Back to Journals » Journal of Pain Research » Volume 15
Pain Management in a Prehospital Emergency Setting: A Retrospective Observational Study
Authors Ferri P , Gambaretto C, Alberti S , Parogni P , Rovesti S , Di Lorenzo R , Sollami A, Bargellini A
Received 2 June 2022
Accepted for publication 23 September 2022
Published 27 October 2022 Volume 2022:15 Pages 3433—3445
DOI https://doi.org/10.2147/JPR.S376586
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Robert Twillman
Paola Ferri,1 Carlo Gambaretto,2 Sara Alberti,3 Pierpaolo Parogni,2 Sergio Rovesti,1 Rosaria Di Lorenzo,4 Alfonso Sollami,5 Annalisa Bargellini1
1Department of Biomedical, Metabolic and Neural Sciences, University of Modena and Reggio Emilia, Modena, Italy; 2Emergency Department, ASST of Mantova, Mantova, Italy; 3Clinical and Experimental Medicine PhD Program, Department of Biomedical, Metabolic and Neural Sciences, University of Modena and Reggio Emilia, Modena, Italy; 4Department of Mental Health and Drug Abuse, AUSL of Modena, Modena, Italy; 5Health Professions Service, University Hospital of Parma, Parma, Italy
Correspondence: Sara Alberti, Clinical and Experimental Medicine PhD Program, Department of Biomedical, Metabolic and Neural Sciences, University of Modena and Reggio Emilia, Modena, 41125, Italy, Tel +390592055599, Email [email protected]
Purpose: Acute pain is a prevalent symptomatology in prehospital emergency care. Although inadequate assessment and treatment of acute pain are associated with various complications, about 43% of adults suffering from pain are undertreated. This phenomenon is poorly studied, and limited data are available in the literature. The objective was to investigate the pain management in a prehospital emergency health-care setting, verifying pain assessment, pharmacological treatment adherence and the effectiveness of pain relief therapy.
Patients and Methods: A retrospective observational study was conducted in a sample including all adults treated by the professionals of nurse-staffed ambulances and medical cars in an Italian Emergency Medical Services (EMS) from 1 January 2019 to 31 May 2019. We collected both demographic information and Numeric Rating Scale scores, which evaluated presence and intensity of pain, from the EMS paper forms. All analyses were performed using SPSS, version 27.
Results: The study sample was composed of 629 people: 310 males (49%) and 319 females (51%), with an average age of 64.2± 22 years (range 18– 108). Pain information was collected in 75.5% (n = 475) of our sample; among them 222 patients (46.7%) suffered from pain. We recorded that 79.7% (n = 177) of the subjects with pain received no pharmacological treatment, and in almost all of the treated cases they did not adhere to the analgesia algorithm in use. Among those who were pharmacologically treated, pain statistically significantly decreased in intensity, from before to after, in both emergency vehicles (nurse-staffed ambulances pre m = 8.36± 0.9 vs post m = 4.18± 2.2, p< 0.001; medical cars pre m = 7.25± 1.7 vs post m = 3.50± 2.6, p< 0.001). Subsequently, pain was only re-ascertained in 24.3% of subjects.
Conclusion: Our findings confirm that pain is a prevalent symptom in prehospital patients, especially in the younger age range, but that it remains an underrecognized, underestimated, and undertreated symptom with the risk of causing worse health outcomes.
Keywords: pain assessment, pain management, prehospital emergency care, emergency medical services, undertreatment of pain
Introduction
Pain is “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”,1 whose assessment and timely and appropriate treatment constitute a standard of quality of care in urgent medicine.2,3 Pain is probably one of the primary reasons for admission to the Emergency Department,4 whose prevalence in prehospital emergency medicine varies from 20% to 53%, reaching up to 70% according to some studies.5–8 The main manifestations of pain are traumatic lesions (21.8%), abdominal pain (12.2%) and chest pain (10%);9 in 34–64% of cases, the pain is moderate/severe.6,10
Inadequate assessment and treatment of acute pain are associated with various complications such as anxiety, heart complications and aggravation of general conditions (eg, tachycardia, blood hypertension or hypotension, hypoventilation in abdominal pain, delirium), longer admissions with an increased risk of infection and becoming chronic with long-term complications, such as post-traumatic syndrome and reduced quality of life.3,11–14 In addition to preventing potential hazards, effective pain treatment makes transport on emergency vehicles more tolerable for the patient.14 Oligoanalgesia, defined as a complete lack of analgesia (unrelieved pain) or an insufficient dose of analgesics (unachieved analgesia) or a postponed analgesic treatment in the prehospital emergency setting, remains a widespread phenomenon.3,7,14,15 It is estimated that in prehospital emergency care pain assessment is not performed in from one-third to almost a half of all cases and even when pain is recorded, in approximately 43% of adults and 85% of paediatric patients, it is undertreated.7,13,16 However, the management of pain in this setting is often inadequate for several reasons: reduced frequency of measuring pain, reluctance of health-care professionals to prescribe or administer opioids (defined as opiophagia), failure to use pain management guidelines, prejudices and cultural factors, fear of excessive sedation and compromising an adequate clinical assessment.4,13,16,17 In addition to these factors, there are others of a managerial-organizational nature such as reduced training and education of health personnel, the limited availability of staff and opioids in the prehospital emergency setting, and the lack of systematic quality management programmes for acute pain management.9,13,14
According to the latest guidelines, proper and effective pain management must be ensured for all patients suffering from pain starting with prehospital emergency care; the main objective is to reduce pain, maintain functioning and minimize adverse effects.13 The use of standardized protocols is recommended, each protocol in the emergency-urgency setting should include: an initial assessment of both the presence and intensity of pain using validated scales and instruments, pharmacological and non-pharmacological interventions for pain management with relevant indications and contraindications, monitoring and reassessment of the patient’s pain after administration of analgesics, transfer of relevant information to hospital staff.4,9,13,18 Moreover, it is recommended that patients should be re-dosed if pain persists.19 The conditions for the administration of analgesic treatment depend on several factors, but mainly on the organization of the emergency-urgency service.20
In many countries pharmacological treatments, particularly opioids, can only be prescribed by doctors; therefore, several supportive strategies have been developed to prevent oligoanalgesia, including specific algorithms for pain management and teleconsultation with the doctor. The latter allow nurses, following specific training, to provide highly specialized services in a prehospital setting on advanced emergency vehicles in the absence of a physician.20,21 However, the literature shows a lack of use of such strategies, in fact from a recent cross-sectional study carried out in 74 emergency-urgency service centres in 107 Italian provinces (2021) it has emerged that the analgesia protocols administered by the nurse are available in less than half of the Italian provinces; these results indirectly indicate potential undertreatment of prehospital pain.14 The epidemiology of pain and its management among prehospital patients is still too little known, despite the relevance and potential impact of pain undertreatment.5,8,10,14,22–24
The research objective was, therefore, to investigate the pain management in a prehospital emergency health-care setting, verifying pain assessment, pharmacological treatment adherence, and the effectiveness of pain relief therapy.
Materials and Methods
Design
This retrospective observational monocentric study was conducted on the management of pain by health-care professionals in advanced prehospital emergency vehicles of an Italian Emergency Medical Service (EMS).
Setting
The EMS recruited for the present study has the function of ensuring the organization of prehospital emergency care in an Italian provincial area. The vehicles used for the advanced prehospital emergency care included:
- nurse-staffed ambulance with a nurse qualified to use clinical-care algorithms according to the instructions provided by telephone by the doctor of the Operations Centre;
- medical car with both a doctor and a nurse.
During prehospital healthcare, professionals complete a standard prehospital emergency care form containing data about the patient’s physical condition, including pain, indicating its intensity according to the Numeric Rating Scale (NRS), type of event and the colour code of prehospital triage in use to make the emergency care universally identifiable for each subject. The 11-point NRS is anchored with 0 as no pain and 10 as maximum imaginable pain.
The colour code of prehospital triage is nationally recognized.25 It consists of 5 classes in order of severity:
- White code means that there is no urgency; the patient does not need first aid and he can contact his general practitioner.
- Green code means minor urgency; the patient reports injuries (minor trauma, fractures, etc.) or complains of symptoms which do not affect vital functions but need treatment.
- Yellow code means urgency; the patient has a partial impairment of the circulatory or respiratory system or he complains of intense pain without immediate danger to life requiring medical check-up as soon as possible.
- Red code means emergency, which indicates a person whose life is in immediate danger with one or more compromised vital functions, such as a state of shock, loss of consciousness, interrupted breathing, cardiac arrest, bleeding and very serious trauma.
- Black code is assigned to the patient deceased during first aid.
For the pharmacological treatment of pain, a treatment algorithm of all potential analgesic medications that may be used to manage pain by its severity is provided:
- Mild pain (NRS 1–3): administration of Paracetamol up to 15 mg/kg intravenously as a slow infusion.
- Moderate pain (NRS: 4–6): administration of Paracetamol up to 15 mg/kg intravenously as a slow infusion or Ketorolac up to 30 mg intramuscularly in adults, accompanied by adequate hydration. If the pain score is equal to 6, opioid medications may be administered.
- Severe pain (NRS 7–10): administration of Fentanyl 1 mcg/kg or Sufentanyl (0.1 mcg/kg) in adults either intravenously slowly or via the Mucosal Atomisation Device at a dose of 1.5 mcg/kg. In the nurse-staffed ambulance, nurses can administrate only fentanyl 1.5 mcg/kg using the mucosal atomization device according to the instructions provided by telephone by the doctor of the Operations Centre; in medical cars, the doctor present can both modify the therapeutic algorithm and decide what to prescribe. As an alternative, intravenous Morphine administration at a dose of 2 mg is indicated, particularly suitable for elderly subjects. In both advanced prehospital emergency vehicles, the dosage can be increased according to medical prescription.
Participant Recruitment
The sample included all adults assisted by professionals of nurse-staffed ambulances and medical cars in an Italian EMS in the period from 1 January 2019 to 31 May 2019. The data were collected from the prehospital emergency care forms according to the following eligibility criteria.
Inclusion Criteria
- persons aged ≥18 years;
- assistance received from professionals of nurse-staffed ambulances or medical cars in an EMS;
- prehospital emergency care forms dated in the period between 1 January 2019 and 31 May 2019;
- all prehospital colour codes.
Exclusion Criteria
- persons aged <18 years;
- emergency care with non-advanced emergency vehicles (without health-care professionals on board);
- very incomplete prehospital emergency care forms with missing essential data or with incomprehensible writing (eg, ID of the form, date of intervention, sex and age of the patient, type of event, state of consciousness);
- prehospital emergency care forms reporting that the pain could not be assessed using the NRS scale (eg, unconscious patient, unable to communicate the pain).
Data Collection
The prehospital emergency care paper forms were manually consulted and selected according to the defined eligibility criteria.
To achieve the objective of the study, the following outcomes were measured:
- sex;
- age;
- type of advanced emergency vehicle (nurse-staffed ambulance or medical car);
- prehospital triage code;
- type of event: traumatic injury or medical condition;
- recording of initial pain scale scores;
- presence and intensity of pain, in relation to age and sex;
- adherence to the algorithm for the pharmacological treatment of pain;
- recording of repeat pain scores after pharmacological treatment;
- effectiveness of pain relief therapy as a reduction in the mean value of pain scale score.
Data Analysis
Descriptive statistics were used to describe the sample characteristics and pain distribution by intensity classes. Continuous variables were presented as means and standard deviations (SDs) and categorical variables as frequencies and percentages. Bivariate statistical analysis techniques were used for the combined analysis of pain-age, pain-sex, pain-emergency vehicle, pain-event and pain-pharmacological treatment. The efficacy of the pain relief therapy was measured as the difference in the sample mean of pain between the first assessment and the reassessment (t-test). Simple linear regression was carried out to test if age and event significantly predict pain and a logistic regression to verify the probability of type of event in relation to age. Lastly, the statistical association between the variables was assessed using hypothesis tests at a significance level P-value <0.05. All analyses were performed using SPSS, version 27.
Ethical Aspects
The present study was approved by the ethics committee of reference (protocol no. 23008 of 24/6/2021) and authorized by the Directorate General of the EMS. Only the study manager and collaborators had access to data in order to respect confidentiality, according to privacy regulations. The data were stored anonymously and transformed into assigned alphanumeric codes.
Results
In the months from January to May 2019, a total of 798 prehospital emergency care interventions were conducted by professionals of nurse-staffed ambulances and medical cars and related prehospital emergency care forms completed. Of these, 169 (21.2%) forms were excluded because 9 (1.1%) were very incomplete, 63 (7.9%) concerned patients <18 years of age and 97 (12.2%) reported patients who were not conscious and therefore unable to communicate the pain.
Demographic Characteristics of the Sample and Type of Prehospital Emergency Care Interventions
The study sample was composed of 629 people, equally distributed by sex: 310 males (49%) and 319 females (51%), with an average age of 64.2±22 SD years (range 18–108). Most emergency care operations were conducted by professionals of medical cars (56%, n = 349), while the remaining 44% (n = 277) by professionals of nurse-staffed ambulances. The prehospital triage colour code was registered on 487 prehospital emergency care forms, which in most cases was yellow (49.5%, n = 241) and green (46.8%, n = 228) and to a much lesser extent red (3.7%, n = 18).
The type of event was recorded in 614 prehospital emergency care forms; in 78% (n = 478) the event was related to a medical condition, whereas in the remaining cases the event was of traumatic origin (22%, n = 136). The average age of the subjects with trauma was 47.82±20.3 SD years, while that of patients with medical conditions was significantly greater: 68.81±19.9 SD years (t=−10.8, p<0.001). We performed a logistic regression and the results seem to suggest that as age increases so does the probability of presenting a medical condition (exp (B)=1.048, χ2 (1)=83.4, p<0.001).
First Assessment of Pain
Pain information was not collected (unknown or missing) in 24.5% (n = 154) of the prehospital emergency care forms, mainly on medical cars (64.7%) compared to nurse-staffed ambulances (32.5%) (χ2=11.38; p<0.001).
Among those with pain information collected, 46.7% (n = 222) of patients had pain, with a similar distribution in the different intensity classes (Table 1). Mild pain was most commonly observed in nurse-staffed ambulances, while moderate and severe pain was more frequent in medical cars (Table 2), with a statistically significant difference (χ2=13.1; p<0.005).
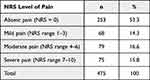 |
Table 1 Distribution of NRS Levels of Pain at the First Assessment |
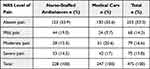 |
Table 2 Distribution of NRS Levels of Pain in Relation to the Prehospital Emergency Vehicle |
Many patients with a medical condition (64%) did not present pain, compared to only 18% of patients with traumatic injury (χ2=70.6; p<0.001) (Table 3). A simple linear regression was carried out to test if type of event significantly predicts pain. It was found that traumatic event was a significant predictor of pain (β =- 0.31, t=- 6.99, p<0.001).
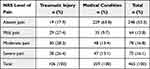 |
Table 3 Distribution of NRS Levels of Pain in Relation to Type of Event |
Pain had a similar prevalence between the two sexes (females 53%, n = 118; males 47%, n = 104); the mean scale score of pain in females was m = 5.26±2.4 SD and in males m = 4.91±2.6 SD, without a significant difference.
A statistically significant difference was observed in the relationship between pain and age (χ2=42.1; p<0.001): 66.4% (n = 71) of subjects in the age range 18 to 44 had pain, compared to only about 1/3 of the persons in the higher age ranges (Table 4). A simple linear regression was carried out to test if age significantly predicts pain. It was found that age significantly predicts pain, specifically, as age decreases pain increases (β=- 0.24, t=- 5.32, p<0.001).
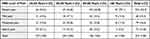 |
Table 4 Distribution of NRS Levels of Pain by Age Classes |
First Pharmacological Treatment of Pain and Adherence to the Clinical Care Algorithm
For 79.7% (n = 177) of persons suffering from pain, no pharmacological treatment was used, with a higher frequency when the emergency vehicle was a nurse-staffed ambulance rather than a medical car (86.7% vs 73.5%, χ2=14.08; p=0.007). As shown in Table 5, mild pain was never treated and moderate pain only in one case in the nurse-staffed ambulances. In severe pain, the nurses observed the instructions of the algorithm in 39.4% (n = 13) of cases. Mild and moderate pain was barely treated also in medical cars, whereas nearly half of severe pain cases received pharmacological treatment (Table 6). Pain was not treated according to the algorithm’s instructions in most cases both in the nurse-staffed ambulances (86.7%, n = 91) and in the medical cars (82.9%, n = 97) (Tables 5 and 6).
 |
Table 5 Pharmacological Treatment in Relation to Levels of Pain in Nurse-Staffed Ambulances |
 |
Table 6 Pharmacological Treatment in Relation to Levels of Pain in Medical Cars |
Pain was treated more frequently in cases of traumatic injuries (Pharmacological treatments 25.3% vs No treatment 74.7%) compared to medical conditions (Pharmacological treatments 17.7% vs No treatment 82.3%), especially when the level of pain was severe (p=0.001), where in almost all cases fentanyl was used (Table 7).
 |
Table 7 Pharmacological Treatment Distributed by Type of Event and Levels of Pain |
Among patients experiencing pain who did not receive a pharmacological treatment, the percentage of males and females was similar (females 52% vs males 48%). Among patients with severe pain, 45% of females and 41% of males received a pharmacological treatment and the pharmaceutical most utilized for both sexes was fentanyl (Table 8). For moderate pain, 15% of females and 10.2% of males received pharmacological treatment. Lastly, mild pain was not treated only in 5.8% of males.
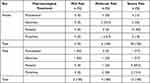 |
Table 8 Pharmacological Treatment Distributed by Levels of Pain and by Sex |
When considering severe pain, the 65–85 years age range was the class with the largest number of no treatments (Table 9). While analyzing pharmacological pain management, it was observed that in this age range, a similar number of each of the 4 pharmaceuticals was used, while in the younger age groups the use of fentanyl was clearly prevalent.
 |
Table 9 Pharmacological Treatment Distributed by Levels of Pain and by Age Classes |
Reassessment of Pain and Efficacy of Pharmacological Treatment
Pain reassessment was recorded only in 24.3% (n = 54) of the ascertained cases of pain. In patients assisted by professionals of nurse-staffed ambulances, the mean pain value decreased from the first assessment to after pharmacological treatment (m = 8.36±0.9 SD vs m = 4.18±2.2 SD), with a statistically significant difference (t-test=6.23, p<0.001). Similarly, in medical cars with both a doctor and a nurse, the mean pain value from the first assessment to after pharmacological treatment decreased (m = 7.25±1.7 SD vs m = 3.50±2.6 SD), with a statistically significant difference (t-test=5.14, p<0.001).
In females, the mean pain value decreased from the first assessment to after pharmacological treatment (m = 7.93±1.2 SD vs m = 4.29±2.7 SD), with a statistically significant difference (t-test=5.74, p<0.001). In males the mean pain value decreased from the first assessment to after pharmacological treatment (m = 7.56±1.9 SD vs m = 3.11±1.8 SD), with a statistically significant difference (t-test=5.67, p<0.001). No statistically significant differences in the mean pain were found between females and males who had received pharmacological treatment, either before or after receiving therapy (Pre: females m = 7.93±1.2 SD vs males m = 7.56±1.9 SD, t = 0.58, p=0.57; Post: females m = 4.29±2.7 SD vs m = 3.11±1.8 SD, t = 1.15, p=0.26).
Among patients who still had pain at the time of reassessment (n = 47), only one case was treated pharmacologically.
Discussion
This study investigated the approach to pain management by health-care professionals in a prehospital emergency care setting. We observed that a quarter of the prehospital emergency care forms analysed did not report any pain scale score. The result is in line with the percentage of incomplete prehospital emergency care paper forms collected in a retrospective study conducted in England (22.8%) and is slightly lower than that observed in a recent Danish study (32%).10,26 The reasons for not recording pain scores are different, from patients who did not suffer from pain to patients with pain that had not been documented, so this aspect must be taken into account when interpreting the data.10 However, the recording of pain data in first-level health interventions, as suggested by the guidelines of the European Society of Emergency Medicine (EUSEM), is the first requirement for effective pain management. In fact, pain assessment and documentation of pain scores improve the percentage of patients who receive analgesia.27,28
At the first assessment, almost half of the patients assessed (46.7%) had pain, thus confirming that it is a prevalent symptom in the prehospital emergency setting.28 The data is difficult to compare with other studies. In a register-based study conducted in Denmark that included patients receiving emergency care on both advanced and non-advanced vehicles, the percentage of patients with moderate or severe pain was 27.7%.10 In another study, investigations into specific patient groups, such as traumatized or infarcted patients, show an even higher prevalence of pain, 73.4% and 85.1%, respectively.26 In our study, we have observed that in patients with physical trauma the prevalence of pain was higher than in patients presenting a medical cause for the emergency call, with a high likelihood of moderate-to-severe pain, in line with other studies.6,9,29 The high prevalence of pain due to traumatic events is also confirmed by an Italian study conducted in a second-level ED.23
The greater prevalence of moderate and severe pain registered by medical cars seems plausible with the set criteria about which advanced prehospital first aid vehicles of an Italian Emergency Medical Service are sent to the emergency call.
We found no differences in the frequency and type of pain in relation to sex, in line with the literature.10,26,30 In accordance with other studies, pain was prevalent in younger age ranges.16,20
In our study, a very low percentage of patients with pain (20%) received pharmacological treatment before arrival in hospital, in accordance with a recent study.31 Similarly, a three-year retrospective study showed that only 15.6% of patients received prehospital pain medications.27 Despite the recognized harmful effects of pain undertreatment, in line with previous studies, our research confirms that oligoanalgesia remains a reality for many patients in prehospital setting.7,27,30 However, access to pain management is a human right and clinicians have an ethical responsibility to relieve pain,32 but effective pain control is a complex burden influenced by various types of barriers.33 Two recent scoping reviews found that patient, practitioner, and environmental factors influenced the administration and practice of prehospital analgesia.24,34 Among practitioner barriers, the accuracy of pain assessment is one of the main concerns, despite the advent of pain assessment tools, because of its subjective nature, the variability of expression and uncertainty of professionals.34,35
We found a major pharmacological undertreatment of pain in the nurse-staffed ambulances. This could be correlated to the fact that the decision to treat pharmacologically, in any case, depended on the telephone instructions of the operating center physician. Decision-making based on distance communication can be difficult, as documented in the literature,34 whereas the presence of the doctor in the medical cars made it possible to treat pain with medications other than the indication of algorithms.
Our data has shown how traumatic pain was more frequently treated compared to pain of medical origin, confirming that when there is a clear association of suggestive pain with a traumatic injury, professional are more willing to administer analgesia.35
In treated patients, pain decreased significantly in intensity, in both emergency vehicles, confirming that analgesia is an effective intervention in prehospital emergency care, although in almost all cases, we reported no adherence to the pharmacological treatment algorithm in both emergency vehicles.13,36
In addition, some studies suggest that males compared to females are more likely to receive opiate-based analgesia in prehospital setting, a finding which was not supported in this study.37,38
When considering severe pain, the age range (65–85 years) was the one with the most no treatments, probably due to patient factors that can constitute a barrier, such as case complexity, patient cooperation and attitudes towards treatment.34
In the context of this study, the algorithm limitations of infusing drugs at a slow rate, often longer than the time it takes to reach the emergency room, should be considered. We observed a low percentage of pain re-evaluation (24.3%) probably due to the fact that the ambulance had in the meantime arrived at the hospital emergency room. The ease of access and proximity to a hospital were identified as possible barriers to analgesia administration in the literature.34 However, as suggested by the EUSEM guidelines, once analgesia is provided, patients should be re-evaluated to ensure they have received relief.13
A recent Italian study (2021)14 has suggested the need for EMS to improve the appropriateness of standard intervention protocols for ambulance nurses, although in our experience the presence of a specific algorithm does not seem to have been sufficient in reducing the risk of oligoanalgesia.
In literature several solutions are proposed;34 among those most easily applicable in the context of this study are developing enhanced pain assessment technology tools and placing a greater emphasis on communication skills in order to support making decisions and providing just in time feedback. In accordance with most guidelines, intervention protocols should be supported by the implementation of appropriate strategies as well as specific education initiatives of proven effectiveness in improving pain management.13,24,39
Limits of the Study
The small sample size, the short observation time and the monocentric design are the main limits to the generalizability of this study results. Moreover, the failure to record pain scores in a quarter of the forms does not allow us to specify whether this omission was a real lack of pain assessment or lack of recording pain presence. Our research assumes that if an EMS health-care professional failed to record the pain scores on the form, assessment and treatment were not done. Another limit of this study is that of being constrained by the characteristics of the data collection tool supplied, which does permit us to obtain and analyze additional data. Nevertheless, to our knowledge, this is one of the very few studies examining the management of pain in the prehospital setting.
Implications for Emergency Clinical Care
The assessment and treatment of pain should be a priority for emergency nurses in the prehospital environment immediately after life-saving interventions. Leaving patients in pain all the way to the hospital can represent not only bad professional practice, but also a human rights violation with ethical and legal implications. Timely and effective analgesic treatment should therefore be a routine task, considering the efficacy, availability, and safety of the pharmacological treatments now available. In a prehospital setting, adequate analgesia facilitates transport problems and improves health outcomes. Unfortunately, our results confirm that pain is still a symptom that remains too far underrecognized, undervalued and undertreated, despite the availability of advanced emergency vehicles and specific algorithms for pain medication. The availability of electronic devices in place of paper forms could facilitate an accurate and timely recording of pain. Lastly, the importance and prevalence of the problem require more attention from health-care workers, both doctors and nurses. Clinical audits and retraining can be tools for raising awareness of staff for correct and effective pain management in a prehospital setting.
Conclusion
This retrospective analysis found that in the prehospital emergency care paper forms where pain was recorded at least half of the prehospital patients had mild, moderate or severe pain; unfortunately, in a quarter of the forms the data was not documented. Despite the presence of a specific pain treatment algorithm, 80% of persons of our sample were not pharmacologically treated, although analgesia is an effective and safe intervention. Pain, therefore, is confirmed as a prevalent symptom suffered by patients in prehospital emergency setting, but remains underrecognized, undervalued and undertreated with the risk of causing worse health outcomes. More appropriate intervention protocols in prehospital emergency care could be implemented to help health-care professionals improve pain management. Pain relief is a fundamental health-care intervention, focused on physical and mental health of the patient with many human rights implications and ethical concerns. Future studies conducted on sufficiently large and representative samples and focused on the assessment and treatment of pain in prehospital emergency health-care settings are needed, especially to understand possible barriers and enabling factors.
Abbreviations
EMS, Emergency Medical Service; NRS, Numeric Rating Scale; EUSEM, European Society of Emergency Medicine.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of Val Padana (protocol no. 23008 of 24/6/2021) and conducted in accordance with the Declaration of Helsinki. The research was carried out in compliance with all the applicable research ethics. The data was stored anonymously and identified on the basis of the assigned alphanumeric code. Furthermore, in compliance with the Italian legislation on the subject, based on Article 110 of Legislative Decree 196/2003, as amended by Legislative Decree 101/2018 “… Informed consent is also not necessary when, due to particular reasons, informing the interested parties is impossible or involves a disproportionate effort, or risks making it impossible or seriously jeopardizing the achievement of the purposes of the research …”, the informed consent was not collected.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Raja SN, Carr DB, Cohen M, et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–1982. doi:10.1097/j.pain.0000000000001939
2. Berry PH, Dahl JL. The new JCAHO pain standards: implications for pain management nurses. Pain Manag Nurs. 2000;1(1):3–12. doi:10.1053/jpmn.2000.5833
3. Ariès P, Montelescaut E, Pessey F, Danguy Des Déserts M, Giacardi C. Pre-hospital emergency medicine: pain control. Lancet. 2016;387(10020):747. doi:10.1016/S0140-6736(16)00325-1
4. Savoia G, Coluzzi F, Di Maria C, et al. Italian intersociety recommendations on pain management in the emergency setting (SIAARTI, SIMEU, SIS 118, AISD, SIARED, SICUT, IRC). Minerva Anestesiol. 2015;81(2):205–225.
5. McLean SA, Maio RF, Domeier RM. The epidemiology of pain in the prehospital setting. Prehosp Emerg Care. 2002;6(4):402–405. doi:10.1080/10903120290938021
6. Galinski M, Ruscev M, Gonzalez G, et al. Prevalence and management of acute pain in prehospital emergency medicine. Prehosp Emerg Care. 2010;14(3):334–339. doi:10.3109/10903121003760218
7. Albrecht E, Taffe P, Yersin B, Schoettker P, Decosterd I, Hugli O. Undertreatment of acute pain (oligoanalgesia) and medical practice variation in prehospital analgesia of adult trauma patients: a 10 yr retrospective study. Br J Anaesth. 2013;110(1):96–106. doi:10.1093/bja/aes355
8. Siriwardena AN, Asghar Z, Lord B, et al. Patient and clinician factors associated with prehospital pain treatment and outcomes: cross sectional study. Am J Emerg Med. 2019;37(2):266–271. doi:10.1016/j.ajem.2018.05.041
9. Schwerin DL, Mohney S EMS pain assessment and management; 2022. Treasure Island (FL): StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554543/.
10. Friesgaard KD, Riddervold IS, Kirkegaard H, Christensen EF, Nikolajsen L. Acute pain in the prehospital setting: a register-based study of 41.241 patients. Scand J Trauma Resusc Emerg Med. 2018;26(1):53. doi:10.1186/s13049-018-0521-2
11. Thomas SH, Shewakramani S. Prehospital trauma analgesia. J Emerg Med. 2008;35(1):47–57. doi:10.1016/j.jemermed.2007.05.041
12. Lenssen N, Krockauer A, Beckers SK, et al. Quality of analgesia in physician-operated telemedical prehospital emergency care is comparable to physician-based prehospital care - a retrospective longitudinal study. Sci Rep. 2017;7(1):1536. doi:10.1038/s41598-017-01437-5
13. Hachimi-Idrissi S, Dobias V, Hautz WE, et al. Approaching acute pain in emergency settings; European Society for Emergency Medicine (EUSEM) guidelines—part 2: management and recommendations. Intern Emerg Med. 2020;15(7):1141–1155. doi:10.1007/s11739-020-02411-2
14. Imbriaco G, Rondelli R, Maroni F, et al. Nurse-administered analgesic treatment in Italian emergency medical services: a nationwide survey. J Pain Res. 2021;14:1827–1835. doi:10.2147/JPR.S303998
15. Wilson JE, Pendleton JM. Oligoanalgesia in the emergency department. Am J Emerg Med. 1989;7(6):620–623. doi:10.1016/0735-6757(89)90286-6
16. Sobieraj DM, Martinez BK, Miao B, et al. Comparative effectiveness of analgesics to reduce acute pain in the prehospital setting. Prehospi Emerg Care. 2020;24(2):163–174. doi:10.1080/10903127.2019.1657213
17. Motov SM, Khan AN. Problems and barriers of pain management in the emergency department: are we ever going to get better? J Pain Res. 2008;2:5–11.
18. The Royal College of Emergency Medicine. Management pain in adults. Best Practice Guidelines; 2021. Available from: https://rcem.ac.uk/wpcontent/uploads/2021/10/RCEM_BPC_Management_of_Pain_in_Adults_300621.pdf.
19. Gausche-Hill M, Brown KM, Oliver ZJ, et al. An evidence-based guideline for prehospital analgesia in trauma. Prehosp Emerg Care. 2014;18(sup1):25–34. doi:10.3109/10903127.2013.844873
20. Kontinen V. Pain outside of the hospital: what is the situation in pre-hospital care, and how could it be improved? Scand J Pain. 2015;8(1):35–36. doi:10.1016/j.sjpain.2015.05.001
21. Brokmann JC, Rossaint R, Hirsch F, et al. Analgesia by telemedically supported paramedics compared with physician-administered analgesia: a prospective, interventional, multicentre trial. Eur J Pain. 2016;20(7):1176–1184. doi:10.1002/ejp.843
22. Marinangeli F, Narducci C, Ursini ML, et al. Acute pain and availability of analgesia in the prehospital emergency setting in Italy: a problem to be solved. Pain Pract. 2009;9(4):282–288. doi:10.1111/j.1533-2500.2009.00277.x
23. Mura P, Serra E, Marinangeli F, et al. Prospective study on prevalence, intensity, type, and therapy of acute pain in a second-level urban emergency department. J Pain Res. 2017;10:2781–2788. doi:10.2147/JPR.S137992
24. Lourens A, McCaul M, Parker R, Hodkinson P. Acute pain in the African prehospital setting: a scoping review. Pain Res Manag. 2019;2019:2304507. doi:10.1155/2019/2304507
25. Conferenza Permanente Per I Rapporti Tra Lo Stato Le Regioni E Le Province Autonome Di Trento E Bolzano. Accordo tra il Ministro della salute, le regioni e le province autonome sul documento di linee-guida sul sistema di emergenza sanitaria concernente:” Triage intraospedaliero (valutazione gravità all’ingresso) e chirurgia della mano e microchirurgia nel sistema dell’emergenza - urgenza sanitaria”; 2001. Available from: https://www.gazzettaufficiale.it/eli/id/2001/12/07/01A12203/sg.
26. Siriwardena AN, Shaw D, Bouliotis G. Exploratory cross-sectional study of factors associated with pre-hospital management of pain. J Eval Clin Pract. 2010;16(6):1269–1275. doi:10.1111/j.1365-2753.2009.01312.x
27. Hewes HA, Dai M, Clay Mann N, Baca T, Taillac P. Prehospital pain management: disparity by age and race. Prehosp Emerg Care. 2018;22(2):189–197. doi:10.1080/10903127.2017.1367444
28. Hachimi-Idrissi S, Coffey F, Hautz WE, et al. Approaching acute pain in emergency settings: European Society for Emergency Medicine (EUSEM) guidelines-part 1: assessment. Intern Emerg Med. 2020;15(7):1125–1139. doi:10.1007/s11739-020-02477-y
29. Ahmadi A, Bazargan-Hejazi S, Heidari Zadie Z, et al. Pain management in trauma: a review study. J Inj Violence Res. 2016;8(2):89–98. doi:10.5249/jivr.v8i2.707
30. Lourens A, Parker R, Hodkinson P. Prehospital acute traumatic pain assessment and management practices in the Western Cape, South Africa: a retrospective review. Int J Emerg Med. 2020;13(1):21. doi:10.1186/s12245-020-00278-w
31. Magnusson C, Carlström M, Lidman N, Herlitz J, Wennberg P, Axelsson C. Evaluation and treatment of pain in the pre-hospital setting. A comparison between patients with a Hip injury, chest pain and abdominal pain. Int Emerg Nurs. 2021;56:100999. doi:10.1016/j.ienj.2021.100999
32. Brennan F, Lohman D, Gwyther L. Access to pain management as a human right. Am J Public Health. 2019;109(1):61–65. doi:10.2105/AJPH.2018.304743
33. Lindbeck G, Shah MI, Braithwaite S, et al. Evidence-based guidelines for prehospital pain management: recommendations. Prehosp Emerg Care. 2022:1–10. doi:10.1080/10903127.2021.2018073
34. Teoh SE, Loh CYL, Chong RIH, et al. A scoping review of qualitative studies on pre-hospital analgesia administration and practice. Am J Emerg Med. 2022;57:81–90. doi:10.1016/j.ajem.2022.04.038
35. Iqbal M, Spaight PA, Siriwardena AN. Patients’ and emergency clinicians’ perceptions of improving pre-hospital pain management: a qualitative study. Emerg Med J. 2013;30:e18.
36. Friesgaard KD, Kirkegaard H, Rasmussen CH, Giebner M, Christensen EF, Nikolajsen L. Prehospital intravenous fentanyl administered by ambulance personnel: a cluster-randomised comparison of two treatment protocols. Scand J Trauma Resusc Emerg Med. 2019;27(1):11. doi:10.1186/s13049-019-0588-4
37. Bendall JC, Simpson PM, Middleton PM. Prehospital analgesia in New South Wales, Australia. Prehosp Disaster Med. 2011;26(6):422–426. doi:10.1017/S1049023X12000180
38. Lord B, Bendall J, Reinten T. The influence of paramedic and patient gender on the administration of analgesics in the out-of-hospital setting. Prehosp Emerg Care. 2014;18(2):195–200. doi:10.3109/10903127.2013.856502
39. Marcotte A, Metz M. Pain management in the prehospital setting. research abstracts. J Emerg Nurs. 2004;30(5):403–404. doi:10.1016/j.jen.2004.07.009
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
