences, Mekelle, Tigray, Ethiopia, Tel +251-91-141-3363, Email [email protected]
Background: Previous works show that noncommunicable diseases (NCDs) are on the rise in developing nations, including Ethiopia, in the background of preexisting communicable diseases (CDs). Data on hospital admission in sub-Saharan Africa are scarce, particularly prospectively collected, and hence this study was done to close the gap in acquiring accurate diagnosis usually faced with retrospective data. We aimed to describe medical admission patterns, their outcomes and determinants at Ayder Comprehensive Specialized Hospital (ACSH) in Tigray, Ethiopia.
Methods: Data were collected prospectively from November 1, 2017 to October 31, 2018 for all medical admissions. Sociodemographic profiles, final diagnosis, outcome of hospitalization, and complications were recorded using a data-abstraction checklist. Data were analyzed using SPSS 26.
Results: There were 2084 medical admissions over 1 year. Median age was 45 years (IQR 31). A majority (1107, 53.1%) were male. The age-group 25– 34 years had the most admissions (19.0%). NCDs constituted 68.2% of admissions. According to the International Classification of Diseases, patients were admitted most frequently due to disease of the circulatory system (36.7%) followed by infectious or parasitic diseases (24.1%). Of NCDs, cardiovascular diseases contributed to 53.9%, followed by cancers (8.6%). Of CDs, HIV/AIDS contributed to 31.3%, followed by tuberculosis (22.8%). A total of 1375 (66%) were discharged improved, while 311 (14.9%) died. On multivariate analysis, the in-hospital mortality was significantly higher (18.7%) for CDs than NCDs (13.2%, AOR 1.8, 95% CI 1.4– 2.3; P< 0.001). Bed occupancy of ACSH medical wards and ICU was 54%.
Conclusion: NCDs were leading causes of medical admissions in ACSH. The presence of CDs and the development of complications were associated with higher risk of death. Attention should be given by policy-makers to curb the higher morbidity from NCDs and mortality from CDs.
Keywords: medical admissions, mortality, Ayder, Ethiopia
Introduction
The burden of diseases among adults in developing nations, particularly in sub-Saharan Africa, (SSA), including Ethiopia, is poorly documented. Some studies have shown that due to epidemiological transition, noncommunicable diseases (NCDs) are on the rise and are adding burden to the preexisting but decreasing burden of communicable diseases (CDs) in SSA.1,2 CDs are the leading causes of morbidity and mortality among medical admission facilities across Africa, while over the last few decades a trend toward NCD dominance over CDs has increasingly been documented.3,4
In SSA, NCDs, including cardiovascular diseases (CVDs), diabetes, cancer, chronic kidney disease, mental illness, and trauma, are important causes of morbidity and mortality and projected to exceed infectious diseases by 2030.5 A 2005–2007 Nigerian study that analyzed 1860 patient records revealed that hypertension, diabetes mellitus, and HIV/AIDS were the leading causes of admissions.6 A retrospective hospital study based in Eastern Sudan also revealed that of 7230 patients admitted, 56.2% were admitted with NCDs, with the main contributors of admission being CVDs (18.4%), snakebites (12.9%), and visceral leishmaniasis (12.0%).7 A 5-year retrospective study of 2011–2015 in the same setting in Tigray, Ethiopia (ACSH) on the levels and trends of mortality showed a similar trend, with NCDs being the major causes of death.8
A systematic review of African adult admissions to hospitals showed that of a total of 86,307 admissions, the leading causes were infectious and parasitic diseases (19.8%) and respiratory (16.2%) and circulatory illnesses (11.3%). These researchers pointed out that the most prevalent methodological deficiencies, present in the two-thirds of the 30 articles they analyzed, were failures to use standardized case definitions and International Classification of Diseases (ICD) guidelines for classifying illnesses, hence the difficulty in comparing the burden of diseases and their trends.9 In this study, we used the World Health Organization (WHO) ICD-10 system to categorize diseases uniformly and collected data prospectively to reduce this limitation.
The 2018 WHO country profile report on Ethiopia showed that communicable, maternal, neonatal, and nutritional diseases, NCDs, and injuries contributed to 49%, 39%, and 12% of total deaths, respectively.10 Despite these estimations, the prevalence of the major NCDs (CVDs, cancers, diabetes mellitus, and chronic obstructive pulmonary disease) are not well documented in Ethiopia. Accurate information on such prevalence, of major public-health importance, is required to provide informed health-policy decisions.11,12 The increase in NCDs and concomitant risk factors in Ethiopia, as in other SSA nations, has not been well documented, especially among adult age-groups, and prospective data on hospital admissions are scanty.13,14
The patterns of medical admission to a given institution can be used to study the morbidity and mortality of the community it serves, as these parameters are partly indicators of the health status of a given community, even though community-based studies provide an accurate picture, as they minimize bias.9 Reports from referral hospitals do not necessarily show the exact distribution of diseases of the population in a given setting, but they may assist decision-makers in terms of where to focus and intervene.14–16 Our study aimed to identify the leading causes of hospitalization and determine the contributions of CDs and NCDs, hospitalization outcomes, and their determinants.
Methods
Study Area and Setting
This study was conducted at Ayder Comprehensive Specialized Hospital (ACSH) in Mekelle University, College of Health Sciences (MU-CHS) in Mekelle, capital of Tigray region. ACSH was established in 2008 as a public hospital and gives service to about 10 million population within the catchment areas of Tigray, north Afar, and northeastern parts of Amhara region. ACSH has 500 inpatient beds, additional outpatient and emergency units, and specialty and subspecialty services. The Department of Internal Medicine has 116 inpatient beds (ICU and ward) and outpatient services within its different subspecialty units equipped for bronchoscopy, spirometry, upper and lower gastrointestinal endoscopy, electroencephalography, echocardiography (ECG), Holter blood pressure, and ECG monitors, resting and stress ECG machines, and a cardiac catheterization laboratory. ACSH is involved in teaching both undergraduate medical and allied health professionals and postgraduate students.
Study Design and Data Collection
This was a prospective study conducted on all patients admitted to internal medicine wards and the ICU at ASCH from November 1, 2017 till October 31, 2018. All adult medical ward admissions were aged >18 years. A structured questionnaire was developed and enriched by reviewing previous literature to capture data. The data collectors were trained medical residents who were also part of the patient care-taking team and were supervised by senior consultant physicians (the investigators and other physicians). All patients were followed with continuous medical examinations and laboratory testing until final diagnosis was settled. Each ward and ICU nurses also helped in the follow-up of each case until discharge, making sure all patients and events were recorded. The final diagnosis was settled by ward attending physicians, comments from morning/grand round sessions, and interdepartmental and subspecialist consultations and recorded at the discharge of each patient. A patient could have more than one problem and the major reason for the patient’s current admission was taken as the final diagnosis based on the ICD-10. Disease category (CD or NCD) followed the US Centers for Disease Control and Prevention and WHO definitions.17,18
Complications of hospitalization or complications of disease progression were all recorded based on the aforementioned methods to reach the final diagnosis. For example, acute kidney injury (AKI) was diagnosed as per the Kidney Disease: Improving Global Outcomes Clinical Practice Guideline for Acute Kidney Injury criteria as an increase in serum creatinine by >0.3 mg/dL within 48 hours or increase in serum creatinine >1.5 times baseline, which is known or presumed to have occurred within the prior 7 days.19 We did not accurately follow the urine output of each and every patient, and hence these criteria were not applied. Diagnosis of aspiration pneumonia, albeit difficult, was made by history, clinical features, risk factors, and supportive findings on chest radiography.20 Generally, all other complications were diagnosed by the methods reiterated earlier, and the investigators used clinical, imaging, physiological, and biochemical parameters when appropriate. Data collected were sociodemographic characteristics, region (state), address (rural/urban), primary diagnosis, comorbidities, complications, duration of hospital stay, outcome of hospitalization (death, discharge, transferred to continue same treatment, and referred), and condition at discharge (improved, left against medical advice [LAMA], same condition).
Data Quality Control
Data quality control was done in parallel with data collection. Before discharge or at time of death, discharge diagnosis and cause of death were documented by ACSH’s medical interns and residents. These discharge and death certificates were reviewed by the study team. Once weekly, the investigation team met in the medical wards and ICU to discuss all deaths or discharges, confirm data-collection accuracy and completeness, and make necessary corrections. Residents and interns of ACSH were updated once every 4 weeks on the proper recording of the appropriate conditions in line with the WHO ICD-10 system.
Operational Definitions
Final diagnosis/cause of admission: The primary diagnosis settled on at discharge by the treating team of physicians with appropriate clinical, laboratory, and imaging means. In rare cases where reaching a final diagnosis became challenging due to a patient’s financial problems or unavailability of tests, the team’s clinical decision was noted as a cause of admission.
Comorbidity: A concurrent disease with the final diagnosis during hospitalization.
Complications
- Hospitalization complications: Hospital-acquired pneumonia (HAP), aspiration pneumonia, AKI, urinary tract infection, and others.
- Complications of disease progression: These may or may not lead to death unless treated.
Outcome of hospitalization: Patient’s condition at the end of hospitalization (death, discharge, LAMA, transferred to continue same treatment, or referred).
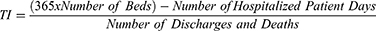
Bed occupancy rate (BOR): A measure of the usage of available hospital beds.
Bed turnover rate (BTR): Number of patients treated in a given bed in a given period.
Turnover interval (TI): Average number of days that beds in hospitals are utilized between successive patient admissions.
Data Analysis
Data were analyzed using SPSS version 26. Both descriptive and inferential statistics were used. Categorical variables were described using frequency, percentage, and graphs. Continuous variables are described using an appropriate combination of measure of central tendency and measure of dispersion. Length-of-stay difference between CDs and NCDs was compared using independent-sample t-tests. Independent predictors of death among admitted patients were identified by multivariate logistic regression. Associations between death and its predictors were reported using ORs with 95% CIs and P-values). Goodness of fit of the multivariate model was assessed using the Hosmer–Lemeshow test. Multicollinearity was assessed using the variance-inflation factor.
Ethics
Ethics clearance was obtained from the Mekelle University College of Health Sciences Institutional Review Board. This study involved review of medical charts when patients were admitted in order to attain an appropriate diagnosis. There were no physical or psychological dangers to patients. There is the potential for participants to be identified, given our access to their personal identifiers. These risks were minimized by maintaining information in separate, deidentified, password-protected files to which only the research team had access. We also obtained a waiver of consent since our study was of minimal risk and involved a huge data set. This research will not affect the rights and welfare of subjects. We also obtained a waiver of documentation of consent from the review board. There was no cost to participate in the study, nor did we provide any compensation to subjects. There may not be any direct benefit to the patients. The results of our study may help enhance our ability to develop guidelines and plan policies and strategies with respect to the prevention and control of the burden of morbidity and mortality that would in general benefit society. Our study complied with the principles of the Declaration of Helsinki.
Results
We followed a total of 2084 patient admissions. More than half (53.1%) were male. The median age was 45 years (IQR 31). The most common age-group was 25–35 years (19.0%). Patients aged 25–54 years accounted for 52.4% of the admissions. A majority (93.3%) of patients were from Tigray regional state (Table 1). According to ICD classifications, the most common categories were diseases of the circulatory system (n=767, 36.8%), infectious/parasitic diseases (n=502, 24.1%), and diseases of the respiratory system (n=125, 6.0%), followed by cancers (n=123, 5.9%). Sex distribution was significantly different across ICD categories (P<0.001, Table 2). NCDs accounted for two-thirds (68.2%) of overall medical admissions and were the dominant causes of admissions in all age-groups. The shares of NCDs continuously increased as the shares of CDs decreased in the age-group 25–34 years. The narrowest gap in the distribution of diseases was in the age-group 25–34 years (58.6% and 41.4% for NCDs and CDs, respectively). NCDs contributed to 63.3% of admissions in the youngest admissions in this study (<25 years) and this percentage increased to 86.9% in patients aged ≥75 years (Figure 1).
 |
Table 1 Sociodemographic characteristics of patients (n=2084) |
 |
Table 2 International Classification of Diseases 10 category of medical admissions (n=2084) |
 |
Figure 1 Distribution of CDs vs NCDs by age-group (n=2084). |
Among CDs, the most common reasons for admission were HIV/AIDS (31.3%) followed by tuberculosis (22.0%) (Figure 2). Among the NCDs, the most common reason for admission was CVDs (54%), followed by cancers (8.6%) and hematologic diseases (8%). (Figure 3). Among the total admissions to ACSH, CVDs were the primary reasons for admission (36.7%), followed by CDs (32%), which were led by HIV/AIDS (10%). Heart failure was the leading primary diagnosis among the CVDs, contributing to 38.6% (n=767), followed by stroke (35.5%) and venous thromboembolism (17.2%). Major underlying causes of heart failure were rheumatic heart disease (42%), ischemic heart disease (29.4%) and cardiomyopathy (19.25%).
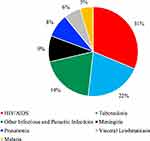 |
Figure 2 Types of CDs causing admissions (n=2084). |
 |
Figure 3 Types of NCDs causing admissions (n=2084). |
Of the total study population, the top-five specific causes of admission were heart failure (14.2%, n=2084), stroke (13.1%), HIV/AIDS (9.9%), tuberculosis (7%), and pulmonary thromboembolism/deep venous thrombosis (6.3%). The top-five specific primary diagnoses among the NCDs were heart failure (20.8%, n=1421), stroke (19.1%), venous thromboembolism (9.2%), cancers (9%), and anemia (7.8%). More than half (55.8%, n=120) the cancers were hematologic malignancies, with lymphoma contributing 43.3% (n=67). Seven patients (0.34% of total admissions) were admitted due to snakebites.
Outcome and Duration of Hospitalization
Of the total admissions, 1706 (81.9%) were discharged: 1375 (80.6%) improved and 257 (15.1%) LAMA. The overall mortality rate was 14.9% (n=311). The proportionate mortality rate for NCDs was 61.1%, whereas for CDs it was 38.9%. The mean hospital stay was 11±10 days. The mean duration of stay for those who died was 8±13 days and for those who left the hospital alive 12±9 days. A majority of patients (1278, 61.4%) stayed ≤10 days in hospital. The mean duration of stay for patients with visceral leishmaniasis was 15.4±9 days, while for those with diabetes it was 17±18 days. Patients with NCDs comprised 60.6% of those who stayed >1 month. Of patients with NCDs who stayed >1 month, CVDs numbered 20 (30.3%) while of those with CDs who stayed >1 month, HIV/AIDS cases numbered 17 (39.%, Table 3).
 |
Table 3 Length of hospital stay and outcomes (n=2084) |
In sum, 345 (16.5%) patients had complications of hospitalization, disease progression, or both. Aspiration pneumonia, hospital-acquired pneumonia, and AKI were the most prevalent complications (Table 4). Aspiration pneumonia was present in in 3% (n=63) of the total study population and in 40.1% of those with complications of hospitalization (n=157). More than half (58.7%) of the patients with aspiration pneumonia had either ischemic or hemorrhagic stroke as a risk factor, followed by pyogenic meningitis in 7.9% and epilepsy and traumatic brain injury (4.8% each). Other risk factors included tetanus (1.6%), organophosphate poisoning (3.2%), brain cancer (3.2%), and subarachnoid hemorrhage with coma (3.2%) (Figure 4). Two patients with aspiration pneumonia and epilepsy had status epilepticus. Of the five patients with pyogenic meningitis who had aspiration pneumonia, three had concomitant comorbidities and/or risk factors, with one of them being a frail 82-year-old diabetic with deep venous thrombosis and schizophrenia. The second patient had alcohol withdrawal, and the third had concomitant HIV/AIDS with esophageal candidiasis. The in-hospital mortality for patients with aspiration pneumonia was 36.5% (n=23).
 |
Table 4 Complications (n=2084) |
AKI was present in 1.2% (n=2084) of the hospitalized patients and 15.3% (n=157) of those with complications of hospitalization. The leading factors associated with AKI were sepsis and heart failure (Table 5). More than half (54%, n=13) of those who had AKI died in hospital. At least one comorbidity was found in 547 (26.5%) patients. The most frequent comorbidity was hypertension (n=311, 14.9), followed by diabetes (n=179, 8.6%) and pneumonia (n=72, 3.5%; Figure 5). Of the 311 deaths, 50 (16.1%) were due to heart failure, followed by HIV/AIDS (15.1%), stroke (11.9%), sepsis (7.4%), kidney failure (7.1%), tuberculosis (5.1%), and cancers (5.1%; Figure 6).
 |
Table 5 Factors associated with development of acute kidney injury and outcomes (n=24) |
 |
Figure 5 Comorbidities (n=2084). Notes: *Hypertensive heart disease, **Community acquired pneumonia, +Degenerative valvular heart disease. |
 |
Figure 6 Top ten causes of death (n=311). Notes: *Acute and chronic decompensated heart failures, acute coronary syndromes. **Chronic kidney disease and acute kidney injury. |
Predictors of Death
A multivariate logistic regression model composed of four variables (age-group, disease category, complication, and comorbidity) was used to identify independent predictors of death among the inpatient admissions. Disease category and complications were identified as independent predictors. The odds of death were 70% higher among patients admitted with CDs (AOR 1.6, 95% CI 1.2–2.1; P<0.001). Developing complications was also remarkably associated with higher odds of death (AOR 4.9, 95% CI 3.7–6.4; P<0.001). Among patients with CDs, those in the age-group 35–44 years had the highest number of deaths (26.7%), while the age-group 65–74 years had the most (19.9%) deaths among the NCDs. The final multivariate model was a good fit for the data (Hosmer–Lemeshow test:  27=7.8, P=0.349). There was no multicollinearity issue (maximum variance-inflation factor 1.03, Table 6). More than half (181, 58.2%) the deaths and 19 (45.2%) referrals to better setup were in the first five days. There was a significant (P<0.001) relationship between length of hospital stay and outcome of hospitalization. The median duration of hospital stay for those who died was 4 days (IQR 9), while for those who were discharged/transferred/LAMA it was 9 days (IQR 9; Table 7).
27=7.8, P=0.349). There was no multicollinearity issue (maximum variance-inflation factor 1.03, Table 6). More than half (181, 58.2%) the deaths and 19 (45.2%) referrals to better setup were in the first five days. There was a significant (P<0.001) relationship between length of hospital stay and outcome of hospitalization. The median duration of hospital stay for those who died was 4 days (IQR 9), while for those who were discharged/transferred/LAMA it was 9 days (IQR 9; Table 7).
 |
Table 6 Predictors of death (n=2084) |
 |
Table 7 Length of hospital stay vs outcome of hospitalization (n=2084) |
Hospital-Resource Utilization/Efficiency Measures (Bed Occupancy Rate, Bed Turnover Rate, and Turnover Interval)
ACSH has 500 beds, and 116 of these beds were used for internal medicine patient admissions (108 for medical ward and eight for medical ICU). The BOR of ACSH medical wards and ICU was 54%, BTR 18 patients per bed per year, and patient TI 9.3 days.
Discussion
This study shows the burgeoning burden of NCDs over CDs in hospitalized medical patients in Tigray, northern Ethiopia, as opposed to hospital data a few years ago from other parts of the nation. The leading reason for hospitalization according to the ICD-10 was CVDs. This study adds to the growing data on the ongoing epidemiological transition in developing nations and also revealed that the diagnosis of CDs and the development of complications were associated with higher risk of death. To the best of the authors’ knowledge, this is the first prospective observational study conducted using both medical ward and medical ICU admission data in Ethiopia.
Our study revealed that more than half the patients were 25–54 years old, which is the most productive breadwinning age-group in a given family. This was also seen in other studies done in Ethiopia and other sub-Saharan African countries.9,11,21,22 One of the reasons for the younger age composition is the fact that CDs are more common in that age-group, as seen in our study, and the common NCDs reported here (heart failure, stroke, and ischemic heart disease) are known to occur at a relatively younger age in sub-Saharan Africa.10,23,24 The higher contribution of rheumatic heart disease and cardiomyopathy to CVD admissions in our study explains the high proportion of young people in this study. Compared to a study conducted 23 years back at Jimma University Hospital in Ethiopia, the median age has increased significantly, from 31 years to 45 years.21,25 Also, our study has shown the proportion of people aged >75 years accounted for a 10th of all medical admissions. We saw there was a slight increment in proportions of admission for men and those coming from urban areas compared to women and rural areas, respectively.
The higher proportion of men in our study (male:female ratio of 1.13:1) has also been seen in earlier retrospective studies in the same setting in ACSH, in southwest Ethiopia at Jimma University, and in Nigeria8,25–27 This can be partly explained by the health-seeking advantage of men over women and urban residence compared to the rural population. This health-seeking advantage may emanate from the fact that men have more resources than women and are more able to pay for their health-care visits and hospital admission. This finding is contrary to the female preponderance found in a study from Addis Ababa.22 Even though a majority of patients were from Tigray regional state, ACSH has been serving patients from major neighboring regions in Ethiopia and also the neighboring country Eritrea.
This study showed that NCDs were leading causes of hospitalization. Our finding is in accordance with recent studies done in hospitalized patients in Ethiopia, Sudan, and other sub-Saharan countries.1,6,8,9,14,22,28 A study from Uganda in 2011–2014 found that a majority of patients hospitalized had NCDs similar to our finding. It was also reported that CDs (malaria, tuberculosis, and pneumonia) showed a progressive decline, while NCDs (chronic kidney disease, hypertension, stroke, and cancer) increased progressively over the 4-year study period.29 Contrary to our finding that the top specific causes of hospitalization were heart failure, stroke, HIV/AIDS, tuberculosis, and thromboembolism — 14.2%, 13.15%, 9.9%, 7% 13.1%, and 6.3%, respectively — the top specific causes of admissions in a Ugandan study were HIV/AIDS, hypertension, tuberculosis, non-TB pneumonia, and heart failure: 30%, 14%, 12%, 11%, and 9.3% respectively.29 This is also in disagreement with our finding when it comes to the top two NCD admissions, as they reported hypertension and diabetes to be the top two causes, as opposed to our finding, where heart failure and stroke were the leaders in NCD admissions. These differences could be due to differences in primary diagnosis recorded in patients with multiple comorbidities like diabetes and hypertension. Inconsistencies in classification may contribute to differences in the epidemiology of some diseases.9
The predominance of NCDs in this study was reflected in the distribution of comorbidities recorded and being dominated by hypertension and diabetes. NCDs accounted for more than two-thirds of all admissions in this study, in contrast to studies done decades back at Jimma University Hospital, which revealed infectious diseases as the main cause of hospitalization.21,25 This study has consolidated on previous reports on the changing burden and pattern of diseases due to epidemiological transition from the dominant CDs to increasing NCDs.9,30,31 Patterns of hospitalizations may not show the exact burden of diseases in a given population. However, they could be indicators of disease burden in the catchment area the hospital serves and assist in further studies and health planning.14
In this study, diseases of the circulatory system were the most common reasons for admission in this ICD-10 category. In addition, CVDs accounted for more than half of NCD cases. Similarly to our study, in a large systematic review done in sub-Saharan African countries, the proportion of admissions due to CVDs, composed mainly of stroke and heart failure, were found to have increased significantly and the proportion of admissions due to infectious and parasitic diseases decreased over the study period.13 In a recent report from eastern Sudan of 7230 patients admitted to Gadarif Hospital, CVDs constituted 18.4%, which is similar to our finding, but it is interesting to note that snakebites contributed to 12.9% in the Sudanese study (the second cause among total admissions), while only 0.34% of total admissions in our study were due to snakebites.7 The relatively high prevalence of NCDs in our study may be partly due to increased urbanization, lifestyle changes, increasing life expectancy, and referral bias, among others.32 Referral bias may contribute to the relatively higher contribution of CVD admissions to ACSH, as this flagship hospital in Tigray has been the only one equipped with advanced imaging modalities, such as CT and MRI, and a cardiac catheterization laboratory. It should be noted that the very high burden of NCDs/CVDs in our study is in line with the report of the 2018 National Commission on Noncommunicable Diseases and Injuries in Ethiopia, as well as health and demographic surveillance site reports in northern, central and southeastern parts of Ethiopia.13,33–36
HIV/AIDS and tuberculosis were found in our study to be the dominant forms of CD, as has been reported in previous studies in Ethiopia and other sub-Saharan African nations, indicating that CDs like HIV/AIDS and tuberculosis remain significant contributors to the burden on the health system of the nation.22,25 On the other hand, the proportions of malaria and relapsing fever, which were common problems in Ethiopia, were observed in our study to have decreased significantly, as reported by other studies in Ethiopia, Sudan, and Uganda, even though these were hospital-based reports that included severe cases of malaria admissions, though is important to remember that this decrement may not necessarily indicate the overall reduction of malaria in the community.21,29
The mean hospital stay in this study (11±10 days), was shorter than that in a retrospective study done in Addis Ababa, where it was >12 days, but longer than in a study done in Nigeria, where it was 10.3 days.6,22 This difference could be due to the type and severity of diseases a given institution handles, but this needs further evaluation by multicenter studies incorporating measures of health-service utilization and levels of subspecialty care, among other parameters. In our study, diabetic patients stayed longer than any other disease type. This study included patients admitted both to the medical ward and ICU. A previous study from ACSH medical ICU showed the length of stay to be 4.1 days.37 The length of stay was significantly higher in this study for CDs (11.8±10 days) than NCDs (10.7±10 days; P=0.021), as opposed to a previous study in Addis Ababa, which found similar length of hospital stay for NCDs and CDs.14 A majority of the deaths (181, 58.2%) occurred in the first 5 days of admission, and this pattern of early death was seen in other studies.25
A significant amount of patients discharged improved (more than two-thirds) while the in-hospital mortality rate was 14.9% and those who left against medical advice comprised 16.6%. Mortality in ACSH is higher than in similar studies done in Sudan, Nigeria, and Jimma,1,6,25 but lower than in other studies done in Ethiopia, Uganda, and Nigeria.22,28,29,38 The mortality might have been underestimated, because a number of patients left against medical advice. On multivariate analysis, the independent predictors of mortality were presence of complications and disease category (CDs vs NCDs). Patients with CDs had a higher mortality rate than those with NCDs but the proportionate mortality rate was higher for NCDs than CDs. Among those with CDs, the age-group 35–44 years had the highest proportion of deaths, while among the NCD cases, the age-group 65–74 years had the most deaths. This implies that comparatively, CDs continue to take the lives of the productive segment of the population of the nation, similarly to other studies in Ethiopia.22 Nevertheless, since the total number of NCD admissions was higher by far than CDs, NCDs contributed 60% of total deaths. In this study, the major causes of in-hospital mortality were heart failure, HIV/AIDS, stroke, sepsis, and kidney failure in 16.1%, 15.1%, 11.9%, 7.4%, and 7.1%, respectively, as opposed to the Ugandan finding, where HIV/AIDS, tuberculosis, non-tuberculosis pneumonia, sepsis, and malaria comprised 44.5%, 19.7%, 17.9%, 9%, and 3.6%, respectively.29 Our study shows the high number of CD deaths from HIV/AIDS, tuberculosis, and sepsis, as is the case with Uganda and other sub-Saharan nations, but clearly depicts the overwhelming contribution of NCDs to the number of deaths, particularly due to CVDs like heart failure and strokes.
Presence of a complication after admission was independently associated with higher mortality. More than 16% of all admissions had complications. The most common complications were aspiration pneumonia, hospital-acquired pneumonia, and AKI. The types of complication were not mentioned in previous similar studies in Ethiopia. The leading risk factor of aspiration pneumonia in our study, stroke, has been reported by previous studies.20,39 This study found a higher proportion of aspiration pneumonia in stroke patients (23.2%) than a study in northwest Ethiopia, where aspiration pneumonia was found in 19% of strokes. Aspiration pneumonia was also the main contributor of mortality in the Ethiopian and Nigerian studies.40,41 The incidence of AKI in our setting (1.2%) was a bit lower than the 3.6% incidence reported from Nigeria, but similarly to our study, septicemia was the leading associated factor of AKI in this and other Nigerian studies.42,43 A study in the US also reported the most common primary diagnoses associated with AKI were circulatory diseases (25.4%) and infection (16.4%), similar to this study.44 We believe that the incidence of AKI in our setting may be an underestimate. First, we did not strictly follow and document the urine output of each and every patient admitted, and secondly there were encounters of financial constraints of all patients for baseline and follow-up creatinine testing, even in those cases with clinically suspected AKI. In-hospital mortality was much higher in our setting (54%) than the Nigerian study, which was 31%.42 This could be due to late recognition and treatment and/or lack of access to dialysis due to financial constraints.
Measures of health-service utilization are very useful to improve the health-care delivery system of the population of a given catchment area a hospital serves. ACSH medical admissions’ average BOR was found to be 54%, which is lower than the conventional benchmark of 85% but higher than what was reported by Usman et al in Pakistan — 51.33%.45 ACSH’s BOR is also higher than what was reported in Nigeria over a 7-year period from three teaching hospitals as 42.14%, but lower than in a report from Tunisia: 58.1% for 40 Hospitals.46 ACSH medical wards had a BTR of 18 patients/bed/year. Hospitals/wards taking care of chronic conditions that need longer stays may have low BTR, and hence care should be taken. The BTR of ACSH medical wards was lower than its counterpart teaching hospitals in Nigeria, which was 21.27 patients/bed/year, and much less than reports from Iran, where the BTR was 61.10–95.54 patients/bed/year. TI should be <3 days, and the longer the TI of a hospital, the less efficient the hospital is. ACSH TI was found to be 9.3 days.46 Overall, this study has found a lower BOR, low BTR, and high TI than set standards and some similar institutions across different countries.
Strengths and Limitations
One of the strengths of the study is that the data were collected prospectively with the aim of avoiding the inherent limitation of retrospective studies. Also, we were able to collect the information we needed from every medical ward and ICU admission during the study period, and hence there were no missed cases. This study was done in the biggest referral center in the northern Ethiopian region, and there are no other specialized or subspecialized centers that are able to take care of specific diseases or conditions. That means that all patients who need tertiary-level care are referred to our institution, and hence all disease varieties would have had an equal chance of being represented in our study.
However, this study may not necessarily reflect the actual disease pattern in the community, and hence it is difficult to extrapolate the findings to the nation/region at large. We reported combined medical ICU and ward admissions and did not analyze them separately, which would have been easier for comparison between ICU and medical admissions. The fact that the study was done in a university teaching hospital with relatively advanced diagnostic and interventional services for specific diseases increases the chance of a referral bias. However, even in our setting, we acknowledge the constraint of resources to confirm some specific final diagnoses (ischemic heart disease, cancers, particularly hematologic disorders, and complications like aspiration pneumonia, among others) in our patient population.
A single-center prospective study gives an overview of the patterns of diseases, but multisite prospective studies and particularly disease-specific registries need to be implemented to create cohorts of patient populations and generate robust data for Ethiopia and the East African region. The reported measures of ACSH medical admissions’ health service–utilization efficiency (hospital/medical ward and ICU performance) can be used by hospital leaders and others as baseline figures for future measures of service-quality improvement of the hospital, but cannot be generalized, particularly to setups with a different case mix of hospital admissions from ACSH.
Conclusion and Recommendations
The pattern of prospectively observed data on medical admission to ACSH over a 1-year period indicated a predominance of NCDs over CDs. CVDs were the most common cause of medical admissions, followed by CDs, which were dominated by HIV/AIDS. Early recognition and prompt treatment of complications like aspiration pneumonia in patients with stroke and AKI in septicemia or heart failure patients is recommended to reduce the associated high case fatality.
This study adds to the growing data on ongoing epidemiological transitions in developing nations. Due attention should be given to the changing pattern of diseases by health professionals, local and national health planners, policy-makers, and related stakeholders to prevent and control the high morbidity and high proportionate mortality due to NCDs and higher case:fatality ratio of CDs. The performance indicators in terms of utilization of hospital beds compared to set standards and similar institutions should be utilized as baseline by hospital administrators of ACSH for further improvement.
Acknowledgment
We are thankful to all colleague consultant physicians in the Department of Internal Medicine at Mekelle University College of Health Sciences (MU-CHS), nurses (those who were involved in assisting data collection by resident physicians), and all other MU-CHS staff who were involved in the care of the patients. We are also grateful to MU-CHS, ACSH, and the patients who were admitted during the study period.
Disclosure
The authors declare no conflicts of interest.
References
1. Noor SK, Elmadhoun WM, Bushara SO, Ahmed MH. The changing pattern of hospital admission to medical wards: burden of non-communicable diseases at a hospital in a developing country. Sultan Qaboos Univ Med J. 2015;15(4):e517–22. doi:10.18295/squmj.2015.15.04.013
2. Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222.
3. Ogun SA, Adelowo OO, Familoni OB, Jaiyesimi AE, Fakoya EA. Pattern and outcome of medical admissions at the Ogun State University Teaching Hospital, Sagamu–a three year review. West Afr J Med. 2000;19:304–308.
4. Dalal S, Beunza JJ, Volmink J, et al. Non-communicable diseases in sub-Saharan Africa: what we know now. Int J Epidemiol. 2011;40(4):885–901. doi:10.1093/ije/dyr050
5. Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: overcoming impediments to prevention and control. JAMA. 2004;291:2616–2622. doi:10.1001/jama.291.21.2616
6. Odenigbo CUOO. Pattern of medical admissions at the federal medical centre, Asaba: a two year review. Nigeria J Clin Pract. 2009;12:395–397.
7. Omar SM, Osman OS, Gasim GI, et al. Pattern and trends in adult hospitalization/admission and mortality among medical ward inpatients at gadarif hospital in eastern Sudan: a four-year retrospective study pattern and trends in adult hospitalization/admission and mortality among medical. Int J Gen Med. 2022;15:5879–5889. doi:10.2147/IJGM.S367513
8. Bayray A, Assefa M, Bekele A. Levels and trends of mortality: a five year retrospective hospital record levels and trends of mortality: a five year retrospective hospital record review. Res Rev J Comput Biol. 2018;6:1.
9. Etyang AO, Anthony J, Scott G, et al. Medical causes of admissions to hospital among adults in Africa: a systematic review Anthony. Glob Heal Action. 2013;6:19090. doi:10.3402/gha.v6i0.19090
10. Damasceno A. Noncommunicable Disease. Heart of Africa: Clinical Profile of an Evolving Burden of Heart Disease in Africa. John Wiley \& Sons; 2016:155–157.
11. Misganaw A, Mariam DH, Araya T, Ayele K. Patterns of mortality in public and private hospitals of Addis Ababa, Ethiopia. BMC Public Health. 2012;12(1):1. doi:10.1186/1471-2458-12-1007
12. Weldearegawi B, Ashebir Y, Gebeye E, et al. Emerging chronic non-communicable diseases in rural communities of Northern Ethiopia: evidence using population-based verbal autopsy method in Kilite Awlaelo surveillance site. Health Policy Plan. 2013;28:891–898. doi:10.1093/heapol/czs135
13. Memirie ST, Dagnaw WW, Habtemariam MK, et al. Addressing the impact of noncommunicable diseases and injuries (NCDIs) in Ethiopia: findings and recommendations from the Ethiopia NCDI Commission. Ethiop J Health Sci. 2022;32(1):161–180. doi:10.4314/ejhs.v32i1.18
14. Marszalek J, De Villiers P. Morbidity profile of admissions to gf jooste hospital, manenberg, Cape Town. South African Fam Pract. 2006;48(6):15–15e. doi:10.1080/20786204.2006.10873402
15. World Health Organization. Global Status Report on Noncommunicable Diseases. World Health Organization; 2014.
16. Woods N, Ahern S, Burke F, Eaton KA, Widström E. The healthcare system and the provision of oral healthcare in European Union member states. Part 7: republic of Ireland. Br Dent J. 2017;222:541–548 p. doi:10.1038/sj.bdj.2017.317
17. World Health Organization. International Statistical classification of diseases and related health problems, 10th revision ICD-10: tabular list. World Health Organiz. 2016;1:332–345.
18. Melisa L, Thombley JD, Daniel D, Stier J. Centers for disease control and prevention. Menu of suggested provisions for state tuberculosis prevention and control laws: definitions for consideration. Available from: www.cdc.gov/tb/programs/laws/menu/definitions.htm.
19. Kellum AJ. Official journal of the international society of nephrology kdigo clinical practice guideline for acute kidney injury. Kidney Int. 2012;2:1.
20. Lionel A, Mandell MD, Michael S, Niederman MDA. Aspiration pneumonia. N Engl J Med. 2019;380:651–663. doi:10.1056/NEJMra1714562
21. Hussein K. Pattern of medical admissions to Jimma Hospital. Bull Inst Heal Sci. 1995.;7(1):51–62.
22. Bane A, Bayisa T, Adamu F, Abdissa SG. Medical admissions and outcomes at saint paul’s hospital, addis Ababa, Ethiopia: a retrospective study Abate. Ethiop J Heal Dev. 2016;30(1):8.
23. Gallagher J, Mcdonald K, Ledwidge M, Watson CJ. Clinical syndromes heart failure in Sub-Saharan Africa. Radcliff Cardiol. 2018;4:21.
24. Dokainish H, Teo K, Zhu J, et al. Heart Failure in Africa, Asia, the Middle East and South America: the INTER-CHF study. Int J Cardiol. 2016;204:133–141. doi:10.1016/j.ijcard.2015.11.183
25. Elias Ali MW. Reasons and outcomes of admissions to the medical wards of Jimma University Specialized Hospital, Southwest Ethiopia. Ethiop J Heal Sci. 2010;20:2.
26. Agu CE, Kalu UA. Pattern of medical admissions in a tertiary health centre. J Biol Agric Healthc. 2013;3(12):90–95.
27. Adeoti AO, Ajayi EA, Ajayi AO, et al. Pattern and outcome of medical admissions in Ekiti State University Teaching Hospital, Ado-Ekiti- A 5 Year review. Am J Med Med Sci. 2015;5(2):92–98.
28. Ike SO. The pattern of admissions into the medical wards of the University of Nigeria Teaching Hospital, Enugu (2). Niger J Clin Pract. 2008;11(3):185–192.
29. Kalyesubula R, Mutyaba I, Rabin T, et al. Trends of admissions and case fatality rates among medical in-patients at a tertiary hospital in Uganda; A four-year retrospective study. PLoS ONE. 2019;14(5):1–14.
30. Tesfaye F, Byass P, Wall S, de Bie RA, Prins MH, Teijink JAW. Population based prevalence of high blood pressure among adults in Addis Ababa: uncovering a silent epidemic. BMC Cardiovasc Disord. 2009;9:9. doi:10.1186/1471-2261-9-9
31. Feleke Y, Yadeta D, Kebede T. Hyperglycemia, dyslipidemia, metabolic syndrome and their determinants in Ethiopia: evidences from the National NCDs STEPS; 2018.
32. Ballard DJ, Bryant SC, O’Brien PC, Smith DW, Pine MB, Cortese DA. Referral selection bias in the medicare hospital mortality prediction model: are centers of referral for medicare beneficiaries necessarily centers of excellence? Health Serv Res. 1994;28(6):771–784.
33. Federal Democratic Republic of Ethiopia Ministry of Health. Addressing the impact of noncommunicable diseases and injuries in Ethiopia: findings and recommendations from Noncommunicable Diseases and Injuries (NCDI) commission of Ethiopia; 2018.
34. Yizengaw HA, Ayele WM, Worku A. The trend and pattern of adult mortality in South- Central Ethiopia: analysis using the 2008–2019 data from butajira health and demographic surveillance system. Glob Health Action. 2022;15(1). doi:10.1080/16549716.2022.2118180
35. Melaku YA, Sahle BW, Tesfay FH, et al. Causes of death among adults in northern Ethiopia: evidence from verbal autopsy data in health and demographic surveillance system. PLoS One. 2014;9(9):e106781. doi:10.1371/journal.pone.0106781
36. Ashenafi W, Eshetu F, Assefa N, et al. Trend and causes of adult mortality in Kersa health and demographic surveillance system (Kersa HDSS), eastern Ethiopia: verbal autopsy method. Popul Health Metr. 2017;15:1–10. doi:10.1186/s12963-017-0144-2
37. Gidey K, Hailu A, Bayray A. Pattern and outcome of medical intensive care unit admissions to ayder comprehensive specialized hospital in Tigray. Ethiopia. 2018;56(1):31–36.
38. Ezeala-Adikaibe B, Aneke E, Aneke C, et al. Pattern of medical admissions at Enugu State university of science and technology teaching hospital: a 5 year review. Ann Med Health Sci Res. 2014;4(3):426. doi:10.4103/2141-9248.133472
39. Dibardino DM, Wunderink RG. Aspiration pneumonia: a review of modern trends. J Crit Care. 2015;30(1):40–48. doi:10.1016/j.jcrc.2014.07.011
40. Greffie ES, Mitiku T, Getahun S. Risk factors, clinical pattern and outcome of stroke in a referral hospital, risk factors, clinical pattern and outcome of stroke in a referral hospital, Northwest Ethiopia. Clin Med Res. 2015;4(6):182–188. doi:10.11648/j.cmr.20150406.13
41. Obiako OR, Oparah SK, Ogunniyi A. Prognosis and outcome of acute stroke in the University College Hospital Ibadan. Nigeria. 2011;14(3):1–4.
42. Edet Effa E, Ohem Okpa H, Mbu PN, Epoke EJ, Otokpa DE. Acute kidney injury in hospitalized patients at the University of Calabar Teaching Hospital: an aetiological and outcome study. IOSR J Dent Med Sci Ver. 2015;14(3):2279–2861.
43. Chijioke A, Makusidi A. Severe acute kidney injury in adult Nigerians from University of Ilorin Teaching Hospital, Ilorin, Kwara state. Bomj. 2011;8(1):5–9.
44. Wang HE, Chertow M, Warnock DG, Warnock DG. Acute kidney injury and mortality in hospitalized patients. Am J Nephrol. 2012;35:349–355. doi:10.1159/000337487
45. Usman G, Khalida Naz Memon SS, Shaikh S. Bed occupancy rate and length of stay of patients in medical and bed occupancy rate and length of stay of patients in medical and allied wards of a tertiary care hospital. J Ayub Med Coll Abbottabad. 2015;27(2):367–370.
46. Aloh HE, Onwujekwe OE, Aloh OG, Nweke CJ, Cheng W, Hu S. Is bed turnover rate a good metric for hospital scale efficiency? A measure of resource utilization rate for hospitals in Southeast Nigeria. Cost Eff Resour Alloc. 2020;18:1–8. doi:10.1186/s12962-019-0198-z
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.