Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
PAID-PL—The Polish Version of the Problem Areas in Diabetes Scale: Perfect Reliability and a One-Factor Structure
Authors Cichoń E, Kiejna A , Gondek TM, Obrębski M , Sutkowska E , Lloyd CE, Sartorius N, Kokoszka A
Received 11 June 2021
Accepted for publication 1 September 2021
Published 2 November 2021 Volume 2021:14 Pages 4433—4441
DOI https://doi.org/10.2147/DMSO.S322850
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ming-Hui Zou
Ewelina Cichoń,1,2 Andrzej Kiejna,1,2 Tomasz M Gondek,3,4 Marcin Obrębski,5 Edyta Sutkowska,6 Cathy E Lloyd,7 Norman Sartorius,8 Andrzej Kokoszka5
1Department of Psychology, WSB University in Torun, Torun, Wroclaw, Poland; 2Department of Psychology, Faculty of Applied Studies, University of Lower Silesia, Wroclaw, Poland; 3Specialty Training Section, Polish Psychiatric Association, Wroclaw, Poland; 4Section on Education, World Psychiatric Association, Wroclaw, Poland; 5II Department of Psychiatry, Medical University of Warsaw, Warsaw, Poland; 6Department and Division of Medical Rehabilitation, Wroclaw Medical University, Wroclaw, Poland; 7Faculty of Health and Social Care, The Open University, Milton Keynes, UK; 8Association for the Improvement of Mental Health Programmes (AIMH), Geneva, Switzerland
Correspondence: Andrzej Kokoszka
II Department of Psychiatry, Medical University of Warsaw, 03-242 Kondratowicza 8 street, Warsaw, Poland
Tel/Fax +48 22 326 58 92
Email [email protected]
Purpose: The aim of this study was to assess the structure and validate the Polish version of the Problem Areas in Diabetes (PAID) scale, as the current translations of the original English version significantly vary in their psychometric properties.
Patients and Methods: Two hundred and sixteen consecutive Polish outpatients were invited to participate in this international cross-sectional study on depression in diabetes. The research was based on the demographic and clinical characteristics of the study population, including the level of glycated hemoglobin (HbA1c) and scores obtained in the Polish versions of the following questionnaires: PAID, World Health Organization-Five Well-Being Index (WHO-5), Patient Health Questionnaire 9 (PHQ-9). The psychiatric diagnosis was conducted with the use of Mini-International Neuropsychiatric Interview (M.I.N.I.).
Results: Exploratory factor analyses yielded a 1-factor structure that included all 20 items. The internal consistency of the Polish version of PAID was high (Cronbach α = 0.97). There were significant positive correlation between PAID and PHQ-9 and a negative correlation between PAID and WHO-5. We also observed a negative association between PAID scores and age and a positive correlation between PAID and HbA1c levels. Patients with depression reported significantly higher PAID scores as compared with those without depressive symptoms.
Conclusion: The Polish version of PAID has a one-factor structure and is a reliable, valid outcome measure for Polish outpatients with type 2 diabetes and it may constitute a useful instrument for screening for psychologic issues in diabetic patients during their appointments at the diabetes clinic.
Keywords: diabetes mellitus, type 2, emotional stress, depression, quality of life, problem areas in diabetes scale
Introduction
In 2017, 451 million people suffered from diabetes, and it is expected that 693 million individuals will be affected by diabetes in 2045.1,2 Diabetes frequently leads to serious, life-threatening, and often lethal cardiovascular complications, such as heart attack, stroke, neuropathy (nerve damage), nephropathy (kidney damage), and retinopathy (eye damage).3–5 The management of diabetes requires the daily monitoring of blood glucose levels and modification of the patient’s life style, which mainly means maintaining a healthy diet and doing regular physical exercise. Ultimately, adhering to these requirements poses a problem to many patients with diabetes.
Psychological factors indeed play a role in this process. In the current guidelines for diabetes treatment, ie, those endorsed by the American Diabetes Association,3 Polish Diabetes Association,4 and International Diabetes Federation,5 it is recommended to include the psychological aspects of diabetes in the diagnosis, treatment, and management of this disease.
The Problem Areas in Diabetes (PAID) scale is one of the most commonly used instruments to assess emotional distress related to problem areas that individuals with diabetes might have. It is a 20-item self-report measure that is applicable in both type 1 and type 2 diabetes.6 This tool is considered a recommended measure of diabetes-related emotional distress.6–8 It has been translated into 12 languages and validated in several countries.9–11 It also has short five- and one-item versions.12 The PAID-5 scale has high sensitivity (94%) and specificity (89%) for recognition of diabetes-related emotional distress. The one-item version, ie, PAID-1, has both sensitivity and specificity of approximately 80% for recognition of diabetes-related emotional distress. The PAID-5 total score very strongly correlates with the PAID-20 total score: r = 0.92, p < 0.001. PAID was originally constructed in English, as a single-domain structure in which all items dealing with emotional distress are related to problems connected with diabetes.13 Indeed, in a cross-cultural Dutch and United States study, principal component analyses confirmed the presence of a single, general 20-item factor; however, a four-factor solution was found in the exploratory factor analysis.6 The four factors were: negative emotions, treatment problems, food-related problems, and lack of social support.6 These dimensions have been widely applied in research that has been conducted in Dutch and in English, although the factorial structure of PAID seems culturally specific, eg, in a validation study of the Chinese version of PAID in Singapore, factor analysis resulted in a three-factor solution that included emotional and management problems, ability to cope with diabetes, and problems with social support.14 However, this solution is not congruent with the one-factor structure of the Chinese version of PAID in Taiwan.15 Siaw et al suggested that some clinical (eg, distress intensity, duration of diabetes) and cultural differences among Taiwanese and Singaporean patients with diabetes as well as variations in health-care settings might explain the differences in the factor structure of PAID.14 The three-factor solution was also found for the Swedish version of PAID, with the subdimensions being diabetes-related emotional problems, treatment-related problems, and social support–related problems.16 Similarly, in a Greek study that included two populations (ie, patients from an urban hospital and patients from a rural primary health-care center), factor analysis yielded three factors, ie, diabetes-related emotional problems, food-related problems, and social support–related problems.17 It is worth mentioning that although both the Greek and the Swedish versions of PAID have a three-factor structure, the Greek version includes food-related problems, whereas the Swedish version contains treatment-related problems instead. Conversely, the factor analysis of the Icelandic version of PAID revealed two factors related to distress in relation to life with diabetes and distress in relation to the management of diabetes.9 A similar finding was shown for the Turkish version of PAID, which identified a diabetes distress factor and a social support–related factor.10
Conversely, some studies disregard any potential cultural differences in the structure of PAID and follow the subdimensions identified by Snoek et al.6 For example, the factor analysis of the Brazilian PAID version yielded one component including all 20 items, but researchers decided to analyze the scale according to four subdimensions: 1) emotional problems, 2) treatment-related problems, 3) food-related problems, and 4) social support–related problems, despite the questionable reliability of three components (Cronbach α was 0.91, 0.60, 0.74, and 0.72, respectively).18 Gross et al.18 substantiated their decision by referring to the original version of PAID by Welch et al.13 Notably, the principal component analyses of the original version of PAID showed high item loadings (>0.30) for all 20 items on the first principal component (52.4% of the variance). The second component accounted for only 5.7% of the variance, and the third one, for 4.9%. These results confirmed the presence of a large, universal, general factor representing emotional functioning in diabetes and supported the use of a total score.13
Given that the factorial structure of PAID seems culturally specific, it is crucial to validate the language versions of this tool. PAID is a very easy to use, quick, and valuable measure of the emotional burden of living with diabetes. However, interpreting Polish translation of PAID according to a widely used four-factor structure can be nonapplicable to the Polish population. Inadequate use of the tool may lead toincomprehensible and wrong treatment decisions in clinical practice and generate artifacts in research. The Polish translation of PAID is based on the original American version by Polonsky et al.7 and was not fully validated. Back translation into English revealed no substantial differences. The reliability of PAID scales, as indicated by Cronbach α, was: 0.92 for the total PAID score, 0.90 for negative emotions, 0.46 for treatment-related problems, 0.57 for food-related problems, and 0.61 for lack of social support.19
Thus, the aim of this study was to conduct the factor analysis of the Polish version of PAID in order to compare its structure with that of other PAID translations and to verify the reliability of the measure and its subscales.
Materials and Methods
The data analyzed in this study were obtained from a Polish sample of consecutive participants of the International Prevalence and Treatment of Depression and Diabetes (INTERPRET-DD) collaborative study, which was conducted in 14 countries.20 A total of 216 participants (100 women, 116 men) aged 28 to 65 years (M = 57.42, SD = 7.32) took part in the study; the duration of diabetes among study participants ranged from 1 to 37 years (M = 9.47, SD = 7.10). Most participants used only oral hypoglycemic agents (n = 147; 68.1%). Twenty patients (9.3%) took only insulin, and 46 participants (21.3%) used both oral agents and insulin. Two participants (0.9%) did not use any antidiabetic medications. A single person missed information about medications taken (0.5%).
Procedure
The general procedure of the study is described in detail in Lloyd et al.20,21
The outpatient clinic attendees with type 2 diabetes were invited to participate in the study by their treating diabetologist. Eligible study participants were adults (aged 18–65 years) with type 2 diabetes diagnosed at least 12 months earlier who provided written informed consent. The exclusion criteria were: diagnosis of type 1 diabetes, communication or cognitive disorders, severe diseases (eg, cancer, stroke in the last 6 months), currently being an inpatient or having hospitalization scheduled (unless for the self-management of diabetes), being pregnant or having given birth in the last 6 months, and having a clinical diagnosis of dependency on alcohol or other substance (not tobacco) or schizophrenia.
Each eligible individual was asked about age, duration of diabetes, family history of diabetes, and presence or history of diabetes complications (cardiovascular disease, retinopathy, peripheral neuropathy, peripheral vascular disease, kidney disease and comorbidities), the most recent blood pressure measurement, HbA1c level, as well as height and weight, location of their accommodation (rural or urban area), level of education (no formal, some or completed primary school, some or completed secondary school, or higher education), marital status (married or cohabiting vs being single or widowed, or divorced), and financial status.
Then, each of the participants completed the set of questionnaires including: World Health Organization-Five Well-Being Index (WHO-5),22,23 Patient Health Questionnaire (PHQ-9),24,25 The Problem Areas in Diabetes (PAID)7,19 and the diagnosis of depression was conducted with the use of Mini-International Neuropsychiatric Interview (M.I.N.I.).26,27
Measures
The measures used for the analyses presented in this study included:
1) The Polish version of The World Health Organization-Five Well-Being Index (WHO-5) questionnaire,22,23 which was used to assess general emotional well-being. WHO-5 is a short, 5-item scale with satisfactory psychometric properties, in which participants rated how often they felt as described in the questionnaire in the previous 2 weeks using a 5-point Likert scale ranging from 0 (not at all) to 5 (all the time).23 The scores were summed up, with higher scores indicating better emotional well-being. In our study sample, Cronbach α was 0.87.
2) The Patient Health Questionnaire (PHQ-9)24,25 which was used to measure the severity of depressive symptoms. We employed the Polish version of PHQ-9.25 This tool includes 9 items assessed on a 4-point Likert scale. Participants estimated the frequency of occurrence of certain states ranging from 0 (not at all) to 3 (nearly every day). The Polish version of PHQ-9 has very good psychometric properties.25 In our study sample, Cronbach α was 0.86.
3) The Problem Areas in Diabetes (PAID) scale,7,19 which is a self-report questionnaire with 20 statements related to common negative emotions experienced by persons with diabetes (eg, “Feeling alone with diabetes” and “Worrying about the future and the possibility of serious complications”). Respondents rate each item on a 6-point Likert scale ranging from 1 (“Not a problem”) to 6 (“Serious problem”). The Joslin Diabetes Center, the owner of the PAID copyright, gave the senior author (AK) of this article the permission for the translation of PAID into Polish. Two persons translated it into Polish, and then a fully bilingual person (a psychologist) translated them back into English. Items that differed were discussed in a group of psychologists including the translators. The Polish version of PAID was submitted to the Joslin Diabetes Center. The reliability of PAID scales, as indicated by Cronbach α, was 0.92 for the total PAID score, 0.90 for negative emotions, 0.46 for treatment-related problems, 0.57 for food-related problems, and 0.61 for lack of social support.
4) The Mini-International Neuropsychiatric Interview (M.I.N.I.),26 Polish version 5.0.0.,27 which is a brief, widely used structured interview for the diagnosis of mental disorders. The applied version was based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) and International Classification of Diseases, Tenth Revision (ICD-10) criteria. There are no data on the psychometric properties of the Polish version, but the psychometric properties of the original, English-language version of M.I.N.I. were assessed as very good on the basis of the Composite International Diagnostic Interview (CIDI). Regarding the diagnosis of depression, the sensitivity and specificity of M.I.N.I. were 94% and 79%, respectively, and the kappa coefficient was 0.83. The instrument can be used by clinicians after a short training. A more intensive training is required for nonprofessionals.
Statistical Analysis
Statistical analyses were carried out using the SPSS version 25 for Windows. In order to identify the specific factors of the Polish version of PAID, exploratory factor analysis with an oblimin rotation was conducted, as we assumed that the factors were correlated. Due to non-normal data distribution, the principal axis factoring (PAF) method was applied. Cronbach α was calculated as a measure of internal consistency. To measure the concurrent and convergent validity, Pearson product-moment correlations were applied. We assumed that the PAID scores positively correlated with PHQ-9 results and negatively with WHO-5 scores. We also investigated whether individuals with both diabetes and depression had higher PAID scores.
Results
The mean total PAID score was 11.00 (SD = 14.22; range 0–62). The demographic, clinical, and psychologic characteristics of both male and female outpatients with diabetes are presented in Table 1. There were no sex differences in the mean PHQ-9 and WHO-5 scores, age, HbA1c levels (%), or the duration of diabetes (years). A statistically significant difference in PAID scores between men and women was observed and is shown in Table 1. The women (M = 13.47, SD = 15.86) showed greater emotional distress than men (M = 9.21, SD = 12.69), t(214) = 2.19; p = 0.03, Cohen d = 0.3.
 |
Table 1 Demographic, Clinical, and Psychological Characteristics of Male and Female Outpatients with Diabetes |
The analysis established a one-factor structure of the Polish version of PAID with eigenvalues >1.0 (10.08; the second highest value was 0.59). The examination of the scree plot also suggested a one-factor structure (see Figure 1).
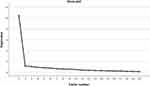 |
Figure 1 Scree plot of the Polish version of the PAID. |
The factor loadings for the one-factor solution are presented in Table 2. However, this solution indicated that the factorial loadings of a single item (15. “Feeling unsatisfied with your diabetes physician”) did not place above the recommended value of 0.3.28 The total variance of the one-factor solution was 50.13%. The final Polish version of PAID has been made available free of charge (see Supplemental Material 1. Problem Areas in Diabetes Scale).
 |
Table 2 The Results of Principal Axis Factoring and Factor Loadings of the 20 PAID Items (N = 216) for One Factor Solution |
In the next step, we assessed the reliability of the PAID scale by calculating Cronbach α reliability coefficients. We obtained a Cronbach α of 0.95. Thus, the reliability of the Polish version of the PAID scale was very high, which indicated the homogeneous structure of the tool. To compare our study version with the commonly used four-factor structure of PAID, we examined the reliability of the subdimensions by calculating Cronbach α reliability coefficients. The results indicated that Cronbach α yielded 0.92 for emotional problems, 0.43 for treatment-related problems, 0.74 for food-related problems, and 0.72 for social support–related problems. Thus, treatment-related problems demonstrated unsatisfactory reliability. Moreover, Cronbach α coefficients for food-related problems and social support–related problems barely met the threshold of reliability.
Then, convergent validity was examined by calculating product-moment correlations between PAID scores and other measures of effect. As expected, there was a significant, moderate positive correlation between PAID and PHQ-9 (r = 0.556; p < 0.001). The analysis of the association of WHO-5 and PAID scales showed a moderate, significant negative correlation (r = −0.524; p < 0.001). Thus, higher scores of emotional distress were associated with poorer quality of life and more severe depressive symptoms. We used the Mini-International Neuropsychiatric Interview (M.I.N.I.) to control for the occurrence of current depression. This procedure allowed us to compare the results obtained with PAID in patients with depression and patients without depression. As we assumed, patients suffering from a depressive disorder obtained PAID results higher (M = 28.69; SD = 20.50; Mrank = 168.44) than patients without depressive symptoms (M = 8.14; SD = 10.41; Mrank = 98.08), U = 1026.00; p < 0.001, gHedges = 1.65. We observed a weak, significant negative correlation between PAID scores and age (r = −0.223; p = 0.001). This implies that younger individuals reported higher emotional distress. There was also a weak positive correlation between PAID scores and HbA1c levels (%) (r = 0.204; p = 0.004) (see Table 3). Thus, patients with the highest HbA1c levels experienced the most negative emotions.
Discussion
The factorial structure of the Polish version of PAID is similar to that of the original version of the instrument described by Welch et al.13 Namely, the results indicated that the structure of the Polish version of PAID may have a one-factor representation. This has also been found in the analysis of both the Brazilian18 and the Taiwanese versions of PAID,15 which yielded a single factor with high internal consistency.15,18 In both the Greek and the Swedish versions of PAID, the factor analysis identified a three-factor structure yet consisting of different subdimensions. The two-factor solution was found for the Icelandic and Turkish versions of PAID. Our results support the conclusion from the review of the psychometric properties of PAID, which indicated that the internal structure of PAID varies across different populations. Our study confirmed the need for a proper assessment of psychometric properties of scales and questionnaires translated from other languages. It also makes the published results of international studies that used the four-factor structure of PAID questionable, eg, those conducted in Croatia, Denmark, Germany, Ireland, Israel, the Netherlands, and Poland. Further research should aim to investigate the determinants of those cross-cultural differences. Moreover, instruments that have been translated or adapted across languages should be tested for equivalence in order to provide valuable information for interpreting results obtained in different cultures.29–31 This assumption relates to some types of equivalence, such as conceptual equivalence.31 With respect to PAID, this type of equivalence refers to the ways in which problem areas in diabetes are conceptualized in various populations and in the values they assign to different domains of problems in diabetes. It seems that researchers automatically assume that domains that are relevant to problems among people with diabetes in one population will also be relevant in other cultures. However, the adapted or translated instruments should be verified for problematic components or aspects in the tool that may be inadequate in certain populations.30 Equivalence between different language versions of the same tool also refers to items.30 In addition, the relevance of PAID domains may vary across cultures, and the validity of the items as measures of particular problem areas may also differ, eg, the item “feel constantly concerned about eating” may not be applicable to cultures in which special food for diabetics is easily accessible. The item asking about feeling angry living with diabetes will not be appropriate in cultures in which the expression of anger is unacceptable. The failure to meet the assumption about equivalence may lead to test bias, which implies that inferences derived from test scores are not equivalent across various groups.32 The four-factor structure of PAID is widely used in research conducted among different populations. Taking the above into account, using the one factor, short, five-item version of PAID seems not only beneficial in terms of saving the time but also appropriate for inferences derived from studies carried out among different populations.
This study investigated both the reliability and the validity of PAID in the Polish patients with diabetes. The Polish version of PAID has a very good internal consistency and factorial validity.
In our study, its Cronbach α is 0.95. This result underlines the excellent internal consistency of the Polish version of PAID. Notably, in the original study on PAID, the researchers observed a very similar Cronbach α (0.94)13 and it has been also observed in other studies conducted in numerous populations.9–11,14–18 As mentioned before, the factorial structure of PAID is likely culture-specific.9–11,14–18 In our study, we investigated the reliability of the components of the PAID scale by calculating Cronbach α reliability coefficients. We found that Cronbach α yielded 0.92 for emotional problems, 0.43 for treatment-related problems, 0.74 for food-related problems, and 0.72 for social support–related problems. Some potential PAID factors demonstrated unsatisfactory convergent validity.
Furthermore, we found support for the convergent and discriminative validity of the Polish version of PAID. The total scores of the PAID scale positively correlated with PHQ-9 scores and negatively with WHO-5 scores, which confirmed the validity of PAID as a useful tool to evaluate both the well-being and the severity of depressive symptoms in persons with diabetes. However, further research is needed to examine the Polish tool version for long-term stability and responsiveness to change.
Although the present study had a cross-sectional design and did not include interventional strategies, we controlled for the occurrence of current depression by using the Mini-International Neuropsychiatric Interview (MINI). Patients with diabetes and a depressive disorder obtained PAID results that were higher than those of patients with diabetes and no depressive symptoms.
We also conducted an additional analysis of the collected data, which exceeded the set study objectives. In line with previous studies,10 we found sex differences in the PAID measures, eg, women reported greater distress. In addition, younger individuals reported higher emotional distress. These findings support previous research results.18 It has been suggested that emotional distress in younger individuals may be higher because of a lower ability to cope with the management of a chronic disease, such as diabetes. The disability to cope with a serious chronic condition among younger patients should be considered in the treatment process. It was shown that young people with diabetes had different health-care needs than older patients.33 Moreover, the most information and/or services related to type 2 diabetes are aimed at older adults.33 The low rate of participation in structured diabetes education sessions in the young population, caused by a short duration of diabetes in their life, may also lead to greater emotional distress. This suggests that the duration of diabetes may be linked to the severity of distress. Indeed, some researchers have shown that shorter diabetes duration is related to higher levels of distress in patients with type 2 diabetes.34 However, we noted no significant correlation between the disease and the PAID scores in our study. Nevertheless, our replication of the relationship between younger age and emotional distress indicates that young patients should, ideally, be routinely supported with psychologic interventions.
Conclusion
The Polish version of PAID is a one-factor, reliable, and valid measure for Polish patients with diabetes and it may be a useful tool for identifying those at increased risk of emotional distress.
Scales and questionnaires translated from other languages should be properly assessed with regard to their psychometric properties. Published results of international studies that used the four-factor structure of PAID are questionable without verification of its structure.
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Bioethics Committee of Medical University of Warsaw.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Acknowledgments
The authors would like to thank all the participants of this study. We thank the Association for the Improvement of Mental Health Programmes (AIMH) (and supported by AIMH and the collaborating institutions) for placing this study, which is part of the INTERPRET-DD study, under their aegis. The authors are grateful to the following individuals: Anna Krolicka-Deręgowska, Marta Jakubczyk, Paulina Ryta, and Magdalena Janusz from Wroclaw, Poland; Agnieszka Kazimierczyk, Agnieszka Misiołek, and Przemysław Łukasiewicz from Warsaw, Poland.
The authors express their gratitude to the Joslin Diabetes Center, the owner of PAID copyright, for permission to translate the original version of PAID and use its Polish version.
Funding
This study received no funding.
Disclosure
Dr Tomasz M Gondek reports personal fees from VP Valeant Polska, personal fees from Lundbeck Poland, personal fees from Janssen-Cilag Polska, personal fees from Apotex Poland (currently Aurovitas Pharma Polska), personal fees from EGIS Polska, personal fees from GL Pharma, outside the submitted work. The authors declare that the study was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi:10.1016/j.diabres.2018.02.023
2. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. doi:10.1016/j.diabres.2019.107843
3. American Diabetes Association [ADA]. Glycemic Targets: standards of Medical Care in Diabetes—2021. Diabetes Care. 2020;44(Suppl1):S73–S84. doi:10.2337/dc21-S006
4. Polish Diabetes Association. 2020 Guidelines on the management of diabetic patients: a position of Diabetes Poland. Clinical Diabetology. 2020;9(1):1–106. doi:10.5603/DK.2020.0001
5. International Diabetes Federation. IDF Diabetes Atlas.
6. Snoek FJ, Pouwer F, Welch GW, Polonsky WH. Diabetes-related emotional distress in Dutch and U.S. diabetic patients: cross-cultural validity of the problem areas in diabetes scale. Diabetes Care. 2000;23(9):1305–1309. doi:10.2337/diacare.23.9.1305
7. Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of Diabetes-Related Distress. Diabetes Care. 1995;18(6):754–760. doi:10.2337/diacare.18.6.754
8. Glasgow RE. Behavioral and psychosocial measures for diabetes care: what is important to assess. Diabetes Spectr. 1997;10(1):12–17.
9. Sigurdardottir AK, Benediktsson R. Reliability and validity of the Icelandic version of the problem area in diabetes (PAID) scale. Int J Nurs Stud. 2008;45(4):526–533. doi:10.1016/j.ijnurstu.2006.10.008
10. Huis In 't Veld EMJ, Makine C, Nouwen A, et al. Validation of the Turkish Version of the Problem Areas in Diabetes Scale. Cardiovasc Psychiatry Neurol. 2011;2011:1–6. doi:10.1155/2011/315068
11. Graue M, Haugstvedt A, Wentzel-Larsen T, Iversen MM, Karlsen B, Rokne B. Diabetes-related emotional distress in adults: reliability and validity of the Norwegian versions of the Problem Areas in Diabetes Scale (PAID) and the Diabetes Distress Scale (DDS). Int J Nurs Stud. 2012;49(2):174–182. doi:10.1016/j.ijnurstu.2011.08.007
12. McGuire BE, Morrison TG, Hermanns N, et al. Short-form measures of diabetes-related emotional distress: the Problem Areas in Diabetes Scale (PAID)-5 and PAID-1. Diabetologia. 2009;53(1):66–69. doi:10.1007/s00125-009-1559-5
13. Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabet Med. 2003;20(1):69–72. doi:10.1046/j.1464-5491.2003.00832.x
14. Siaw M, Tai B, Lee J. Psychometric Properties of The Chinese Version of Problem Areas In Diabetes Scale (Sg-Paid-C) Among High-Risk Polypharmacy Patients With Uncontrolled Type 2 Diabetes In Singapore. Value Health. 2016;19(7):A901. doi:10.1111/jdi.12556
15. Huang M-F, Courtney M, Edwards H, McDowell J. Validation of the Chinese Version of the Problem Areas in Diabetes (PAID-C) Scale. Diabetes Care. 2009;33(1):38–40. doi:10.2337/dc09-0768
16. Amsberg S, Wredling R, Lins P-E, Adamson U, Johansson U-B. The psychometric properties of the Swedish version of the Problem Areas in Diabetes Scale (Swe-PAID-20): scale development. Int J Nurs Stud. 2008;45(9):1319–1328. doi:10.1016/j.ijnurstu.2007.09.010
17. Papathanasiou A, Koutsovasilis A, Shea S, et al. The Problem Areas in Diabetes (PAID) scale: psychometric evaluation survey in a Greek sample with type 2 diabetes. J Psychiatr Ment Health Nurs. 2012;21(4):345–353. doi:10.1111/j.1365-2850.2012.01875.x
18. Gross CC, Scain SF, Scheffel R, Gross JL, Hutz CS. Brazilian version of the Problem Areas in Diabetes Scale (B-PAID): validation and identification of individuals at high risk for emotional distress. Diabet Res Clin Pract. 2007;76(3):455–459. doi:10.1016/j.diabres.2006.09.022
19. Kokoszka A, Jodko A, Power F, et al. Serious diabetes-specific emotional problems in patients with type 2 diabetes who have different levels of comorbid depression: a Polish study from the European Depression in Diabetes (EDID) Research Consortium. Eur Psychiatr. 2009;24:425–430. doi:10.1016/j.eurpsy.2009.04.002
20. Lloyd CE, Nouwen A, Sartorius N, et al. Prevalence and correlates of depressive disorders in people with Type 2 diabetes: results from the International Prevalence and Treatment of Diabetes and Depression (INTERPRET-DD) study, a collaborative study carried out in 14 countries. Diabet Med. 2018;35(6):760–769. doi:10.1111/dme.13611
21. Lloyd CE, Sartorius N, Cimino LC, et al. The INTERPRET-DD study of diabetes and depression: a protocol. Diabet Med. 2015;32(7):925–934. doi:10.1111/dme.12719
22. de Wit M, Pouwer F, Gemke RJBJ, Delemarre-van de Waal HA, Snoek FJ. Validation of the WHO-5 Well-Being Index in Adolescents With Type 1 Diabetes. Diabetes Care. 2007;30(8):2003–2006. doi:10.2337/dc07-0447
23. Cichoń E, Kiejna A, Kokoszka A, et al. Validation of the Polish version of WHO-5 as a screening instrument for depression in adults with diabetes. Diabetes Res Clin Pract. 2020;159:107970. doi:10.1016/j.diabres.2019.107970
24. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi:10.1046/j.1525-1497.2001.016009606.x
25. Cichoń E, Kiejna A, Kokoszka A, et al. People with diabetes need a lower cut-off than others for depression screening with PHQ-9. PLoS One. 2020;15:10. doi:10.1371/journal.pone.0240209
26. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a Structured Diagnostic Psychiatric Interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33.
27. Masiak M, Przychoda J. M.I.N.I. Mini International Neuropsychiatric Interview. Polish Version 5.0.0.1998. Klinika Psychiatrii Akademii Medycznej Lublin;1998.
28. Field A. Discovering Statistics Using IBM SPSS Statistics: And Sex and Drugs and Rock ‘N’ Roll. London: Sage Publications; 2013.
29. Geisinger KF. Cross-cultural normative assessment: translation and adaptation issues influencing the normative interpretation of assessment instruments. Psychol Assess. 1994;6(4):304–312. doi:10.1037/1040-3590.6.4.304
30. Hambleton RK. Guidelines for adapting educational and psychological tests: a progress report. Eur J Psychol Assess. 1994;10(3):229–244.
31. Herdman M, Fox-Rushby J, Badia X. A model of equivalence in the cultural adaptation of HRQoL instruments: the universalist approach. Qual Life Res. 1998;7(4):323–335. doi:10.1023/a:1024985930536
32. Sireci SG, Bastari B. Evaluating Construct Equivalence Across Adapted Tests. Paper Presented at the Annual Meeting of the American Psychological Association, August 14, 1998. San Francisco, CA; 1998.
33. Browne JL, Scibilia R, Speight J. The needs, concerns, and characteristics of younger Australian adults with type 2 diabetes. Diabet Med. 2013;30(5):620–626. doi:10.1111/dme.12078
34. Welch GW, Jacobson AM, Polonsky WH. The Problem Areas in Diabetes Scale. An evaluation of its clinical utility. Diabetes Care. 1997;20:760–766. doi:10.2337/diacare.20.5.760
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

