Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Path Analysis of Self-Efficacy, Coping Style and Resilience on Depression in Patients with Recurrent Schizophrenia
Authors Wang L , Li M, Guan B, Zeng L, Li X, Jiang X
Received 25 July 2023
Accepted for publication 19 August 2023
Published 1 September 2023 Volume 2023:19 Pages 1901—1910
DOI https://doi.org/10.2147/NDT.S421731
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Liyi Wang,1,2,* Meizhi Li,3,* Bi Guan,4,* Liangnan Zeng,4 Xinchun Li,3 Xiaojian Jiang2
1Department of Oncology, Chengdu Fifth People’s Hospital, Chengdu University of Traditional Chinese Medicine, Chengdu, Sichuan Province, People’s Republic of China; 2College of Nursing, Hunan University of Chinese Medicine, Changsha, Hunan, People’s Republic of China; 3Hunan Provincial Brain Hospital (Hunan Second People’s Hospital), Changsha, Hunan, People’s Republic of China; 4Department of Nursing, Fifth People’s Hospital, Chengdu University of Traditional Chinese Medicine, Chengdu, Sichuan Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaojian Jiang, College of Nursing, Hunan University of Chinese Medicine, Changsha, Hunan, People’s Republic of China, Email [email protected] Xinchun Li, Hunan Provincial Brain Hospital (Hunan Second People’s Hospital), Changsha, Hunan, People’s Republic of China, Email [email protected]
Purpose: Based on the two mediating variables of self-efficacy and coping style, a multiple mediating model was constructed to explore the mechanism by which psychological resilience affects depression in patients with recurrent schizophrenia.
Methods: A total of 210 patients with recurrent schizophrenia who were hospitalized in a tertiary hospital in Hunan Province, China, were enrolled. The Connor Davidson Resilience Scale (CD-RISC), Self-rating Depression Scale (SDS), General Self-Efficacy Energy Scale (GSES) and Simplified Coping Style Questionnaire (SCSQ) were used to evaluate resilience, self-efficacy, coping style and depression. Path analysis was performed by constructing a structural equation model, and the mediating effect between variables was verified by the bias-corrected nonparametric percentile bootstrap method.
Results: Resilience, self-efficacy and positive coping together explained 53.2% of the variance in depression. (1) The total scores of self-efficacy, coping style, resilience and depression in patients with recurrent schizophrenia were 2.54± 0.61, 31.73± 9.62, 58.06± 17.26 and 50.48± 12.55, respectively. (2) Pearson analysis showed that the scores of self-efficacy, positive coping, resilience and depression were significantly correlated with depression (r=− 0.24– 0.51, P< 0.01). (3) The path analysis showed that resilience directly affects depression (β=− 0.401); additionally, resilience indirectly affects depression through self-efficacy (β=− 0.179) and through the chain mediating effect of self-efficacy and positive coping style (β=− 0.024).
Conclusion: There is a high incidence of depression in patients with recurrent schizophrenia in China, and intervention is needed. This research revealed that resilience directly affects depression in patients with recurrent schizophrenia and that self-efficacy and positive coping play a part in mediating resilience and depression in patients with recurrent schizophrenia in China. Implementing targeted interventions based on action paths to improve the level of resilience and reduce the incidence of depression has guiding significance in the field of occupational rehabilitation of patients with recurrent schizophrenia.
Keywords: recurrent schizophrenia, depression, resilience, coping style, path analysis, mediating role, structural equation model
Introduction
Schizophrenia is often accompanied by depression, which is one of the important factors for the high recurrence rate of schizophrenia and an important intermediary leading to self-injury and even suicide in patients with schizophrenia.1 According to a study, the prevalence of first-episode schizophrenia associated with depression was 15.1%,2 and the prevalence of depression in patients with relapse was 47–68%, far more than that in first-episode patients, affecting the social function of patients with relapse and increasing the disease burden.3,4 Studies have shown that5,6 at present, drug therapy is often used to intervene in patients with schizophrenia recurrence and depression, but only short-term control of symptoms requires long-term adherence to medication. Once the drug is discontinued, patients will have similar or different mental symptoms, which are more serious than the previous symptoms or even mental symptoms. In addition, the side effects of drugs, such as insomnia, emotional indifference, slow response, and forgetfulness, increase the mental burden on patients.5 Some researchers have found7–9 that increasing psychotherapy on the basis of drug therapy, such as group mindfulness therapy, narrative nursing, music therapy, etc., can effectively reduce the adverse reactions caused by drug intervention, improve the positive emotions and optimism of patients, and reduce the mental burden of patients. However, the treatment path of psychotherapy is not clear. Researchers can only blindly try psychotherapy on patients one by one, which not only consumes time and energy but also has a low level of treatment effect on patients’ inapplicability, which will hit patients’ self-confidence and enthusiasm.10 It is worth studying the psychological treatment index and psychological treatment path of patients with schizophrenia recurrence and depression.
Resilience is the ability of individuals to achieve positive adaptation by stimulating potential cognitive and psychological traits and using internal and external resources to actively repair negative events such as adversity and trauma.11 Studies have shown that resilience, as a positive psychological factor, plays an important role in the prevention and mitigation of depression, and the resilience of patients with depression is related to self-efficacy, subjective well-being, and coping styles.12 Self-efficacy is the individual’s belief in his or her ability to mobilize motivation, cognitive resources and action processes. Relevant studies have shown that13 self-efficacy is directly related to depression and can affect individuals’ responses to events. Coping style determines the specific coping activities after the cognitive evaluation of the stress process, and positive coping styles are conducive to reducing the risk of depression.14 It is speculated that self-efficacy and coping style play important roles in the influence path of psychological resilience on depression, but previous studies have mostly explored the relationships among variables.15–17
The self-efficacy and coping style found in a separate study of patients with recurrent schizophrenia are related to resilience and depression; however, which one accounts for the pathogenesis of resilience affecting depression and whether there is a chain mediating effect between them is still unclear. We assume that (1) self-efficacy and coping style may mediate the relationship between resilience and depression and that (2) self-efficacy and positive or negative coping styles may play a chain mediating role in the relationship between resilience and depression. In addition, the incidence and degree of depression in patients with recurrent schizophrenia in China are not yet clear. Therefore, the purpose of this study was to explore (1) the incidence and degree of depression in Chinese patients with recurrent schizophrenia; (2) the correlations among self-efficacy, coping style (positive and negative), resilience and depression in patients with recurrent schizophrenia; and (3) a path analysis of self-efficacy, coping style and resilience to depression in patients with recurrent schizophrenia. This study provides a theoretical basis for improving the resilience level and reducing the incidence of depression in patients with recurrent schizophrenia.
Materials and Methods
Study Design and Participants
A research group was established to investigate the whole process; it included 1 expert in the field of mental health, 1 clinical nursing expert, and 3 psychological nursing specialist nurses for one-on-one face-to-face investigation. From May 2021 to December 2021, 210 patients with recurrent schizophrenia were recruited from Hunan Brain Hospital, China. Eligible individuals met the following criteria: (1) patients with schizophrenia diagnosed by CCMD-3 or ICD-10;18 (2) patients with a history of acute psychiatric recurrence;19,20 and (3) patients who could cooperate in the stable period.
Measures
Individuals’ Characteristics
The general situation questionnaire after literature review and analysis included two dimensions: (1) social demographic survey, such as gender, age, education, occupation, family income, and marital status, and (2) disease investigation, such as course of disease, age of onset, untreated period, number of hospitalizations, and medication.
General Self-Efficacy Scale (GSES)
The GSES was compiled by Schwartzel et al21 and revised by Wang Caikang et al in 2001. It has 10 questions scored on a four-level scale; the total score is divided by 10, yielding a score range of 1–4 points. Higher scores indicate higher levels of self-efficacy. The Cronbach’s alpha of the scale was 0.924.22
Self-Rating Depression Scale (SDS)
The SDS was developed in 1965 by Zung23 from the United States. It is one of the most commonly used self-rating depression tools, and patients respond based on their experience over the past week. It contains 20 items rated on a 4-point scale ranging from 1 (none) to 4 (always) points, with items 2, 5, 6, 11, 12, 13, 15, 16, 17, and 20 reverse scored. The scores of all items are summed and multiplied by 1.25. A total score below 50 points is normal, 50–59 points suggests mild depression, 60–69 points suggests moderate depression, and more than 70 points suggests severe depression. In this research, Cronbach’s alpha was 0.92,24,25 which indicates good reliability.
Connor Davidson Resilience Scale (CD–RISC)
This scale was compiled by Connor and Davidson; it is used to evaluate an individual’s resilience.26 The CD-RISC scale included self-improvement (8 items), optimism (4 items) and tenacity (13 items).27,28 A total of 25 items are scored on a 5-point scale ranging from 1–5, indicating “completely incorrect”, “slightly correct”, “sometimes correct”, “more correct”, and “completely correct”, respectively. Higher scores indicate better resilience. In this study, the Cronbach’s α coefficients were 0.85, 0.88 and 0.84 for self-improvement, optimism, and tenacity, respectively.
Simplified Coping Style Questionnaire (SCSQ)
The SCSQ is a self-rating scale compiled by Xie Yaning.29 It adopts multilevel scoring of 0–3 points ranging from not adopted to often adopted. It contains 20 items for the two dimensions (subscales) of positive coping and negative coping. The positive coping dimension consists of items 1–12, such as “try to see the good side of things”; the negative coping dimension is composed of items 13–20, such as “relieve trouble by smoking and drinking”. In this study, the Cronbach’s α coefficient was 0.90, the retest correlation coefficient was 0.89, and the α coefficient of the positive coping subscale was 0.89. The α coefficient of the negative coping subscale was 0.78.30
Data Analysis
All statistical analyses were performed using SPSS 21.0 and AMOS23.0. Patients were divided into four groups according to their depression: no depression group, mild depression group, moderate depression group and severe depression group. The differences in resilience levels among the four groups were compared by one-way analysis of variance. Pearson’s correlation was conducted to analyse the correlation between variables, and then multiple stepwise regression was conducted to analyse the explanatory degree of each variable for depression variation. Path analysis was performed by constructing a structural equation model, and the mediating effect between variables was verified by the bias-corrected nonparametric percentile bootstrap method. Repeated sampling was performed 5000 times,31 the test level was bilateral α= 0.05, and the 95% confidence interval was calculated. P<0.05 was statistically significant.
Results
General Characteristics of Patients with Recurrent Schizophrenia
In total, 210 patients with recurrent schizophrenia participated in the study. Demographic characteristics and disease investigation are shown in Table 1.
 |
Table 1 Demographic Characteristics and Disease Investigation of Patients with Recurrent Schizophrenia (N=210) |
Comparison of Resilience Levels of Depression Across Groups
The resilience levels of depression across groups are shown in Table 2.
 |
Table 2 The Resilience Levels of Depression in Different Groups (P<0.01) |
(1) A total of 210 patients with recurrent schizophrenia had depression (51%), including 88 patients with moderate to severe depression (42%), indicating a high prevalence and severity of depression in patients with recurrent schizophrenia. (2) There were statistically significant differences in the levels of resilience across depression groups (P<0.01). The total resilience score in the group without depression was higher than that in the group with depression (P<0.01). The total resilience score in the mild depression group was higher than that in the moderate and severe depression groups (P<0.01 or P<0.05). The total resilience score in the moderate depression group was higher than that in the severe depression group (P<0.01). The above results indicate that the level of resilience is significantly negatively correlated with the severity of depression. Improving the level of resilience can reduce the degree of depression.
The correlations among the continuous variables are shown in Table 3. There were significant correlations between depression, self-efficacy, coping style and resilience among patients with recurrent schizophrenia. Specifically, there were strong and significant negative relationships between depression and resilience, self-efficacy and positive coping style (r=−0.24–0.51, P<0.01 or p<0.05). There was a strong and significant positive relationship between depression and negative coping style (r=0.364, P<0.01).
 |
Table 3 Correlation Analysis of Depression, Coping Style, Self-Efficacy and Resilience in Patients with Recurrent Schizophrenia |
Multiple Regression Analysis of Depression, Self-Efficacy, Positive Coping Style and Negative Coping Style on Resilience
Multiple regression analysis was conducted with resilience as the independent variable and depression as the dependent variable (F=27.147, P<0.001). The results are shown in Table 4. Psychological resilience explained 22% of the variation in depression, with statistical significance (P < 0.01).
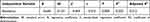 |
Table 4 Multiple Regression Analysis of Resilience on Depression |
Multiple stepwise regression analysis was performed with resilience, self-efficacy, positive coping, and negative coping as independent variables and depression as the dependent variable. The first layer is resilience, the second layer is self-efficacy, the third layer is positive coping, and the fourth layer is negative coping. The results are shown in Table 5. After adding negative coping, P > 0.05, the regression coefficient of negative coping on depression was not statistically significant. The regression equation obtained after removing negative coping (F = 35.627, P < 0.0001, DW = 2.050, VIF ≈1.2) explained 53.2% of the variation in depression, with statistical significance (P<0.01).
 |
Table 5 Multiple Stepwise Regression Analysis of Resilience, Self-Efficacy, and Positive and Negative Coping Styles on Depression |
Measurement Model and Hypothesis Model of Resilience, Self-Efficacy, and Positive and Negative Coping Styles for Depression
Confirmatory factor analysis was adapted to test the measurement model. Depression, self-efficacy, positive coping style, negative coping style and resilience were all latent variables. The results showed that except for the chi-square test, the fitting degree was good, and the fitting results were χ2/df = 26.228 (χ2 = 26.228, df=1), GFI=0.913, AGFI=0.298, NFI=0.809, RFI=0.906, IFI=0.815, TLI=0.976, CFI=0.802, and RSMEA=0.05. Based on the current theory and research, this study assumes that the resilience of patients with recurrent schizophrenia affects depression through five mediating effects (the model is shown in Figure 1): (1) resilience affects self-efficacy as follows: depression, resilience→self-efficacy→depression, a1*b1; (2) resilience affects positive coping on depression, resilience→positive coping→depression, a2*b2; (3) resilience affects negative coping on depression, resilience→negative coping→depression, a3*b3; (4) resilience affects self-efficacy and positive coping on depression, resilience→self-efficacy→positive coping→depression; a1*d1*b2; and (5) resilience affects self-efficacy and negative coping on depression, resilience→self-efficacy→negative coping→depression, a1*d2*b3. In addition, the direct effect of resilience on depression is C.
 |
Figure 1 Measurement and Hypothesis Model. |
The Structural Equation Model of Resilience, Self-Efficacy and Positive Coping Style on Depression
Negative coping style as a mediating variable was not significant after the fitting test and multiple linear regression analysis (P > 0.05); therefore, it was not adapted as a mediating variable of resilience affecting depression. After removal, the maximum likelihood method was adapted to fit and modify the hypothesis model. The structural equation model is shown in Figure 2. The fitting results showed the following model fitting indexes: χ2/df=2.406 (χ2=2.406, df=1), GFI = 0.988, AGFI = 0.879, NFI = 0.975, RFI = 0.851, IFI = 0.985, TLI = 0.907, CFI = 0.985, and RSMEA = 0.012.
 |
Figure 2 The structural equation model of resilience, self-efficacy and positive coping style on depression. Notes: **P < 0.01, ***P < 0.001. |
Path analysis showed that resilience directly affected depression (β = −0.401) and indirectly affected depression through two mediating paths. (1) Ind1: resilience→self-efficacy→depression (β=−0.179,0.13* (−1.358)), with a relative effect value of 29.64% (−0.179/-0.604) (2) Ind2: Chain mediating effect of resilience→self-efficacy→positive coping→depression, (β=−0.024,0.13*3.69*-0.487), with a relative effect value of 3.97% (−0.024/-0.604). The bias-corrected nonparametric percentile bootstrap method was adopted to test the mediating effect of depression. A total of 5000 bootstrap samples were randomly selected from the original data, and their 95% CI was calculated. The results are shown in Table 6. The total mediating effect of resilience on depression was 95% CI (−0.377, −0.048), and the interval did not include 0, indicating that the mediating effect of self-efficacy and positive coping on depression was established. The two mediating paths and the 95% CI of their difference do not contain 0, indicating that the subpath is also statistically significant. According to the subpath difference, the mediating effect of Ind1 is far greater than that of Ind2. The total effect of resilience on depression was 60.4%. The direct effect value of resilience on depression was 66.39%, and the total mediating effect value was 33.61% after the mediating variables of self-efficacy and positive coping were introduced.
 |
Table 6 The Path Analysis Results of Resilience, Self-Efficacy and Positive Coping Style on Depression |
Discussion
This study is the first to analyse the path analysis of the relationships between resilience, self-efficacy, coping style and depression in patients with recurrent schizophrenia by constructing a structural equation model. Resilience can directly or indirectly affect depression, and the mechanism of self-efficacy and coping style in the effect of resilience on depression is analysed. The goodness of fit of the model confirms our hypothesis, which means reducing the prevalence of depression in patients with recurrent schizophrenia and adding a new path.
The Direct Effect of Psychological Resilience on Depression in Patients with Recurrent Schizophrenia
The results of this study showed that there was a significant negative correlation between the severity of depression and resilience (β = −0.401), which directly affected depression. The effect size was 66.39%; that is, the lower the level of resilience was, the more severe the depression. High levels of resilience lead to low depression or no depression, which is consistent with the results of Wang Annie29 and Yan Zhiqiang.30 The reason is that as a special group of people, the psychological resilience of patients with recurrent schizophrenia after multiple recurrences will have a damage superposition effect, which will prevent patients from actively repairing their internal and external resources in the face of risk factors or negative events of recurrence, thus reducing their optimistic cognitive ability and increasing the prevalence of depression.32,34 Therefore, in clinical and community work, we should strengthen patients’ resilience monitoring and take positive psychological intervention measures in a timely manner to improve the level of psychological resilience and reduce the prevalence of depression.
Mediating Effect of Self-Efficacy and Positive Coping Style on Depression in Relapsed Schizophrenia Patients
This study found that self-efficacy and positive coping style partially mediated the influence path of resilience on depression in patients with recurrent schizophrenia, with an effect value of 33.61%. Some studies have noted that improving self-efficacy can effectively alleviate depression.35,36 The reason is that when relapsed patients face stressful events again, strength and optimism can positively affect self-efficacy, improve patients’ confidence and positive coping ability in the face of negative events, and help transform frustration difficulties into experience resources to alleviate negative experiences such as depression, stigma and inferiority and have a protective effect on depression. This is consistent with the research results of Liu D.33 Therefore, interventions such as human function model rehabilitation training,37 focus solution model38,39 and structural dance therapy can effectively improve patients’ self-efficacy and psychological resilience, increase their positive psychological levels and reduce the risk of depression.
This is the first study in China to study the mechanism by which self-efficacy and coping style affect the relationship between resilience and depression in patients with recurrent schizophrenia. It not only enriches the research on the effect of resilience on depression in patients with recurrent schizophrenia but also clarifies the effects of self-efficacy and positive coping style. The effect value provides a theoretical basis for improving the resilience of patients and reducing the incidence of depression. However, the study found that the influencing factors in the relationship between resilience and depression are not only self-efficacy and positive coping styles but also unexplored influencing variables, which are worthy of further exploration and verification. For example, the psychological impact indicators related to resilience and depression, such as self-esteem level, hope level, discrimination-stigma, etc., are worthy of path analysis by constructing a structural equation model.
However, there are still limitations in this study. The source of the research object is relatively singular. This study included only one inpatient with relapsed schizophrenia. Patients who were not included in the community may have had a closed hospitalization environment, leading to a high incidence of depression. Second, the sample size of patients was relatively small. In the future, the sample size should be increased, and samples should be taken from other provinces and across levels of hospitals or nursing homes to expand the scope of research.
Conclusion
The high incidence of depression in patients with recurrent schizophrenia in China requires intervention. This research revealed that resilience directly affects depression in patients with recurrent schizophrenia and that self-efficacy and positive coping play a part in mediating the relationship between resilience and depression in patients with recurrent schizophrenia in China. Implementing targeted interventions based on action paths to improve the level of resilience and reduce the incidence of depression has guiding significance in the field of occupational rehabilitation of patients with recurrent schizophrenia.
Ethics Statement
This study complies with the Declaration of Helsinki. All patients and their families signed informed consent forms, adhering to the principle of voluntary anonymity and fairness, and the study was approved by the Medical Ethics Committee of Hunan Brain Hospital (Hunan Second People’s Hospital). The approval number is K2019011.
Author Contributions
Conception: Liyi Wang, Xiaojian Jiang, Meizhi Li and Xinchun Li. Study design: Liyi Wang, Xiaojian Jiang, Meizhi Li, Liangnan Zeng, Bi Guan and Xinchun Li. Execution: Liyi Wang, Meizhi Li, Liangnan Zeng and Bi Guan. Data collection, analysis and interpretation: Liyi Wang, Liangnan Zeng, Bi Guan and Meizhi Li. Original drafting of the manuscript: Liyi Wang. Critical revision of the manuscript: Xiaojian Jiang, Xinchun Li. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the 2022 “Disciplinary Reveal System” project of Hunan University of Chinese Medicine (Grant no. 22JBZ044); the project funded by Research Project of Teaching Reform in Colleges and Universities in Hunan Province (Grant no. HNJG-2022-0140); the project funded by Hunan Provincial Administration of Traditional Chinese Medicine Project (Grant no. B2023123); the project funded by the 2023 Hunan Social Science Achievements Review Committee (Grant no. XSP2023GLC121) and the projects funded by Hunan Innovative Province Construction Special Funding (Grant no. 2021 SK2009).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhi-qiang Y, Xiao Z, Shou Z, et al. The relationship between affective empathy and depression in adolescent: a chain mediating effect of shame and resilience. Chin J Clin Psychol. 2022;30 (01):77–80.
2. Qian-kun H, Jun-ying L, Jing Z. Effects of structured group mental health treatment on depression and anxiety in schizophrenia inpatients. Health Educ China. 2022;38 (07):662–666.
3. McEnery C, Lim MH, Tremain H, et al. Prevalence rate of social anxiety disorder in individuals with a psychotic disor- der: a systematic review and meta-analysis. Schizophr Res. 2019;208:25–33. doi:10.1016/j.schres.2019.01.045
4. Steel C, Korrelboom K, Baksh MF, et al. Positive memory training for the treatment of depression in schizophrenia: a random- ised controlled trial. Behav Res Ther. 2020;135:103734. doi:10.1016/j.brat.2020.103734
5. Jha MK, Mathew SJ. Pharmacotherapies for treatment-resistant depression: how antipsychotics fit in the rapidly evolving therapeutic landscape. Am J Psychiatry. 2023;180 (3):190–199. doi:10.1176/appi.ajp.20230025
6. Johnston JN, Greenwald MS, Henter ID, et al. Inflammation, stress and depression: an exploration of ketamine’s therapeutic profile. Drug Discov Today. 2023;28 (4):103518. doi:10.1016/j.drudis.2023.103518
7. Rogan T, Wilkinson ST. The role of psychotherapy in the management of treatment-resistant depression. Psychiatr Clin North Am. 2023;46 (2):349–358. doi:10.1016/j.psc.2023.02.006
8. Bhattacharya S, Kennedy M, Miguel C, et al. Effect of psychotherapy for adult depression on self-esteem: a systematic review and meta-analysis. J Affect Disord. 2023;325:572–581. doi:10.1016/j.jad.2023.01.047
9. Dippel N, Szota K, Cuijpers P, et al. Family involvement in psychotherapy for depression in children and adolescents: systematic review and meta-analysis. Psychol Psychother. 2022;95 (3):656–679. doi:10.1111/papt.12392
10. Bartova L, Fugger G, Dold M, et al. Psychotherapy’s role for treatment-resistant depression? Am J Psychiatry. 2022;179 (9):687. doi:10.1176/appi.ajp.20220212
11. Yeo JJ, Chew QH, Sim K. Resilience and its interrelationship with symptomatology, illness course, psychosocial functioning, and mediational roles in schizophrenia: a systematic review. Asia Pac Psychiatry. 2022;14 (2):e12486. doi:10.1111/appy.12486
12. He Q, Jantac Mam-Lam-Fook C, Chaignaud J, et al. Influence of polygenic risk scores for schizophrenia and resilience on the cognition of individuals at-risk for psychosis. Transl Psychiatry. 2021;11 (1):518. doi:10.1038/s41398-021-01624-z
13. Sha-sha LI, Yi-xuan H, An-li H, et al. The mediating effect of diabetic distress on depressive symptoms and self-efficacy in elderly patients with T2DM. Chin J Dis Control Prev. 2022;26 (05):513–516+564.
14. Gangjun G, Hui MA. Relationship between depressive emotion and personality of undergraduates: analysis of coping style as a mediator or moderator. China J Health Psychol. 2022;30 (03):426–431.
15. Qiang Z, Dongfang S, Haiping Z. Effect of drug therapy combined with psychotherapy on anxiety and depression in inpatients with anxiety and depression in acute stage. China Med Pharm. 2019;9 (1):176–179.
16. Lecomte T, Théroux L, Paquin K, et al. Can social anxiety impact facial emotion recognition in schizophrenia? J Nerv Ment Dis. 2019;207 (3):140–144. doi:10.1097/NMD.0000000000000934
17. Faghel-Soubeyrand S, Lecomte T, Bravo MA, et al. Abnormal visual representations associated with confusion of per- ceived facial expression in schizophrenia with social anxiety disorder. NPJ Schizophr. 2020;6 (1):28. doi:10.1038/s41537-020-00116-1
18. Yunfei D, Zeping X. Comparison of Chinese classification and diagnostic criteria for mental disorders version 3 with International Classification of Diseases Version 10. J Clin Psychiatry. 2013;23 (6):426–427.
19. Yanling H, Mingyuan Z. Positive and Negative Syndrome Scale (PANSS) and its application. Clin J Psychiatry. 1997;1997:35–37.
20. Correll CU, Davis RE, Weingart M, et al. Efficacy and safety of lumateperone for treatment of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2020;77 (4):349–358. doi:10.1001/jamapsychiatry.2019.4379
21. Schwarzer R, Born A. Optimistic self-beliefs:assessment of general perceived self-efficacy in thirteen cultures. World Psychol. 1997;3 (1/2):177–190.
22. Wang CK, Hu ZF, Liu Y. Research on reliability and validity of general self-efficacy scale. Appl Psychol. 2001;7 (1):37–40.
23. Sun X. Zung Self-Evaluation and Hamilton Anxiety and Depression Scale in Patients with Coronary Heart Disease. Dalian Medical University; 2018.
24. Chen X-N, Hu Y, Hu W-H, et al. Risk of adverse perinatal outcomes and antenatal depression based on the Zung Self-Rating Depression Scale. Reprod Develop Med. 2021;5 (1):23–29. doi:10.4103/2096-2924.313683
25. Conner M, Davidson RT. Development of a new resilience scale: the Connor-Davidson ResilienceScale (CD-RISC). Depress Anx. 2003;18 (2):76–82. doi:10.1002/da.10113
26. Yu XN, Zhang JX. A comparison between the Chinese version of Ego-Resiliency Scale and Connor-Davidson Resilience Scale. Psychol Sci. 2007;30 (5):1169–1171.
27. Jia-jun-ni L, Zhou X-J, Jia-yan C, et al. Reliability and validity of simplified coping style questionnaire among people affected by leprosy. Mod Prev Med. 2021;48 (14):2507–2509, 2514.
28. Jing F, Ya-ting W, Shui-yuan X. Reliability and validity of simplified coping style questionnaire among adolescents. Chin J Clin Psychol. 2018;26 (5):905–909.
29. Anni W, Wen Z, Yufang G, et al. Resilience--based multifactorial model of depression among people who lost an only child in China. J Cent South Univ. 2021;46 (01):75–83.
30. Qiang Yan Z, Shan L. Relationship between empathy and depression: the modulation of peer relationships. Psychol Behav Res. 2021;19 (03):424–430.
31. Yu YH, Peng MM, Bai X, et al. Schizophrenia, social support, caregiving burden and household poverty in rural China. Soc Psychiatry Psychiatr Epidemiol. 2020;55 (12):1571–1580. doi:10.1007/s00127-020-01864-2
32. Cheng KY, Yen CF. The social support, mental health, psychiatric symptoms, and functioning of persons with schizophrenia participating in peer codelivered vocational rehabilitation: a pilot study in Taiwan. BMC Psychiatry. 2021;21 (1):268. doi:10.1186/s12888-021-03277-0
33. Liu D, Zhou Y, Li G, He Y. The factors associated with depression in schizophrenia patients: the role of self-efficacy, self-esteem, hope and resilience. Psychol Health Med. 2020;25 (4):457–469. doi:10.1080/13548506.2019.1695862
34. Yuan S, Zhenhong W, Zhang Q, et al. Intervention effect of human functional model rehabilitation training on self-efficacy and stigma in patients with schizophrenia. Chin J Nurs. 2022;57 (02):158–164.
35. Chui A, Pan C, Li R, et al. The effect of focus resolution patterns on psychological resilience and self-efficacy in psychiatric patients during inpatient rehabilitation. Chin J Med Doctors. 2021;23 (01):110–113.
36. Aijun C, Changge P, Ruiling L, et al. The effect of focus-solving model on resilience and self-efficacy of hospitalized psychiatric patients during rehabilitation. Chin J Physician. 2021;23 (01):110–113.
37. Jianmei C, Sujuan M, Mingming Z, et al. The relationship between nutritional risk and depression, resilience and self-management behaviour in hospitalized patients with inflammatory bowel disease. Chin J Health Psychol. 2023;31 (4):514–518.
38. Xiangchun Z, Annie W, Tingyu G, et al. Caring ability of caregivers and depression of disabled elderly: chain mediating effect analysis of family resilience and psychological resilience. Milit Nurs. 2023;40 (6):43–47, 52.
39. Fan CH, Hsu SC, Hsiao FH, et al. The association of social support and symptomatic remission among community-dwelling schizophrenia patients: a cross-sectional study. Int J Environ Res Public Health. 2021;18 (8):3977. doi:10.3390/ijerph18083977
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
