Back to Journals » International Journal of General Medicine » Volume 16
Patient-Reported Outcomes After Ferric Carboxymaltose Treatment for Iron Deficiency Anemia: A Prospective Observational Study
Authors Kwong WJ, Numan S, Hunter TD , Alves D, Patel A, Shanbhag S
Received 22 March 2023
Accepted for publication 17 July 2023
Published 2 August 2023 Volume 2023:16 Pages 3291—3300
DOI https://doi.org/10.2147/IJGM.S413105
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Winghan J Kwong,1 Syed Numan,2 Tina D Hunter,3 Dalila Alves,3 Anish Patel,4 Satish Shanbhag5
1Daiichi Sankyo, Inc, Basking Ridge, NJ, USA; 2American Regent, Norristown, PA, USA; 3CTI Clinical Trial & Consulting Services, Covington, KY, USA; 4Brooke Army Medical Center, San Antonio, TX, USA; 5Cancer Specialists of North Florida, Jacksonville, FL, USA
Correspondence: Tina D Hunter, CTI Clinical Trial & Consulting Services 100 E. Rivercenter Blvd, Covington, KY, 41011, USA, Tel +1 513-598-9290, Fax +1 859-261-3757, Email [email protected]
Background: Iron deficiency anemia (IDA) is a common cause of fatigue and impaired quality of life. The present study aimed to evaluate the impact of intravenous iron supplementation with ferric carboxymaltose (FCM) on fatigue, physical function, and general health among patients with IDA attending routine clinical care.
Methods: This was a prospective, single arm, observational study of adult patients prescribed with intravenous FCM for the treatment of IDA during routine clinical care. We used Patient-Reported Outcomes Measurement Information System (PROMIS) instruments to evaluate fatigue (PROMIS Short Form v1.0 13a [FACIT-Fatigue]), general health status (PROMIS Scale v1.2), and physical function (PROMIS Short Form v2.0 4a) before and at 3 and 6 months after FCM treatment.
Results: A total of 152 patients were enrolled. Mean age was 47.4 ± 16.0 years and 82.2% were female. Mean serum hemoglobin was 10.2 ± 1.4 g/dL at baseline. All patients were treated with at least one FCM dose at baseline, with 77.6% receiving a two-dose treatment course. The mean baseline FACIT-Fatigue score was 61.0 ± 9.0, improving significantly to 50.2 ± 9.5 at 3 months after FCM treatment. A minimum 5-point improvement, pre-defined as clinically meaningful, was seen in the FACIT-Fatigue, PROMIS Global Physical Health, Global Mental Health and PROMIS Physical Function scores for 72.7%, 52.8%, 41.7% and 39.8% of patients at 3 months (p < 0.0001 for each change from baseline), with statistically significant improvement continuing at 6 months. Mean serum hemoglobin was significantly increased at both 3 and 6 months (12.8 g/dL [N = 44] and 12.4 g/dL [N = 54], respectively).
Conclusion: IDA patients attending routine clinical practice reported substantial levels of fatigue and impairments in physical function and global health prior to intravenous iron treatment. Patients experienced significant improvements in fatigue symptoms, physical function, and global health at 3 months after treatment with FCM, which were sustained at 6 months.
Keywords: iron deficiency anemia, quality of life, patient-reported outcomes, ferric carboxymaltose, intravenous iron
Introduction
Anemia is a major public health problem across the globe, affecting over a third of the world’s population, predominantly women and children.1,2 Anemia was responsible for 8.8% of the global total years of life lived with disability in 2010, surpassing major depression and chronic respiratory diseases.3
Iron deficiency is the most common cause of anemia, accounting for half of the worldwide cases.1,3,4 The risk of developing iron deficiency is far greater in women, particularly among those of reproductive age owing to menstrual blood loss.5 Iron is an essential component of various proteins, including hemoglobin in erythrocytes and myoglobin in muscles, and plays an important role in multiple cellular mechanisms such as enzymatic processes, oxygen transportation, mitochondrial energy generation, and DNA synthesis.1,6 In iron deficiency, the reduction in serum hemoglobin levels hinders the effective delivery of oxygen from the lungs to the body’s tissues. Consequently, the affected tissues experience insufficient oxygen for their metabolic processes that produce energy. As a result, fatigue is recognized as the cardinal symptom of iron deficiency anemia and represents a central concern to patients.7,8
IDA adversely impacts the patients’ quality of life, work productivity, and cognitive performance, as well as the prognosis of various chronic conditions.9–11 In women, this condition represents the leading cause of years lived with disability.12
Iron supplementation is recommended for the treatment of IDA, with the goal of replenishing iron stores and normalizing hemoglobin levels.1,6 Parenteral iron is indicated when patients are intolerant or unresponsive to oral iron therapy, blood loss exceeds the absorptive capacity for iron, or in the presence of iron malabsorption.1 Various studies have demonstrated that parenteral iron is able to safely and effectively replenish iron stores and normalize hemoglobin concentrations in patients with IDA.13–15
Several intravenous iron formulations are currently available. Ferric carboxymaltose (FCM) is a dextran-free iron complex approved by the United States Food and Drug Administration for the treatment of IDA in adult and pediatric patients with intolerance or an unsatisfactory response to oral iron and in adults with non-dialysis dependent chronic kidney disease.16
While studies on parenteral iron therapy have commonly evaluated hematological outcomes,13–15 few have focused on the patients’ perspective and perceived improvements in quality of life, particularly in real-world clinical practice settings. The present study aimed to evaluate the impact of FCM treatment on the fatigue, physical function, and general health of adult patients with IDA receiving routine clinical care, as measured by a set of patient-reported outcome (PRO) instruments.
Materials and Methods
This was a prospective, single arm, longitudinal, observational study of adult patients prescribed with FCM for the treatment of IDA during routine clinical care. The study was conducted across seven clinical primary and specialty care sites in the United States. Patient enrollment began in August 2020 and completed in October 2021.
The study protocol was reviewed and approved by the Institutional Review Board (IRB) at each study site. All methods were performed in accordance with the ethical guidelines of the 1989 Declaration of Helsinki and all patients provided written informed consent.
Study Population
Adult patients (≥18 years) diagnosed with IDA were invited to participate in the study at the time FCM was prescribed during routine clinical care visits at the study sites. All treatment decisions were per normal standard of care. Eligible patients had baseline serum hemoglobin of >7 g/dL and <13 g/dL for males or <12 g/dL for females, no potential contraindications to FCM, and no parenteral iron therapy within 3 months prior to study enrollment. No specific ferritin or transferrin saturation levels were required.
Study Data
Data on baseline demographics, laboratory values (serum hemoglobin, ferritin, and transferrin saturation levels), medical history, and medication history for IDA were collected based on medical records review. Any subsequent assessment of serum hemoglobin or IDA treatments received by the patients up to 6 months after the first FCM dose were also recorded.
We used three Patient-Reported Outcomes Measurement Information System (PROMIS) instruments in this study. The PROMIS Short Form v1.0 13a (Functional Assessment of Chronic Illness Therapy [FACIT]-Fatigue) is a 13-item instrument that evaluates fatigue over a 7-day recall period and its impact on daily activities.17,18 The PROMIS Scale v1.2 (Global Health) is a 10-item instrument that assesses the patients’ general health status, including physical, mental, and social domains. Two separate scores (physical and mental health scores) are constructed from the overall scale.19 The PROMIS Short Form v2.0 4a (Physical Function) is a 4-item questionnaire used to evaluate the patients’ physical function as derived from their ability to perform various physical activities.20 PROMIS instruments use a standardized T-score metric against normative data for the general population of the US, in which 50 and 10 are the mean and standard deviation, respectively, of the reference population.21,22 A higher FACIT-Fatigue or a lower PROMIS Physical Function, PROMIS Global Physical Health or Mental Health score indicate more health problems. PRO instruments were administered before and at 3 and 6 months after the first FCM dose. PROs were completed online outside of the clinical setting at the follow-up timepoints.
Outcomes
The primary outcome was the change from baseline in FACIT-Fatigue scores, measured at 3 and 6 months after the first dose of FCM. Secondary outcomes included changes in PROMIS Physical Function and Global Health Physical and Mental scores and in serum hemoglobin levels from baseline to 3 and 6 months, and associations between baseline serum hemoglobin levels and baseline PRO scores.
Statistical Analysis
A target sample size of 150 was chosen to provide over 80% statistical power to detect a difference of 3 points in pre-treatment versus post-treatment FACIT-Fatigue scores in the resulting per-protocol population. Key assumptions included a Type 1 error of 0.05, a 14.2-point difference in mean fatigue scores, an expected standard deviation between 12 and 24, and correlation between pre- and post-treatment scores of 0.1–0.5.
Absolute changes in PRO scores and serum hemoglobin levels from baseline to 3 and 6 months after the first FCM dose, as well as between 3 and 6 months, were computed and evaluated for statistical significance with the paired t-test or the non-parametric Wilcoxon signed-rank test. The proportions of patients with no improvement, an improvement between 2.5 and 5 points, and an improvement of at least 5 points were calculated for each PRO measure at 3 and 6 months post the first FCM dose. We defined clinically meaningful improvement as a decrease (for FACIT-Fatigue) or an increase (for the remaining PRO measures) of ≥5 points from baseline.23 A change between 2 and 6 points has been considered appropriate to define minimal important changes in PROMIS measures.23 Associations between each PRO score and serum hemoglobin levels at baseline, 3, and 6 months were assessed using Spearman’s rank correlation coefficient or Pearson’s correlation coefficient. Time to additional parenteral iron treatment was defined as the time between the last dose of the baseline FCM course and the administration of any additional parenteral iron treatment within 6 months of the first FCM dose. We defined additional parenteral iron treatments as those administered more than 4 weeks after the first FCM dose.
All statistical tests were two-sided at a significance level of 5%. Statistical analyses were performed with SAS® software (version 9.4; SAS Institute Inc., Cary, NC, USA).
Results
A total of 152 patients who were prescribed FCM for the treatment of IDA as part of routine clinical practice were included in the study. The great majority (n = 130, 92.8%) completed the study, of whom 110 and 98 completed at least one follow-up PRO survey at 3 and 6 months, respectively. Of the remaining 11 patients, nine were lost to follow-up, one died, and one discontinued due to other reason.
Patient Baseline Characteristics
Patients’ mean age was 47.4 ± 16.0 years and most (82.2%) were female (Table 1). Median IDA duration was 2 years (range: 0 to 30 years) among the 97 patients with non-missing data. Approximately 17% of patients had inflammatory bowel disease. The prevalence of other chronic diseases frequently associated with IDA was relatively low among the study sample, namely for chronic kidney disease (2.0%), heart failure (0%), and cancer (9.2%).
 |
Table 1 Baseline Patient Characteristics |
Over one-third of patients (34.9%) had been treated with oral iron within 3 months prior to FCM prescription, whereas blood transfusions were rarely performed during this period (2.6%). Parenteral iron therapy in the prior 12 months was recorded for 6.6% of patients.
Patients had a mean serum hemoglobin level of 10.2 ± 1.4 g/dL at baseline and a median serum ferritin level of 9.2 ng/m.
Baseline Ferric Carboxymaltose Treatment
All patients were treated with at least one dose of FCM at baseline, of whom the majority (77.6%) received a two-dose treatment course (i.e., two doses within 4 weeks of each other). The cumulative dose of iron averaged 1332.2 ± 313.6 mg across baseline courses. FCM was administered via infusion in all but one case – IV push injection, always at a dose of 750 mg per administration.
Follow-Up Treatments
Fourteen patients (9.7%) required additional parenteral iron treatment within 6 months of the baseline FCM course. Median time from baseline to additional intravenous treatment was 86.5 days (range: 13 to 167 days). No patient was treated with erythropoietin stimulating agents, while one patient received a blood transfusion in this period.
Patient-Reported Outcomes
Results on PRO scores at each time point (baseline, 3, and 6 months) are provided in Figure 1.
 |
Figure 1 Patient-reported outcome scores. |
Fatigue
The mean baseline score for the FACIT-Fatigue scale was 61 ± 9. Most patients completed the FACIT-Fatigue scale at 3 and 6 months (110 [72.4%] and 98 [64.5%], respectively). Fatigue symptoms improved after FCM treatment, as indicated by significantly lower (p < 0.0001) scores at both time points (50.2 ± 9.5 at 3 months and 52.4 ± 9.3 at 6 months). Over two-thirds of the patients who completed the questionnaire had a clinically meaningful reduction in the FACIT-Fatigue score from baseline to 3 and 6 months (72.7% and 67.3%, respectively) (Figure 2).
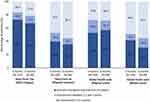 |
Figure 2 Patients with clinically meaningful improvements in patient-reported outcome scores at 3 and 6 months after the first ferric carboxymaltose dose. |
Physical Function
Physical function, as assessed via the PROMIS Physical Function score, was also meaningfully impaired at baseline in the study population (mean score of 41.3 ± 8.6). The mean score was significantly increased (p < 0.0001) at 3 and 6 months after FCM treatment among patients with available data (46.1 ± 8.5 [N = 108] and 45.2 ± 8.9 [N = 98], respectively). Over 35% of patients attained clinically meaningful improvements in the physical function score at 3 and 6 months (Figure 2).
Global Health
The mean Global Physical Health and Global Mental Health component scores of the PROMIS Global Health scale were each more than 5 points below population norms at baseline (41.1 ± 39.8 and 43.9 ± 43.5, respectively). Statistically significant improvements were observed for both scores at 3 and 6 months among patients with non-missing data (Figure 1). Over half of the patients had a clinically meaningful improvement in the Global Physical Health component score at each time point (Figure 2). Lower proportions of patients attained clinically meaningful improvements in the Global Mental Health component score (41.7% and 30.6% at 3 and 6 months, respectively).
Durability of Improvements in Patient Reported Outcomes
There were no statistically significant differences between mean scores at 3 and 6 months for any PROMIS measure, indicating that improvements in patient reported outcomes were mostly sustained up to the end of the follow-up period (Figure 1).
Serum Hemoglobin
Hemoglobin levels were collected for approximately one-third of included patients at 3 and 6 months, averaging 12.8 ± 1.2 g/dL (N = 44) and 12.4 ± 1.9 g/dL (N = 54), respectively. These constitute statistically significant increases of 2.6 ± 1.4 g/dL and 2.3 ± 1.8 g/dL at 3 and 6 months, respectively, compared to the mean baseline value of 10.2 ± 1.4 g/dL (p < 0.0001 for both increases).
Association Between Hemoglobin and Patient-Reported Outcomes
Correlations between baseline serum hemoglobin levels and baseline PRO scores were borderline to highly statistically significant within the study population. A negative correlation between serum hemoglobin and the FACIT-Fatigue score (r=−0.294; p = 0.0002) indicated that lower serum hemoglobin was associated with increased fatigue, while positive correlations with the physical function (r = 0.286; p = 0.0004), physical health (r = 0.276; p = 0.0006), and mental health (r = 0.151; p = 0.0647) indicated that lower serum hemoglobin was associated with lower levels in these scales.
Figure 3 illustrates how serum hemoglobin concentration changes over time are accompanied by similar changes in PRO scores. As with the patient-level correlations at baseline, population-level changes are negatively proportional between hemoglobin and fatigue, and are positively proportional between hemoglobin and the remaining PRO measures.
Discussion
Evidence regarding the impact of intravenous iron therapy on the quality of life of patients with IDA is currently limited in real-world clinical practice settings. The present study collected data in a sample of patients with IDA of various underlying causes, who were prescribed FCM according to routine clinical care. Over three quarters of patients (77.6%) received a two-dose treatment course at baseline. PROMIS instruments were used to evaluate fatigue symptoms, physical function, and global health before and at 3 and 6 months after intravenous iron supplementation.
Prior research has demonstrated that fatigue represents a primary and burdensome symptom in patients with IDA.8,24,25 Accordingly, our results demonstrated a substantial impact of fatigue on the daily activities of enrolled patients, as evidenced by a mean baseline FACIT-Fatigue score (61.0 ± 9.0) more than one standard deviation (10) above the population norm. We found that FACIT-Fatigue scores were normalized to values similar to those of the general population at 3 months post-FCM treatment (mean of 50.5), following a significant decrease from baseline averaging 10.3 points (p < 0.0001). This is consistent with prior literature, which demonstrated the efficacy of intravenous FCM treatment in reducing fatigue among patients with IDA.26–28 While the first follow-up assessment was carried out at 3 months in the current study, prior clinical trial data suggest that significant improvements in fatigue may be noticeable as early as 2 weeks following intravenous FCM treatment.27 Results of the current study also corroborate previous results that showed improvement in fatigue symptoms after treatment with IV iron in a placebo-controlled study evaluating the efficacy and safety of ferumoxytol.24
A key strength of the present research is the 6 month follow-up period, which is considerably longer than that of prior studies exploring the benefit of intravenous iron supplementation on fatigue.24–29 The longer follow-up allowed us to better evaluate the durability of the improvement in fatigue symptoms that patients experience after treatment. Our data indicate that benefits were mostly sustained up to 6 months after the baseline FCM course, as evidenced by a similar mean FACIT-Fatigue score to that found at 3 months (52.4 vs 50.2; p = 0.1326). Similar conclusions can be drawn for the remaining PRO measures.
Baseline data on the more general PRO measures (PROMIS Short Form Physical function and Global Health scale) suggest that IDA has a broad impact on the patients’ quality of life. The scores derived from these instruments for the study sample were all more than 5 points below the population norm, indicating that patients with IDA experience considerable impairments in physical function and global health. As with fatigue, patients also experienced significant improvements in physical function and global health at 3 and 6 months after treatment with FCM. Other studies evaluating general quality of life (via the 36-item Short Form Survey Vitality scale and the energy domain of the Linear Analogue Scale Assessment) have also demonstrated clinically meaningful improvements following intravenous iron supplementation.24,25
The proportion of patients achieving an increase of at least 2 g/dL in serum hemoglobin has been commonly used as a standard efficacy outcome in studies evaluating treatments for IDA.24,29,30 In the present study, serum hemoglobin increased by an average of over 2 g/dL from baseline to 3 and 6 months (2.6 [95% CI: 2.1, 3.0] g/dL and 2.3 [95% CI:1.8, 2.8] g/dL), reflecting the effectiveness of FCM in increasing hemoglobin levels among patients with IDA. This is consistent with literature demonstrating the ability of intravenous iron supplementation in normalizing hemoglobin concentrations, one of the goals of IDA treatment.24,29,30 Moreover, a clinical trial on intravenous FCM for the treatment of IDA in pregnant women reported a similar increase in hemoglobin at approximately 2.8 months post-treatment (2.9 g/dL).28
All correlations between baseline serum hemoglobin and baseline patient-reported outcomes measures, with the exception of mental health, were highly significant (p-values 0.0002 to 0.0006) but the associated correlation coefficients were relatively low (absolute values 0.2756 to 0.2938), indicating a combination of strong population-level association and low patient-level precision. This is typically reflective of heterogeneous patient populations, and is commonly seen in real-world clinical studies.31 At the population level, serum hemoglobin increases mirrored improvements in patient reported outcomes over the course of study. Importantly, these improvements in hematological and quality of life outcomes were mostly achieved after a single course of FCM, with only a small proportion of patients (9.7%) requiring additional intravenous iron treatment throughout the 6 months of study period.
Limitations
The level of missingness for PROs and serum hemoglobin at follow-up assessments constitutes one of our study’s limitations. The fact that PROs were administered online likely contributed to missing data, while electronic reminders that were sent likely helped. The follow-up survey completion rate for this study at 3 months (71%) and 6 months (64%) were higher than the 45% rate without reminders and 62% with reminders seen for email surveys in a study of PRO response rates that compared survey delivery methods.32 While it is difficult to assess the effect of these missing data on our study results, a study of breast reconstruction patients found that non-response at one year was unrelated to 3-month satisfaction, but instead was related to a number of socio-demographic factors.33 If our data missingness was similarly unrelated to patient outcomes, it would have a minimal effect on study results, but if patients who felt better or worse were more likely to respond, the results could include a bias. Follow-up data on Hgb level for this study was limited because the study protocol did not require patients to have a follow-up Hgb level after receiving FCM. Any laboratory assessment during the course of this study was at the physician’s clinical discretion to reflect real-world clinical practice and those assessments that fell outside of the protocol-defined survey windows were not utilized in the analysis.
An additional limitation of the present study was its single arm design. Placebo-controlled trials have demonstrated improvements in FACIT-Fatigue scores among patients receiving placebo for up to 2 weeks after placebo administration.24,29 While there could potentially be some level of placebo effect in our study, we saw improvements out through 6 months. In addition, the improvements in PROs scores were accompanied by increases in hemoglobin concentrations. Therefore, the clinical benefits experienced by the patients in our study are likely to be mostly or fully attributable to the baseline FCM treatment.
Conclusion
IDA patients attending routine clinical practice reported substantial levels of fatigue and impairments in physical function and global health prior to intravenous iron treatment. Patients experienced significant improvements in fatigue symptoms, physical function, and global health at 3 months after treatment with FCM. These clinical benefits were sustained at 6 months, with only a small proportion of patients requiring additional parenteral iron treatment beyond the baseline FCM course.
Patient assessments may provide a valuable supplement to traditional clinical outcomes for evaluating treatment effectiveness in a real-world setting. Improvements in PRO scores observed in this single-arm study require confirmation in randomized placebo-controlled studies to confirm the proportion of the benefit attributable to FCM.
Data Sharing Statement
The original raw data used in this study is available from the corresponding author and can be provided upon reasonable request.
Ethics Approval
The study protocol was reviewed and approved by an IRB at each study site. Three sites used their individual IRB (John Hopkins Medicine IRB, Regional Health Command-Central IRB, and Northwestern University IRB). Four sites used the Advarra IRB.
Acknowledgments
The authors would like to acknowledge Dr. Bobbie Jean Sweitzer, Dr. Joseph Garza, Dr. Marlon Kleinman, Dr. Alyssa Parian, and Dr. George Sanchez for their assistance in patient recruitment, Dr. Maria Aziz for her contribution to this study, and Diogo Ribeiro of CTI Clinical Trial & Consulting Services for medical writing support.
Funding
This study was funded by Daiichi Sankyo, Inc. (Basking Ridge, NJ). The Sponsor participated in the study design, interpretation of data, writing of the manuscript, and decision to submit the article for publication.
Disclosure
Winghan J Kwong is an employee of Daiichi Sankyo, the study sponsor. Syed Numan is an employee of American Regent, a Daiichi Sankyo Group Company. Tina D. Hunter and Dalila Alves are employees of CTI Clinical Trial & Consulting, which is a consultant to Daiichi Sankyo, the study sponsor. Anish Patel is a consultant for AbbVie and a speakers bureau member for Bristol Myers Squibb, Janssen, and Takeda. Satish Shanbhag is a consultant for Beigene and Takeda. The authors report no other conflicts of interest in this work.
References
1. Lopez A, Cacoub P, Macdougall IC, et al. Iron deficiency anaemia. Lancet. 2016;387:907–916.
2. Coad J, Pedley K. Iron deficiency and iron deficiency anemia in women. Scand J Clin Lab Invest Suppl. 2014;244:82–89.
3. Kassebaum NJ, Jasrasaria R, Naghavi M, et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;123:615–624.
4. WHO. Iron Deficiency Anaemia Assessment, Prevention, and Control: A Guide for Programme Managers. Geneva: World Health Organization; 2001.
5. Coad J, Conlon C. Iron deficiency in women: assessment, causes and consequences. Curr Opin Clin Nutr Metab Care. 2011;14:625–634.
6. Kumar A, Sharma E, Marley A, et al. Iron deficiency anaemia: pathophysiology, assessment, practical management. BMJ Open Gastroenterol. 2022;9:e000759.
7. Sobrero A, Puglisi F, Guglielmi A, et al. Fatigue: a main component of anemia symptomatology. Semin Oncol. 2001;28:15–18.
8. Acaster S, Dickerhoof R, DeBusk K, et al. Qualitative and quantitative validation of the FACIT-fatigue scale in iron deficiency anemia. Health Qual Life Outcomes. 2015;13:60.
9. Cappellini MD, Comin-Colet J, de Francisco A, et al. Iron deficiency across chronic inflammatory conditions: international expert opinion on definition, diagnosis, and management. Am J Hematol. 2017;92:1068–1078.
10. Agrawal S, Kumar S, Ingole V, et al. Does anemia affects cognitive functions in neurologically intact adult patients: two year cross sectional study at rural tertiary care hospital. J Family Med Prim Care. 2019;8:3005–3008.
11. Haas JD, Brownlie T. Iron deficiency and reduced work capacity: a critical review of the research to determine a causal relationship. J Nutr. 2001;131:676S–688S.
12. Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017;390:1211–1259.
13. Shao Y, Luo W, Xu H, et al. The Efficacy of Ferumoxytol for Iron Deficiency Anemia: a Meta-Analysis of Randomized Controlled Trials. Acta Haematol. 2019;142:125–131.
14. Cançado RD, de Figueiredo PON, Olivato MCA, et al. Efficacy and safety of intravenous iron sucrose in treating adults with iron deficiency anemia. Rev Bras Hematol Hemoter. 2011;33:439–443.
15. Seid MH, Derman RJ, Baker JB, et al. Ferric carboxymaltose injection in the treatment of postpartum iron deficiency anemia: a randomized controlled clinical trial. Am J Obstet Gynecol. 2008;199:435.e1–7.
16. Food and Drug Administration [homepage on the Internet]. INJECTAFER - ferric carboxymaltose injection, solution, Highlights of prescribing information. Available from: https://www.accessdata.fda.gov/spl/data/2e2e2ed2-9aa5-4466-96ca-989f7a8d3ba8/2e2e2ed2-9aa5-4466-96ca-989f7a8d3ba8.xml.
17. Cella D, Lai J-S, Chang C-H, et al. Fatigue in cancer patients compared with fatigue in the general United States population. Cancer. 2002;94:528–538.
18. Yellen SB, Cella DF, Webster K, et al. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage. 1997;13:63–74.
19. Hays RD, Bjorner JB, Revicki DA, et al. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18:873–880.
20. Stephan A, Stadelmann VA, Leunig M, et al. Measurement properties of PROMIS short forms for pain and function in total Hip arthroplasty patients. J Patient Rep Outcomes. 2021;5:41.
21. Shaw BE, Syrjala KL, Onstad LE, et al. PROMIS Measures can be used to assess symptoms and function in long term Hematopoietic Cell Transplantation Survivors. Cancer. 2018;124:841–849.
22. Evans JP, Smith A, Gibbons C, et al. The National Institutes of Health Patient-Reported Outcomes Measurement Information System (PROMIS): a view from the UK. Patient Relat Outcome Meas. 2018;9:345–352.
23. Terwee CB, Peipert JD, Chapman R, et al. Minimal important change (MIC): a conceptual clarification and systematic review of MIC estimates of PROMIS measures. Quality of Life Research. 2021;30:2729.
24. Vadhan-Raj S, Strauss W, Ford D, et al. Efficacy and safety of IV ferumoxytol for adults with iron deficiency anemia previously unresponsive to or unable to tolerate oral iron. Am J Hematol. 2014;89:7–12.
25. Hetzel D, Strauss W, Bernard K, et al. A Phase III, randomized, open-label trial of ferumoxytol compared with iron sucrose for the treatment of iron deficiency anemia in patients with a history of unsatisfactory oral iron therapy. Am J Hematol. 2014;89:646–650.
26. Herfs R, Fleitmann L, Kocsis I. Treatment of Iron Deficiency with or without Anaemia with Intravenous Ferric Carboxymaltose in Gynaecological Practices – a Non-Interventional Study. Geburtshilfe Frauenheilkd. 2014;74:81–88.
27. Boomershine CS, Koch TA, Morris D. A Blinded, Randomized, Placebo-Controlled Study to Investigate the Efficacy and Safety of Ferric Carboxymaltose in Iron-Deficient Patients with Fibromyalgia. Rheumatol Ther. 2018;5:271–281.
28. Jose A, Mahey R, Sharma JB, et al. Comparison of ferric Carboxymaltose and iron sucrose complex for treatment of iron deficiency anemia in pregnancy- randomised controlled trial. BMC Pregnancy Childbirth. 2019;19:54.
29. Ford DC, Dahl NV, Strauss WE, et al. Ferumoxytol versus placebo in iron deficiency anemia: efficacy, safety, and quality of life in patients with gastrointestinal disorders. Clin Exp Gastroenterol. 2016;9:151–162.
30. García-López S, Bocos JM, Gisbert JP, et al. High-dose intravenous treatment in iron deficiency anaemia in inflammatory bowel disease: early efficacy and impact on quality of life. Blood Transfus. 2016;14:199–205.
31. Holzner B, Kemmler G, Greil R, et al. The impact of hemoglobin levels on fatigue and quality of life in cancer patients. Ann Oncol. 2002;13:965–973.
32. Hansen E, Fonager K, Freund KS, et al. The impact of non-responders on health and lifestyle outcomes in an intervention study. BMC Res Notes. 2014;7:632.
33. Berlin NL, Hamill JB, Qi J, et al. Non-response Bias in Survey Research: lessons from a Prospective Study of Breast Reconstruction. J Surg Res. 2018;224:112–120.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

