Back to Journals » International Journal of General Medicine » Volume 15
Outcomes of General Internal Medicine Consultations for Diagnosis from Specialists in a Tertiary Hospital: A Retrospective Observational Study
Authors Yokose M , Harada Y , Hanai S , Tomiyama S, Shimizu T
Received 11 June 2022
Accepted for publication 7 September 2022
Published 13 September 2022 Volume 2022:15 Pages 7209—7217
DOI https://doi.org/10.2147/IJGM.S378146
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Masashi Yokose, Yukinori Harada, Shogo Hanai, Shusaku Tomiyama, Taro Shimizu
Department of Diagnostic and Generalist Medicine, Dokkyo Medical University Hospital, Mibu, Tochigi, 321-0293, Japan
Correspondence: Taro Shimizu, Department of Diagnostic and Generalist Medicine, Dokkyo Medical University Hospital, Kitakobayashi 880, Shimotsuga, Mibu, Tochigi, 321-0293, Japan, Tel +81 282 86-1111, Email [email protected]
Purpose: The data on the diagnostic contribution of general internal medicine (GIM) consultations for undiagnosed health problems from specialists are scarce. This study aims to explore the role of generalists as diagnostic medicine consultants in tertiary care settings.
Patients and Methods: We conducted a retrospective observational study at a Japanese university hospital. GIM consultations for diagnosis from other departments on outpatients aged ≧ 20 years from January 2018 to December 2020 were included. Data were extracted from electronic medical records. The primary outcome was new diagnosis rates. The secondary outcomes were new diagnosis rates with clinical significance and clinical outcomes at 90 days from the index visit.
Results: A total of 328 patients were included. The top five consulting departments were orthopedics (17.0%), cardiovascular (10.3%), otorhinolaryngology (8.8%), neurology (8.8%), and gastroenterology (7.9%). GIM identified 456 chief complaints (CCs), and the top five were fever (10.9%), abnormal laboratory results (8.3%), fatigue (5.9%), and pain (7.4%) or numbness (4.6%) in the extremities. There were 139 (104/328 patients: 31.8%) specialty consultations from GIM, and the top five departments were rheumatology (21.1%), gastroenterology (19.2%), orthopedics (9.6%), psychiatry (9.6%), and neurology (9.6%). In total, 277 new diagnoses were established in 232 patients (70.7%), and 203 patients had new diagnoses with clinical significance (61.8%). Clinical outcomes at 90 days from the time of the index visit were resolution/improvement (60.7%), unchanged/worsened (22.3%), and unknown (17.0%).
Conclusion: Over 70% of GIM consultations from other departments established new diagnoses with favorable outcomes in > 60% of the patients.
Keywords: consultation, specialists, diagnostic error, diagnostic excellence, diagnostic uncertainty
Introduction
Generalists perform various tasks, including long-term chronic disease management, handling patients with complex medical problems, and health promotion or disease prevention.1 Gatekeeping is one of their important roles, and they assess every new patient and decide the need for specialist referral.2,3 Accurate diagnoses of undiagnosed health problems is essential for gatekeeping. An experimental study by Hashem et al using mock scenarios based on actual patient charts revealed that generalists had better diagnostic accuracy than other internal medicine sub-specialties (cardiology, hematology, and infectious diseases).4
Diagnostic errors, defined as “the failure to (a) establish an accurate and timely explanation of the patient’s health problem(s) or (b) communicate that explanation to the patient”,5 are common problems in daily practice. According to recent studies, diagnostic errors occur in approximately 5% of outpatients,5,6 and one-third of them result in avoidable patient harm, including death.6,7 Inappropriate referral and a lack of appropriate differential diagnoses are risk factors of diagnostic errors.2,8 Some studies reported that specialists see more patients with stable chronic diseases than generalists9–11 in daily practice; therefore, when they encounter patients with undiagnosed new health problems that are irrelevant to their specialty domain, more unnecessary cross-referrals to other specialists and diagnostic tests occur,9,11,12 which result in diagnostic errors, patient harm, and consumption of healthcare resources.2,5 Indeed, a previous study showed that approximately 10% of infectious disease consultations from other specialty departments associated with fever or inflammation of undetermined origin were due to non-infectious diseases.13 In such a situation, generalists can work as “diagnostic medicine consultants” for undiagnosed health problems to improve patient experience and reduce healthcare costs. Previous studies have demonstrated the diagnostic advantages of generalists in primary and secondary care settings, and the rate of new diagnoses was approximately 10%;14,15 however, research on referrals from specialists to generalists in tertiary care settings (ie, facilities providing highly technical and specialized care for patients with unusually severe, complex, or uncommon health problems)16,17 is limited.18 Therefore, the role of generalists as diagnostic medicine consultants in tertiary care settings has not yet been well explored. If this role is delineated, generalists can qualify as diagnostic specialists in any healthcare setting. This study aimed to reveal the role of generalists as diagnostic medicine consultants in tertiary care settings. Through this study, we could illustrate an ideal healthcare system framework between specialists and generalists to optimize diagnostic pathways and diagnostic excellence.7
Materials and Methods
Study Design
This single-center, retrospective, observational study was conducted at the Dokkyo Medical University Hospital (DMUH) in Japan. The Department of Diagnostic and Generalist Medicine (DGM) in DMUH covers the role of usual departments of general internal medicine (GIM) in Japan, which includes medical outpatient clinic, urgent care clinic, emergency medicine, and hospital medicine. Further, DGM serves a special role as a diagnostic medicine department that receives referrals of difficult-to-diagnose cases from within DMUH and from other hospitals in Japan and abroad. In addition to DGM, DMUH has 28 major specialty departments (Table 1), while it does not have some departments such as the department of infectious diseases or geriatric medicine seen in many tertiary care settings. We included GIM consultations for diagnosis from other departments in DMUH on outpatients aged ≧ 20 years from January 2018 to December 2020. We excluded GIM consultations for reasons other than diagnosis (eg, treatment for an established diagnosis).
 |
Table 1 Summary of Consultations Between General Internal Medicine (GIM) and Specialty Departments |
Ethical Consideration
The study was approved by the independent ethics committee of DMUH (No. R-47-10J). We followed the Declaration of Helsinki and The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.19 The written informed consent was waived by the ethics committee under the condition that we used an opt-out method. We informed patients by showing the detailed information of the study in the GIM outpatient waiting area.
Data Collection and Definition
First, we extracted data on patient age, sex, and consulting specialty departments. Second, two out of four researchers (MY, YH, SH, and ST) independently reviewed patients’ electronic medical records and collected the following data: chief complaints (CCs), specialty consultations from GIM (the number and name of specialty departments), new diagnoses, clinical outcome at 90 days from the time of the index visit, and the duration between the index consultation visit and the end of follow-up at GIM. When a new diagnosis was established, we entered the name, International Classification of Diseases-10 (ICD-10) category (version: 2019), likelihood (definite or suspected), relation with CCs (yes or no), and clinical significance (yes or no). We defined definite diagnosis as correct diagnosis with sufficient evidence, and suspected diagnosis as correct diagnosis with insufficient evidence. Clinical significance was defined as ”any new treatment was started based on new diagnoses, the patient’s symptoms improved or disappeared after follow-up observation under new diagnoses, or any useful information for subsequent patient and family decision-making was provided based on new diagnoses.” Clinical outcomes at 90 days from the time of the index visit were divided into the following three categories: resolved or improved, unchanged or worsened, and unknown. Inconsistencies in judgments between the first and second researchers were resolved by discussion with a third independent researcher.
Outcomes
The primary outcome was rate of new diagnoses established in GIM consultations. The secondary outcomes were rate of newly established diagnoses with clinical significance and clinical outcomes (resolution/improvement, unchanged/worsened, or unknown) at 90 days from the time of the index visit.
Statistical Analysis
Continuous data are presented as median with 25th and 75th percentiles. Categorical data are presented as count and proportion (%) and were compared using the chi-squared test or Fisher’s exact test. For the primary outcome, we calculated the rate of new diagnoses established in GIM consultations with a 95% confidence interval (CI) by dividing the number of new diagnoses by the total number of consultation cases. We calculated inter-researcher agreement between first and second researchers for the overall new diagnoses, by dividing the number of cases where both researchers gave the same decision (ie, the establishment of new diagnoses) by the number of cases where at least one researcher gave that decision. We also calculated the rate of new diagnoses (overall, definite, and suspected), CC-related new diagnoses, new diagnoses with clinical significance, and clinical outcomes at 90 days from the time of the index visit in sub-groups with or without specialty consultation from GIM. All p-values in the statistical tests were two-tailed, and p-values < 0.05 were considered statistically significant. All statistical analyses were conducted using R software (version 4.1.0; R Foundation for Statistical Computing). Based on the previous studies and our pilot data,14,15,20 we estimated the prevalence of diagnosis in our study population as 25%. Considering an acceptable margin of error of 5% at a 95% confidence level, we estimated a sample size of 289 patients.
Results
From a total of 333 eligible patients, we excluded five due to consultation not for diagnosis (Figure 1). Therefore, a total of 328 patients were included in the analysis. The median age was 58.0 years (42.0–72.5), and 142 (43.3%) were women. The median duration between the index consultation visit and end of follow-up at GIM was 22 days (range, 6.75–91.0 days).
 |
Figure 1 Flowchart of this study. Abbreviation: GIM, general internal medicine. |
During the study period, 26 out of 28 specialty departments consulted with GIM, and the top five consulting departments were orthopedic surgery (17.0%), cardiovascular medicine (10.3%), otorhinolaryngology, head and neck surgery (8.8%), neurology (8.8%), and gastroenterology (7.9%) (Table 1). We identified a total of 456 CCs, and the top five were fever (10.9%), abnormal laboratory results (8.3%), pain in the extremities (7.4%), fatigue (5.9%), and numbness in the extremities (4.6%) (Table 2 and Table S1).
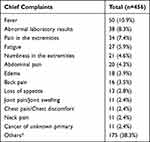 |
Table 2 Main Chief Complaints |
There were 139 specialty consultations from GIM (104/328 patients: 31.8%), and of these patients, 27/104 (25.9%) required two or more consultations. GIM consulted with 23 out of 28 specialty departments, and the top five departments were rheumatology (21.1%), gastroenterology (19.2%), orthopedic surgery (9.6%), psychiatry (9.6%), and neurology (9.6%) (Table 1).
In total, 277 new diagnoses were established in 232/328 patients (70.7%, 95% CI 65.4–75.6); 35/328 patients (10.7%) had two new diagnoses, and 6/328 patients (1.8%) had three new diagnoses. The inter-researcher agreement on the overall new diagnoses was 67.4% (176/261). Definite new diagnoses were established in 100/328 patients (30.4%, 95% CI 25.5–35.7). Of the 328 patients, 223 (67.9%, 95% CI 62.3–72.7) had CC-related new diagnoses. A total of 203 patients had new diagnoses with clinical significance (203/328, 61.8%, 95% CI 56.7–67.4). The top five ICD-10 categories of new diagnoses were the musculoskeletal system and connective tissue (15.5%); mental and behavioral (13.3%); endocrine, nutritional, and metabolic (13.3%); nervous system (9.7%); and symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified (8.6%) (Figure 2). Table S2 shows details of the new diagnoses. Clinical outcomes at 90 days from the time of the index visit were as follows: resolution or improvement, 199/328 (60.7%); unchanged or worsened, 73/328 (22.3%); and unknown, 56/328 (17.0%). Table 3 shows the comparison of diagnoses and clinical outcomes between patients with and without specialty consultations from GIM.
 |
Table 3 The Comparison of Diagnosis and Clinical Outcome between Patients with and without Additional Specialist Consultation from General Internal Medicine (GIM) |
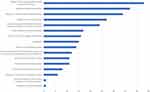 |
Figure 2 International Classification of Diseases-10 categories of new diagnoses. Horizontal axis is the number of diagnoses. |
Patients with specialty consultations from GIM had significantly higher rate of new diagnoses (overall and definite), CC-related new diagnoses, and new diagnoses with clinical significance than those without specialty consultations from GIM. More patients with specialty consultation from GIM had favorable outcomes (72.1% vs 55.4%, P<0.001).
Discussion
In our study at a general hospital in Japan, the rate of new diagnoses in outpatient-based GIM consultations was 70.7%. Most of the new diagnoses were CC-related and clinically significant. Over 80% of the departments interacted with GIM via consultations for diagnosis, and approximately one-third of the patients had specialty consultations from GIM. Symptoms improved in 60.7% of the patients and remained unchanged or worsened in 22.3%.
We demonstrated that various specialty departments consulted with GIM for numerous symptoms, and GIM made diagnoses of wide-ranging diseases. This indicates that generalists work as clinical hubs in tertiary care settings. While the categories of specialty departments were different from those in our study, other previous studies have demonstrated similar results.18,21 In addition, we showed that generalists could complete approximately 70% of consultations without further specialty consultations (224/328), and 60.7% of the patients (199/328) experienced symptom resolution or improvement within 90 days, regardless of the presence of diagnoses. Furthermore, patients with specialty consultations from GIM had a higher rate of definite diagnoses than those without specialty consultations from GIM (55.8% vs 18.8%, p<0.001). This implies that generalists distinguish patients who need specialty consultation appropriately, ie, they refer some patients with specific diseases to appropriate specialists, while they manage other patients with undiagnosed health problems without specialist assistance. By functioning as effective clinical hubs in tertiary care settings, generalists could reduce inappropriate or unnecessary consultations and the burden to specialists, and improve patient outcomes.
Fever, abnormal laboratory results (elevated C-reactive protein was the most common), pain in the extremities, fatigue, and numbness in the extremities were the top five CCs. The musculoskeletal system, connective tissue, and mental and behavioral categories were the main ICD-10 categories of new diagnoses. This indicates that specialists in tertiary care settings often refer patients with non-specific or uncertain problems to generalists. Some previous studies showed that general symptoms such as fatigue or fever were the most frequent reasons for referral to generalists (up to 40%),14,15,18 or that generalists in primary and secondary care settings also frequently encounter patients with health problems associated with the musculoskeletal system and psychiatry.22,23 We feel stress or anxiety due to the uncertainty of patients’ symptoms, which leads to excessive testing and increasing healthcare costs.24 Therefore, it is valuable for generalists to handle non-specific or uncertain problems appropriately. We assume that generalists are used to managing these types of problems because many generalists have published research on fever or inflammation of unknown origin,20,25–27 and Breivik et al showed in their research on chronic pain in 15 European countries and Israel that general practitioners (GPs) saw 70% of the patients.28 Additional training in non-specific or uncertain health problems, musculoskeletal pathology, and psychiatric conditions in the GIM curriculum in medical school and continuing medical education would strengthen knowledge base of generalists in the domains that are not covered by other specialists. This would further enhance their value in any healthcare setting.
The overall new diagnosis rate in our study (70.7%) was higher than that of the two previous studies in the Netherlands.14,15 They studied the outcomes of GIM second opinions in a university hospital, and the new diagnosis rate was approximately 10%. We attribute this gap to differences in data collection. While they included only definite diagnoses to calculate the new diagnosis rate, we included all diagnoses, regardless of their likelihood. As mentioned above, generalists encounter many patients with poorly defined conditions, and Rosendal et al reported in their study that GPs see approximately 36% of patients with symptoms without any specific diagnosis.29 Based on this, we included not fully established diagnoses because evaluating such an uncertain entity would describe the real value of generalists. The small difference between the rate of overall and CC-related new diagnoses, and the large gap between the rate of overall and definite new diagnoses indicate that generalists make valid but uncertain diagnoses.
There are many recent reports on diagnostic excellence.7,30,31 Diagnostic excellence refers to making accurate and timely diagnoses while allowing diagnostic uncertainty through cost-effective and patient-centered processes.7,30,31 Our results show that generalists contribute significantly to diagnostic excellence in tertiary care settings. Although previous studies have reported that multidisciplinary, team-based activities could improve diagnoses,31,32 we suggest building a new standardized system that includes a high-performance team with generalists as diagnostic medicine specialists and specialized departments for diagnostic quality management to achieve better diagnostic excellence. Future multicenter studies are needed to quantify the practical benefits derived from diagnostic excellence provided by generalists, such as healthcare cost reduction.
This study has several limitations. First, this was a single-center, retrospective, observational study. Second, we did not have some specialty departments, such as the department of infectious diseases, which deals with patients with fever or inflammation of undetermined origin.13,33,34 This would increase the percentage of fever and elevated C-reactive protein in CCs, and might have affected the results. Third, the rate of definite new diagnoses with the agreement of the two researchers was relatively low (approximately 20%). We think this was due to the many functional diseases for which clinicians found it difficult to reach a consensus. A strict definition of definite diagnosis might have led to this result. Fourth, the time between the index specialist visit and the GIM consultation might contribute to a better diagnostic rate by generalists. Generalists can work with more symptoms and test results. During this period, much information would help the clinical reasoning process. To address this “20/20 hindsight” issue and confirm the diagnostic superiority of generalists, we need an additional study comparing a matched cohort of patients with or without GIM consultations during the same period. Finally, we included only outpatients; therefore, additional studies focusing on inpatient GIM consultations are needed in the future.
Conclusion
In tertiary care hospitals, the GIM department could provide efficient diagnostic support to patients and other departments by functioning as a diagnostic center that directly leads to the relevant diagnosis. Further, the department could serve as a diagnostic hub that refers patients to the optimal department for diagnosis, contributing to the overall diagnostic quality. Hospitals may achieve diagnostic excellence by developing a system that can collaborate effectively between GIM and other departments for undiagnosed patients.
Acknowledgment
We would like to thank Editage for English language editing.
Disclosure
Dr Yukinori Harada reports personal fees from PRECISION, Inc., outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. ACP. General internal medicine career path information. Available from: https://www.acponline.org/about-acp/about-internal-medicine/general-internal-medicine.
2. Akbari A, Mayhew A, Al-Alawi MA, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane effective practice and organisation of care group. Cochrane Database Syst Rev. 2008. doi:10.1002/14651858.CD005471.pub2
3. Franks P, Clancy CM, Nutting PA. Gatekeeping revisited--protecting patients from overtreatment. N Engl J Med. 1992;327(6):424–429. doi:10.1056/NEJM199208063270613
4. Hashem A, Chi MTH, Friedman CP. Medical errors as a result of specialization. J Biomed Inform. 2003;36(1–2):61–69. doi:10.1016/S1532-0464(03)00057-1
5. Committee on Diagnostic Error in Health Care, Board on Health Care Services, Institute of Medicine, The National Academies of Sciences, Engineering, and Medicine. In: Balogh EP, Miller BT, Ball JR, eds. Improving Diagnosis in Health Care. National Academies Press; 2015:21794. doi:10.17226/21794
6. Singh H, Meyer AND, Thomas EJ. The frequency of diagnostic errors in outpatient care: estimations from three large observational studies involving US adult populations. BMJ Qual Saf. 2014;23(9):727–731. doi:10.1136/bmjqs-2013-002627
7. Yang D, Fineberg HV, Cosby K. Diagnostic Excellence. JAMA. 2021;326(19):1905. doi:10.1001/jama.2021.19493
8. Matulis JC, Kok SN, Dankbar EC, Majka AJ. A survey of outpatient internal medicine clinician perceptions of diagnostic error. Diagnosis. 2020;7(2):107–114. doi:10.1515/dx-2019-0070
9. Hashim MJ. Provision of primary care by specialist physicians: a systematic review. Fam Med Com Health. 2020;8(1):e000247. doi:10.1136/fmch-2019-000247
10. Rosenblatt RA, Hart LG, Baldwin LM, Chan L, Schneeweiss R. The generalist role of specialty physicians: is there a hidden system of primary care? JAMA. 1998;279(17):1364. doi:10.1001/jama.279.17.1364
11. Edwards ST, Mafi JN, Landon BE. Trends and quality of care in outpatient visits to generalist and specialist physicians delivering primary care in the United States, 1997–2010. J Gen Intern Med. 2014;29(6):947–955. doi:10.1007/s11606-014-2808-y
12. Scott IA, Campbell DA. The gaps in specialists’ diagnoses. Med J Aust. 2018;208(5):196–197. doi:10.5694/mja17.00905
13. Itoh N, Hadano Y, Yamamoto Y, Terada N, Kurai H. Infectious disease specialist consultations in a Japanese cancer center: a retrospective review of 776 cases. BMC Health Serv Res. 2020;20(1):500. doi:10.1186/s12913-020-05380-6
14. Burger PM, Westerink J, Vrijsen BEL. Outcomes of second opinions in general internal medicine. PLoS One. 2020;15(7):e0236048. doi:10.1371/journal.pone.0236048
15. Mustafa MK, Bijl M, Gans ROB. What is the value of patient-sought second opinions? Eur J Intern Med. 2002;13(7):445–447. doi:10.1016/S0953-6205(02)00138-3
16. Flegel K. Tertiary hospitals must provide general care. CMAJ. 2015;187(4):235. doi:10.1503/cmaj.150056
17. National Center for Biotechnology Information. Tertiary healthcare. Available from: https://www.ncbi.nlm.nih.gov/mesh/68063128.
18. Kita K, Shimizu Y, Yamashiro S. Referral and consultation practice between generalists and specialists at a university hospital: a retrospective cross-sectional study. Off J Japan Prim Care Assoc. 2019;42(2):92–97. doi:10.14442/generalist.42.92
19. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–577. doi:10.7326/0003-4819-147-8-200710160-00010
20. Harada Y, Masuda M, Hirosawa T, et al. Safety and efficacy of outpatient follow-up for referred patients with undiagnosed fever: a retrospective cohort study. Medicine. 2020;99(5):e18532. doi:10.1097/MD.0000000000018532
21. Jordan MR, Conley J, Ghali WA. Consultation patterns and clinical correlates of consultation in a tertiary care setting. BMC Res Notes. 2008;1(1):96. doi:10.1186/1756-0500-1-96
22. Bindman AB, Forrest CB, Britt H, Crampton P, Majeed A. Diagnostic scope of and exposure to primary care physicians in Australia, New Zealand, and the United States: cross sectional analysis of results from three national surveys. BMJ. 2007;334(7606):1261. doi:10.1136/bmj.39203.658970.55
23. Van Such M, Lohr R, Beckman T, Naessens JM. Extent of diagnostic agreement among medical referrals. J Eval Clin Pract. 2017;23(4):870–874. doi:10.1111/jep.12747
24. Meyer AND, Giardina TD, Khawaja L, Singh H. Patient and clinician experiences of uncertainty in the diagnostic process: current understanding and future directions. Patient Educ Couns. 2021;104(11):2606–2615. doi:10.1016/j.pec.2021.07.028
25. Vanderschueren S, Del Biondo E, Ruttens D, Boxelaer IV, Wauters E, Knockaert DDC. Inflammation of unknown origin versus fever of unknown origin: two of a kind. Eur J Intern Med. 2009;20(4):415–418. doi:10.1016/j.ejim.2009.01.002
26. Naito T, Tanei M, Ikeda N, et al. Key diagnostic characteristics of fever of unknown origin in Japanese patients: a prospective multicentre study. BMJ Open. 2019;9(11):e032059. doi:10.1136/bmjopen-2019-032059
27. Vanderschueren S, Knockaert D. Tackling fever and inflammation of unknown origin: the do’s and don’ts. Acta Clin Belg. 2014;69(6):412–417. doi:10.1179/2295333714Y.0000000070
28. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287. doi:10.1016/j.ejpain.2005.06.009
29. Rosendal M, Carlsen AH, Rask MT, Moth G. Symptoms as the main problem in primary care: a cross-sectional study of frequency and characteristics. Scand J Prim Health Care. 2015;33(2):91–99. doi:10.3109/02813432.2015.1030166
30. Meyer AND, Singh H. The path to diagnostic excellence includes feedback to calibrate how clinicians think. JAMA. 2019;321(8):737. doi:10.1001/jama.2019.0113
31. Singh H, Connor DM, Dhaliwal G. Five strategies for clinicians to advance diagnostic excellence. BMJ. 2022;376:e068044. doi:10.1136/bmj-2021-068044
32. Graber ML, Rusz D, Jones ML, et al. The new diagnostic team. Diagnosis. 2017;4(4):225–238. doi:10.1515/dx-2017-0022
33. Hadano Y, Watari T, Yasunaga H. Infectious disease consultations and newly diagnosed cancer patients: a single-center retrospective observational study. Medicine. 2020;99(25):e20876. doi:10.1097/MD.0000000000020876
34. Hadano Y, Matsumoto T. Infectious disease consultations in a Japanese tertiary care teaching hospital: a retrospective review of 508 cases. BMC Health Serv Res. 2018;18(1):983. doi:10.1186/s12913-018-3802-6
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
