Back to Journals » Clinical Ophthalmology » Volume 17
Pars Plana Vitrectomy for Retained Lens Fragments After Cataract Surgery: Outcomes Based on Timing of Surgery
Authors Rohowetz LJ , Jabbehdari S, Yannuzzi NA, Sridhar J, Smiddy WE , Berrocal AM, Albini TA, Townsend JH , Fortun JA, Flynn HW Jr
Received 3 October 2022
Accepted for publication 16 November 2022
Published 1 February 2023 Volume 2023:17 Pages 479—485
DOI https://doi.org/10.2147/OPTH.S391795
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Landon J Rohowetz,1 Sayena Jabbehdari,2 Nicolas A Yannuzzi,1 Jayanth Sridhar,1 William E Smiddy,1 Audina M Berrocal,1 Thomas A Albini,1 Justin H Townsend,1 Jorge A Fortun,1 Harry W Flynn Jr1
1Department of Ophthalmology, Bascom Palmer Eye Institute, Miami, FL, USA; 2Jones Eye Institute, University of Arkansas for Medical Sciences, Little Rock, AR, USA
Correspondence: Harry W Flynn Jr, Tel +1 305 326 6118, Fax +1 351 207 3928, Email [email protected]
Purpose: To evaluate the outcomes and complications in patients with retained lens fragments (RLF) after cataract surgery, comparing those who received pars plana vitrectomy (PPV) on the same day, within 1 week, or later than 1 week after cataract surgery.
Patients and Methods: Retrospective case series of all patients who underwent PPV for RLF at Bascom Palmer Eye Institute between January 1, 2012 and September 30, 2020. Individuals with less than 3 months of follow-up, chronic uveitis, congenital cataract, previtrectomy retinal detachment (RD), and severe trauma were excluded. All analyses for categorical and binary variables used chi-squared tests. Analyses for continuous variables were performed using multivariate analyses of covariance, adjusting for differences in baseline visual acuity before cataract surgery.
Results: The study included 246 eyes of 246 patients. The timing distribution included the following: 140 (57%) eyes underwent same-day PPV, 33 (13%) eyes underwent same-week PPV, and 73 (30%) eyes underwent PPV after 1 week (up to 90 days). When all eyes were included in analysis, there were no statistically significant differences in mean best-corrected visual acuity (BCVA) between groups at last follow-up examination (P = 0.07). When only eyes without known pre-existing ocular disease (N = 157) were included in analysis, there were no differences in mean BCVA between groups at all postoperative timepoints (P > 0.05). The rate of RD did not differ between groups when eyes with and without pre-existing ocular disease were analyzed (P > 0.05).
Conclusion: In the current study, there were no statistically significant differences in postoperative BCVA or rates of RD at last follow-up examination in eyes undergoing PPV for RLF on the same day, within 1 week, or later than 1 week after cataract surgery.
Keywords: retained lens fragments, pars plana vitrectomy, cataract surgery, retinal detachment
Introduction
Cataract surgery is among the most widely performed surgical procedures and yields a high rate of favorable outcomes. Retained lens fragments (RLF), one of the most frequent complications of cataract surgery, occurs in 0.1 to 1.5% of cases (Figure 1).1,2 Secondary complications of RLF include glaucoma, cystoid macular edema, vitreous hemorrhage, uveitis, and retinal detachment (RD).3–7
 |
Figure 1 Fundus photo demonstrating posteriorly dislocated retained lens fragments after cataract surgery. |
Pars plana vitrectomy (PPV), the treatment of choice for posteriorly dislocated RLF, has been shown to improve visual outcomes.6,8,9 The timing of PPV is debated.10 Some studies have demonstrated better visual acuity outcomes with same-day PPV and reduced rates of ocular hypertension, RD, and lens-induced inflammation.11–17 However, others have reported similar outcomes regardless of the timing of PPV.3,18–20
The purpose of the current study was to evaluate outcomes in patients with RLF who received PPV on the same day, within 1 week, and more than 1 week after cataract surgery during the current era of cataract and vitrectomy surgery.
Materials and Methods
The study was approved by the Institutional Review Board at the University of Miami and conformed to the requirements of the United States Health Insurance Portability and Privacy Act. All investigations were conducted in accordance with the Declaration of Helsinki.
The study design was a retrospective, interventional case series including all patients who underwent PPV for RLF (defined as presence of any amount of cortical or nuclear lens material within the posterior segment) after cataract surgery between January 1, 2012 and September 30, 2020 at a university-affiliated medical center. The following patients were excluded from the study: individuals <21 years of age, pregnant women, prisoners, and patients with a history of chronic uveitis, congenital cataract, previtrectomy RD (rhegmatogenous or tractional), and trauma.
Subjects were analyzed in 3 groups based on the timing of PPV: the same day, within 1 week, and more than 1 week after cataract surgery. Patients in the same-day group received PPV in the same operating room as the original cataract surgery. Patients who underwent surgery beyond the same day were referred from within or outside of our institution after identification or suspicion of RLF. All surgeries were performed on an outpatient basis with a peribulbar anesthetic block.
Data collected included age, gender, eye, prior ocular history, best-corrected visual acuity (BCVA) before cataract surgery, time between cataract surgery and PPV, BCVA before PPV, development of postoperative RD, intraocular lens (IOL) status at last follow-up examination, and postoperative BCVA at 3 months, at 6 months, and at last follow-up examination. Visual acuity was measured by Snellen charts and was converted to logMAR for comparison and statistical analyses. Patients were followed up for at least 3 months.
All analyses for categorical and binary variables used chi-squared tests. Analyses for continuous variables were performed using multivariate analyses of covariance, adjusting for differences in baseline visual acuity before cataract surgery.
Results
A total of 283 eyes of 283 patients underwent PPV for RLF. Thirty-seven eyes received PPV more than 90 days after cataract surgery and thus were excluded, leaving a total of 246 study eyes. The number of eyes comprised 140 (57%) in the same-day group, 33 (13%) in the within 1-week group, and 73 (30%) in the more than 1-week group. The mean age of patients was 70.0 ± 10.4, 70.9 ± 7.9, and 71.2 ± 11.9 years in the same-day, within 1-week, and more than 1-week groups, respectively. There were no significant differences in mean age between groups (P = 0.69).
The mean interval to PPV in the same-week group was 5 ± 1.8 days while the mean interval to PPV in the more than 1-week group was 31 ± 22.3 days. Mean baseline BCVA before cataract surgery was 20/282 for the same-day group, 20/178 for the same-week group, and 20/132 for the more than 1-week group (P = 0.06). The mean previtrectomy BCVA was 20/317 in the same-week group and 20/205 in the more 1-week group (P = 0.33).
Pre-existing corneal endothelial disease as diagnosed by clinical exam, pachymetry, or specular microscopy was more prevalent in the more than 1-week group (5.5%) compared to the same-day group (0.7%; P = 0.04). There were no differences in pre-existing corneal endothelial disease between the same-week group and the same-day and more than 1-week groups (P > 0.05). Diabetic retinopathy was more common in the same-day group when compared to the more than one-week group (P = 0.03) and there were no differences in the rates of diabetic retinopathy between the other groups. There were no differences in rates of all other pre-existing ocular conditions between groups (P > 0.05; Table 1).
 |
Table 1 Demographic Data and Baseline Details in Eyes That Underwent Pars Plana Vitrectomy for Retained Lens Fragments |
After PPV, a posterior chamber intraocular lens was present in 113 (80.7%) eyes in the same-day group, 26 (78.8%) eyes in the within 1-week group, and 55 (75.3%) eyes in the more than 1-week group. An anterior chamber intraocular lens was present in 17 (12.1%) eyes in the same-day group, 4 (12.1%) eyes in the within 1-week group, and 7 (9.6%) eyes in the more than 1-week group. Due to poor visual potential from concurrent vitreoretinal disease, 2 (1.4%), 1 (3.0%), and 4 (5.5%) eyes remained aphakic in the same-day, same-week, and more than one-week groups, respectively. No differences were observed between groups (P = 0.63; Table 2).
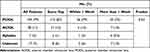 |
Table 2 Lens Status at Last Follow-Up in Eyes That Underwent Pars Plana Vitrectomy for Retained Lens Fragments |
Outcomes in All Eyes
Mean postoperative BCVA at 3 months was 20/56 in the same-day group, 20/54 in the same-week group, and 20/73 in the more than 1-week group (P = 0.07). Mean postoperative BCVA at 6 months was 20/56, 20/43, and 20/115 in the same-day, same-week, and more than 1-week groups, respectively. Mean BCVA at 6 months was superior in the same-day group compared to the more than 1-week group (P = 0.04) but did not differ between the other groups (P > 0.05). Mean BCVA at last follow-up for same-day, within 1-week and more than 1-week eyes was 20/56, 20/42, and 20/76 (P = 0.07). Mean BCVA improved from 20/224 before cataract surgery to 20/55 at last follow-up examination (P < 0.001).
Best-corrected visual acuity at last follow-up examination was 20/40 or better in 94 (67.1%), 22 (66.7%), and 38 (52.1%) eyes in the same-day, same-week, and more than 1-week groups, respectively (P = 0.09). Final BCVA was 20/200 or worse in 24 (17.1%) eyes in the same-day group, 3 (9.1%) eyes in the within 1-week group, and 19 (26.0%) eyes in the more than 1-week group (P = 0.09).
Retinal detachment occurred in 6 (4.4%) patients in the same-day group, 2 (6.1%) patients in the same-week group, and 7 (9.6%) patients in the more than 1-week group (P = 0.33). Only 1 patient was noted to have an RD intraoperatively during cataract surgery.
Outcomes in Eyes Without Pre-Existing Ocular Disease
To control for confounding variables, 157 eyes without pre-existing ocular disease were separately identified and analyzed from those with glaucoma, pseudoexfoliation, diabetic retinopathy, corneal endothelial disease, and uveitis. Mean BCVA at 3 months was 20/55, 20/59, and 20/73 in the same-day, within 1-week, and more than 1-week groups, respectively (P = 0.80). Mean BCVA at 6 months was 20/62 in the same-day group, 20/43 in the within 1-week group, and 20/91 in the more than 1-week group (P = 0.59). At last, follow-up examination, mean BCVA in the same-day, within 1-week, and more than 1-week groups was 20/50, 20/36, and 20/54, respectively (P = 0.84). Mean BCVA improved from 20/240 before cataract surgery to 20/47 at last follow-up examination (P < 0.001).
At last, follow-up examination, BCVA was 20/40 or better in 62 (72.1%), 17 (70.8%), and 30 (63.8%) eyes who underwent PPV the same day, within 1-week, or more than 1-week after cataract surgery, respectively (P = 0.61). Furthermore, 13 (15.1%) same-day eyes, 2 (8.3%) within 1-week eyes, and 8 (17.0%) more than 1-week eyes had a BCVA of 20/200 or worse at last follow-up examination (P = 0.61; Table 3).
 |
Table 3 Visual Acuity Outcomes at Last Follow-Up Examination in Eyes That Underwent Pars Plana Vitrectomy for Retained Lens Fragments |
Retinal detachment occurred in 4 (4.8%) patients in the same-day group, 2 (8.3%) patients in the same-week group, and 5 (10.6%) patients in the more than one-week group (P = 0.45).
Discussion
Retained lens fragments is an uncommon complication of cataract surgery, causing varying degrees of intraocular inflammation due to the immunogenic nature of lens material.2,21 Removal of RLF via PPV reduces long-term sequalae and improves visual acuity by decreasing inflammation.6,9,21
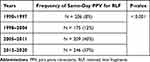
The optimal timing of PPV for RLF has been debated. Many patients who do not get same-day PPV are initially managed with topical steroids and antihypertensive drops before PPV.22 Same-day, or at least expedited, PPV has been suggested in patients with larger fragments, extensive media opacities, and significant intraocular inflammation. The current authors found rates of same-day PPV for retained lens fragment to have gradually increased, from 8% in 1990 to 1997, 12% from 1998 to 2004, 40% from 2005 to 2011, and 57% from 2012 to 2020 (P < 0.001; Table 4).
The current study did not detect differences in BCVA at last follow-up examination in patients who received same-day, same-week, or more than one-week PPV. Although BCVA at 6 months was superior in patients who underwent same-day PPV compared to more than one-week PPV, there were no differences at this timepoint when patients with pre-existing ocular disease were excluded from analysis. Furthermore, the proportion of patients with postoperative RD, BCVA ≥ 20/40 at last follow-up examination, or BCVA ≤ 20/200 at last follow-up examination did not differ between groups when patients with and without ocular disease were included in the analysis. These findings are in accordance with previous work which has demonstrated similar outcomes regardless of PPV timing (Table 5).3,18–20,22 Prompt PPV might not be available in many instances, so the finding that outcomes do not seem to be disadvantaged by a delay is pertinent.
 |
Table 5 Visual Acuity Outcomes at Last Follow-Up Examination After Pars Plana Vitrectomy for Retained Lens Fragments at a University-Affiliated Medical Center |
The retrospective design of the current study limits the decisiveness of our findings. Certain factors such as the degree of RLF and the type of posterior chamber IOL were not recorded but may have influenced outcomes. Furthermore, a fraction of patients were lost to follow-up before the 3-month postoperative visit, which may have introduced a bias in ascertaining patients in this study. It seems highly unlikely that this research question would be studied in a prospective manner to overcome these limitations.
Conclusion
PPV for RLF requires access to a variety of resources including vitreoretinal surgical support. Same-day PPV in the same operating room for RLF may be a preferred approach when available, but the current study demonstrates that later PPV does not appear to compromise outcomes.
Informed Consent
Requirement of informed consent was waived by the institutional review board due to the retrospective nature of the study.
Funding
NIH Center Core Grant P30EY014801 (Bethesda, MD), Research to Prevent Blindness-Unrestricted Grant to BPEI (GR004596; New York, NY). The sponsors had no role in the design or execution of the study.
Disclosure
Nicolas A Yannuzzi is a consultant/advisor for EyePoint, Genentech, Regeneron, REGENXBIO, and Gyroscope. Jayanth Sridhar is a consultant for Genentech, Regeneron, Alcon, Apellis, Ocuterra, DORC, and Allergan. Audina M Berrocal is a consultant for Alcon, Allergan, Bayer, DORC, Phoenix Clinical, Visunex Medical System, Novartis, and Zeiss. Thomas A Albini is a consultant for Allergan and EyePoint. Jorge A Fortun is a consultant for DORC and Carl Zeiss and receives financial support from Aldreya. The authors report no other conflicts of interest in this work.
References
1. Wang W, Yan W, Fotis K, et al. Cataract surgical rate and socioeconomics: a global study. Invest Ophthalmol Vis Sci. 2016;57(14):5872–5881. doi:10.1167/iovs.16-19894
2. Lin WV, Scott MN, Tendhar C, et al. Outcomes of cataract surgery complicated by retained lens fragments requiring pars plana vitrectomy. Clin Ophthalmol. 2020;14:939–946. doi:10.2147/OPTH.S239100
3. Modi YS, Epstein A, Smiddy WE, Murray TG, Feuer W, Flynn HW
4. Chalam KV, Murthy RK, Priluck JC, Khetpal V, Gupta SK. Concurrent removal of intravitreal lens fragments after phacoemulsification with pars plana vitrectomy prevents development of retinal detachment. Int J Ophthalmol. 2015;8(1):89–93. doi:10.3980/j.issn.2222-3959.2015.01.16
5. Cohen SM, Davis A, Cukrowski C. Cystoid macular edema after pars plana vitrectomy for retained lens fragments. J Cataract Refract Surg. 2006;32(9):1521–1526. doi:10.1016/j.jcrs.2006.04.019
6. Kim IK, Miller JW. Management of dislocated lens material. Semin Ophthalmol. 2002;17(3–4):162–166. doi:10.1076/soph.17.3.162.14779
7. Moore JK, Scott IU, Flynn HW
8. Vilar NF, Flynn HW
9. Blodi BA, Flynn HW
10. Vanner EA, Stewart MW. Meta-analysis comparing same-day versus delayed vitrectomy clinical outcomes for intravitreal retained lens fragments after age-related cataract surgery. Clin Ophthalmol. 2014;8:2261–2276. doi:10.2147/OPTH.S71494
11. Vanner EA, Stewart MW, Liesegang TJ, Bendel RE, Bolling JP, Hasan SA. A retrospective cohort study of clinical outcomes for intravitreal crystalline retained lens fragments after age-related cataract surgery: a comparison of same-day versus delayed vitrectomy. Clin Ophthalmol. 2012;6:1135–1148. doi:10.2147/OPTH.S27564
12. Ho LY, Doft BH, Wang L, Bunker CH. Clinical predictors and outcomes of pars plana vitrectomy for retained lens material after cataract extraction. Am J Ophthalmol. 2009;147(4):587–594 e581. doi:10.1016/j.ajo.2008.10.026
13. Merani R, Hunyor AP. Medical versus surgical management of retained lens fragments. J Cataract Refract Surg. 2009;35(12):2181. doi:10.1016/j.jcrs.2009.10.012
14. Merani R, Hunyor AP, Playfair TJ, et al. Pars plana vitrectomy for the management of retained lens material after cataract surgery. Am J Ophthalmol. 2007;144(3):364–370. doi:10.1016/j.ajo.2007.05.027
15. Wilkinson CP, Green WR. Vitrectomy for retained lens material after cataract extraction: the relationship between histopathologic findings and the time of vitreous surgery. Ophthalmology. 2001;108(9):1633–1637. doi:10.1016/S0161-6420(01)00698-4
16. Al-Khaier A, Wong D, Lois N, Cota N, Yang YC, Groenewald C. Determinants of visual outcome after pars plana vitrectomy for posteriorly dislocated lens fragments in phacoemulsification. J Cataract Refract Surg. 2001;27(8):1199–1206. doi:10.1016/S0886-3350(01)00750-7
17. Chen CL, Wang TY, Cheng JH, Tai MC, Lu DW, Chen JT. Immediate pars plana vitrectomy improves outcome in retained intravitreal lens fragments after phacoemulsification. Ophthalmologica. 2008;222(4):277–283. doi:10.1159/000139953
18. Scott IU, Flynn HW
19. Colyer MH, Berinstein DM, Khan NJ, et al. Same-day versus delayed vitrectomy with lensectomy for the management of retained lens fragments. Retina. 2011;31(8):1534–1540. doi:10.1097/IAE.0b013e31821800fc
20. Peck T, Park J, Bajwa A, Shildkrot Y. Timing of vitrectomy for retained lens fragments after cataract surgery. Int Ophthalmol. 2018;38(6):2699–2707. doi:10.1007/s10792-017-0719-8
21. Gilliland GD, Hutton WL, Fuller DG. Retained intravitreal lens fragments after cataract surgery. Ophthalmology. 1992;99(8):1263–1269. doi:10.1016/S0161-6420(92)31814-7
22. Kim JE, Flynn HW
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.