Back to Journals » Patient Preference and Adherence » Volume 16
Patients’ Preference Between DPP4i and SGLT2i for Type 2 Diabetes Treatment: A Cross-Sectional Evaluation
Authors Costa Gil JE , Garnica Cuéllar JC , Perez Terns P, Ferreira-Hermosillo A , Cetina Canto JA , Garduño Perez ÁA, Mendoza Martínez P, Rista L, Sosa-Caballero A, Vázquez-Mendez E, Tejado Gallegos LF, Chen H, Elizalde A, Tomatis VB
Received 19 January 2022
Accepted for publication 6 April 2022
Published 9 May 2022 Volume 2022:16 Pages 1201—1211
DOI https://doi.org/10.2147/PPA.S355638
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
José Esteban Costa Gil,1 Juan Carlos Garnica Cuéllar,2 Paula Perez Terns,3 Aldo Ferreira-Hermosillo,4 José Antonio Cetina Canto,5 Ángel Alfonso Garduño Perez,2 Pedro Mendoza Martínez,6 Lucas Rista,7 Alejandro Sosa-Caballero,6 Estefanía Vázquez-Mendez,8 Luis Fernando Tejado Gallegos,8 Hungta Chen,9 Agustina Elizalde,10 Virginia B Tomatis10
1Departamento de Endocrinología, Instituto de Cardiología La Plata, La Plata, Buenos Aires, Argentina; 2Departamento de Endocrinología del Centro Médico Nacional “ 20 de Noviembre”, ISSSTE, Ciudad de México, México; 3Dirección Médica, Cardiología Palermo - Centro de Investigaciones Clínicas, Buenos Aires, Argentina; 4Unidad de Investigación Médica en Enfermedades Endócrinas. Centro Médico Nacional Siglo XXI, IMSS, Ciudad de México, México; 5Hospital Regional ISSSTE, Mérida, Yucatán estado, México; 6Endocrinología, Hospital Angeles Lindavista, Ciudad de México, México; 7Diabetes, Innovación e Investigación, Centro de Diabetes y Nutrición - Investigaciones Clínicas (CEDyN), Rosario, Santa Fé, Argentina; 8Medical Affairs, AstraZeneca - México, Ciudad de México, México; 9Global Medical & Payer Evidence Statistics, AstraZeneca, Gaithersburg, Maryland, USA; 10Medical Affairs, AstraZeneca – South Cone, Buenos Aires, Argentina
Correspondence: José Esteban Costa Gil, Costa Gil Departamento de Endocrinología, Instituto de Cardiología La Plata, Calle 6, número 212, La Plata, 1900, Buenos Aires, Argentina, Tel +54 9 2214 20-7359, Email [email protected]
Purpose: Despite newer type 2 diabetes (T2D) medications, patients do not always achieve metabolic targets, remaining at risk for cardiorenal complications. Therapeutic decisions are generally made by the healthcare team without considering patients’ preferences. We aimed to evaluate patients’ T2D treatment preference in two Latin-American countries between two different oral medication profiles, one resembling dipeptidyl peptidase-4 inhibitors (DPP4i) and another resembling sodium-glucose cotransporter-2 inhibitors (SGLT2i).
Patients and Methods: In this cross-sectional, multicenter study from June to September 2020, patients with T2D from Argentina and Mexico (n = 390) completed a discrete choice experiment questionnaire to identify preferences between DPP4i (medication profile A) and SGLT2i (medication profile B). The reason behind patients’ choice, and the association between their baseline characteristics and their preference were evaluated using logistic regression methods.
Results: Most participants (88.2%) preferred SGLT2i’s profile. Participants with older age (p = 0.0346), overweight or obesity (p < 0.0001), high blood pressure (BP; p < 0.0001), high total cholesterol (p = 0.0360), and glycosylated hemoglobin (HbA1c) < 7% (p = 0.0001) were more likely to choose SGLT2i compared with DPP4i’s profile. The most and least important reasons to choose either drug profile were HbA1c reduction and genital infection risk, respectively. The likelihood of selecting the SGLT2i’s profile significantly increased in participants with increased body mass index (BMI; odds ratio [OR] = 8.9, 95% confidence interval [CI]: 3.5– 22.5, p < 0.05), high BP (OR = 4.9, 95% CI: 1.9– 12.4, p < 0.05), and lower education level (OR = 3.6, 95% CI: 1.0– 12.6, p < 0.05).
Conclusion: Latin-American patients with T2D preferred medication with a profile resembling SGLT2i over one resembling DPP4i as a treatment option. A patient-centered approach may aid the healthcare team in decision-making for improved outcomes.
Keywords: dipeptidyl peptidase-4 inhibitors, patient preference, sodium-glucose cotransporter-2 inhibitors, type 2 diabetes
Introduction
Type 2 diabetes (T2D) is a threat in low and middle-income countries.1 Latin-American (LatAm) countries have shown an accelerated increase in the number of patients with T2D, reaching nearly 32 million in 2021, with an expected rise to 49 million in 2045, if the current trend continues.2–5 This negatively impacts national healthcare systems in LatAm.6
Cardiorenal complications occur early in patients with T2D leading to disability and death.7,8 To achieve T2D targets, self-care behaviors with a healthy lifestyle and metformin are mostly recommended as first-line therapy.9–12 Dipeptidyl peptidase-4 inhibitors (DPP4i) may also be used in patients with poor glycemic control with metformin.13 International guidelines recommend the use of sodium-glucose cotransporter-2 inhibitors (SGLT2i) or glucagon-like peptide-1 receptor agonists (GLP-1 RA) as second-line treatment in patients with T2D with established cardiorenal complications, regardless of glycemic control, and as first-line treatment in drug naïve patients with high/very high cardiovascular (CV) risk.11–13
Compared with DPP4i, SGLT2i lower body weight (BW), slightly reduce systolic blood pressure (SBP), and provide marked cardiorenal protection, but are associated with increased risk of genital infections.11,14 Both DPP4i and SGLT2i are oral agents and may be more suitable than GLP-1 RA injectables due to improved adherence and health-related quality of life (QoL), as patients’ preferences depend on the route of administration, frequency, and complexity of treatment.15
Despite guidelines recommendations, the use of SGLT2i and GLP-1 RA in clinical and real-life studies is moderate compared with other established treatments.12,16,17 In “Diabetes en America Latina (DEAL)” the most frequently used T2D medications were biguanides (51%), sulfonylureas (SU; 36%) and their combination with other agents.18
Frequently, patients’ preferences are not sufficiently considered by the healthcare team, despite the knowledge that achieving treatment goals is largely dependent on compliance and adherence to treatment.19–21 The ADA, the EASD, and the Patient Protection and Affordable Care Act position statement encourages a patient-centered approach in T2D treatment and recommends considering patients’ preferences, needs, and values in healthcare decision-making. With patient engagement, it is believed that improvements in treatment adherence, overall healthcare quality, and safety will be achieved.18,22,23 However, in real life, therapeutic decisions are mostly managed by the healthcare team without considering patients’ preferences.
The present cross-sectional study aimed to evaluate the preference between DPP4i and SGLT2i’s profiles in LatAm patients with T2D.
Materials and Methods
Study Design
This was a cross-sectional, multicenter, observational study conducted in two LatAm countries from June to September 2020 in patients with T2D. It enrolled 390 participants from nine sites (Argentina: 3; Mexico: 6) to understand their preference between DPP4i and SGLT2i’s profiles. The study was conducted according to the Declaration of Helsinki, Good Clinical Practice guidelines, and local bioethics regulations and laws. All participants provided written informed consent.
Patient Population
All patients attending the sites’ outpatient department from June to September 2020 who met the inclusion/exclusion criteria were invited to participate in the study. Patients aged ≥18 years, diagnosed with T2D, and who willingly provided informed consent were included in the study. Patients were excluded if they were pregnant, had type 1 diabetes (T1D), gestational diabetes, and/or treatment with DPP4i and/or SGLT2i.
Data Collection
Each consented participant was provided a questionnaire for their completion. They had the option to complete it in paper format at the site or via teleconference at home (due to the COVID-19 pandemic situation), with a trained facilitator capturing their responses. Trained facilitators were available at each site to provide an overview and instructions for participants to complete the questionnaire, and to answer any questions from participants to facilitate its completion. All data from eligible participants who completed the questionnaire were included in the final analysis.
The questionnaire contained a set of instructions followed by a series of questions structured in the following sections:
Socio-Demographic and Clinical Characteristics
Socio-demographic data included age, gender, and the highest level of education. Clinical characteristics included height and weight (to calculate body mass index [BMI]), smoking, glycosylated hemoglobin (HbA1c), time since T2D diagnosis, current diabetes treatment – type and number of medications, diagnosis of hypertension or antihypertensive treatment, diagnosis of dyslipidemia or hypolipidemic treatment, and presence of other comorbidities (renal and CV).
Discrete Choice Experiment (DCE)
DCE is an accepted methodology to evaluate patients’ preferences in the presence of two or more possible treatment options. It provides patients the opportunity to grade the perceived relative importance of treatments, including parameters related to the route of administration, dosing frequency, and potential risk of side effects, among others.24 Based on previous patients’ preference surveys,20,24,25 DCE was used to evaluate patients’ preference by asking them to choose between two alternate treatment options which differed in their benefit-risk attributes (form of administration; effect on HbA1c; weight; risk of hospitalization for heart failure [hHF] and kidney disease; risk of adverse events [hypoglycemia and genital infections])17,26–29 and to rank the importance of the reasons for their decision. Following an introductory explanation, participants were presented with a comparative table displaying each oral agent’s profile identified with a different letter (medication A resembling a DPP4i’s profile and medication B resembling an SGLT2i’s profile; Supplementary Table 1) and asked to choose their preferred one (assuming that these were the only two treatment alternatives and their cost was similar). After participants reported their overall preference for medication A or B, they were asked to rank the importance of the following reasons for their preference (considering “1” to be the most important and “5” to be the least important reason): glycemic efficacy, BW loss, reduction of risk of hHF and kidney disease, and genital infection risk (Supplementary Table 2).
Data were anonymized and collected in an electronic case report form.
Sample Size Calculation and Statistical Analysis
A sample size of 390 participants was calculated to detect a difference of 10% between the two drug classes with power >90% at the 0.05 level, assuming the preference of DPP4i was 40% in a one-sample Chi-square test.
Patient- and treatment-based characteristics were summarized using descriptive statistics. Continuous and categorical variables were analyzed using Student’s t-test and Chi-square test, respectively. Continuous variables were presented as mean and standard deviations and categorical variables as frequencies and percentages. The number and percentage of participants were summarized with a 95% confidence interval (CI) by their overall drug profile choice and by each of the participants’ characteristics. The primary objective was achieved if the lower limit of the CI was >50%. Each of the reasons for which participants preferred one oral T2D agent profile over the other was summarized by medication group (DPP4i or SGLT2i). The association between patient-reported preferences and socio-demographic/clinical characteristics was evaluated using a logistic regression model, and corresponding odds ratio (OR) and 95% CI were reported. P-value < 0.05 was considered statistically significant. All analyses were performed using SAS® Version 9.4.
Results
Baseline Characteristics
A total of 390 eligible participants (Argentina, n = 147; Mexico, n = 243) completed the questionnaire from June to September 2020, and their data were included in the final analysis. The socio-demographic and clinical characteristics of the overall study participants by their choice of medication are presented in Tables 1 and 2.
 |
Table 1 Patients’ Self-Reported Socio-Demographic Characteristics - Overall and per Preferred Medication’s Profile |
 |
Table 2 Patients’ Self-Reported Clinical Characteristics - Overall and per Preferred Medication’s Profile |
More than half of the participants were women (53.1%), with the majority being overweight/obese (86.9%) and having completed high school/tertiary education (40.3%). An HbA1c level <7% was observed in 44.4% of the participants, more than half reported high BP (59.5%) and cholesterol (52.6%), and the majority had no history of cardiovascular disease (CVD; 82.1%), kidney problems (83.6%), or smoking habit (87.4%). Duration of T2D was of at least 10 years in 37.7% of participants, 60.0% reported baseline T2D treatment with oral medication, whereas 3.6% did not take medication. The most frequent baseline T2D medication was metformin (83.6%), followed by insulin (21.5%), SU (15.9%), and GLP-1 RA (4.6%).
Discrete Choice Experiment
Participants’ Baseline Characteristics and Choice of Medication
The majority of participants (n = 344, 88.2%, 95% CI: 84.6–91.2%) preferred SGLT2i, whereas 11.8% (n = 46) selected DPP4i as preferred T2D medication profile. The univariate analysis based on participants’ baseline characteristics (socio-demographic and clinical) by their choice of medication is presented in Tables 1 and 2.
Participants preferring SGLT2i’s profile were significantly older (58.0±12.5 vs 53.8±11.1 years, p = 0.0346) and overweight/obese (BMI ≥25 kg/m2; 90.1% vs 63.0%, p < 0.0001) compared with participants preferring DPP4i’s profile. A larger proportion of participants preferring SGLT2i’s profile reported having primary education/incomplete studies compared with those choosing DPP4i’s profile (33.4% vs 15.2%, p = 0.0204), and more participants choosing DPP4i’s profile had completed university/postgraduate studies (37.0% vs 20.6%). However, a similar proportion of participants from both groups reported completion of high school/tertiary education (DPP4i: 39.1%, SGLT2i: 40.4%). A significantly larger proportion of participants preferring SGLT2i’s profile reported high BP (64.5% vs 21.7%, p < 0.0001) and high cholesterol (54.9% vs 34.8%, p = 0.0360) compared with those preferring DPP4i's profile. More patients choosing SGLT2i’s profile reported HbA1c level <7% (46.8% vs 26.1%, p = 0.0001) and ≥7 (37.2% vs 32.6%, p = 0.0001), whereas 41.3% of participants preferring DPP4i’s profile were unaware of their HbA1c level. There was a trend towards significance in the duration of diabetes between the groups, with a larger proportion of participants choosing SGLT2i’s profile reporting diabetes for >5 years (65.1% vs 50.0%, p = 0.0560).
Approximately half of the participants were women in both groups (DPP4i: 52.2%, SGLT2i: 53.2%). Most participants preferring either medication profile reported not having a history of CVD, kidney disease, or smoking. Regardless of medication preference, about two-thirds of the participants reported taking oral T2D medication (60.9% and 59.9% of those choosing DPP4i and SGLT2i’s profile, respectively), whereas few participants were treated with injectables (13.0% of those preferring DPP4i and 8.4% of those preferring SGLT2i’s profile). Among participants reporting previous history of medication, metformin consumption was significantly more frequent in participants favoring SGLT2i compared with DPP4i’s profile (85.2% vs 71.7%, p = 0.0209).
Reasons for Preference of Medication
The numerical differences in the percentage of participants who ranked each attribute according to the reasons for their choice of medication profile are shown in Figure 1. Amongst participants preferring SGLT2i’s profile, reduction of HbA1c was the highest-ranked attribute (ranking “1” – most important reason) to choose this medication (43.6%; Figure 1A). More than two-thirds of the participants choosing SGLT2i’s profile (68.9%) ranked the risk of genital infection as the least important attribute (rating “5” – least important reason).
Amongst participants preferring DPP4i’s profile, the majority (67.4%) considered reduction of HbA1c as the most important reason (ranking “1”) to choose this medication (Figure 1B). The least important attributes (ranking “5”) selected by participants preferring DPP4i's profile were risk of genital infection (37%) and reduction in BW (37%).
Association of Patients’ Characteristics and Their Choice of Medication
According to the univariate analysis, SGLT2i’s profile was more likely selected as the preferred T2D medication by participants who were overweight/obese (91.5%, 95% CI: 87.9–94.2), had HbA1c <7% (93.1%, 95% CI: 88.2–96.4), high BP (95.7%, 95% CI: 92.2–97.9), high cholesterol (92.2%, 95% CI: 87.6–95.5), history of metformin medication (89.9%, 95% CI: 86.1–92.9), and primary level of education/incomplete studies (94.3%, 95% CI: 88.5–97.7) (Data not shown).
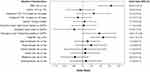
Significant associations were found in the multivariate logistic regression analysis between SGLT2i’s profile preference and increased BMI, high BP, and lower education level. Overweight/obese participants were almost nine times more likely to choose SGLT2i’s profile compared with participants with BMI < 25kg/m2 (OR = 8.9, 95% CI: 3.5–22.5, p < 0.05). Participants with high BP had a significantly greater chance to choose SGLT2i's profile than those with normal BP (OR = 4.9, 95% CI: 1.9–12.4, p < 0.05). Participants with primary/incomplete studies were almost four times more likely to choose SGLT2i's profile compared with those with university/postgraduate studies (OR = 3.6, 95% CI: 1.0–12.6, p < 0.05). (Figure 2).
Discussion
To our knowledge, this is the first study to assess patients’ preferences between two oral agents (DPP4i and SGLT2i) for T2D treatment in LatAm. Our questionnaire revealed that a greater proportion of patients with T2D preferred the SGLT2i’s profile (88.2%) given the conditions that only these medications were available, and their cost was similar.
Consistent with our study findings, another DCE study among Singapore adults with T2D reported that a larger proportion of patients preferred SGLT2i (88%) over DPP4i (12%), without considering their physician’s recommendation.30 A previous cross-sectional analysis in the United States revealed that patients with T1D and T2D preferred SGLT2i over other classes of drugs such as biguanides, SU, GLP-1 RA, long-acting insulins, and thiazolidinediones, primarily due to a favorable regimen and adverse event profile. However, the preference for SGLT2i (47.1%) was comparable with that of DPP4i (52.9%).21
In the present study, most participants ranked reduction in HbA1c as the most important reason for choosing either DPP4i or SGLT2i’s profile. While several factors may have contributed to this finding, a possible explanation could be that T2D management (both from the physicians’ and self-management perspective) is still primarily focused on HbA1c monitoring and control, rather than a holistic approach including T2D associated risks and comorbidities.31,32
Almost 70% of the participants ranked genital infections risk as the least relevant reason to choose SGLT2i’s profile. Our findings are consistent with previous work wherein patients prioritized benefits over risks while choosing a medication.33 Several participants (37%) choosing DPP4i’s profile also ranked genital infections as the least important attribute for their choice, likely as it was not listed as a risk for this medication. An equal 37% of the participants choosing DPP4i’s profile ranked BW as the least important reason, possibly because DPP4i were not shown to reduce BW.14
Patients’ choice of medication may also be attributable to their socio-demographic and/or clinical characteristics. In this study, participants preferring SGLT2i’s profile were slightly older, a larger proportion of them was overweight/obese, had high BP, increased cholesterol levels and HbA1c <7%, as well as primary school/incomplete studies, compared with participants choosing DPP4i’s profile. The multivariate logistic regression analysis showed that the likelihood of selecting the SGLT2i’s profile significantly increased in participants with increased BMI, high BP, and lower education levels.
Participants who were overweight/obese and/or hypertensive were more likely to select SGLT2i’s profile possibly because this medication’s profile was shown to reduce BW in our DCE questionnaire.14 Despite their low education level, participants may have been more likely to choose the SGLT2i’s profile due to the CV and renal benefits presented for this medication in our DCE questionnaire.
The results of the current study support the need for clear discussions between physicians and patients before finalizing the treatment strategy. Considering patients’ preferences and needs while designing a treatment regimen may aid in better compliance and medication adherence, thus improving overall healthcare quality and safety. Major diabetes professional organizations regard patient-centered decision-making to be of paramount significance for individualized T2D care.22,34 Our study results may assist healthcare professionals in educating patients and making shared treatment decisions to improve T2D management.
To our knowledge, this is the first study to provide evidence on T2D patients’ choices of oral antihyperglycemic medications in LatAm. Government and policymakers could consider our findings in strategically designing and planning methods to improve T2D management and reduce the risk of associated comorbidities. Future research is needed to evaluate the generalizability of these results.
Limitations
There are limitations inherent to the cross-sectional and patient’s self-reported nature of this study. Patients included were from two LatAm countries, which limits the generalizability of the results. DCE is a widely used and accepted methodology to evaluate patients’ preferences in the presence of two or more possible treatment options. Efforts were made to minimize bias in exploring patients’ medication preferences by including questions that were clear and easy to understand for the respondents, and by providing a trained facilitator to clarify any queries they could have while completing the questionnaire. Despite these considerations, it remains elusive whether the reported preferences reflect the actual preferences in real-life situations, thus results may lack external validity and should be carefully interpreted.
Conclusion
In this cross-sectional evaluation, SGLT2i’s profile was preferred over DPP4i’s profile as a treatment option by LatAm patients with T2D regardless of baseline characteristics. As shown here, treatment preference is a result of multiple aspects that influence patients’ decisions. We, therefore, believe that a patient-centered approach involving a thorough understanding of patients’ preferences and education needs, with physicians engaging patients in the decision-making process, via fluid communication and a healthy patient-healthcare team relationship, will not only lead to improved treatment adherence but will also improve personal satisfaction, QoL, and overall healthcare outcomes.
Ethics Approval
This study was approved by Comité Independiente de Ética para Ensayos en Farmacología Clínica Fundación de Estudios Farmacológicos y Medicamentos Prof. Luis M. Zieher (FEFyM), Iniciativa y Reflexión Bioética (IRB) Fundación Grupo Colaborativo Rosario (GCR) - Investigación y Prevención Médica and Comité Provincial de Bioética, Ministerio de Salud Gobierno de Santa Fé in Argentina, and by Comité de Ética en Investigación de la Unidad Clínica de Bioequivalencia S. de R.L. de C.V. (UNEBI) in México. Informed consent was obtained from each subject prior to participation.
Acknowledgments
The authors would like to thank Sulekha Shafeeq, PharmD and Ramu Periyasamy, Ph.D. (Indegene Pvt Ltd, Bangalore, India), for providing medical writing support and technical assistance in the preparation of this manuscript. We would also like to thank Dr. César Javier Zaidman for his contribution towards participant recruitment and data collection.
Funding
This study was funded by AstraZeneca. Medical writing assistance provided by Indegene was funded by AstraZeneca.
Disclosure
JECG, JCGC, PPT, JACC, AAGP, PMM, LR, and ASC have received consulting and/or speaker and/or advisory board fees from AstraZeneca. JCGC, PPT, AFH, JACC, AAGP, PMM, LR, and ASC have received investigators’ fees from AstraZeneca. JECG has received consulting and/or speaker and/or advisory board fees from Novo Nordisk and Abbott (outside the submitted work) and is the President of ALAD (Asociación Latinoamericana de Diabetes). JCGC has received consulting and/or speaker and/or advisory board fees from Novo Nordisk, Sanofi, Merck, Novartis, Takeda, Janssen, and MSD (outside the submitted work). PPT has received speaker and advisory board fees from Novo Nordisk and Boehringer Ingelheim (outside the submitted work). AFH has received speaker and/or advisory board fees from Sanofi, Novo Nordisk, Boehringer Ingelheim, and Medtronic (outside the submitted work). JACC has received speaker and/or advisory board fees from Novo Nordisk, Sanofi, Abbott, and Boehringer Ingelheim (outside the submitted work). AAGP has received advisory board fees from Novo Nordisk, Merck, Novartis, and Sanofi (outside the submitted work). PMM has received speaker and/or advisory board fees from Novo Nordisk, Sanofi, Amgen, and Boehringer Ingelheim (outside the submitted work). LR has received speaker and/or advisory board fees from Roche, Novo Nordisk, and Craveri (outside the submitted work). ASC has received speaker and/or advisory board fees from Novo Nordisk, Merck, Silanes, and Armstrong (outside the submitted work). EVM, LFTG, HC, AE, and VBT are employees of AstraZeneca. HC is a shareholder of AstraZeneca. The authors report no other conflicts of interest in this work.
References
1. Khunti K, Chen H, Cid-Ruzafa J, et al. Glycaemic control in patients with type 2 diabetes initiating second‐line therapy: results from the global DISCOVER study programme. Diabetes Obes Metab. 2020;22(1):66–78. doi:10.1111/dom.13866
2. Aschner P, Aguilar-Salinas C, Aguirre L, et al. Diabetes in South and Central America: an update. Diabetes Res Clin Pract. 2014;103(2):238–243. doi:10.1016/j.diabres.2013.11.010
3. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. doi:10.1016/j.diabres.2019.107843
4. Avilés-Santa ML, Monroig-Rivera A, Soto-Soto A, Lindberg NM. Current state of diabetes mellitus prevalence, awareness, treatment, and control in Latin America: challenges and innovative solutions to improve health outcomes across the continent. Curr Diab Rep. 2020;20(11):62. doi:10.1007/s11892-020-01341-9
5. International Diabetes Federation. IDF Diabetes Atlas.
6. Arredondo A. Type 2 diabetes and health care costs in Latin America: exploring the need for greater preventive medicine. BMC Med. 2014;12(1):136. doi:10.1186/s12916-014-0136-z
7. Thomas MC. Type 2 diabetes and heart failure: challenges and solutions. Curr Cardiol Rev. 2016;12(3):249–255. doi:10.2174/1573403X12666160606120254
8. Gallardo-Rincón H, Cantoral A, Arrieta A, et al. Review: type 2 diabetes in Latin America and the Caribbean: regional and country comparison on prevalence, trends, costs and expanded prevention. Prim Care Diabetes. 2021;15(2):352–359. doi:10.1016/j.pcd.2020.10.001
9. Buse JB, Wexler DJ, Tsapas A, Rossing P. 2019 update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43(2):487–493. doi:10.2337/dci19-0066
10. Guías ALAD sobre el Diagnóstico. Control y Tratamiento de la Diabetes Mellitus Tipo 2 con Medicina Basada en Evidencia Edición 2019. Rev ALAD; 2019:1–119.
11. Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm – 2019 executive summary. Endocr Pract. 2019;25(1):69–101. doi:10.4158/CS-2018-0535
12. Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323. doi:10.1093/eurheartj/ehz486
13. Buse JB, Wexler DJ, Tsapas A, et al. 2019 update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43(2):487–493.
14. Wang Z, Sun J, Han R, et al. Efficacy and safety of sodium‐glucose cotransporter 2 inhibitors versus dipeptidyl peptidase 4 inhibitors as monotherapy or add‐on to metformin in patients with type 2 diabetes mellitus: a systematic review and meta‐analysis. Diabetes Obes Metab. 2018;20(1):113–120. doi:10.1111/dom.13047
15. Boye K, Ross M, Mody R, Konig M, Gelhorn H. Patients’ preferences for once‐daily oral versus once weekly injectable diabetes medications: the REVISE study. Diabetes Obes Metab. 2021;23(2):508–519. doi:10.1111/dom.14244
16. Kosiborod M, Cavender MA, Fu AZ, et al. Lower risk of heart failure and death in patients initiated on sodium-glucose cotransporter-2 inhibitors versus other glucose-lowering drugs. Circulation. 2017;136(3):249–259. doi:10.1161/CIRCULATIONAHA.117.029190
17. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–357. doi:10.1056/NEJMoa1812389
18. Lopez Stewart G, Tambascia M, Rosas Guzmán J, Etchegoyen F, Ortega Carrión J, Artemenko S. Control of type 2 diabetes mellitus among general practitioners in private practice in nine countries of Latin America. Rev Panam Salud Pública. 2007;22(1):12–20. doi:10.1590/S1020-49892007000600002
19. Gelhorn HL, Stringer SM, Brooks A, et al. Preferences for medication attributes among patients with type 2 diabetes mellitus in the UK. Diabetes Obes Metab. 2013;15(9):802–809. doi:10.1111/dom.12091
20. Marchesini G, Pasqualetti P, Anichini R, et al. Patient preferences for treatment in type 2 diabetes: the Italian discrete-choice experiment analysis. Acta Diabetol. 2019;56(3):289–299. doi:10.1007/s00592-018-1236-6
21. Flood EM, Bell KF, de la Cruz MC, Ginchereau-Sowell FM. Patient preferences for diabetes treatment attributes and drug classes. Curr Med Res Opin. 2017;33(2):261–268. doi:10.1080/03007995.2016.1253553
22. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35(6):1364–1379. doi:10.2337/dc12-0413
23. Millenson ML, Macri J. Will the Affordable Care Act move patient-centeredness to center stage? Published 2012. Available from: https://www.urban.org/sites/default/files/publication/25186/412524-Will-the-Affordable-Care-Act-Move-Patient-Centeredness-to-Center-Stage-.PDF.
24. Clark MD, Determann D, Petrou S, Moro D, de Bekker-grob EW. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics. 2014;32(9):883–902. doi:10.1007/s40273-014-0170-x
25. Evans M, McEwan P, O’Shea R, George L. A retrospective, case-note survey of type 2 diabetes patients prescribed incretin-based therapies in clinical practice. Diabetes Ther. 2013;4(1):27–40. doi:10.1007/s13300-012-0015-6
26. Rosenstock J, Mathieu C, Chen H, Garcia-Sanchez R, Saraiva GL. Dapagliflozin versus saxagliptin as add-on therapy in patients with type 2 diabetes inadequately controlled with metformin. Arch Endocrinol Metab. 2018;62(4):424–430. doi:10.20945/2359-3997000000056
27. Scott R, Morgan J, Zimmer Z, et al. A randomized clinical trial of the efficacy and safety of sitagliptin compared with dapagliflozin in patients with type 2 diabetes mellitus and mild renal insufficiency: the CompoSIT-R study. Diabetes Obes Metab. 2018;20(12):2876–2884. doi:10.1111/dom.13473
28. Scirica BM, Bhatt DL, Braunwald E, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369(14):1317–1326. doi:10.1056/NEJMoa1307684
29. Mosenzon O, Leibowitz G, Bhatt DL, et al. Effect of saxagliptin on renal outcomes in the SAVOR-TIMI 53 trial. Diabetes Care. 2017;40(1):69–76. doi:10.2337/dc16-0621
30. Ozdemir S, Baid D, Verghese NR, et al. Patient preferences for medications in managing type 2 diabetes mellitus: a discrete choice experiment. Value Heal. 2020;23(7):842–850. doi:10.1016/j.jval.2020.01.023
31. Rushforth B, McCrorie C, Glidewell L, Midgley E, Foy R. Barriers to effective management of type 2 diabetes in primary care: qualitative systematic review. Br J Gen Pract. 2016;66(643):e114–e127. doi:10.3399/bjgp16X683509
32. Ofori S, Unachukwu C. Holistic approach to prevention and management of type 2 diabetes mellitus in a family setting. Diabetes Metab Syndr Obes Targets Ther. 2014;7:159–168. doi:10.2147/DMSO.S62320
33. Mol PGM, Arnardottir AH, Straus SMJ, et al. Understanding drug preferences, different perspectives. Br J Clin Pharmacol. 2015;79(6):978–987. doi:10.1111/bcp.12566
34. Qaseem A, Snow V, Owens DK, Shekelle P. Clinical guidelines committee of the American college of physicians. The development of clinical practice guidelines and guidance statements of the American college of physicians: summary of methods. Ann Intern Med. 2010;153(3):194–199. doi:10.7326/0003-4819-153-3-201008030-00010
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.