Back to Journals » Journal of Pain Research » Volume 12
Patterns of drug treatment in patients with osteoarthritis and chronic low back pain in Japan: a retrospective database study
Authors Akazawa M , Mimura W , Togo K , Ebata N , Harada N, Murano H, Abraham L, Fujii K
Received 30 January 2019
Accepted for publication 16 April 2019
Published 21 May 2019 Volume 2019:12 Pages 1631—1648
DOI https://doi.org/10.2147/JPR.S203553
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Katherine Hanlon
Manabu Akazawa,1 Wataru Mimura,1 Kanae Togo,2 Nozomi Ebata,3 Noriko Harada,4 Haruka Murano,5 Lucy Abraham,6 Koichi Fujii3
1Public Health and Epidemiology, Meiji Pharmaceutical University, Tokyo, Japan; 2Corporate Affairs, Health & Value, Pfizer Japan Inc., Tokyo, Japan; 3Medical Affairs, Pfizer Japan Inc., Tokyo, Japan; 4Clinical Research, Pfizer R&D Japan G.K., Tokyo, Japan; 5Clinical Research Professionals, Clinical Study Support Inc., Nagoya, Japan; 6Patient & Health Impact, Pfizer Ltd., Surrey, UK
Purpose: Musculoskeletal diseases, including osteoarthritis (OA) and low back pain (LBP), are the leading causes of years lived with disability, and are associated with lowered quality-of-life, lost productivity, and increased healthcare costs. However, information publicly available regarding the Japanese real-world usage of prescription medications is limited. This study aimed to describe the clinical characteristics of patients with OA and chronic LBP (CLBP), and to investigate the patterns of medications and opioid use in Japanese real-world settings.
Materials and methods: A retrospective study was conducted using a Japanese administrative claims database between 2013 and 2017. The outcomes were patient characteristics and prescription medications, and they were evaluated separately for OA and CLBP.
Results: The mean age of 118,996 patients with OA and 256,402 patients with CLBP was 68.8±13.1 years and 64.8±16.4 years, respectively. Approximately 90% of patients with OA and CLBP were prescribed non-steroidal anti-inflammatory drugs (NSAIDs). Other prescriptions included hyaluronate injection (35.6%), acetaminophen (21.4%), and steroid injection (20.0%) in patients with OA, and pregabalin (39.0%) and acetaminophen (22.4%) in patients with CLBP. Weak opioids were prescribed to 10.7% and 20.6% of patients with OA and CLBP, respectively. The prescription of COX-2 inhibitors (OA: +6.5%; CLBP: +6.7%) and acetaminophen (OA: +16.4%; CLBP: +14.4%) increased between 2013 and 2017. The first commonly prescribed medication among patients with OA and CLBP were NSAIDs; hyaluronate injection (patients with OA) and pregabalin (patients with CLBP) were also common first-line medications. Acetaminophen, steroid injection (patients with OA), and weak opioids were prescribed more in the later phases of treatment.
Conclusion: Most patients were prescribed limited classes of pain drugs, with NSAIDs being the most common pain medication in Japan for patients with OA and CLBP. Opioid prescription was uncommon, and were weak opioids when prescribed.
Keywords: osteoarthritis, chronic low back pain, non-steroidal anti-inflammatory drugs, opioid, pain
Introduction
The life expectancy of the Japanese population as of 2016 was 81.1 and 87.1 years for men and women, respectively;1 however, the healthy life expectancy of Japanese men and women is 72.6 and 76.9 years,2 respectively, which is approximately 8–10 years shorter, due to diseases and/or injuries, than their life expectancies. Musculoskeletal diseases including osteoarthritis (OA) and low back pain (LBP) are the leading causes of years lived with disability in Japan,3 and are associated with lowered quality-of-life (QoL), lost productivity, and increased healthcare costs.4–7 Both OA and chronic LBP (CLBP) are common health problems in Japan (prevalence of radiographic knee and hip OA: 55.6%8 and 2.4%;9,10 prevalence of CLBP in ages >50: 15.4%11). These diseases negatively impact the healthy aging of the present and future populations.12,13
Treatments of OA focus on alleviating pain, reducing stiffness, maintaining functional capacities, and improving QoL.6 The Japanese Osteoarthritis Research Society International (OARSI) guideline for knee OA recommends non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and intra-articular injection of steroid and hyaluronate as first-line pharmacological treatments.14 The use of weak opioids can be considered for the treatment of refractory pain, where other pharmacological agents have been ineffective or are contraindicated. The guideline recommends not to use strong opioids and to consider non-pharmacological treatments.14 First-line non-pharmacological treatments are rehabilitation (eg, aerobic exercise, muscle strengthening)14 and surgery, including total knee arthroplasty and total hip replacement, both of which are reported as effective in improving function and QoL for patients whose pain cannot be relieved with pharmacotherapy.15,16
The treatments of CLBP aim to relieve pain and improve function, rather than cure.17 This is because the diagnosis of CLBP pathology is often limited, except for patients with radiculopathy, spinal stenosis, or other specific spinal causes,18 the diagnosis of which may be established by magnetic resonance imaging or computed tomography. The Japanese guideline for CLBP recommends NSAIDs, COX-2 inhibitors, and acetaminophen as the first-line pharmacological treatments.19 Similar pain medications are recommended in the UK.20 Second-line pharmacological recommendations include tricyclic antidepressants, opioids, and anticonvulsants, supplemented by appropriate non-pharmacological measures, such as exercise programs, manual therapies, behavioral therapies, interventional pain management, and traction.19
Opioids, classified as weak (eg, codeine, tramadol, buprenorphine) or strong (eg, morphine, oxycodone, fentanyl, remifentalil, methadone) in Japan, are a type of analgesic for both neuropathic and nociceptive pain.21 They are largely prescribed for chronic pain,22 and are a potential pain medication for patients with OA and CLBP. However, high risk of misuse, abuse, and harm associated with opioids has been reported, particularly in the United States of America (US).23 In Japan, opioids are generally prescribed when pain cannot be controlled with other pharmacotherapies.14,19 However, the sales and use of opioids for treating chronic pain have been increasing since their approval in Japan in 2011.21,24
Limited information is publicly available regarding the Japanese real-world usage of prescription medications, including opioids, among patients with OA and CLBP. Therefore, this study aimed to describe the clinical characteristics of patients with OA and CLBP and to investigate the patterns of medications and opioid use in Japanese real-world settings.
Materials and methods
Data source
A retrospective study was conducted using an administrative claims database provided by Medical Data Vision Co., Ltd. (MDV, Tokyo, Japan). At the time of this study (as of July 2018), the electronic record-based hospital claims database contained medical information of more than 23 million patients in Japan from 364 facilities that participated in the diagnosis procedure combination per-diem payment system (DPC/PDPS).
The MDV database contained information from hospitals capable of treating advanced stage patients, including, but not limited to, acute care facilities. The database excluded patients’ data from clinics, nursing homes, and hospices, but included both in- and outpatients, including demographics (eg, age, sex) and medical records (eg, examination, procedures, prescriptions, disease names based on the International Classification of Diseases 10th revision [ICD-10, 2013], Japanese claims codes).
Ethics statement
The study was conducted in accordance with the guidelines of Good Pharmacoepidemiology Practices (GPP) issued by the International Society for Pharmacoepidemiology. Informed consent for this study was not required because this was an observational study using de-identified structured claims data, and the Japanese Ethical Guidelines for Medical and Health Research Involving Human Subjects do not apply to studies utilizing anonymized secondary data.
Study population
We used patient records from January 1, 2013 to December 31, 2017. The start of the study period was selected to be approximately 1.5 years after the launch of Tramcet®, a combination drug of tramadol and acetaminophen, in Japan in 2011. The target populations were patients diagnosed with OA or CLBP.
The inclusion criteria of the OA cohort were 1) an initial diagnosis record of OA with ICD-10 codes (2013) of M16 (coxarthrosis) or M17 (gonarthrosis) but excluding M16.1 (rapid destructive coxarthrosis with a claim code of 2096965), 2) ≥2 prescriptions of pain drugs on separate dates by orthopedists or anesthesiologists, and 3) age of ≥18 years at index date (the date of the first drug prescription for pain treatments following the initial diagnosis record of OA, Figure 1). The classes of pain drugs examined were NSAIDs (oral or transdermal), acetaminophen, hyaluronate injection, steroid injection, weak opioids (tramadol, codeine, buprenorphine), strong opioids (fentanyl), serotonin-norepinephrine reuptake inhibitors (SNRI), duloxetine, and other non-opioid drugs (Table S1). The exclusion criteria were 1) malignancy (ICD-10 codes of C00-C97 and D00-D09), and 2) diagnosis of CLBP.
The CLBP cohort was identified first with ICD-10 codes of M40 (kyphosis and lordosis), M41 (scoliosis), M43 (spondylolysis), M45–49 (spondylopathy), or M50–54 (other dorsopathies), but excluding sub-items listed in Table S2. Chronic pain was defined as having at least two ICD10 diagnoses of LBP within 3 months and ≥1 month apart. The second and the third inclusion criteria were the same as those for the OA cohort, but the class of pain drugs for this cohort included pregabalin but excluded hyaluronate injection and steroid injection. The exclusion criteria were 1) malignancy, and 2) diagnosis of OA.
Statistical analysis
The baseline information was evaluated for all patients with OA or CLBP meeting the inclusion and exclusion criteria, and patients with a follow-up period of ≥1 year. To describe demographic and clinical characteristics of the patients, information including age, sex, duration of disease at index date, in- or outpatient, and comorbidities of interest at baseline were summarized. To investigate the prescription pattern and treatment sequence, we examined the pain drug classes prescribed after the index date by an orthopedist or anesthesiologist (Table S1). To investigate opioid use, time to the first weak opioid prescription, treatment duration (the duration from the date of the first weak opioid prescription to the end date of the prescription, including days without prescription medicines), dose of weak opioids, and the number of drug classes prescribed before the weak opioid prescription were examined. The treatment duration and dose of weak opioids were evaluated separately for tramadol and the combination of tramadol and acetaminophen (thereafter tramadol/acetaminophen combination).
The follow-up period was defined from the index date to the end date of pain drug prescription or the date of surgery for patients with OA (Table S3), whichever occurred later. The prescription medications were examined for all patients from 2013 to 2017 and examined separately for each year, and the treatment sequence from the first to fifth treatment was examined for patients with a follow-up period of ≥1 year.
Patient demographic and characteristics at baseline and prescription medicines were summarized using descriptive analysis, with mean±standard deviation or median [the first quartile=Q1, the third quartile=Q3] for continuous variables or number and percentage (%) for categorical variables.
The time to the first weak opioid prescription was censored during surgery if surgery was performed before the first prescription of a weak opioid; the median time was calculated using the Kaplan–Meier method. Treatment duration with weak opioids was also estimated using the Kaplan–Meier method, censoring the duration at surgery or the last visit if the treatment was ongoing. The number of weak opioid prescriptions and drug classes prescribed before the weak opioid prescription was also summarized using descriptive statistics. Results were presented as described above. All statistical analyses were performed using SAS Release 9.3 (SAS Institute, Cary, NC, USA).
Results
We identified 20,806,511 patient records between January 1, 2013 and December 31, 2017 (Figure 2), wherein 687,793 and 1,695,811 patients with OA and CLBP, respectively, were identified. Among these, 44.3% (OA) and 17.9% (CLBP) of patients had both CLBP and OA, and therefore were excluded from the OA or CLBP cohorts. Finally, 118,996 patients and 256,402 patients with OA and CLBP, respectively, met the inclusion and exclusion criteria.
 | Figure 2 Flow of patient extraction. Abbreviations: CLBP, chronic low back pain; MDV, Medical Data Vision Co., Ltd.; OA, osteoarthritis. |
Demographic and clinical characteristics
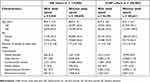
Demographic and clinical characteristics of patients with OA and CLBP are summarized in Table 1. The mean age of patients with OA (68.8±13.1 years) was slightly higher than that of patients with CLBP (64.8±16.4 years). There were more women in the OA cohort (73.3%), but both sexes were equally represented in the CLBP cohort (females: 52.1%). Among patients with OA, 83.4% and 16.6% had gonarthrosis and coxarthrosis, respectively. The proportion of hospitalized patients was slightly higher in the OA cohort (21.5%) than the CLBP cohort (17.6%). The most common comorbidity was cardiovascular disease in both cohorts (OA: 34.8%; CLBP: 35.7%), followed by sleep disorder (OA: 8.7%; CLBP: 11.8%) and gastrointestinal disorder (OA: 8.4%; CLBP: 11.0%). The median follow-up period was 24.1 [6.3–77.1] weeks and 24.6 [8.1–77.7] weeks for patients with OA and CLBP, respectively, and patients with a follow-up period of ≥1 year consisted >30% in both cohorts. The baseline demographic and clinical characteristics of patients with OA and CLBP with a follow-up period of ≥1 year were similar to those of the overall patients.
 | Table 1 Patient demographics and clinical characteristics at baseline |
Prescriptions
The majority of the 118,996 patients with OA and 256,402 patients with CLBP were prescribed NSAIDs (OA: 92.0%; CLBP: 88.2%, Table 2). The prescription of oral NSAIDs was slightly more common than transdermal NSAIDs among patients with CLBP (oral: 71.0%; transdermal: 60.6%). With regard to oral NSAIDs, non-selective COX inhibitors were prescribed to more than two thirds of patients in both cohorts (OA: 67.0%; CLBP: 72.6%), whereas COX-2 inhibitors were prescribed to approximately half of the patients (OA: 48.4%; CLBP: 42.1%). The second most frequently prescribed pain drugs differed depending on the cohort. Among patients with OA, hyaluronate injection (35.6%) was the second most prescribed pain drug, followed by acetaminophen (21.4%) and steroid injection (20.0%). Among patients with CLBP, pregabalin (39.0%) was the second most prescribed pain drug, followed by acetaminophen (22.4%).
 | Table 2 Pain drug classes prescribed since the day of the first pain drug prescription (index date) for all patients combined (total) and patients from 2013 to 2017 |
NSAIDs were consistently highly prescribed in both cohorts from 2013 to 2017 (>80%), with a small reduction in the prescription of oral NSAIDs only among patients with CLBP (−10.5%) in 5 years (Table 2). The prescription of non-selective COX inhibitors slightly decreased between 2013 and 2017 among patients with OA and CLBP, whereas that of COX-2 inhibitors increased by similar proportions. The prescription of acetaminophen was uncommon in 2013 (OA: 4.7%; CLBP: 7.0%), but gradually increased over the next 5 years, with an increase of 16.4% among patients with OA and 14.4% among patients with CLBP.
Weak opioids were prescribed to 10.7% of patients with OA, but were more commonly prescribed among patients with CLBP (20.6%, Table 2). Tramadol was the main weak opioid prescribed in both cohorts, and codeine, buprenorphine, and strong opioid (fentanyl) were rarely prescribed. From 2013 to 2017, the prescription of weak opioids increased 5.7% among patients with OA and 6.6% among patients with CLBP.
Treatment sequence
As the first-line treatment for pain, approximately half of patients with OA with a follow-up period of ≥1 year were prescribed oral NSAIDs (48.9%) or transdermal NSAIDs (59.0%, Table 3), followed by hyaluronate injection (26.2%). In contrast, steroid injections (8.2%) and acetaminophen (3.9%) were rarely administered as the first-line treatment, but these drugs were prescribed more in the later phases of pain treatment. Only 3.2% of patients with OA received weak opioids as a first-line treatment, but their prescription increased to 20.7% by the fifth treatment.
 | Table 3 Treatment sequence of pain drug classes prescribed first to fifth line among patients with a follow-up period of ≥1 year |
Similar to patients with OA, patients with CLBP were most frequently prescribed NSAIDs as the first-line treatment (oral: 51.4%; transdermal: 50.2%, Table 3). Pregabalin was also commonly prescribed first (20.8%), but its prescription became less common in the later phases of treatment. Weak opioids (8.2%), acetaminophen (6.5%), and duloxetine (0.7%) were prescribed rarely as initial treatments, but were more frequently prescribed in the later phases. Similar to patients with OA, only 8.2% of patients with CLBP were prescribed weak opioids as the first-line treatment, but the proportion of patients prescribed weak opioids increased to 15.9% by the fifth treatment.
The number of patients with OA prescribed at least three classes of pain drugs was relatively small (19.7%), with a few being prescribed four classes (5.1%) or five or more classes (1.2%) of pain drugs (Table 2). The number of patients with CLBP prescribed at least three classes of pain drugs was slightly higher (30.8%) compared with that of patients with OA, but only a few patients were prescribed four classes (10.5%) or five or more classes (3.4%) of pain drugs.
Prescriptions among patients with opioid treatments
The median time to the first weak opioid prescription was 92 [1–491] days among patients with OA and 71 [1–432] days among patients with CLBP, with a follow-up period of ≥1 year. The median treatment duration in patients with OA was 55 [15–329] days and 108 [28–442] days for tramadol and tramadol/acetaminophen combination, respectively, with the median dose being 50.0 [45.4–94.3] mg/day (tramadol) and 75.0 [62.5–112.5] mg/day (tramadol/acetaminophen combination) (Table 4). The treatment duration of weak opioids in patients with CLBP was 140 [28–459] days and 254 [43–624] days for tramadol and tramadol/acetaminophen combination, respectively, with a median dose of 66.7 [50.0–100.0] mg/day (tramadol) and 93.8 [75.0–112.5] mg/day (tramadol/acetaminophen combination). The majority of patients with OA (68.5%) and CLBP (87.9%) who were prescribed weak opioids used one-to-three classes of pain drugs before the first weak opioid prescription. Compared with the patients with OA and CLBP with a follow-up period of ≥1 year, the time to first weak opioid and the treatment duration of overall patients were shorter among overall patients, but the treatment doses and the number of pain drugs prescribed before weak opioid prescriptions were similar.
 | Table 4 Time to the first weak opioid prescription, treatment duration and dose, and number of drug classes prescribed before weak opioids |
Patients with OA who were prescribed weak opioids used acetaminophen and steroid injection more than those without a weak opioid prescription (acetaminophen: 23.3% vs 13.2%; steroid injection: 28.6% vs 19.0%, Table S4). Pregabalin was prescribed more to patients with CLBP using weak opioids than those who did not (61.6% vs 35.2%). The baseline demographic and clinical characteristics of patients with OA and CLBP who were and were not prescribed weak opioids were similar in terms of age, sex, duration of disease, and comorbidities (Table S5).
Discussion
This is the first study that examined prescription medications among patients with OA and CLBP in a real-world setting using Japanese hospital claims data with more than 370,000 patients. As expected,25 women comprised the majority in the OA patient group and almost half in the CLBP patient group. Published data of age in Japan have shown a broad range, from 54 years in OA patients26 and 52 years in LBP patients27 to approximately 70 years in patients with knee OA and lumbar spondylosis.25 The mean ages observed in this study (OA: 68.8 years, CLBP: 64.8 years) are in this range. One reason for the younger population of CLBP than OA is considered the relationship between the development of CLBP and occupations.28
The study showed that NSAIDs were prescribed to approximately 90% of patients with OA and CLBP, and were the most standard pain treatment in Japan. The study also found that NSAIDs were prescribed for long-term use, and most patients were treated with limited classes of pain drugs, with only a few patients prescribed three or four classes of pain drugs. The prescription of NSAIDs was remarkably high in Japan compared with the published records in the US (37.1–65.4% of patients with OA;29–31 35.0–56.1% of patients with CLBP31–33), although over-the-counter (OTC) NSAIDs drugs (as well as acetaminophen) may be more widely used in the US. This is because the use of transdermal NSAIDs are common in Japan. The Japanese OARSI guideline for knee OA recommends the use of transdermal NSAIDs as the first-line treatment.14,34 Transdermal NSAIDs have a superior safety profile with fewer adverse events than oral NSAIDs.19,35,36 However, an online survey in Japan found that approximately half of patients were unsatisfied with the analgesic effect of NSAID patches, and 37% of patients prescribed with NSAIDs patches used these in combination with oral NSAIDs.37 No guidelines exist on the concurrent use of transdermal and oral NSAIDs, and further research is needed to investigate the safety and effectiveness for concurrent use.
The use of non-selective COX inhibitors decreased between 2013 and 2017, whereas that of COX-2 inhibitors increased. Non-selective COX inhibitors were possibly replaced by acetaminophen or COX-2 inhibitors because of their adverse reactions. Although there is a high level of evidence for NSAIDs regarding short-term pain relief and improvements in activities of daily living, the Japanese guidelines do not recommend their use in high-risk patients or for long-term use14,19 because of adverse events (eg, gastrointestinal disorder, kidney failure, and cardiovascular disease).38–44
Acetaminophen was prescribed more in the later phases of pain treatment, although acetaminophen is recommended as a first-line treatment in the Japanese guidelines for both OA and CLBP.14,19 The reason may be because NSAIDs are the preferred choice as a first-line treatment due to better efficacy, but then a waning of response, side-effects, or concerns with long-term safety result in switching to acetaminophen. The increase of acetaminophen use between 2013 and 2017 may be due to the approval of its higher dosage in 2011 (maximum dose of 400 mg/day) and the 2012 guideline recommendation to use as a first-line treatment.14,19
The prescription pattern of opioids in Japan greatly differs from that in the US.41,45 Opioids are more commonly prescribed in the US, accounting for 37.0−79.0% of prescriptions for patients with OA31,32 and 48.0−71.7% for patients with CLBP.30,31 The lower percentage of opioid prescription in Japan is likely driven by legal regulations, guidelines, and preferences of patients and doctors. Among the types of opioids, tramadol is the only one without any legal regulations. Fentanyl and buprenorphine can only be prescribed by doctors who have taken e-learning modules,22 and the prescription period is restricted to 14 days (buprenorphine) and 30 days (fentanyl) under the regulation for narcotic and psychotropic drugs in Japan. The extremely low level of opioid use may be because guidelines report a lack of evidence for their efficacy and discourage the use of opioids, especially strong opioids.14,46 Furthermore, the preference of doctors and patients may also affect the prescribing of opioids in Japan. Based on an online survey regarding opioid prescriptions for chronic pain,22 65% of physicians answered that treatment expectations of patients affect opioid prescribing, and Japanese respondents were less likely to consider opioids as the standard of care for chronic pain compared with American respondents (42.9% in Japan vs 56.0% in the US). In addition, Japanese physicians are more likely to select opioids only when other therapeutic choices are ineffective (73.9% in Japan vs 58.7% in the US).
Weak opioids were rarely selected in the early phases of treatment and were only used short-term once prescribed. The recommended dose of tramadol was 50 mg/day for patients with OA and 67 mg/day for patients with CLBP, and that of tramadol/acetaminophen combination was 75 mg/day for patients with OA and 94 mg/day for patients with CLBP. Because the daily dose of tramadol described on the package insert is 100–300 mg/day and 150–300 mg/day for the combination, our study found that the daily dose prescribed to patients with OA and CLBP was much lower than recommended. These results seem to reflect the treatment guidelines for chronic pain, warning against the long-term administration of weak opioids because of uncertain effectiveness and safety.14 Opioids have common adverse events, such as constipation, somnolence, and nausea,47 with additional risks of misuse and abuse, which are social issues in the US.23 However, similar issues are not anticipated in Japan in the near future because the prescription of opioids is strictly controlled by the aforementioned regulations.
Limitations
The database used in this study contains patient information from hospitals that utilize DPC/PDPS and provide acute inpatient medical care (≥20 beds), covering approximately 20% of 364 DPC facilities in Japan (as of July 2018), but it does not include patient records from clinics. Thus, the study population may not represent all patients with OA and CLBP in Japan. For instance, patients who visit the DPC hospitals may have severe conditions and be more likely to receive more medications than patients visiting clinics. In addition, patients in this study population may have more complications compared with the general population with OA and CLBP because the reason some of these patients may have visited the hospital was to treat their complications. For this study, the CLBP cohort was defined using the organic disease names to investigate the patterns of medications for pain because patients with CLBP are often diagnosed with having organic diseases in Japan. However, this may have resulted in the cohort including some patients with asymptotic conditions or those with another neuropathic pain disorder rather than LBP. Another limitation inherent to the use of the hospital-based database is that it was not possible to obtain patients’ treatment history recorded outside of hospital. Patient records from the first pain prescription provided at the DPC hospitals were examined; however, some of the patients may have been treated somewhere else first (eg, a previous clinic). Furthermore, no data was available regarding pain severity, status of pain control, or side-effects. Finally, a relatively large number of patients had both OA and CLBP and underwent surgery, and further examination may reveal pharmacotherapy in these subgroups of patients.
Conclusion
This is the first report on the current status of pharmacotherapy among patients with OA and CLBP in Japanese real-world clinical settings. Despite the aforementioned limitations, the study showed that, although a range of drug classes is available in Japan, the most frequently prescribed pain medication is NSAIDs. Tramadol represents the majority of opioid prescriptions in Japan. Further research is required to clarify the reason for the high prescribing rate of NSAIDs and low prescribing rate of opioids, and to provide a more detailed understanding of NSAID use.
Acknowledgments
This study was sponsored by Pfizer Japan Inc. Support for statistical analyses and medical writing were provided by Clinical Study Support, Inc. and Rie Hagihara from Clinical Study Support, Inc.
Disclosure
Kanae Togo, Nozomi Ebata, and Koichi Fujii are employees of Pfizer Japan Inc. Noriko Harada is an employee of Pfizer R&D Japan G.K. Lucy Abraham is an employee and shareholder of Pfizer Ltd. Haruka Murano is an employee of Clinical Study Support Inc. Manabu Akazawa and Wataru Mimura were not financially compensated for their collaboration in this project or for the development of this manuscript. Manabu Akazawa reports personal fees from Pfizer, and Takeda, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1.
2.
3.
4. Sadosky AB, DiBonaventura M, Cappelleri JC, Ebata N, Fujii K. The association between lower back pain and health status, work productivity, and health care resource use in Japan. J Pain Res. 2015;8:119–130.
5. Jordan KM, Arden NK, Doherty M, et al. EULAR recommendations 2003: an evidence-based approach to the management of knee osteoarthritis: report of a task force of the standing committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003;62(12):1145–1155. doi:10.1136/ard.2003.011742
6. Muraki S, Akune T, Oka H, et al. Association of radiographic and symptomatic knee osteoarthritis with health-related quality of life in a population-based cohort study in Japan: the ROAD study. Osteoarthr Cartil. 2010;18(9):1227–1234. doi:10.1016/j.joca.2009.11.014
7. Nagashima H, Suzuki M, Araki S, Yamabe T, Muto C,
8. Muraki S, Akune T, Oka H, et al. Association of occupational activity with radiographic knee osteoarthritis and lumbar spondylosis in elderly patients of population-based cohorts: a large-scale population-based study. Arthritis Rheum. 2009;61(6):779–786. doi:10.1002/art.24514
9. Inoue K, Wicart P, Kawasaki T, et al. Prevalence of hip osteoarthritis and acetabular dysplasia in French and Japanese adults. Rheumatology (Oxford). 2000;39(7):745–748. doi:10.1093/rheumatology/39.7.745
10. Pereira D, Peleteiro B, Araújo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthr Cartil. 2011;19(11):1270–1285. doi:10.1016/j.joca.2011.08.009
11. Iizuka Y, Iizuka H, Mieda T, et al. Prevalence of chronic nonspecific low back pain and its associated factors among middle-aged and elderly people: an analysis based on data from a musculoskeletal examination in Japan. Asian Spine J. 2017;11(6):989–997. doi:10.4184/asj.2017.11.6.989
12. Webb MP, Helander EM, Menard BL, Urman RD, Kaye AD. Tanezumab: a selective humanized mAb for chronic lower back pain. Ther Clin Risk Manag. 2018;14:361–367. doi:10.2147/TCRM.S144125
13. Suka M, Yoshida K. Low back pain deprives the Japanese adult population of their quality of life: a questionnaire survey at five healthcare facilities in Japan. Environ Health Prev Med. 2008;13(2):109–115. doi:10.1007/s12199-008-0038-9
14.
15. Harris WH, Sledge CB. Total hip and total knee replacement (1). N Engl J Med. 1990;323(11):725–731. doi:10.1056/NEJM199009133231106
16. Harris WH, Sledge CB. Total hip and total knee replacement (2). N Engl J Med. 1990;323(12):801–807. doi:10.1056/NEJM199009203231206
17. Patrick N, Emanski E, Knaub MA. Acute and chronic low back pain. Med Clin North Am. 2014;98(4):777–789, xii. doi:10.1016/j.mcna.2014.03.005
18. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736–747. doi:10.1016/S0140-6736(16)30970-9
19.
20.
21. Kanai A. Issues of opioid analgesics and expectations of buprenorphine. Locomot Pain Front. 2017;6(2):52–59. Japanese.
22. Onishi E, Kobayashi T, Dexter E, Marino M, Maeno T, Deyo RA. Comparison of opioid prescribing patterns in the United States and Japan: primary care physicians’ attitudes and perceptions. J Am Board Fam Med. 2017;30(2):248–254. doi:10.3122/jabfm.2017.02.160299
23. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths - United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(50–51):1445–1452. doi:10.15585/mmwr.mm655051e1
24. Wright EA, Katz JN, Abrams S, Solomon DH, Losina E. Trends in prescription of opioids from 2003–2009 in persons with knee osteoarthritis. Arthritis Care Res (Hoboken). 2014;66(10):1489–1495. doi:10.1002/acr.22125
25. Yoshimura N, Muraki S, Oka H, et al. Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J Bone Miner Metab. 2009;27(5):620–628. doi:10.1007/s00774-009-0080-8
26. Nakata K, Tsuji T, Vietri J, Jaffe DH. Work impairment, osteoarthritis, and health-related quality of life among employees in Japan. Health Qual Life Outcomes. 2018;16(1):64. doi:10.1186/s12955-018-0896-9
27. Takahashi N, Kikuchi S, Konno S, et al. Discrepancy between disability and the severity of low back pain: demographic, psychologic, and employment-related factors. Spine. 2006;31(8):931–9.28. doi:10.1097/01.brs.0000209319.94256.89
28. Matsudaira K, Kawaguchi M, Isomura T, et al. Assessment of psychosocial risk factors for the development of non-specific chronic disabling low back pain in Japanese workers-findings from the Japan Epidemiological Research of Occupation-related Back Pain (JOB) study. Ind Health. 2015;53(4):368–377. doi:10.2486/indhealth.2014-0260
29. Gore M, Tai K-S, Sadosky A, Leslie D, Stacey BR. Clinical comorbidities, treatment patterns, and direct medical costs of patients with osteoarthritis in usual care: a retrospective claims database analysis. J Med Econ. 2011;14(4):497–507. doi:10.3111/13696998.2011.594347
30. Dunn JD, Pill MW. A claims-based view of health care charges and utilization for commercially insured patients with osteoarthritis. Manag Care. 2009;18(12):44–50.
31. Gore M, Tai K-S, Sadosky A, Leslie D, Stacey BR. Use and costs of prescription medications and alternative treatments in patients with osteoarthritis and chronic low back pain in community-based settings. Pain Pract. 2012;12(7):550–560. doi:10.1111/j.1533-2500.2012.00532.x
32. Gore M, Sadosky A, Stacey BR, Tai K-S, Leslie D. The burden of chronic low back pain: clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine. 2012;37(11):E668–677. doi:10.1097/BRS.0b013e318241e5de
33. Ivanova JI, Birnbaum HG, Schiller M, Kantor E, Johnstone BM, Swindle RW. Real-world practice patterns, health-care utilization, and costs in patients with low back pain: the long road to guideline-concordant care. Spine J. 2011;11(7):622–632. doi:10.1016/j.spinee.2011.03.017
34. McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartil. 2014;22(3):363–388. doi:10.1016/j.joca.2014.01.003
35. Pontes C, Marsal JR, Elorza JM, Aragón M, Prieto-Alhambra D, Morros R. Analgesic use and risk for acute coronary events in patients with osteoarthritis: a population-based, nested case-control study. Clin Ther. 2018;40(2):270–283. doi:10.1016/j.clinthera.2017.12.011
36. Derry S, Conaghan P, Da Silva JAP, Wiffen PJ, Moore RA. Topical NSAIDs for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2016;4:CD007400. doi:10.1002/14651858.CD007400.pub3
37. Takeda O, Chiba D, Ishibashi Y, Tsuda E. Patient-physician differences in desired characteristics of NSAID plasters: an online survey. Pain Res Manag. 2017;2017:5787854. doi:10.1155/2017/8123812
38. Tramèr MR, Moore RA, Reynolds DJ, McQuay HJ. Quantitative estimation of rare adverse events which follow a biological progression: a new model applied to chronic NSAID use. Pain. 2000;85(1–2):169–182. doi:10.1016/S0304-3959(99)00267-5
39. Ofman JJ, MacLean CH, Straus WL, et al. A metaanalysis of severe upper gastrointestinal complications of nonsteroidal antiinflammatory drugs. J Rheumatol. 2002;29(4):804–812.
40. Jüni P, Nartey L, Reichenbach S, Sterchi R, Dieppe PA, Egger M. Risk of cardiovascular events and rofecoxib: cumulative meta-analysis. Lancet. 2004;364(9450):2021–2029. doi:10.1016/S0140-6736(04)17514-4
41. Aldington S, Shirtcliffe P, Weatherall M, Beasley R. Increased risk of cardiovascular events with parecoxib/valdecoxib: a systematic review and meta-analysis. N Z Med J. 2005;118(1226):U1755.
42. Caldwell B, Aldington S, Weatherall M, Shirtcliffe P, Beasley R. Risk of cardiovascular events and celecoxib: a systematic review and meta-analysis. J R Soc Med. 2006;99(3):132–140. doi:10.1177/014107680609900315
43. Towheed T, Maxwell L, Judd M, Catton M, Hochberg MC, Wells GA. Acetaminophen for osteoarthritis. Cochrane Database Syst Rev. 2006;(1):CD004257. doi: 10.1002/14651858.CD004257.pub2
44. Hernández-Díaz S, Varas-Lorenzo C, García Rodríguez LA. Non-steroidal antiinflammatory drugs and the risk of acute myocardial infarction. Basic Clin Pharmacol Toxicol. 2006;98(3):266–274. doi:10.1111/j.1742-7843.2006.pto_302.x
45. Gore M, Sadosky A, Leslie D, Tai K-S, Seleznick M. Patterns of therapy switching, augmentation, and discontinuation after initiation of treatment with select medications in patients with osteoarthritis. Clin Ther. 2011;33(12):1914–1931. doi:10.1016/j.clinthera.2011.10.019
46. Balmaceda CM. Evolving guidelines in the use of topical nonsteroidal anti-inflammatory drugs in the treatment of osteoarthritis. BMC Musculoskelet Disord. 2014;15(1):27. doi:10.1186/1471-2474-15-27
47. Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain. 2004;112(3):372–380. doi:10.1016/j.pain.2004.09.019
Supplementary materials
 | Table S1 Pain drug classes examined in this study |
 | Table S2 Patients excluded from the CLBP cohort |
 | Table S3 Surgery for OA patients |
 | Table S4 Pain drug classes prescribed to patients with and without weak opioid prescription |
 | Table S5 Baseline clinical characteristics of overall patients with and without weak opioid prescription |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

