Back to Journals » Patient Preference and Adherence » Volume 17
Patients’ Use of a Standardized Medication List - A Mixed Methods Study
Authors Eickhoff C , Müller U , Thomas S, Schmidt C , Hartling LS, Michael S, Schulz M , Bertsche T
Received 22 June 2023
Accepted for publication 19 September 2023
Published 30 October 2023 Volume 2023:17 Pages 2655—2666
DOI https://doi.org/10.2147/PPA.S427192
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Qizhi (Cathy) Yao
Christiane Eickhoff,1 Uta Müller,1 Sophie Thomas,2 Christian Schmidt,2 Lisa Sophie Hartling,3 Sebastian Michael,3,4 Martin Schulz,1,5 Thilo Bertsche2,6
1Department of Medicine, ABDA – Federal Union of German Associations of Pharmacists, Berlin, Germany; 2Clinical Pharmacy Department, Institute of Pharmacy, Medical Faculty, Leipzig University, Leipzig, Germany; 3Löwen-Apotheke Waldheim e.K, Waldheim, Germany; 4Saxon Pharmacists Association, Leipzig, Germany; 5Institute of Pharmacy, Freie Universität Berlin, Berlin, Germany; 6Drug Safety Center, Medical Faculty, Leipzig University and Leipzig University Hospital, Leipzig, Germany
Correspondence: Christiane Eickhoff, Department of Medicine, ABDA – Federal Union of German Associations of Pharmacists, Heidestrasse 7, Berlin, 10557, Germany, Tel +49 30 40004-529, Fax +49 30 40004-513, Email [email protected]
Purpose: A medication list (ML) is a document listing the patient’s entire medication, instructions for use, and indications. In Germany, a national standard was established in 2016 by law. However, data on patients’ use of this standardized ML are scarce. We investigated (i) patients’ practical use of the ML, (ii) patients’ understanding of the ML, (iii) completeness and correctness of the current ML version, and (iv) reasons why patients did not adhere to their ML.
Patients and Methods: Community pharmacists recruited patients possessing a standardized ML with ≥ 5 medications. Information sources to evaluate the ML were: (a) brown bag analysis, (b) practical demonstration, (c) patient interview, and (d) patient file. Data were analyzed using qualitative and quantitative methods.
Results: Two hundred and eighty-eight patients (median age: 76 years, range: 27– 95) were enrolled. (i) 38.5% of the patients used their ML regularly to prepare their medication and 73.3% to inform their physician. (ii) Overall, patients’ understanding of the ML was good, with > 80% of the patients being able to identify all relevant information. (iii) While n = 2779 medications were actually taken, n = 2539 were documented on the ML. No ML was fully correct and complete. Regarding particularly relevant items, ie, active ingredient, strength, dosage, medication missing or listed but not taken, 79.2% of ML were incorrect or incomplete. Handwritten modifications on the ML were frequent. (iv) Almost 60% of all patients did not follow their ML with “fear of adverse drug reactions” being the most frequently (n = 50) mentioned reason.
Conclusion: Completeness and correctness of the current ML version was poor with handwritten modifications being frequent. Additionally, most of the patients did not adhere to their ML. This indicates that measures that lead to correct and up-to-date ML and improvements in patient counseling about their medication should be developed and implemented into routine practice.
Keywords: medication list, medication schedule, medication plan, community pharmacy, medication safety, polypharmacy
Introduction
New therapeutic options and an ageing population with multimorbidity have resulted in ever more complex medication regimes and an increasing frequency of polypharmacy, most often defined as concurrent pharmacotherapy with at least 5 prescribed medications.1 A medication list (ML) is a written document listing the patient’s entire medication, prescribed as well as self-medication, including indications and instructions for use.2 Other terms used are medication schedule,3 medication plan,4,5 or medication chart.6 These documents aim to facilitate the taking of multiple drugs as agreed with the healthcare professionals (HCP). A ML not only informs the patients but also other HCP (eg, general practitioners (GP), medical specialists, nurses, pharmacists, dentists), thereby improving inadequate communication across care interfaces.3,7 ML has been identified as a relevant factor for patient safety.8,9 Additionally, it has been shown that further information, especially on drug handling, helps to improve patient knowledge about medication compared to control groups receiving only standard information.10,11 ML has, therefore, been used for many years and is often created by the patients themselves.12
In several countries, it has been discussed on how to generate an overview on the current medication in addition to developing systems to share such information between the HCP electronically, eg, in joint databases across care levels.11–16
In Germany, there is no central electronic database with patients’ data, prescribed drugs, or medical records, although electronic documentation is common across all sectors and a digital strategy in health care was recently published.17 Nevertheless, it is generally recognized that patients need written information on their medication. This was the main reason why the legislator introduced a federal standard of a ML already in 2016 including information on the active ingredient, trade name, strength, dosage form, dosage regimen, administration information, and the medical indication of each medication on the ML (an example for a ML is shown in supplementary information, Figure S1).4 Since then, all ambulatory patients insured with the Statutory Health Insurance (SHI) system, covering 88% of the population, ie, approximately 74.3 million people, and taking at least three prescribed medications for at least 28 days are entitled to receive such a ML.18 This ML is initially issued by the patients’ GP upon patients’ request. The ML can be updated by all medical specialists, hospitals, and community pharmacists, if requested by the patient, although the processes and the responsibilities have not been defined specifically. Currently, a paper-based version of the ML is printed out for the patient. An additional electronic copy is still optional.
Despite the assumed advantages of such a ML, the benefits under routine conditions remain to be proven. Although studies5,17 have already been carried out on the practical applicability of this ML standard, these were rather theoretical in nature, using a mock-up of a ML and therefore cannot be used to evaluate the ML in practice. Nevertheless, it was shown that especially patients at older age, with cognitive impairment, or having a lower educational status faced challenges in understanding a ML.19 Additionally, studies have been performed showing that ML containing errors and discrepancies are frequent.20–22 However, further aspects limiting the practical use of a standardized ML especially from the patients’ perspective are pending. In this respect, reasons for the lack of adherence to the information delivered by the ML are missing.
We, therefore, investigated (i) patients’ practical use of the ML, (ii) patients’ understanding of the ML, (iii) completeness and correctness of the current ML version, and (iv) reasons why patients did not adhere to their ML.
Materials and Methods
Study Design and Setting
We conducted a cross-sectional survey enrolling consecutive patients with a standardized medication list (ML) from May to October 2021 in community pharmacies in the German federal state of Saxony.
Enrolled Patients
Inclusion criteria were defined as: ≥18 years old, living at home, possessing a standardized ML with ≥5 medications, understanding and speaking German, and having given written informed consent. Patients were excluded if they were cared for by a nursing service or participated in the interprofessional medication management program ARMIN, in which ML was created jointly by community pharmacists and GP and therefore represented particularly structurally optimized processes that go beyond the usual procedure in everyday primary care.23
To include a convenience sample of at least 200 patients we aimed to invite 20 community pharmacies to participate. The community pharmacies were approached by the Saxon Pharmacist Association (SAV). Patients were recruited by the pharmacies. If patients fulfilled the inclusion criteria and were willing to participate, a meeting was scheduled in the pharmacy to conduct an interview. Patients were requested to bring their current ML as well as their entire medication including over-the-counter (OTC) drugs.
Data Collection
The following information sources were used to evaluate the ML and the currently taken medication. All data was collected by two pharmacy interns (CS and ST):
- Brown bag analysis: Patients brought along their entire current medication.
- Practical demonstration: Patients were observed in the pharmacy while preparing their medication for use by filling weekly pill boxes according to the information given on the ML.
- Patient interview: A pharmacy intern asked patients about all currently taken medications. The interview used two questionnaires and was performed in the pharmacy or at patient’s home.
- Patient file: The medication profile of the patient file in the pharmacy containing the currently prescribed medication and OTC drugs.
Questionnaire-Based Patient Interview
The information given by the patients in the interview was documented on two paper-based questionnaires (available upon request from the corresponding author). Both questionnaires were assessed for face validity and a cognitive pretest was performed with 4 patients (not enrolled in the main study). This resulted in wording clarification. No significant changes were made to the survey and monitoring as a result to the pretest.
The first questionnaire consisted of 23 items on sociodemographic data, overall health condition, organization of the medication intake, medical aids used, handling problems with the medication, use of OTC products, use of and opinions on the ML.
With the second questionnaire, patients’ understanding of the ML was assessed in two sections:
Patients’ Orientation on the Medication List and Understanding the 10 Structural Elements
General information (patient’s name, GP’s name that issued the ML, date of issue, and QR-code, an element allowing HCP to scan the ML and process the information from the ML in their local software systems) as well as information on each medication listed on the ML (active ingredient, product name, dosage, instructions for administration, medical indication), and if applicable, subheadings. Subheadings are optional elements on the ML inserted by HCP in order to structure the listed medications into different sets, eg, long-term medication vs medication as needed (see supplementary information, Figure S1).
Understanding the Information on the Medication List
This was assessed either by an oral explanation by the patient of how he/she administered the medication (including dosage and if applicable instructions for use) or by a practical demonstration by filling the mediation into compartments of a pill box (morning, noon, afternoon, and at bedtime) for two consecutive days.
Data Analyses
Statistical analyses were conducted using ExcelTM 2019 for Windows and SPSSTM, Version 25. Descriptive data are presented as sums, medians, means, and range. Associations between patients’ orientation on and understanding of their ML versus patients‘age and educational degree were evaluated with the Kruskal Wallis test. Associations between age of the ML (days since print out) versus completeness and correctness were evaluated using the Mann–Whitney U-test. A p-value of <0.05 indicated statistical significance.
Completeness and correctness of the medication on the ML were assessed for each medication of the patients’ schedule for the following items: active ingredient, product name, strength, dosage, indication, medications listed on the ML. It was checked whether the medication was no longer taken or was missing from the ML. Furthermore, instructions for administration were assessed if clinically relevant; this was defined as the following active ingredients: L-thyroxine, iron, pantoprazole, omeprazole, esomeprazole, alendronic acid, risedronic acid, lercanidipine, and methotrexate.
Completeness and correctness were evaluated by comparing the information on the current ML, which the patient presented during the interview, with the actual medications taken by the patient. The latter was assessed by the questionnaire-based patient interview. Additional information sources (as described above) were considered, if available, to assess the actual medication, ie, brown bag analysis, practical demonstration, and patient file.
After assessing completeness and correctness of the ML, patients were asked if they deliberately deviated from the corrected ML which was produced at the end of the assessment, and then scored as the basis for accuracy. These deviations were evaluated quantitatively. Additionally, all reasons given for not taking their medication as stated on the corrected ML were documented and analyzed with a qualitative conceptual, deductive content analysis.24 Data were first analyzed by one researcher not involved in the interviews (CS or ST) in the following steps: sorting, paraphrasing, generalizing, and reducing the phrases to categories. The initial categories were discussed with two other investigators (CE and CS or ST) and nine categories were decided upon. Data were then analyzed separately by two investigators (CS and ST). Deviations were discussed until consensus was reached. All data were checked for plausibility.
Results
Patient Characteristics
The characteristics of the 288 patients enrolled by 21 community pharmacies are shown in Table 1. Patients had a median age of 76 years and 57.6% were female. Whereas a median number of 8 medications were recorded on the ML, a median number of 9 medications were actually taken by the patients.
 |
Table 1 Patients‘Characteristics (N = 288) |
One hundred and sixteen patients (40.3%) were not willing to participate in the practical demonstration (b), and for 94 patients (32.6%), besides the ML, only the patient interview (c) was available for evaluation. For the majority of those patients (n = 86, 91.5%) a patient file (d) with the patient’s medication was available additionally. Since these groups did not differ significantly in all relevant variables (data not shown), we decided not to differentiate those subgroups for which not all information sources were available in the analyses. For 78 patients (27.1%) all information sources (a) to (d) were available.
Patients’ Practical Use of the Medication List
Most patients (n = 211; 73.3%) used their ML to inform their medical specialists about their medication. Furthermore, the ML was used at hospital admissions (n = 190; 66.0%), when travelling (n = 142; 49.3%), and when visiting a community pharmacy (n = 6; 2.1%). While most patients (n = 242; 84.0%) indicated purchasing OTC products in the pharmacy, only 50.3% (n = 145) informed their GP or specialist about this. 38.5% of the patients used their ML regularly to prepare their daily/weekly medication for use, eg, in a pill box.
Patients’ Understanding of the Medication List
Nearly all patients (99.7%) correctly understood the different structural elements of the ML (Figure 1). The subheadings were the only optional structural elements inserted on the ML by HCP if needed and subheadings existed on 38 ML; of these, 35.7% (n = 10) were identified by the patients.
 |
Figure 1 Patients‘orientation on their medication list (N = 288). Notes: *Percentage relates to the number of medication lists with subheadings (n = 38). |
Concerning the comprehensibility of the structural elements of the ML (Figure 2), the results were comparable with up to 97.5% of correct patients’ answers, with the two categories subheadings as well as the QR code least understood with 39.3% and 27.4%.
 |
Figure 2 Comprehensibility of the structural elements of the medication list (N = 288). Notes: *Percentage relates to the number of medication lists with subheadings (n = 38). |
Patients’ orientation on the ML as well as the understanding of the structural elements were associated with age and educational level being significantly lower in older patients and in patients with a lower educational degree (both p < 0.01). No significant association was found with sex, number of medications on the ML or taken, or the living situation.
Completeness and Correctness of the Current Medication List
A total of 2539 medications were printed on the ML with 2779 medications actually taken by the 288 patients. During the interviews, 70 patients (24.3%) indicated 102 medications listed on the ML that were not taken any more and 122 patients (42.4%) stated taking additional medications (n = 264) that were not listed on the ML. On the ML of 44 patients (15.3%) medications (n = 88) had been added by hand. Table 2 summarizes all evaluated items. None of the evaluated ML was fully complete and correct. When only taking the most relevant items into account, ie, active ingredient, strength, dosage, medication missing or listed but not taken any more, 79.2% (n = 228) of the patients had an incorrect or incomplete ML. None of those items were associated with the time the ML had been printed out.
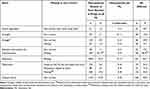 |
Table 2 Completeness and Correctness of 288 Medication Lists (ML) Documenting 2539 Medications |
Table 3 provides an overview on the therapeutic indications, with cardiovascular drugs being the most common. Drug classes often documented on the ML but not taken any more were analgesics (8.2%, n = 19) and antacids (11.2%; n = 15). Medications missing on the ML were often related to self-medication: This was most frequently observed for eye drops (47.9%), followed by minerals (42.4%), vitamins (31.0%), analgesics (21.6%), and antidepressants/hypnotics/sedatives (20.5%).
 |
Table 3 Therapeutic Indications of Medications Taken, Medications Documented on the Medication List but not Taken and Medication Missing on the Medication List (N = 288 Patients) |
Three hundred and forty-one handwritten modifications (described in Table 4) related to 156 medications (6.1% of all medications on the ML) were observed on 99 ML (34.4%). The most common handwritten change was an added drug (n = 88).
 |
Table 4 Number and Type of Handwritten Modifications on 288 Medication Lists |
Most of the 99 ML with handwritten modifications were amended by the patients themselves (84%) and less often by the GP (12%). In four cases, the pharmacist or the GP were involved. The median time since creation of ML with handwritten amendments (189 days since print-out) differed significantly from ML without any handwritten amendment (46 days; p < 0.001). No associations were found between any of the items concerning correctness and completeness of the ML (Table 2) and time since ML creation.
Reasons Why Patients Did Not Adhere to Their Medication List
One hundred and sixty-nine patients (58.6%) indicated reasons other than missing or incorrect information on the ML for not taking their medication as stated on the ML. This affected 309 medications (12.2%) of all medications printed on the ML (n = 2539). Most often, these were deviations from the individual dose (n = 89; 28.8%), the number of daily doses (n = 88; 28.5%), administration time (n = 62; 20.1%), intake with respect to meals (n = 39; 12.6%), and duration of intake (n = 31; 10.0%).
The top five medications with the most frequent intentional deviations from the ML were: Parkinson disease medication (ATC-Code: N04) with 25.6%, antacids (A02) with 21.1%, antidepressants/hypnotics/sedatives (N05/N06) with 17.3%, analgesics (N02) with 14.7%, and thyroid hormones (H03) with 14.0%.
Of the 169 patients that reported deliberate deviations from their ML, 117 reported a total of 151 explanations and reasons for their deviations. The results of this analysis with its themes, frequencies, and patient quotes are summarized in Table 5. The most frequent reason for patients’ intentional deviations from the ML was fear for adverse drug reactions which accounted for one-third (n = 50) of all reasons, followed by insufficient communication (n = 37) and increasing or persisting symptoms (n = 28).
 |
Table 5 Patients’ Concerns and Reasons for Deviating from Their Medication List (n = 151 Concerns and Reasons Reported by n = 117 Patients) |
Discussion
The main finding of our study is that none of the 288 ML was complete, correct and up to date. Handwritten modifications were common, and almost 60% of the patients did not adhere to their ML for various reasons, mainly for fear of adverse drug reactions.
Patients’ Practical Use and Understanding of the Medication List
For the first time, patients’ orientation and understanding regarding their own standardized ML were assessed under routine conditions in Germany. It was found that 1 in 3 patients regularly used their ML to prepare their medications and 3 in 4 patients used it to inform their medical specialists.
A particularly important criterion for the usability of the ML is the competence of patients to find their way around it. Patients indicated the structural elements of their own ML and additionally explained the respective meanings. Most structural elements of the ML were identified and explained correctly by more than 90% of the patients, including relevant information such as the dosage. Just above 80% of the patients understood where instructions for administration are to be found.
A two-dimensional QR code is printed on the ML, which enables the ML to be read in automatically. However, according to our survey, the patients knew little about the QR code. This code enables HCP to electronically process the information quickly and effectively in their software system. While patients do not need to be familiar with the technical details, they should of course be aware of the opportunities that arise to their benefit.
A comparison with the data of Botermann et al5,19,25 is of particular interest. These studies assessed the comprehensibility of a mock-up ML presenting six different drugs in the standardized format. As in our study with real ML, patients were asked to identify the information on the ML. Comparably, results were obtained for patients’ orientation on the ML. This leads to the conclusion that patients are in general competent in finding relevant information on their ML. Nevertheless, not all patients demonstrated sufficient understanding and a significant, albeit moderate correlation was found between understanding the ML with the level of education (r = 0.45) and as well with patients’ age (r=−0.46); additionally, cognitive impairment was identified as a relevant factor.25 Our findings support these recommendations that HCP have to consider that a ML alone is not sufficient for all patients and additional counselling tailored to the patients’ individual needs might be required to ensure a correct administration of medication.
Completeness and Correctness of the Current Medication List
None of the 288 ML was complete and up to date. Handwritten modifications, mainly added by the patients themselves, were frequently found. Considering only the most relevant items for patient safety, only 1 in 5 ML was correct. Of concern, patients reported a median of one additional drug taken but not documented on their ML. Self-medication was frequently not added. As a conclusion, HCP should consider that OTC drugs should also be documented on the ML, since it should be a comprehensive list of all medications taken by the patient. Furthermore, drugs were documented on the ML that were no longer taken. This is in line with other studies: Waltering et al21 found that dosage was missing in 35% of medications, while indication was missing in 95% and intake recommendation was missing in 97%. Dormann et al20 showed that only 36% of the medication documented on the ML was in line with the medications presently taken by the patients. Müller et al reported 166 medication discrepancies for 774 listed medications.26
Missing, incorrect, or outdated information on the ML might explain the high prevalence of handwritten modifications. Since we did not see an increase in deviations in terms of completeness and correctness with increasing time since the ML had been created and printed out, it is doubtful that these ML were complete and correct at the time of issue. One approach to obtain an overview of the complete medication is a brown bag medication review as done in the German interprofessional medication management program ARMIN, for example.23 In this program, GP and community pharmacists jointly compiled the information on the entire patients’ medication starting with a brown bag review in the community pharmacy. They also agreed on a structured process and defined responsibilities on how to regularly update the ML when medication changes occur.27 Two other studies evaluating the implementation of the ML found similar findings and jointly published their recommendations for the implementation of ML.21 It was also emphasized that the ML should be best updated electronically as already established in some settings.28,29 Implementing a digital infrastructure that can be assessed by different professions in the healthcare system in order to assess medication data electronically may result in less discrepancies.13,14
Reasons Why Patients Did Not Adhere to Their Medication List
Especially for patients on multiple medications, reconciliation of the ML is a tool to identify drug-related issues based on discrepancies.2 However, while it is described in the literature30 that the number of correct ML without discrepancies is with 22% low in principle, little is known so far about why patients intentionally deviate from their ML; in our study almost 60% of all patients. This aspect does not necessarily refer to medication non-adherence as patients might be fully adherent to their own list. Not all deviations on ML are due to knowledge deficits which are to be prevented by pharmaceutical consultation to a particularly high degree.31 As recently reported,32 general medication beliefs do not seem to be crucial for a decision to use a ML but other influential factors, such as individual benefits and barriers and socio-psychological factors are more important in this respect.
As reported by others,33 the most common reason for non-adherence is forgetfulness but concerns about the long-term effects of the medication are also significant.
This is in line with the results shown in this study that fear for adverse drug reactions and symptoms that persist or increase were reasons most often indicated by patients indicating that both are justified concerns in the need of careful management by a HCP since patients might otherwise not follow their ML. Adjustment of medication intake to the daily routine is another reason that was given frequently, potentially improving medication adherence and outcomes.34 Patients deliberately disregarded some GP recommendations,35 as shown, for example, by surveys in the treatment of statin side effects. Clinicians should have this in mind when handing out a ML and address this topic during patient encounters.
Only if the extent and the reasons for deliberate deviations are known, HCP may find solutions together with the patient, ie, shared decision-making. Communication problems with HCP were another reason frequently mentioned by patients for deviating from their ML.
Limitations
Firstly, the study was performed only in 21 community pharmacies in one federal state. Statements on generalizability should, therefore, be made with caution. Secondly, not all patients invited were willing to participate. It can be assumed that the study cohort represents better-informed patients. It is therefore likely that a survey of routine patients outside of those who participated voluntarily in this study would have led to even more negative results in terms of information deficits. Thirdly, at the time of our study, the medication management project ARMIN was implemented in the states of Saxony and Thuringia. We cannot fully exclude that the patients in our study, although not enrolled in ARMIN, still benefited from the general increase in knowledge and optimization of processes in the participating pharmacies, also regarding the quality of the ML. Additionally, the data from two of the four sources (brown bag and practical demonstration) were not available for all patients. However, these subgroups did not differ significantly on all relevant variables, so the available sources are assumed to be representative.
Conclusions
Although standardized medication lists (ML) in primary care are understandable to the majority of patients, they are neither complete nor correct nor up to date. One may conclude: “Never take a ML for granted”. Therefore, a structured process with defined responsibilities on generating and updating ML is needed. This should be a joint task for all HCP, in particular GP, medical specialists, hospitals, and pharmacists. Furthermore, a digital infrastructure (in the sense of electronically based, fast, and secure communication between physicians and all other players in the healthcare system of all medical information needed for the treatment of patients) is required to update the ML at all levels of the medication process beginning with prescribing and not ending at dispensing.
Additionally, the patient’s perspective with his or her knowledge, beliefs, and limitations as potential reasons for deviations including non-adherence needs to be known and considered.
Abbreviations
CP, community pharmacy; GP, general practitioner; HCP, healthcare professional; ML, medication list; OTC, over-the-counter.
Data Sharing Statement
The data can be requested for scientific questions from the corresponding author.
Ethics Approval and Informed Consent
The study was approved by the local ethics committee of the Leipzig University (127/20-ek from May 4th, 2020). Written informed consent was obtained from all participating patients.
Acknowledgments
We would like to thank all pharmacists involved, especially Claudia Sehmisch (“Albert Schweitzer” Pharmacy, Leipzig) and Heike Senf (“Sonnen” Pharmacy, Leipzig) for their active support in planning and implementing this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The project was funded in part by grants from the ABDA – Federal Union of German Associations of Pharmacists, Berlin, and the Saxon Pharmacists Association (SAV), Leipzig.
Disclosure
All authors declare to have no conflicts of interest in regard to this study.
References
1. Masnoon N, Shakib S, Kalisch-Ellett L, et al. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. doi:10.1186/s12877-017-0621-2
2. Van der Nat DJ, Taks M, Huiskes VJB, van den Bemt BJF, van Ozenoort HAW. Risk factors for clinically relevant deviations in patients’ medication lists reported by patients in personal health records: a prospective cohort study in a hospital setting. Int J Clin Pharm. 2022;44(2):539–547. doi:10.1007/s11096-022-01376-w
3. Kenning C, Protheroe J, Gray N, et al. The potential for using a universal medication schedule (UMS) to improve adherence in patients taking multiple medications in the UK: a qualitative evaluation. BMC Health Serv Res. 2015;15(1):94. doi:10.1186/s12913-015-0749-8
4. Kassenärztliche Bundesvereinigung [National Association of Statutory Health Insurance Physicians]. The standardized medication plan. [based on: “Vereinbarung eines bundeseinheitlichen Medikationsplans – BMP”. Available from: https://www.kbv.de/html/medikationsplan.php.
5. Botermann L, Krueger K, Eickhoff C, Kloft C, Schulz M. Patients’ handling of a standardized medication plan: a pilot study and method development. Patient Prefer Adherence. 2016;22(10):621–630. doi:10.2147/PPA.S96431
6. Dietrich FM, Hersberger KE, Arnet I. Benefits of medication charts provided at transitions of care: a narrative systematic review. BMJ Open. 2020;10(10):e037668. doi:10.1136/bmjopen-2020-037668
7. The Joint Commission. “What did the doctor say?:” Improving health literacy to protect patient safety; 2007. Available from: https://psnet.ahrq.gov/issue/what-did-doctor-say-improving-health-literacy-protectpatient-safety.
8. Wenger NS, Young RT. Quality indicators for continuity and coordination of care in vulnerable elders. J Am Geriatr Soc. 2007;55(Suppl 2):S285–S292. doi:10.1111/j.1532-5415.2007.01334.x
9. Kuske S, Lessing C, Lux R, Schmitz A, Schrappe M. Patientensicherheitsindikatoren zur Arzneimitteltherapiesicherheit (AMTS-PSI): internationaler Status, Übertragbarkeit und Validierung [Patient safety indicators for medication safety (AMTS-PSI): international status, transferability and validation]. Gesundheitswesen. 2012;74(2):79–86. doi:10.1055/s-0030-1269838
10. Send AF, Peters-Klimm F, Bruckner T, Haefeli WE, Seidling HM. A randomized controlled trial to assess the effect of a medication plan containing drug administration recommendations on patients’ drug knowledge after 2 months. J Clin Pharm Ther. 2017;42(1):69–74. doi:10.1111/jcpt.12476
11. Send AF, Schwab M, Gauss A, Rudofsky G, Haefeli WE, Seidling HM. Pilot study to assess the influence of an enhanced medication plan on patient knowledge at hospital discharge. Eur J Clin Pharmacol. 2014;70(10):1243–1250. doi:10.1007/s00228-014-1723-9
12. Freigofas J, Seidling HM, Quinzler R, et al. Characteristics of medication schedules used by elderly ambulatory patients. Eur J Clin Pharmacol. 2015;71(9):1109–1120. doi:10.1007/s00228-015-1888-x
13. Josendal AV, Bergmo TS, Granas AG. Implementation of a shared medication list in primary care – a controlled pre-post study of medication discrepancies. BMC Health Serv Res. 2021;21(1):1335–1343. doi:10.1186/s12913-021-07346-8
14. Claeys C, Foulon V, de Winter S, Spinewine A. Initiatives promoting seamless care in medication management: an international review of the grey literature. Int J Clin Pharm. 2013;35(6):1040–1052. doi:10.1007/s11096-013-9844-2
15. Uitvlugt EB, van den Bemt BJF, Chung WL, Dik J, van den Bemt PMLA, Karapinar-çarkit F. Validity of a nationwide medication record system in the Netherlands. Int J Clin Pharm. 2019;41(3):687–690. doi:10.1007/s11096-019-00839-x
16. Grimes T, Fitzsimons M, Galvin M, Delaney T. Relative accuracy and availability of an Irish National Database of dispensed medication as a source of medication history information: observational study and retrospective record analysis. J Clin Pharm Ther. 2013;38(3):219–224. doi:10.1111/jcpt.12036
17. Bundesministerium für Gesundheit [Federal Ministry of Health]. Gemeinsam digital: Digitalisierungstrategie für das Gesundheitswesen und die Pflege [jointly digital: digitization strategy for the health care system and nursing]. Available from: https://www.bundesgesundheitsministerium.de/themen/digitalisierung/digitalisierungsstrategie.html.
18. Law for secure digital communication and applications in the health care system. E-Health act. Available from: https://www.bgbl.de/xaver/bgbl/start.xav?startbk=Bundesanzeiger_BGBl&start=//*[@attr_id=%27bgbl115s2408.pdf%27]#__bgbl__%2F%2F*%5B%40attr_id%3D%27bgbl115s2408.pdf%27%5D__1601463267910.
19. Botermann L, Wachter A, Monzel K, et al. Do patients with diabetes type 2 or chronic heart failure understand a medication plan? Pharmazie. 2017;72(12):764–768.
20. Dormann H, Maas R, Eickhoff C, et al. The federal standard medication plan in routine care [Der bundeseinheitliche Medikationsplan in der Praxis]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018;61(9):1093–1102. doi:10.1007/s00103-018-2789-9
21. Waltering I, Schwalbe O, Hempel G. Informationsgehalt von Medikationsplänen vor dem Hintergrund der Einführung des einheitlichen patientenbezogenen Medikationsplans [information content of medication schedules prior to the implementation of the federal standard medication plan]. Z Evid Fortbild Qual Gesundhwes. 2016;115-116:24–32. doi:10.1016/j.zefq.2016.06.004
22. Amelung S, Bender B, Meid A, et al. Wie vollständig ist der bundeseinheitliche Medikationsplan? Eine Analyse bei Krankenhausaufnahme [How complete is the Germany-wide standardised medication list (“Bundeseinheitlicher Medikationsplan”)? An analysis at hospital admission]. Dtsch Med Wochenschr. 2020;145(21):e116–e122. doi:10.1055/a-1212-2836
23. Meid AD, Wirbka L, Moecker R, et al. Mortality and hospitalizations among patients enrolled in an interprofessional medication management program. Results of the Medicines Initiative Saxony–Thuringia (Arzneimittelinitiative Sachsen-Thüringen, ARMIN). Dtsch Arztebl Int. 2023;120(15):253–260. doi:10.3238/arztebl.m2023.0014
24. Mayring P. Qualitative content analysis. Forum Qual Soc Res. 2000;1(2, Art. 20):1–10.
25. Botermann L, Monzel K, Krueger K, et al. Evaluating patients‘comprehensibility of a standardized medication plan. Eur J Clin Pharmacol. 2016;72(10):1229–1237. doi:10.1007/s00228-016-2082-5
26. Mueller MA, Opitz R, Grandt D, Lehr T. The federal standard medication plan in practice: an observational cross-sectional study on prevalence and quality. Res Social Adm Pharm. 2020;16(10):1370–1378. doi:10.1016/j.sapharm.2020.01.013
27. Moecker R, Weissenborn M, Klingenberg A, et al. Task sharing in an interprofessional medication management program - a survey of general practitioners and community pharmacists. BMC Health Serv Res. 2022;22(1):1005–1014. doi:10.1186/s12913-022-08378-4
28. Jurado C, Calmels V, Lobinet E, et al. The electronic pharmaceutical record: a new method for medication reconciliation. J Eval Clin Pract. 2018;24(4):681–687. doi:10.1111/jep.12942
29. Bugnon B, Geissbuhler A, Bischoff T, Bonnabry P, von Plessen C. Improving primary care medication processes by using shared electronic medication plans in Switzerland: lessons learned from a participatory action research study. JMIR Form Res. 2021;5(1):e22319. doi:10.2196/22319
30. Wolf O, Åberg H, Tornberg U, Jonsson KB. Do orthogeriatric inpatients have a correct medication list? A pharmacist-led assessment of 254 patients in a Swedish university hospital. Geriatr Orthop Surg Rehabil. 2016;7(1):18–22. doi:10.1177/2151458515625295
31. Zimmer J, Niemann D, Seltmann K, et al. Managing of oral medicines in paediatric oncology: can a handbook and a pharmaceutical counselling intervention for patients and their parents prevent knowledge deficits? A pilot study. Eur J Hosp Pharm. 2016;23(2):100–105. doi:10.1136/ejhpharm-2015-000716
32. Straßner C, Mahler C, Strauß B, et al. Medication beliefs and use of medication lists - is there a connection? Results from a before-and-after study in Germany. BMC Geriatr. 2020;20(1):116. doi:10.1186/s12877-020-01513-y
33. Unni EJ, Gupta S, Sternbach N. Trends of self-reported non-adherence among type 2 diabetes medication users in the United States across three years using the self-reported medication adherence reasons scale. Nutr Metab Cardiovasc Dis. 2022;32(1):151–159. doi:10.1016/j.numecd.2021.09.018
34. Laufs U, Böhm M, Kroemer HK, Schüssel K, Griese N, Schulz M. Strategies to improve medication adherence [Strategien zu Verbesserung der Einnahmetreue von Medikamenten]. Dtsch Med Wochenschr. 2011;136(31–32):1616–1621. doi:10.1055/s-0031-1281566
35. Izuka NJ, Alexander MAW, Balasooriya-Smeekens C, Mant J, De Simoni A. How do stroke survivors and their carers use practitioners’ advice on secondary prevention medications? Qualitative study of an online forum. Fam Pract. 2017;34(5):612–620. doi:10.1093/fampra/cmx023
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
