Back to Journals » International Journal of General Medicine » Volume 17
Overlap Between Gastroesophageal Reflux Disease and Functional Constipation and Associated Risk Factors Among the General Population in Saudi Arabia
Authors Al Jalal BA, Alnawah AK, Alturkie FM , Alqadhib KJ, Alabbadi MS, Ali SI, Al Hussaini HA
Received 16 October 2023
Accepted for publication 11 February 2024
Published 26 February 2024 Volume 2024:17 Pages 669—683
DOI https://doi.org/10.2147/IJGM.S443974
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Hossam El-Din Shaaban
Bashaeer Abdullh Al Jalal,1 Ahmed Khalid Alnawah,1 Fahad Mohammed Alturkie,1 Khalid Jafar Alqadhib,1 Mohammed Sami Alabbadi,1 Sayed Ibrahim Ali,2 Hessah Abdulaziz Al Hussaini1
1Department of Internal Medicine, College of Medicine, King Faisal University, Al Ahsa, 31982, Saudi Arabia; 2Department of Family and Community Medicine, College of Medicine, King Faisal University, Al Ahsa, 31982, Saudi Arabia
Correspondence: Bashaeer Abdullh Al Jalal, Email [email protected]
Introduction: Gastroesophageal reflux disease (GERD) and functional constipation (FC) are two common gastrointestinal disorders that affect many age groups in the community. A few studies were conducted to find the association between GERD and FC, but no study had been conducted in Saudi Arabia. Therefore, this study aims to find the overlap between GERD and FC and associated risk factors among the general population in the Eastern Province, Saudi Arabia.
Methods: A cross-sectional study was conducted in the eastern province of Saudi Arabia between August and September 2022. GERDQ and Rome IV criteria were used to collect the data with participants’ characteristics through an online questionnaire.
Results: Out of 2007 respondents, 1481 filled the required criteria, among them 320 (21.6%) had GERD, and 1292 (87.2%) respondents had FC based on the listed criteria. Eighty percent of respondents with GERD had overlapping FC. Men were more likely than women to experience this significant relationship (53.1% versus 46.9%).
Conclusion: There is a significant relationship between GERD and FC among the general population of the eastern province of Saudi Arabia. Consequently, this study could be used to improve the understanding of the overlapping between these gastrointestinal disorders and further new guidelines could be carried out to find the best treatment for these patients.
Keywords: GERD, functional constipation, overlap, Saudi Arabia
Introduction
Gastroesophageal reflux disease (GERD) is a widespread, chronic, and recurrent gastrointestinal disease that affects people worldwide, particularly in the Western world.1,2 GERD is a disorder in which stomach contents reflux into the esophagus, causing symptoms and/or complications or significant discomfort.3 The presence of typical mucosal damage visible during endoscopy and/or abnormal esophageal acid exposure indicated in a reflux monitoring study objectively confirms GERD.3 Given that GERD symptoms are nonspecific, they may coexist or be misidentified for those of other disorders, which implies the need for endoscopy and sometimes MII-ph impedance monitoring for patients without erosions to confirm the diagnosis.3,4 Age, obesity, lifestyle, and smoking are all risk factors.5 GERD is globally common, with an estimated GERD prevalence globally of 13.98%.1 Based on a study conducted in Saudi Arabia to evaluate the prevalence of GERD among the general population, 17.8% of the Saudi population had GERD.6 The impact of such a common disease on the patient’s health-related quality of life is significant (HRQL).7
On the other hand, constipation is a prevalent problem encountered in the field of gastroenterology.8 Functional constipation is a disorder, and it can be chronic when the duration of symptoms persists for more than three months.9 Initially, other organic etiologies (ie, colorectal cancer) should be excluded to diagnose functional constipation (FC).10 Constipation is characterized by infrequent bowel movements or challenges in effectively emptying the bowels. It manifests through symptoms such as hard stools, the need to strain during bowel movements, a feeling of blockage in the rectal area, incomplete evacuation, as well as abdominal discomfort and bloating.11 Lifestyle and dietary factors, specifically a low-fiber diet and insufficient water intake, are common causes of constipation.12 Patients with constipation experience low HRQL.9 The global prevalence of constipation in adults is estimated to be 16%.12 Self-perception, Rome III, and Bristol are three different criteria used by a study conducted in Riyadh, central Saudi Arabia to diagnose constipation among the general population, which showed a result of 43%, 60%, and 25%, respectively.13
Multiple studies were conducted globally to determine the association between GERD and constipation. In Japan, two studies were conducted to determine the relationship, and both reported positive findings.14,15 Constipation has also been linked to GERD and dyspepsia, with research in the United States finding that constipation was present in 5.7% of reflux patients and 3.9% of dyspepsia patients.16 Another study in Nord-Trondelag found that severe GERD symptoms were associated with constipation symptoms in 39% of the patients.17 In southeastern Iran, a study was conducted to investigate the prevalence and associated risk factors related to chronic constipation, and they found chronic constipation is associated with GERD.18 In Korea, a study was conducted among patients who have constipation and found that there is a common overlap between GERD and dyspepsia among these patients.19 In children, a combination of GERD and FC has been reported.20,21
To the best of our knowledge, there have been few studies published globally about the overlap between GERD and constipation, and no published research has been undertaken in Saudi Arabia. This overlap is useful in the treatment of these diseases since GERD and constipation are common gastrointestinal diseases in Saudi Arabia.6,13
This study aimed to identify the overlap between GERD and constipation among the general population in the eastern province of Saudi Arabia. In addition, we aimed to explore the prevalence of GERD and constipation separately in the same population.
Materials and Methods
Study Design and Participants
A cross-sectional study was conducted from August 10 to September 13, 2022, in the eastern province of Saudi Arabia with an estimated population of 5,148,598 according to the General Authority for Statistics in Saudi Arabia 2019.22 Using the Raosoft website, the sample size was determined in accordance with a 95% confidence level, 5% margin of error, and a 50% predicted frequency; the minimum number of participants required for this study was 385. Therefore, 2007 participants were enrolled in this study randomly using a convenience sampling technique. The study was approved by the Deanship of scientific research of King Faisal University, reference number (KFU-REC-2022- MAY – ETHICS28).
It is a self-administered online questionnaire was made by using Google form as open-access and was distributed to the general population living in different cities of the eastern province of Saudi Arabia by data collectors in each city with reminders using different social media platforms and during different time periods to minimize selection bias. Participants were asked to send the survey with their peers and the researcher also ensured that the survey had reached different age groups and different classes of society to ensure that the study population would be representative of Saudi Arabia’s eastern province. The inclusion criteria were all people aged 18 or above who provided informed consent and were living in the eastern province of Saudi Arabia. Exclusion criteria were people not living in the Eastern Province, aged less than 18, inability to complete the questionnaire, pregnant females, those having gastrointestinal cancer, inflammatory bowel disease, and open abdominal surgery except appendicitis.
Study Tool
The researchers used prior validated questionnaires to create a survey; GERD questionnaire for GERD and a modified version of ROME IV criteria for functional constipation.23,24 In line with the absence of a validated Arabic version of these surveys, the researchers translated them into Arabic, and then 10 bilingual gastroenterologist consultants’ opinion was taken, and some modifications were made accordingly. Additionally, the reliability of the questionnaire was checked using Cronbach’s alpha and the result showed that the value of Cronbach’s alpha was 0.892, which implies that the questionnaire is highly reliable.
The survey consisted of multiple sections starting with instructions, the informed consent statement, and screening for people who did not meet the inclusion criteria. The participant demographic and medical data were also collected in the second section, including (weight, height, smoking status, marital status, nationality, educational level, current job, monthly income, city of living, self-perception of constipation, constipation medication usage including types, and gastric medication usage). The third section assessed GERD prevalence, and the GERD questionnaire (GERDQ) was used to achieve the study objectives.23 The GERDQ questionnaire includes six questions, of which four are positive predictors (heartburn, regurgitation, sleep distribution owing to heartburn and/or regurgitation, over the counter (OTC) medication usage) and two are negative predictors (nausea, epigastric pain). For the positive predictors, a Likert scale was utilized with scoring as follows: 0 = none; 1 = 1 day; 2 = 2–3 days; and 3 = 4–7 days; the opposite scoring scale was used for the negative predictors (3 = none). The respondent answered the questions regarding the mentioned points for the last week. Eight was the cut point for diagnosing the respondent with GERD. For GERDQ, the specificity and sensitivity are 71% and 65%, respectively.23 The last section was for assessing the prevalence of constipation, and a modified version of ROME IV criteria was used for that.24 These criteria diagnose the patient with constipation if they have symptoms for the last three months that started at least six months ago and it has six items in which the respondent has to select the statement if he had the symptom mentioned for more than one-fourth of the defecation including (straining, lumpy or hard stool, the sensation of incomplete evacuation, the sensation of anorectal blockage, using manual maneuver) and (less than three weekly spontaneous bowel movements). Each statement holds one point, and two or more points are needed for the diagnosis.
Statistical Analysis
The Statistical Package for Social Sciences (SPSS) computer program version 26, which is used for quantitative statistical analysis, was employed after the data had been first exported to Microsoft Excel. Descriptive statistics were used for each variable. To explore the relationship between qualitative items, a chi-square test was used. The statistically significant P value was considered in the case of 0.05 or less.
Results
Participants’ Characteristics
The sociodemographic characteristics of participants are presented in Table 1. Two thousand and seven people filled the questionnaire, among them 1481 were included in the study after excluding people who did not meet the inclusion criteria and people who were part of the pilot study. Six hundred and seventy-three (45.4%) were males, and 808 (54.6%) were females. Approximately half (46%) of the participants belong to the youngest age group (18–29 years old). More than half (54.2%) of the participants were married. Most of the participants (97.7%) were Saudis. About 31.5%, 37.2%, and 22.1% of the participants were students, employees, and unemployed, respectively. Nearly half (49.6%) of the participants had a bachelor’s level of education. The majority of participants (85.3%) were non-smokers. More than half (54.6%) of the participants were receiving less than 5000 SAR monthly income. About 38.6% of participants were from Al-Ahsa city, 20.4% from Dammam, and 19.6% from Qatif. Regarding body mass index (BMI), 6.8% were underweight, 40.8% were within normal weight, 29.7% were overweight, and 22.7% were obese. Regarding comorbidities, 4% had diabetes mellitus, 4.6% had hypertension, and 3.6% had hemorrhoids.
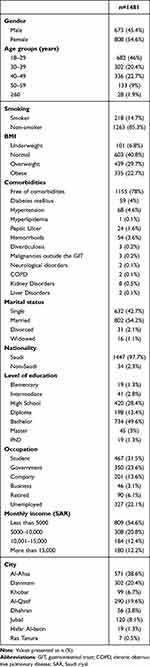 |
Table 1 Participants’ Sociodemographic Characteristics |
Gastroesophageal Reflux Disease Prevalence
Three hundred and twenty (21.6%) of the respondents had GERD based on GERDQ cut point. Among those, 50.9% were males, 37.5% were young (18–29 age group), and 59.7% were married. Nearly half (49%) had a bachelor’s level of education. About 25.6%, 46.2%, and 28.1% were students, employed, and unemployed, respectively. Regarding BMI, 6.2% were underweight, 41% were within normal weight, 25.6% were overweight, and 26.5% were obese. About 36.2% were using gastric medications. Moreover, 9% were using constipation medications. Figure 1 shows the frequency of reported symptoms. Approximately one-fifth (17.8%) were smokers. Table 2 demonstrates the factors associated with GERD. We observed old age group (≥60 years old) (p=0.007), male gender (p=0.026), living in Khobar (p=0.005), diverticulosis and other comorbidities as presented in Table 3 (p<0.001), and using gastric medications (p<0.001), and constipation medications (p=0.003), to be significantly related to GERD. While BMI (p=0.155), smoking (p=0.078), marital status (p=0.062), level of education (p=0.840), occupation (p=0.057), and monthly income (p=0.762) were found to be insignificant.
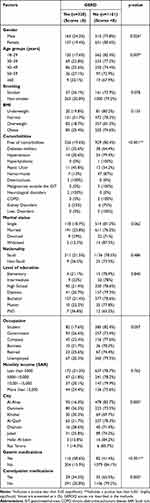 |
Table 2 Factors Associated with GERD |
 |
Table 3 Factors Associated with Functional Constipation |
Functional Constipation Prevalence
One thousand two hundred and ninety-two (87.2%) respondents had FC based on ROME IV criteria. Compared to males, the prevalence of FC was higher in females (52.5% versus 47.5%). Nearly half (48.2%) were young (18–29 age group), 52.4% were married, and 48.7% had bachelor’s education. Only a small percentage (8.3%) of constipated respondents were using constipation medications. Of those who used constipation medications, 53.6%, 36.58, and 6.5% used fibers, laxatives, and enemas, respectively. Figure 2 shows the frequency of different symptoms according to ROME IV criteria. The most reported symptom was the sensation of anorectal obstruction/blockage (80.1%). Significantly, one-third (34.5%) of participants never perceived themselves to have constipation when asked about their self-perception (p<0.001). Table 3 demonstrates the factors associated with FC. We examined the relationship between FC with other factors. We found male gender (p<0.001), underweight (p=0.046), young age group (p<0.001), single (p=0.001), diploma education (p=0.037), and students (p=0.001) and using gastric medications (p=0.046) to be significantly related to constipation. Significant comorbidities associated with FC are presented in Table 3 (p<0.001). Surprisingly, not using medications for constipation was also significant (p<0.001), while smoking (p=0.289), monthly income (p=0.087), and city of living (p=0.529) were found to be insignificant.
 |
Figure 2 Frequency of symptoms according to Rome IV to assess functional constipation. Notes: Symptoms experienced more than 25% of defecations in the last 3 months that started at least 6 months ago. |
GERD and FC Relationship
We found a significant association between GERD and FC (OR = 0.483, 95% CI 0.347–0.672, p<0.001), Table 4. Furthermore, 80% of respondents with GERD had associated constipation. Compared to women, men had a higher rate of overlap (53.1% versus 46.9%). Regarding BMI, 7.8% were underweight, 42.9% had normal BMI, 23.8% were overweight, and 25% were obese. Young age group (18–29 years old) had a high prevalence of overlap (41.4%). Approximately, one-fifth (17.9%) were smokers. More than half (57.8%) were married, and nearly one-third (39%) were single. Nearly half (48.8%) were bachelor educated. About 46.5% were employed, 26.5% were students, and 27% were unemployed. One-third (34%) were using gastric medications. We further investigated to find the association with other factors. Table 5 demonstrates the factors associated with the overlap. We observed male gender (p=0.007), using gastric medications (p<0.001), diverticulosis (p<0.001), living in Khobar (p=0.038) to be significantly related with the overlap. While age (p=0.196), BMI (p=0.162), marital status (p=0.298), level of education (p=0.827), occupation (p=0.239), monthly income (p=0.710), smoking (p=0.107), and using constipation medications (p=0.461) were found to be insignificant.
 |
Table 4 GERD and FC Overlap |
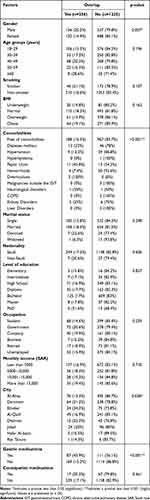 |
Table 5 Factors Associated with the Overlap Between GERD and FC |
Discussion
Our study provides valuable insights into the association between gastroesophageal reflux disease (GERD), functional constipation, and related risk factors among the general population of Saudi Arabia. A significant portion of the participants fell within the young adult age group, indicating that the onset and prevalence of GERD and constipation may be influenced by age-related factors. Moreover, the diverse occupational and educational backgrounds observed among the participants underscore the importance of considering lifestyle and socio-economic factors in understanding these conditions. The prevalence of non-smokers among the participants suggests a possible protective effect against GERD and constipation, as smoking is a known risk factor for gastrointestinal diseases.25,26
Geographic variations in participant distribution across cities in Saudi Arabia imply the influence of regional factors on these conditions. These factors could range from dietary preferences to environmental exposures. The presence of comorbidities like diabetes mellitus, hypertension, and hemorrhoids among a small percentage of participants emphasizes the need for comprehensive assessments. These conditions often intersect with GERD and constipation, suggesting potential interactions that warrant further investigation.
Regarding the prevalence of GERD and its associated risk factors. Among the respondents, 21.6% were identified as having GERD based on the GERDQ cut point. Notably, this condition affected a diverse demographic. This suggests that GERD might not be strongly associated with socio-economic factors in this population. Furthermore, the study identified several factors significantly associated with GERD, including old age, male gender, living in Khobar, the presence of comorbidities like diverticulosis, and the use of gastric medications and constipation medications. These findings suggest that there may be a complex interplay of lifestyle, geographic, and medical factors contributing to GERD prevalence in Saudi Arabia.27
Regarding the prevalence of functional constipation (FC) and its associated risk factors within this population. FC was more prevalent among females compared to males. This gender discrepancy suggests a potential gender-related susceptibility to constipation.28 FC was notably prevalent among young adults, with 48.2% falling into this age group. This age-related pattern is consistent with the study conducted by Lim et al (2016), which indicated a higher incidence of FC among young adults in similar populations.29 However, the surprising finding that 34.5% of participants never perceived themselves as having constipation, despite meeting the ROME IV criteria, raises questions about the awareness and understanding of this condition among the Saudi population. Regarding factors associated with FC, the study identified several significant correlations. Male gender, underweight status, being single, having a diploma-level education, being a student, and using gastric medications were all significantly related to constipation. Additionally, comorbidities were strongly associated with FC, highlighting the importance of considering the broader health context when addressing constipation in this population.
The significant association observed between gastroesophageal reflux disease (GERD) and functional constipation (FC) in this study. In practical terms, this suggests that there may be some shared factors or mechanisms between these two gastrointestinal conditions that result in a relationship.14 It is important to note that while GERD involves the regurgitation of stomach acid into the esophagus, often causing heartburn and discomfort,30 FC is characterized by infrequent bowel movements and difficulty passing stool.31 The correlation between GERD and FC found in this study aligns with prior research by Ahmadipour et al (2022), reinforcing the notion that these two conditions may have interconnected factors or pathways influencing their occurrence.21 However, further investigation is needed to elucidate the underlying mechanisms and clinical implications of this relationship, which could potentially inform preventive and treatment strategies for individuals with these gastrointestinal conditions.
The observation that men exhibited a higher rate of overlap between gastroesophageal reflux disease (GERD) and functional constipation (FC) (53.1%) compared to women (46.9%) in our study is an intriguing finding. This gender difference suggests that there might be distinct physiological, hormonal, or lifestyle factors at play that influence the co-occurrence of these two gastrointestinal conditions. It is essential to delve deeper into this gender-related variation in future research to uncover the underlying mechanisms driving this difference. Such investigations could explore hormonal influences, dietary habits, stress levels, or even genetic predispositions that might contribute to the observed variation. Understanding these factors could have significant implications for tailoring diagnostic and treatment approaches that are more gender-specific, ultimately improving the management of GERD and FC for both men and women.
Younger individuals, particularly those in the 18–29 age group, exhibited a higher prevalence of overlap between gastroesophageal reflux disease (GERD) and functional constipation (FC). This suggests that there may be age-specific factors or lifestyle influences that contribute to this co-occurrence in younger adults.32 While the distribution of body mass index (BMI) categories and age did not show significant associations with this overlap, it is important to note that these findings may indicate the complexity of the relationship between age, BMI, and the comorbidity of GERD and FC. Future research should delve deeper into understanding the age-specific risk factors that might be driving this phenomenon, such as dietary choices, physical activity levels, or hormonal changes.
Similarly, the use of gastric medications appears to have a significant impact on this relationship, potentially indicating a link between the management of GERD symptoms and the development of FC.33 The influence of geographic location, particularly living in Khobar, underscores the importance of regional variations in healthcare practices, environmental factors, or dietary habits that could contribute to the observed overlap. Understanding these lifestyle and regional nuances is crucial for tailoring interventions and treatment strategies that account for these specific influences, ultimately leading to more effective management of GERD and FC for individuals in different contexts.
The non-significant associations between sociodemographic factors, including marital status, level of education, occupation, monthly income, the use of constipation medications, tobacco smoking, and the overlap between gastroesophageal reflux disease (GERD) and functional constipation (FC) in our study indicate that these variables may not be primary determinants of the association between these gastrointestinal conditions. This finding suggests that the co-occurrence of GERD and FC may be influenced more by other factors such as lifestyle choices, geographic location, or perhaps physiological mechanisms, rather than sociodemographic characteristics.34 This highlights the complexity of these conditions and the need to consider a broader set of factors when studying their relationship. Future research could further explore the interplay between these sociodemographic variables and other potential determinants to gain a more comprehensive understanding of the factors contributing to the overlap between GERD and FC.
This study has several limitations that should be acknowledged. Firstly, the reliance on a questionnaire-based survey may introduce sampling and recall bias, potentially affecting the representativeness and accuracy of reported data. The cross-sectional design limits the ability to establish causality and track changes over time, while the exclusive focus on self-reported symptoms and medication use may not align with clinical diagnoses, potentially introducing misclassification bias. In addition, confirmatory diagnostic tests were not employed in our study to diagnose GERD, FC, and comorbidities. Furthermore, the present study acknowledges the challenge posed by selection bias, given that the sample was derived exclusively from one province in Saudi Arabia. Therefore, it is imperative to approach the generalization of the findings with caution and engage in a thoughtful discourse regarding their applicability to broader populations. The possibility of multi-collinearity among risk factors and potential non-response bias also warrant consideration.
Conclusion
In the current study, the frequency of GERD was reported as similar to the national range, whereas the frequency of constipation was higher than the national range. However, a different diagnostic tool may be needed to confirm it. The results revealed association between GERD and constipation in Eastern Province, Saudi Arabia. Many factors related to this association were identified, namely male gender, use of gastric medications, diverticulosis, as well as the self-perception of sometimes being constipated. To facilitate the treatment of patients with both diseases, it is important to attract the attention of physicians and provide them with new guidelines. Additionally, promoting research collaboration among healthcare professionals specializing in these conditions can deepen the understanding and lead to innovative treatment approaches. It can significantly improve patient outcomes and quality of life for individuals affected by the association between these diseases.
Data Sharing Statement
The data presented in this study are available within the paper.
Ethical Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of King Faisal University (KFU-REC-2022- 321MAY-ETHICS28, data of approval 22/05/2022) and all the patients have provided informed consent.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Deanship of Scientific Research, Vice Presidency for Graduate Studies and Scientific Research, King Faisal University, Al Ahsa, Kingdom of Saudi Arabia (Grant No. 5821).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Nirwan JS, Hasan SS, Babar ZUD, Conway BR, Ghori MU. Global Prevalence and Risk Factors of Gastro-oesophageal Reflux Disease (GORD): systematic Review with Meta-analysis. Sci Rep. 2020;10(1):5814. doi:10.1038/s41598-020-62795-1
2. Antunes C, Aleem A, Curtis SA. Gastroesophageal Reflux Disease. StatPearls Publishing; 2023. Available from: http://www.ncbi.nlm.nih.gov/books/NBK441938/.
3. Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol. 2022;117(1):27–56. doi:10.14309/ajg.0000000000001538
4. Marabotto E, Savarino V, Ghisa M, et al. Advancements in the use of 24-hour impedance-pH monitoring for GERD diagnosis. Curr Opin Pharmacol. 2022;65:102264. doi:10.1016/j.coph.2022.102264
5. Al Ghadeer HA, Alabbad ZE, AlShaikh SB, et al. Prevalence of Gastroesophageal Reflux Disease and Associated Risk Factors in the Eastern Region, Saudi Arabia. Cureus. 2014;13(11):e19599. doi:10.7759/cureus.19599
6. Al-Zahrani S, Mohamed M, Mohammed A, et al. Gastroesophageal reflux disease and heartburn among the general population of Saudi Arabia. IJMDC. 2019:933–940. doi:10.24911/IJMDC.51-1567426442
7. Moraes-Filho JPP, Domingues G, Chinzon D, Roveda F, Lobão Neto AA, Zaterka S. IMPACT OF HEARTBURN AND REGURGITATION ON INDIVIDUALS’ WELL-BEING IN THE GENERAL POPULATION: a BRAZILIAN NATIONAL SURVEY. Arq Gastroenterol. 2021;58:5–9. doi:10.1590/S0004-2803.202100000-03
8. Milosavljevic T, Popovic DD, Mijac DD, Milovanovic T, Krstic S, Krstic MN. Chronic Constipation: gastroenterohepatologist’s Approach. Dig Dis. 2022;40(2):175–180. doi:10.1159/000516976
9. Gray JR. What is chronic constipation? Definition and diagnosis. Can J Gastroenterol. 2011;25(SupplB):7B–10B.
10. Aziz I, Whitehead WE, Palsson OS, Törnblom H, Simrén M. An approach to the diagnosis and management of Rome IV functional disorders of chronic constipation. Expert Rev Gastroenterol Hepatol. 2020;14(1):39–46. doi:10.1080/17474124.2020.1708718
11. Sadler K, Arnold F, Dean S. Chronic Constipation in Adults. Am Fam Physician. 2022;106(3):299–306.
12. Forootan M, Bagheri N, Darvishi M. Chronic constipation. Medicine. 2018;97(20):e10631. doi:10.1097/MD.0000000000010631
13. Alhusainy YA, Alhowaish NY, Alorabi HZ, et al. Symptoms and Prevalence of Constipation among Adult Population of Riyadh City: an Internet Based Survey. Egypt J Hosp Med. 2018;70(8):1317–1322. doi:10.12816/0044641
14. Ogasawara N, Funaki Y, Kasugai K, et al. Overlap Between Constipation and Gastroesophageal Reflux Disease in Japan: results From an Internet Survey. J Neurogastroenterol Motil. 2022;28(2):291–302. doi:10.5056/jnm21065
15. Momma E, Koeda M, Tanabe T, et al. Relationship between gastroesophageal reflux disease (GERD) and constipation: laxative use is common in GERD patients. Esophagus. 2021;18(1):152–155. doi:10.1007/s10388-020-00770-5
16. Locke GR, Zinsmeister AR, Fett SL, Melton LJ, Talley NJ. Overlap of gastrointestinal symptom complexes in a US community. Neurogastroenterol Motil. 2005;17(1):29–34. doi:10.1111/j.1365-2982.2004.00581.x
17. Jansson C, Nordenstedt H, Wallander MA, et al. Severe symptoms of gastro-oesophageal reflux disease are associated with cardiovascular disease and other gastrointestinal symptoms, but not diabetes: a population-based study. Aliment Pharmacol Ther. 2008;27(1):58–65. doi:10.1111/j.1365-2036.2007.03537.x
18. Moezi P, Salehi A, Molavi H, et al. Prevalence of Chronic Constipation and Its Associated Factors in Pars Cohort Study: a Study of 9000 Adults in Southern Iran. Middle East J Dig Dis. 2018;10(2):75–83. doi:10.15171/mejdd.2018.94
19. Park KS, Jee SR, Lee BE, et al. Nationwide Multicenter Study for Overlaps of Common Functional Gastrointestinal Disorders in Korean Patients With Constipation. J Neurogastroenterol Motil. 2017;23(4):569–577. doi:10.5056/jnm17033
20. Baran M, Cagan Appak Y, Karakoyun M, Yalcinkaya S, Eliacik K, Dundar BN. The overlap of gastroesophageal reflux disease and functional constipation in children: the efficacy of constipation treatment. Eur J Gastroenterol Hepatol. 2017;29(11):1264–1268. doi:10.1097/MEG.0000000000000979
21. Ahmadipour S, Salami-Khaneshan A, Farahmand F, Baharvand P. Co-occurrence of childhood functional constipation and gastroesophageal reflux disease (GERD). Ann Med Surg Lond. 2022;74:103302. doi:10.1016/j.amsu.2022.103302
22. GASTAT. Accessed 2022. Available from: https://database.stats.gov.sa/home/indicator/410
23. Jones R, Junghard O, Dent J, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther. 2009;30(10):1030–1038. doi:10.1111/j.1365-2036.2009.04142.x.
24. Drossman DA. Functional Gastrointestinal Disorders: history, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016. doi:10.1053/j.gastro.2016.02.032
25. Berkowitz L, Schultz BM, Salazar GA, et al. Impact of Cigarette Smoking on the Gastrointestinal Tract Inflammation: opposing Effects in Crohn’s Disease and Ulcerative Colitis. Front Immunol. 2018;9:74. doi:10.3389/fimmu.2018.00074
26. Taraszewska A. Risk factors for gastroesophageal reflux disease symptoms related to lifestyle and diet. Rocz Panstw Zakl Hig. 2021;72(1):21–28. doi:10.32394/rpzh.2021.0145
27. Alsuwat OB, Alzahrani AA, Alzhrani MA, Alkhathami AM, Mahfouz MEM. Prevalence of Gastroesophageal Reflux Disease in Saudi Arabia. J Clin Med Res. 2018;10(3):221–225. doi:10.14740/jocmr3292w
28. Narayanan SP, Anderson B, Bharucha AE. Sex- and Gender-Related Differences in Common Functional Gastroenterologic Disorders. Mayo Clin Proc. 2021;96(4):1071–1089. doi:10.1016/j.mayocp.2020.10.004
29. Lim YJ, Rosita J, Chieng JY, Hazizi AS, Prevalence T. Symptoms Characteristic of Functional Constipation Using Rome III Diagnostic Criteria among Tertiary Education Students. PLoS One. 2016;11(12):e0167243. doi:10.1371/journal.pone.0167243
30. Clarrett DM, Hachem C. Gastroesophageal Reflux Disease (GERD). Mo Med. 2018;115(3):214–218.
31. Andrews CN, Storr M. The pathophysiology of chronic constipation. Can J Gastroenterol. 2011;25 Suppl B(Suppl B):16B–21B.
32. Zhang M, Hou ZK, Huang ZB, Chen XL, Liu FB. Dietary and Lifestyle Factors Related to Gastroesophageal Reflux Disease: a Systematic Review. Ther Clin Risk Manag. 2021;17:305–323. doi:10.2147/TCRM.S296680
33. Garg V, Narang P, Taneja R. Antacids revisited: review on contemporary facts and relevance for self-management. J Int Med Res. 2022;50(3):3000605221086457. doi:10.1177/03000605221086457
34. Ahmed S, Jamil S, Shaikh H, Abbasi M. Effects of Life style factors on the symptoms of gastro esophageal reflux disease: a cross sectional study in a Pakistani population. Pak J Med Sci. 2020;36(2):115–120. doi:10.12669/pjms.36.2.1371
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

