Back to Journals » Orthopedic Research and Reviews » Volume 15
Outcome of Surgical Management of Dermatofibrosarcoma Protuberance: A Single-Institution Multidisciplinary Approach
Authors Alhabeeb AY , Idrees AO, Alhowaish TS , Alhamadh MS , Masudi E, Alanazi A, Aljuhani W
Received 25 August 2023
Accepted for publication 9 November 2023
Published 20 November 2023 Volume 2023:15 Pages 237—243
DOI https://doi.org/10.2147/ORR.S437175
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Abdulrahman Yousef Alhabeeb,1,2 Ahmed O Idrees,2,3 Thamer S Alhowaish,2,4 Moustafa S Alhamadh,1,2 Emad Masudi,1,2 Abdullah Alanazi,1,2 Wazzan Aljuhani2,3
1College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Ministry of the National Guard-Health Affairs, Riyadh, Kingdom of Saudi Arabia; 2King Abdullah International Medical Research Center, Ministry of the National Guard-Health Affairs, Riyadh, Kingdom of Saudi Arabia; 3Department of Orthopedic Surgery, King Abdulaziz Medical City, Ministry of National Guard - Health Affairs, Riyadh, Saudi Arabia; 4Division of Neurology, King Abdulaziz Medical City, Ministry of the National Guard Health Affairs, Riyadh, Kingdom of Saudi Arabia
Correspondence: Thamer S Alhowaish, Email [email protected]
Introduction: Dermatofibrosarcoma protuberans (DFSP) is a rare, slow-growing, and locally aggressive soft tissue tumor with a high recurrence rate and metastatic potential, even with the proper treatment.
Methods: This was a retrospective (case series) study that took place at King Abdulaziz Medical City, Riyadh, Kingdom of Saudi Arabia, to determine the outcomes of and appropriate margin excision for DFSP. All patients who were diagnosed with DFSP from 2016 to 2021 were included. The following variables were assessed: demographics, tumor characteristics, management options, and most importantly, whether patients were managed with an oncology-oriented approach or a non-oncology-oriented approach.
Results: There were a total of seventeen patients with DFSP, four of whom had fibrosarcomatous differentiation (FS-DFSP). The majority (N = 13, 76.5%) of the patients were females. The lower extremities and back were the most common locations for DFSP, accounting for 47.1% and 23.5%, respectively. Only two (11.76%) patients had metastatic disease, one of whom had FS-DFSP. The minimum resection margin was 3 cm, and the maximum was 5 cm. Thirteen (76.47%) patients were managed with an oncology-oriented approach (Group I), 23% of whom had post-excision positive margins. However, all patients who were managed with a non-oncology-oriented approach (Group II) had positive margins post-excision. More than three-quarters (76.9%) of group I underwent wide resection. Split-thickness skin grafting and primary closure were the most commonly used reconstruction methods in groups I and II, respectively. The mean planned margins in groups I and II were 3.9 cm and 1.7 cm, respectively.
Conclusion: The findings of this study suggest that a planned wide-margin excision with a minimum safe margin of 3– 5 cm should be implemented to reduce the recurrence, metastasis, and need for further surgeries in patients with DFSP.
Keywords: dermatofibrosarcoma protuberans, surgical oncology, management, approach
Introduction
Dermatofibrosarcoma protuberans (DFSP) is a rare soft tissue tumor that occurs in the dermis, subcutaneous fat, and occasionally, muscle and fascia. DFSP has a low-moderate rate of metastasis, but it is known for its high recurrence rate after surgical resection.1 More than 90% of DFSP cases are due to a chromosomal translocation t(17;22) that produces a platelet-derived growth factor beta (PDGF-b)/collagen type 1A1 fusion gene, leading to the constitutive production of collagen.2 Anyone of any age (from birth to the 90s) can be affected by DFSP. However, it is common among adults in their third and fifth decades.
Although it can arise in any part of the body, DFSP most often affects the trunk, head, neck, and proximal extremities.3 DFSP affects 4.1 people per million each year, and women’s risks are 1.14 times higher than men’s. In addition, older age, male gender, black race, and anatomic location of the limbs and head, as compared with the trunk, are associated with a poorer prognosis.2
The diagnosis of DFSP requires a tissue biopsy and subsequent histopathology. Surgical excision with wide margins is considered the treatment of choice for DFSP, and it is usually curative. The surgical margins usually range between 1 and 5 cm, with studies recommending a minimum of 2 cm of surgical margins. Following the resection, many techniques can be used for wound closure depending on the size and site of tumor, including primary closure, muscle flap, or skin grafts.4,5 Other treatment options exist for inoperable cases. For example, radiation therapy might be considered for patients in whom the tumor cannot be surgically removed, whose postoperative margins are microscopically or macroscopically positive, or who have had multiple recurrences. Also, it can be used for patients in whom wide-margin excision would cause significant cosmetic or functional impairment. Following treatment, patients should be clinically evaluated every six months for at least five years to detect local recurrence, lung metastasis, or lymph node metastases.4
Fibrosarcomatous dermatofibrosarcoma protuberans (FS-DFSP) represents a rare form of DFSP with an unpredictable biological behavior and a poor prognosis. Based on a large systematic review, compared to DFSP, FS-DFSP has a 2.2, 5.5, and 6.2 times higher rate of local recurrence, metastasis, and mortality, respectively.6
Although it is well known that surgical excision with wide margins is the gold standard treatment for DFSP, the appropriate margin is still debatable. In this study, we described the experience of one of the largest hospitals in Saudi Arabia in diagnosing and managing patients with DFSP and FS-DFSP via an oncology-oriented and a non-oncology-oriented approaches. In addition, we tried to define an appropriate margin that should be excised to potentially reduce the risk of recurrence and treatment failure in our population.
Methods
Objective
To determine the outcomes of and define an appropriate margin excision for DFSP and FS-DFSP.
Study Design, Settings, and Subject
This was a retrospective (case series) study that took place in the National Guard Health Affairs (MNG-HA), King Abdulaziz Medical City (KAMC), Riyadh, Kingdom of Saudi Arabia. KAMC is an academic, government-funded tertiary hospital that combines clinical care, training, academic research, and state-of-the-art medical technologies. The study included all patients who were diagnosed with DFSP from 2016 to 2021.
Data Collection
After obtaining the ethical approval, the electronic records of all patients with a diagnosis of dermatofibrosarcoma from 2016 to 2021 were requested. Then, the required variables were collected by screening the patient’s electronic records, using the KAMC electronic system Best-Care; Seoul, South Korea: ezCaretech Co.
The following variables were collected: Patients’ gender, age, location of the tumor, size of the tumor, the clinical presentation, biopsy method, margin type, planned margins in cm, pathology margin status as positive or negative, use of radiation, use of systemic therapy, metastasis, resection method, and oncology (group I) or non-oncology (group II) approach.
The oncology-oriented approach was defined as a wide local excision, and the non-oncology-oriented approach was defined as an unplanned excision.
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS) version 22 (Armonk, NY, USA: IBM Corp.) was used for data analysis. The categorical variables were presented as frequency and percentage, and the numerical variables as mean ± standard deviation.
Ethical Consideration
The study was approved by the Institutional Review Board of King Abdullah International Medical Research Center, MNG-HA, Riyadh, Kingdom of Saudi Arabia (RC20/682/R). Informed consent was waived because of the retrospective nature of this study. Access to the data was restricted to the researchers. The confidentiality of all patients was protected, and no names or medical record numbers were used. Privacy and confidentiality were assured, and all the data, both hard and soft copies, were kept in a secure place within the MNG-HA. This study complies with the Declaration of Helsinki.
Results
There were a total of seventeen patients with DFSP, four (23.53%) of whom had FS-DFSP. More than three-quarters (N = 13, 76.5%) of the patients were females. The most common location of DFSP was the lower limbs, followed by the back, chest or abdomen, and upper limbs, accounting for 47.1%, 23.5%, 17.6%, and 11.8%, respectively (Figure 1). More than half of the patients (64%) presented as a mass for investigation. Less than half (N = 7, 41%) of the patients had positive margins post unplanned excision, one of whom had FS-DFSP. Only two (11.76%) patients had metastatic disease, one of whom received systemic therapy (Imatinib), and the other was planned for systemic therapy but was lost to follow-up for an unknown reason. In both DFSP and FS-DFSP, the minimum resected margin was 3 cm, and the maximum was 5 cm. A total of five (29.41%) patients needed radiation therapy; three had it before the resection, one after the resection, and one both before and after the resection (Table 1). Four patients had a total dose of 50 Gy each, and one patient had a total dose of 66 Gy.
 |
Figure 1 Anatomical location of DFSP in patients treated with an oncology-oriented approach and a non-oncology-oriented approach. |
 |
Table 1 Baseline Characteristics of the Patients |
Almost three-quarters (N = 13, 76.4%) of the patients were managed with an oncology-oriented approach (Group I). Only three (23.1%) patients in group I had post-excision positive margins, whereas all the patients in group II had post-excision positive margins. Wide resection was done in almost all (N = 12, 92.31%) of the patients in group I; only one patient had an intralesional resection. Regarding the reconstruction method, more than two-thirds (N = 8, 66.7%) of the patients in group I had split thickening and skin grafting, with only three (23.1%) and one (7.69%) had primary closure and muscle flap, respectively. However, in group II, three-quarters (N = 3, 75%) of the patients had primary closure, and only one (25%) had breast reconstruction (Figure 2). Lastly, the mean planned margin in group I was 3.9 and 1.7 in group II (Table 2).
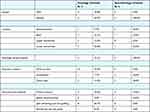 |
Table 2 Comparison Between the Patients Based on the Treatment Approach |
 |
Figure 2 Resection and reconstruction methods in patients treated with an oncology-oriented approach and a non-oncology-oriented approach. |
Discussion
Dermatofibrosarcoma is a rare, slow-growing mesenchymal tumor that is often misdiagnosed. Unfortunately, misdiagnosis can lead to many unplanned non-oncological excisions and higher rates of recurrence. Unlike previously published studies, more than two-thirds of our patients were females.7,8 Furthermore, most studies found the trunk as the most common location for DFSP. However, our results showed that almost half of the cases were in the lower limbs.5,8–10 The tumor size can vary, ranging from 0.2 cm to more than 10 cm, with an average of 2 to 3.5 cm.11 In our study, however, the mean size was 7.4 cm, with the smallest being 2 cm, and the largest being 18.5 cm. Furthermore, the median planned margin ranges from 2.5 to 3 cm based on the literature, which is almost similar to what we found in our study (4 cm).12 For the reconstruction method, the majority of our patients had split-thickness skin grafting. Other studies have reported random flaps and primary closure as prominent methods.13,14
We noticed in our comparison between the two groups of approaches that there was a big difference in margins between the two groups, which could be explained by the fact that most of group II (50%) had an intralesional resection. The wide resection in group I led to fewer positive pathology margins (23%) in comparison to group II, which had 100% positive pathology margins. Furthermore, patients who had positive margins after wide local excision with large tumors (>5 cm), or patients with positive margins after unplanned excision were candidates for radiation therapy. Moreover, there was a clear variation in the reconstruction methods between the two groups. The majority of group I underwent reconstruction with split thickening skin graft, which is usually used when the resection results in a significant skin defect, whereas the majority of group II underwent primary closure. This variation can be understood in the sense that patients who had an unplanned excision at first will likely undergo further surgeries, have a bigger safe margin, and likely need more extensive reconstructive surgeries. Furthermore, in cases involving extensive excision and large defects, surgeons may need to consider alternative reconstructive options, such as a myocutaneous flap. For example, a case of 53-year-old woman with a recurrent DFSP of the clavicular area underwent extensive excision encompassing the external cortical bone of the left clavicle. For the reconstruction used, a pedicled Latissimus Dorsi myocutaneous flap was used in order to overcome the nerve and vessels lost, and to fill the subcutaneous tissue and fascia lost after the excision.15 In addition, anterolateral thigh perforator free flap was used in the case of 21-year-old man with a history of slowly growing subcutaneous lesion of the left preauricular area over the course of seven months. Superior left thyroid artery and vein were used as recipient vessels, and the external jugular vein was used to receive the second vein anastomosis. Anterolateral thigh perforator flap not only can reconstruct the soft tissue but it is also a hair bearing and malleable flap which color also matches the area.16
The term “unplanned excision” is described as a tumor resection without aiming to achieve a wide surgical margin or tumor-free margin. Unplanned excision carries more disadvantages than advantages. It influences many perspectives, which include but are not limited to patients, metastasis, reconstruction methods, and morbidity and mortality.17
All cases of DFSP should be managed by an oncology team to avoid complications such as recurrence, reoperation, and the use of chemotherapy and radiotherapy. In terms of limitations, our study was limited by the low number of cases and the retrospective design. Many factors, such as missed diagnosis cases and tumor recurrence, contributed to the lack of further statistical analysis. A larger study with a higher sample size is needed to come up with solid and reliable recommendations for treating DFSP and mitigating its risk of recurrence and/or metastasis.
Conclusion
DFSP is a slow-growing tumor that has a high recurrence rate and metastatic potential, if not treated properly. It seems that DFSP is best handled by an oncology team with a wide-margin excision after staging a workup to mitigate its complications and improve its outcomes. Also, the study suggests targeting a minimum safe margin of 3–5 cm. Moreover, the study revealed that lower extremities were the most common location, wide resection was the most frequent resection method used, and split-thickness skin grafting was the most commonly used reconstruction technique. Unplanned excision should be avoided as it increases the need for further surgeries, recurrence, and metastasis, and worsens survival and limb function.
Institutional Review Board
The study was approved by the Institutional Review Board of King Abdullah International Medical Research Center, MNG-HA, Riyadh, Kingdom of Saudi Arabia (Study Number: RC20/682/R).
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author.
Funding
No funding was received in order to conduct this study.
Disclosure
The authors have no conflict of interest to declare.
References
1. Brooks J, Ramsey ML. Dermatofibrosarcoma Protuberans. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020.
2. Kreicher KL, Bordeaux JS, Kurlander DE, Gittleman HR, Barnholtz-Sloan JS. Incidence and survival of primary dermatofibrosarcoma protuberans in the United States. Dermat Surg. 2016;42:S24–S31. doi:10.1097/DSS.0000000000000300
3. Sirvent N, Maire G, Pedeutour F. Genetics of dermatofibrosarcoma protuberans family of tumors: from ring chromosomes to tyrosine kinase inhibitor treatment. Genes Chromosomes Cancer. 2003;37(1):1–19. doi:10.1002/gcc.10202
4. Ugurel S, Kortmann R-D, Mohr P, et al. S1 guidelines for dermatofibrosarcoma protuberans (DFSP) - update 2018. J Dtsch Dermatol Ges. 2019;17(6):663–668.
5. Wiesmueller F, Agaimy A, Perrakis A, et al. Dermatofibrosarcoma protuberans: surgical management of a challenging mesenchymal tumor. World J Surg Onc. 2019;17(90). doi:10.1186/s12957-019-1627-3
6. Liang CA, Karia PS, Schmults CD, Jambusaria-Pahlajani A, Elenitsas R, Zhang PD. A systematic review of outcome data for dermatofibrosarcoma protuberans with and without fibrosarcomatous change. J Am Acad Dermatol. 2014;71(4):781–786. doi:10.1016/j.jaad.2014.03.018
7. Cammarata E, Esposto E, Veronese F, et al. Safety margins for dermatofibrosarcoma protuberans: a comparison between wide local excision and Mohs Tubingen technique. Europ J Dermatol. 2020;30(3):289–293. doi:10.1684/ejd.2020.3771
8. Woo KJ, Bang SI, Mun GH, Oh KS, Pyon JK, Lim SY. Long-term outcomes of surgical treatment for dermatofibrosarcoma protuberans according to width of gross resection margin. J Plast Reconstr Aesthet Surg. 2016;69(3):395–401. doi:10.1016/j.bjps.2015.10.027
9. Tan YG, Chia CS, Loh WL, Teo MC. Single-institution review of managing dermatofibrosarcoma protuberans. ANZ J Surg. 2016;86(5):372–376. doi:10.1111/ans.13276
10. Zhou X, Sun D, Liu Y, et al. Dermatofibrosarcoma protuberans: our 10-year experience on 80 patients. J Dermatolog Treat. 2020;31(6):554–558. doi:10.1080/09546634.2019.1622629
11. Castle KO, Guadagnolo BA, Tsai CJ, Feig BW, Zagars GK. Dermatofibrosarcoma protuberans: long-term outcomes of 53 patients treated with conservative surgery and radiation therapy. Int J Radiat Oncol Biol Phys. 2013;86(3):585–590. doi:10.1016/j.ijrobp.2013.02.024
12. Larbcharoensub N, Kayankarnnavee J, Sanpaphant S, Kiranantawat K, Wirojtananugoon C, Sirikulchayanonta V. Clinicopathological features of dermatofibrosarcoma protuberans. Oncol Lett. 2016;11(1):661–667. doi:10.3892/ol.2015.3966
13. Huis In ‘t Veld EA, Grünhagen DJ, van Coevorden F, et al. Adequate surgical margins for dermatofibrosarcoma protuberans - A multi-centre analysis. Eur J Surg Oncol. 2021;47(2):436–442. doi:10.1016/j.ejso.2020.06.022
14. Chappell AG, Doe SC, Worley B, et al. Multidisciplinary surgical treatment approach for dermatofibrosarcoma protuberans: an update. Arch Dermatol Res. 2021;313:367–372. doi:10.1007/s00403-020-02124-8
15. Longo B, D’orsi G, Orlando G, Giacalone M, Cervelli V. Recurrent dermatofibrosarcoma protuberans of the clavicular region: radical excision and reconstruction with latissimus dorsi myocutaneous flap. Plast Reconstr Surg. 2022;1:14–19. doi:10.57604/PRRS-002
16. Longo B, Paolini G, Costantino B, Pagnoni M, Santanelli F, Belli E. Wide excision and anterolateral thigh perforator flap reconstruction for dermatofibrosarcoma protuberans of the face. J Craniofac Surg. 2013;24(6):e597-e599–e599. doi:10.1097/SCS.0b013e3182a238c1
17. Tokumoto H, Akita S, Kubota Y, Mitsukawa N. Effect of unplanned excision of soft tissue sarcomas on skin defects and reconstructive procedures. J Plast Surg Hand Surg. 2020;54(6):372–376. doi:10.1080/2000656X.2020.1799817
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
