Back to Journals » Orthopedic Research and Reviews » Volume 15
Orthopedic Surgical Management of Complicated Congenital Popliteal Pterygium Syndrome: A Case Report
Authors Hasan M, Muhammad H , Cein CR , Ahmad H, Baskara AANN
Received 26 November 2022
Accepted for publication 9 March 2023
Published 24 March 2023 Volume 2023:15 Pages 47—57
DOI https://doi.org/10.2147/ORR.S392024
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Meirizal Hasan,1 Hilmi Muhammad,2 C Rayhan Cein,1 Husein Ahmad,1 Anak Agung Ngurah Nata Baskara1
1Department of Orthopedic and Traumatology, Sardjito General Hospital / Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia; 2Division of Pediatric Orthopedic, Department of Orthopedic and Traumatology, Sardjito General Hospital / Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
Correspondence: Hilmi Muhammad, Department of Orthopedics and Traumatology, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito Hospital, Jl. Kesehatan No. 1, Yogyakarta, 55281, Indonesia, Email [email protected]
Introduction: Popliteal pterygium syndrome (PPS) is a rare autosomal-dominant condition that causes fixed flexion deformity of the knee. The popliteal webbing and shortening of the surrounding soft tissue could limit the functionality of the affected limb unless it is surgically corrected. We reported a case of PPS in a pediatric patient encountered in our hospital.
Case: A 10-month-old boy came with a congenital abnormally flexed left knee with bilateral undescended testis and syndactyly of the left foot. The left popliteal pterygium extending from the buttock to the calcaneus was observed, with an associated fixed flexion contracture of the knee and equine position of the ankle. Normal vascular anatomy was seen in the angiographic CT scan; therefore, multiple Z-plasty and fibrotic band excision were performed. The sciatic trunk was exposed on the popliteal level, and the fascicular segment was excised from the distal stump and sutured to the proximal stump under the microscope to extend the sciatic nerve for approximately 7 cm. No postoperative complications were reported. Multiple tendons and soft tissue reconstruction were performed when the patient was 2-year-old to correct the adductus and equine deformity of the left foot.
Discussion: Surgical correction for popliteal pterygium demands staged techniques to deal with the shortened structure. In our case, multiple Z-plasty were performed, and the fibrotic band was excised until its base with meticulous consideration of the underlying neurovascular bundle. Fascicular shifting technique for sciatic nerve lengthening can be considered in unilateral popliteal pterygium with difficulty extending the knee due to shortened sciatic nerve. The unfavorable outcome of nerve conduction disturbance resulting from the procedure may be multifactorial. Still, the existing foot deformity, including a certain degree of pes equinovarus could be treated by multiple soft tissue reconstructions and adequate rehabilitation to achieve the desired outcome.
Conclusion: Multiple soft tissue procedures resulted in acceptable functional outcomes. However, the nerve grafting procedure is still a challenging task. Further study is required to explore the technique in optimizing the nerve grafting procedure for popliteal pterygium.
Keywords: popliteal pterygium syndrome, multiple z-plasty, fascicular shifting, flexion contracture, case report
Introduction
Epidemiology and Incidence
Popliteal pterygium syndrome (PPS) is a rare autosomal dominant congenital anomaly. Trelat first described PPS in 1869 as a congenital anomaly that includes the orofacial, cutaneous, musculoskeletal, and genitalia.1 The term PPS was proposed by Gorlin et al in 1968 based on the most unusual anomaly, which was the cutaneous webbing or skinfold that arises from the popliteal fossa down to the heel and is further identified with the term “popliteal pterygium”. This popliteal webbing often inhibits the movement of the leg unless surgically corrected. PPS is considered a rare disease, with an incidence of only 1 in 300.000 live births.2,3
Etiology and Pathogenesis
PPS is believed to be related to the Interferon regulatory factor 6 (IRF-6) gene mutation, which is localized in chromosome 1q32.2. IRF-6 provides genetic instructions in producing a protein that plays an essential role in the early development of the facial, skin, and genital organs.10 This protein is a transcription factor which attaches to specific DNA regions and helps control the activity of the genes. Mutation of the IRF-6 gene is believed to be responsible for several maxillofacial congenital anomalies, one of which includes PPS and others such as Van der Woude syndrome (VWS) only differing in the mutated exon location.7,8,10 IRF-6 is involved in epithelial differentiation as a component of the regulatory feedback loop that controls epidermal cells’ proliferative potential.
Through family tree analysis, PPS was thought to be inherited with an autosomal-dominant pattern and confirmed by genetic studies performed in earlier research.4,9,10 The appearance of lower lip pit is a remnant of the lateral grooves due to a congenital anomaly. The pathogenesis differs from multiple pterygium syndrome caused by intra-uterine immobilization.5,11,28 In PPS, the pathogenesis is partially understood. Membranes and thread-like Intra oral bands are caused by hyperproliferation of epithelial cell layers in the first trimester.
Clinical Manifestation
The variety of PPS facial manifestations spans widely, from orofacial anomalies such as cleft-lip, cleft-palate, and or paramedian pits or lower lip pits. The cleft-lip or cleft palate findings were reported as high as 90% of the cases with severity ranging from incomplete-unilateral to complete-bilateral cleft.4 Lower lip pit was reported in slightly less than half of the cases. Another facial phenotype seen in PPS is filiform adhesion between the eyelid, known as ankylo-blepharon-fili-formeadnatum, which was reported in 20% of the cases.1,4 Choanal atresia can also be found in PPS patients.4 Around 43% of the patients also present with intra-oral tissue band or syngnathia, which seriously affects mouth opening and requires immediate surgical intervention.4,5
Genital abnormalities have been described in 4% of cases of popliteal pterygium syndrome, namely cryptorchidism, bifid scrotum, hypoplastic or absence of scrotum, and hypoplastic or aplastic labia majora.6 In addition, inguinal hernias are occasionally present. The most common genital anomaly in boys is bifid scrotum and hypoplastic or aplastic labia majora in girls.6 In severe cases, genital abnormalities may result in fertility disturbances.
The musculoskeletal anomaly varies even greater. Other musculoskeletal deformities reported include syndactyly and brachydactyly, which occurred in half of the reported cases. However, the main finding in PPS is the popliteal pterygium reported in 90% of the cases. The pterygium might appear unilaterally or bilaterally. The web usually extends from ischial tuberosity towards the calcaneus, severely limiting the movement of the leg. The skinfold might have a palpable band of connective tissue, popliteal artery, or peroneal nerve. This band is an anomalous muscle known as calcaneoischiadicus. The sciatic nerve is usually shortened and runs posteriorly towards its usual location.3 Absence or abnormally-inserted hamstring or calf muscle along the band may occur. Additional pterygium in the inguinal region was reported in about 9% of the case. Another finding is the presence of pyramidal skinfold that resides on nail’s outer part, reported in one-third of the cases. Another nail abnormality, including hypoplasia of the nail can occur and are usually found in the toe.5
PPS is considered as a manifestation of arthrogryposis and often accompanied by other congenital anomalies such as talipes equine varus, hidden spina bifida, bifid ribs, and short sternum. The ipsilateral hip flexors are often contracted due to the pterygium along with skeletal shortening of the femur, tibia and fibula. Due to its high variability, diagnostic criteria for PPS have been established, including cleft/lip palate, popliteal pterygium, paramedian lower lip pits, genital, and nail abnormalities. PPS is diagnosed if at least 3 of mentioned manifestations are present.5 These musculoskeletal anomalies differentiate PPS from VDW syndrome.3
Differential diagnoses of PPS can be divided into two groups: syndromes with facial anomaly and syndromes with limb anomaly. VWS presents with similar maxillo-facial defects (paramedian lip pit, oral cleft) to PPS but lacks limb anomalies. It is inherited by the same pathway as PPS and caused by the IRF-6 gene mutation mentioned before. Another example is Juberg-Hayward Syndrome which may present with a hypoplastic thumb, cleft lip and palate in addition to microcephaly. Fraser syndrome also falls into this category with syndactyly and genital hypoplasia presentation. However, the most akin differential diagnosis is lethal pterygium syndrome, also called Bartsocas–Papas syndrome, which is inherited with autosomal-recessive pattern and has numerous symptoms of popliteal membranes, facial clefts, syngnathia, ankyloblepharon, aplasia of thumb, syndactyly, hypoplasia of labia majora, microcephaly, corneal aplasia, hypoplasia of nasal wings.29 More severe conditions may also co-exist, such as absent kidney, cracks within the sacral vertebrae, epithelial lesions and dystrophic scalp, dull hair, dystrophic nails, fungal skin infection (tinea) and subungual hyperkeratosis with enlargement and thinning of the sheet. The most important and distinctive feature of PPS is mental retardation, scar atrophy of the scalp, and ectodermal dysplasia.5,29
Treatment
Since the manifestation of PPS varies, treatment of PPS is adjusted based on the necessity. Intra-oral band requires immediate surgery since it might cause obstructive apnea.14 Similarly, cleft palate should be reconstructed within the first year of life and consequently followed by speech therapy.12 The surgical therapy for genital anomalies can be adjusted depending on the severity. In regards to the popliteal pterygium, the treatment is also evaluated according to its severity. The aim of surgical treatment is to improve functional outcome especially in PPS which affect lower limb mobilization, but realistically the main goal is to achieve lower limb which braces could be applied according to the anatomical segment. When left untreated, the extreme knee flexion of the patient will greatly impact their activities of daily living.
Soft tissue release can be performed together in adjunct to serial casting and bracing in patients with minimum popliteal webbing. For more severe webbing, consider several procedures such as Z-plasties through posterior approach with wide flaps, excision of the fibrotic band after meticulous dissection, hamstring lengthening, posterior capsulotomy, or any combination of mentioned procedure that should be done gradually. Any anomalous muscle should be detached from the fibrotic band, and the nerve that runs along the band must be protected at any time. Achilles tendon lengthening might be considered if equine foot deformity is present, followed by cast application reaching up to the knees. Corrective casting with a gradually increased extension should be done if the skin coverage is adequate. Patients which require multiple surgery are at risk of acquiring nerve injury and failure of nerve lengthening is not uncommon, which in PPS the sciatic nerve might be one of the affected main nerves. If so, nerve grafting is an option for related conditions. Alternative to Z-plasties, Ilizarov external fixation can be done following hamstring tenotomy on the ischial tuberosity, tenotomy of the flexor hallucis longus, and Z-lengthening of the Achilles tendon on the ankle as done by Kim et al.15 Unfortunately, 15-degrees of knee flexion contracture reoccurred later in the report. Another treatment alternative of lengthening the nerve by fascicular shifting have been reported in several studies which we performed in this report.
The ideal timing of corrections remains controversial. Parikh et al suggested correction to be done as early as possible considering the high re-occurrence rate.4,24 It is also important to pay attention to other co-existing musculoskeletal anomalies like Pes equinovarus, syndactyly, clinodactyly, and nail dysplasia which require treatment. It is reasonable to combine other procedures associated with the additional anomalies for best cosmetic result and avoidance of adverse psychological implications caused by repetitive procedures.
Case Report
This case report describes a male child delivered at term via elective cesarean section without any complication. Both his parents were healthy and came to the obstetrician regularly for antenatal monitoring. The patient was the family’s first child with no history of his relatives suffering from the same condition. From physical examination, an abnormally flexed left knee was observed at birth along with bilateral undescended testis and syndactyly of the left foot. The left popliteus pterygium runs from the buttock to the calcaneus, with an associated knee flexion contracture. The patient could not extend his knee as the popliteal pterygium caused a 90° rigid knee-flexion contracture (Figure 1). The parents opted for multiple traditional massages, and physiotherapies were performed without satisfactory results. The patient was initially encountered in our outpatient department at ten months of age. The delayed treatment was due to administrative problems including health insurance and the referral process.
 |
Figure 1 Preoperative marking and plain radiograph. Note the presence of sacral dimple prior to surgery but no abnormality seen from x-ray. |
Surgical intervention was planned after an angiographic CT scan revealed that there were no vascular disturbances (Figure 2). We thoroughly informed the patient’s parents that although fascicular shifting is a relatively new technique to be implemented especially in human and its failure rate is considered common, the realistic goal from releasing the contracture is to enable brace utilization daily. To these, the parents gave their full informed consent.
Multiple Z-plasties through a posterior approach along with excision of the fibrotic band were performed. After meticulous dissection, a tight sciatic nerve was encountered (Figure 2). Fascicular shifting procedure was performed to extend the sciatic nerve for approximately 7 cm. The sciatic trunk was exposed at the popliteal level, and an 8-cm fascicular segment was excised from the distal stump and sutured to the proximal stump using 10/0 non-absorbable thread under an operating microscope (Zeiss) (Figure 3). The chosen length of fascicular segment was unlike previous reports in other centers which excised a much shorter segment.20,27
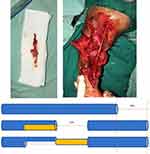 |
Figure 3 Fascicular shifting methods. |
Skin flaps were sutured with 2/0 absorbable thread, and immediate post-operative measurements showed an angle of 120° in the operated knee, adding a 30° immediate improvement compared with 90° preoperatively. A long leg posterior splint was applied until the wound healed. The patient was closely monitored for soft tissue healing and no post-operative complication nor adverse events were reported (Figure 4). Nerve evaluation was conducted through clinical measurements. Ten months after the procedure, a laparoscopic procedure was performed by the urologist to treat the undescended testicles and done without any complication.
On his latest visit at two years of age, the patient’s motoric ability was excellent, as he was able to stand with only little help. In contrast, the results of serial nerve conduction study were unsatisfactory. Moreover, the left foot was still in extreme plantar flexion and knee flexion contracture remained at 30° (Figure 5). The patient underwent a second procedure consisting of Achilles tendon, FHL lengthening, soleus lengthening, release of posterior capsule and release of medial plantar fascia performed simultaneously (Figure 6). A long-leg cast was applied post-operatively to maintain the 90° dorsiflexion that had been achieved through the procedures (Figure 7).
 |
Figure 5 Fourteen-months post-operative ROM evaluation. Range of motion of the knee was 25°–140°. Ankle was in equinovarus position. |
 |
Figure 7 Post-operative long leg cast application. |
During this visit, the operative wound has healed and the dorsiflexion was successfully maintained at 90° without the cast. It was noted during this visit that his knee was still in 30° of flexion contracture. However, there was flexible ankle joint which allowed the patient to reach a plantigrade position in passive dorsiflexion. The ability to reach a plantigrade position was necessary for the patient to stand with both legs (Figure 8). A Knee-Ankle-Foot orthosis (KAFO) was utilized to help the patient in performing his daily activities and the patient will be closely-monitored into adulthood in case any further changes occur. The patients’ parents were pleased for their child’s gait and physical improvement from the procedure. Although gradual, the patients’ overall recovery was satisfying for the parents.
Discussion
The popliteal pterygium or popliteal webbing is widely reported as part of a more complex syndrome, including Human Disorganization Syndrome and popliteal pterygium syndrome where multiple congenital anomalies present. The etiology is currently related to the mutation of the gene Interferon Regulatory Factor 6 (IRF-6), which is inherited in an autosomal-dominant pattern.29 Our patient lacks family history risk factors and presented with no other congenital anomalies except genital anomaly of undescended testicles.
The indication of PPS treatment is mainly functional limitation in ambulation and deformity. Due to the uncommonness of PPS, the reports of surgical treatment are also limited. In spite of its rarity, Parikh et al suggested several methods for PPS treatment. It consists of conservative treatment, such as serial casting and bracing. Conservative treatment cannot be used as the only management since it produces poor outcome. We performed the procedure during patient’s infancy period and reflected on the limited evidence available as to when would be the most ideal time to intervene invasively. Although many reports and reviews prefer “early intervention” to allow for gait learning, there has been no agreement as to the exact age recommended.24,25
We performed soleus lengthening which was followed by the Achilles tendon to achieve greater correction of the equine foot based on previous study.30 If multiple surgeries are required, femoral shortening or extension osteotomy through a lateral approach should be done to prevent nerve injury from repeated posterior exposure. For moderate to severe cases, initial fixed-flexion femoral shortening or supracondylar femoral extension osteotomy should be combined with soft tissue releases. However, complete lengthening often fails because the nerves and vessels in the affected site are short and grow into the web attached to adjacent tissues. Sewilam et al proposed a theory of nerve maldevelopment which resulted in short nerve formation and disturbed the normal growth of the surrounding tissue such as the muscles, tendons, and skin folds.13 This theory might explain the location of the sciatic nerve that superficially bowstrings at the fibrous band’s free end. This short nerve remains a major problem in treating popliteal pterygium with severe flexion deformity. Several methods have been described for milder cases, including serial casting combined with a variety of soft- tissue releases, Ilizarov procedure and bony osteotomies. Soft tissue release with multiple Z- plasty have proved to be insufficient in severe cases, alternate traction and casting have also been reported even though it leads to an unsuccessful result, and the reported patient eventually underwent bilateral leg amputation.17 Bony osteotomies are indicated for bilateral defects, and their results vary depending on the severity of flexion contracture.
Strategies to overcome the short sciatic nerve, including cable nerve grafting, have resulted in satisfactory outcomes.18 However, this procedure is highly aggressive as two nerves are involved (the donor and the recipient) and requires a combination of highly skilled team and tools to perform such method. As an alternative, Maral et al reported nerve expansion using a 75-cc tissue expander placed under the nerve-muscle complex and gradually filled with 5 cc saline weekly. However, their experiment had to be halted as wound dehiscence was observed when a total of 60 cc saline has been reached.19 The author reported an additional achievement of a 40-degree extension through the procedure. Spencer et al preferred to avoid nerve grafting to prevent motoric and sensory dysfunction and instead opted for bilateral femoral osteotomy to match the limbs to the available nerve length.25
The fascicular shifting technique has been reported in animal studies with superior results to the sensory graft in terms of motor recovery. The main idea is to “shift” a fascicular group from a distal nerve segment and attach it to the defect site. We opted for this technique instead due to the advantage of a comparable result to autologous motor graft without additional morbidity to the donor site. Furthermore, the composition of motor and sensory fibers is maintained, as proven by histochemical analysis.20 Partial gap because of the “shift” also regenerates well alongside the healthy nerve graft, as elaborated in the animal study.21 We took a long (8 cm) fascicular graft so that the final length of the nerve made its position beneath the deep muscle fascia with minimal stretch in extension. The unsatisfactory result of the nerve conduction study might be caused by the length of graft although the animal study we used as reference achieved successful sensory nerve regeneration in their fascicular shifting procedure.20 Another suggestion explaining the sensory deficiency was the presence of a dimple on the patient’s sacrum area. Sensory deficits were also encountered by several reports after performing other techniques of nerve repair mentioned earlier, which flags the importance of possible future complications such as plantar ulcers.13,26 During the early regeneration process after the procedure, fluid permeation from the surrounding tissue was the primary nutrient mode of transport for the graft. Micro-vessels started to grow on both ends of the graft and penetrated the nerve matrix along the long axis. After 14 days, newly formed micro vessels were expected to have robust anastomosis at the middle part of the graft.22 Longer nerve grafts require different times to complete the vascularization, depending on the approach used. It would take approximately five days for a 60 mm autograft before the first signs of vascularization in the mid-graft appear.23
The prolonged time required to obtain adequate vascularization in longer grafts might be the cause of cell damage and senescence, oxidative stress, and other numerous pathological processes including ischemia, degeneration, and necrosis. Angiogenesis and the formation of new vascular networks within the nerve graft are the two critical processes for successful nerve regeneration. They must be considered in the development of functional nerve grafts.16 Further histological study needs to be conducted to determine the ideal length of a fascicular nerve graft in lower extremities.
Besides the popliteal web, other associated extremity malformations should also be treated with a properly-functioning limb as the main outcome. Foot deformities, including certain degree of pes equinovarus, should be treated with the current standard methods. Our patient underwent Achilles tendon lengthening, FHL lengthening, soleus lengthening, release of posterior capsule, and release of medial plantar fascia to overcome the problem. Post-operative serial casting might be applied for better results.13 However, previous literatures have reported recurrence being commonly observed as patients grow. Therefore, patients with popliteal pterygium should be closely monitored after undergoing treatments and parents should be educated regarding the possibility of repeated surgical corrections to achieve the best functional result. Weight-bearing achievement does not rule out the possibility of unrefined gait and physiotherapy will be required in order to improve it.
This case report has its own strength and weaknesses. Our surgical approach of shifting the fascicle to lengthen the shortened neurovascular bundle managed to refine the patient’s physical performance and gait. This would be a novelty as the unfamiliar approach was done on PPS patient unlike prior studies. The patient’s outcome imply that a more aggressive approach might aid in improving patients’ ambulatory which is essential especially in a growing child. But the slight persistence of knee contracture also allowed us to conclude that the fascicle lengthening is not the final treatment. With our patient’s slight persistence of knee contracture and poor sensory nerve stimulation, fascicular lengthening procedure using a longer segment may not be the best approach. Although we successfully maintained a close monitor on the patient for 14 months after the initial surgery, a longer period of follow up time should be done in order to evaluate the long-term effect of this surgical approach especially as the child grows and develops into puberty. Another point was genetic analysis was not performed on this patient nor towards his parents. As PPS pathogenesis is believed to rely heavily on genetic mutation, this analysis became pivotal especially for the parents’ future plans of having another child. Due to the rarity of PPS, our case report shared the diagnostic and treatment approach which may help in expanding the current knowledge of this anomaly.
Conclusion
Popliteal pterygium is a rare condition and recognizing its clinical manifestation has not been easy. Treatment involving multiple soft tissue procedures have resulted in acceptable functional outcomes, although it is still very challenging to graft the nerve tissue. This report highlights that the lengthening of excised nerve still failed to result in the most suited technique even after opting for longer fascicular segment to overcome the difficult problem reflected by unsatisfactory EMG result. Future cases of popliteal pterygium and the opted treatment, especially in extreme cases, should be openly-reported in the orthopedic community to allow experience sharing in determining the best management for similar conditions. The patient’s persistence of slight knee contracture imply that a longer segment of fascicle excise does not necessarily guarantee the optimal outcome and further studies are required to determine the most suited length to allow improvement of patients’ ambulatory which is essential especially in a growing child.
Ethics Approval and Consent to Participate
The authors have obtained signed informed consent for patient’s information and photos publication from the patients’ parents as the patient is considered underaged. This report has received ethical approval by Medical and Health Research Ethics Committee, Faculty of Medicine, Public Health and Nursing Universitas Gadjah Mada - Dr. Sardjito General Hospital and adhered to the Case Report (CARE) 2013 Guidelines and fulfilled the checklists.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gorlin RJ, PindborgJJ CM. Syndromes of the Head and Neck.
2. Froster-Iskenius UG. Popliteal pterygium syndrome. J Med Genet. 1990;27(5):320–326. doi:10.1136/jmg.27.5.320
3. Bennun RD, Stefano E, Moggi LE. Van der woude and popliteal pterygium syndromes. J Craniofac Surg. 2018;29(6):1434–1436. PMID: 29916977. doi:10.1097/SCS.0000000000004698
4. Hamamoto J, Matsumoto T. A case of facio-genito-popliteal syndrome. Ann Plast Surg. 1984;13(3):224–229. PMID: 6093671. doi:10.1097/00000637-198409000-00009
5. Bahsas F. Fevre-languepin syndrome popliteal pterygium syndrome a case report. Pediatr Neonatal Biol Open Access. 2016;1. doi:10.23880/PNBOA-16000104
6. Fahmy M. Rare Congenital Genitourinary Anomalies. Berlin, Heidelberg: Springer Berlin Heidelberg; 2015.
7. Busche A, Hehr U, Sieg P, Gillessen-Kaesbach G. Van der woude and popliteal pterygium syndromes: broad intrafamilial variability in a three generation family with mutation in IRF6. Am J Med Genet A. 2016;170(9):2404–2407. doi:10.1002/ajmg.a.37791
8. Little HJ, Rorick NK, Su L, et al. Dixon, Paul Shore, Missense mutations that cause Van der Woude syndrome and popliteal pterygium syndrome affect the DNA-binding and transcriptional activation functions of IRF6. Hum Mol Genet. 2009;18(3):535–545. doi:10.1093/hmg/ddn381
9. Ghassibé M, Revencu N, Bayet B, et al. Six families with van der Woude and/or popliteal pterygium syndrome: all with a mutation in the IRF6 gene. J Med Genet. 2004;41:e15. doi:10.1136/jmg.2003.009274
10. Ferreira de lima RL, Hoper SA, Ghassibe M, et al. Prevalence and nonrandom distribution of exonic mutations in interferon regulatory factor 6 in 307 families with Van der Woude syndrome and 37 families with popliteal pterygium syndrome. Genet Med. 2009;11:241–247. doi:10.1097/GIM.0b013e318197a49a
11. Traisrisilp K, Luewan S, Sirilert S, Jatavan P, Tongsong T. Prenatal sonographic and molecular genetic diagnosis of popliteal pterygium syndrome. Diagnostics. 2021;11(10):1819. doi:10.3390/diagnostics11101819
12. Karmakar S, Mishra B. A neglected case of popliteal pterygium syndrome presenting in adulthood. Clin Med Img Lib. 2020;6:159. doi:10.23937/2474-3682/1510159
13. Sewilam M, Hassan AS, Shoaib A, Alrayes M. Surgical correction of popliteal pterygium with serial splinting: a case report and review of literature. plastic and reconstructive surgery. Global Open. 2021;9(11):e3913. doi:10.1097/GOX.0000000000003913
14. Posey JE, Dariya V, Edmonds JL, Lee EI, Probst FJ, Premkumar MH. Syngnathia and obstructive apnea in a case of popliteal pterygium syndrome. Eur J Pediatr. 2014;173(12):1741–1744. doi:10.1007/s00431-014-2453-9
15. Kim HM, Park IJ, Jeong C. Treatment of popliteal pterygium using an Ilizarov external fixator. Clin Orthop Surg. 2009;1(4):236–239. doi:10.4055/cios.2009.1.4.236
16. Lovati AB, D’Arrigo D, Odella S, Tos P, Geuna S, Raimondo S. Nerve repair using decellularized nerve grafts in rat models. A review of the literature. Front Cell Neurosci. 2018;12:427. doi:10.3389/fncel.2018.00427
17. Hecht F, Jarvinen J. Heritable dysmorphic syndrome with normal intelligence. J Pediatr. 1967;70:927–937. doi:10.1016/S0022-3476(67)80265-8
18. Tuerk D, Edgerton MT. The surgical treatment of congenital webbing (pterygium) of the popliteal area. Plast Reconstr Surg. 1975;56:339–444. doi:10.1097/00006534-197509000-00020
19. Maral T, Tuncali D, Ozgur F, ??afak T, G??rsu KG. A case of popliteal pterygium treated along with nerve expansion. Plast Reconstr Surg. 1997;100:91–95. doi:10.1097/00006534-199707000-00016
20. Hader M, Sporer ME, Roche AD, et al. Fascicular shifting: a novel technique to overcome large nerve defects. J Neurosurg Spine. 2017;27:723–731. doi:10.3171/2017.3.SPINE16276
21. McCallister WV, Cober SR, Norman A, Trumble TE. Using intact nerve to bridge peripheral nerve defects: an alternative to the use of nerve grafts. J Hand Surg Am. 2001;26:315–325. doi:10.1053/jhsu.2001.22918
22. He B, Zhu Z, Zhu Q, et al. Factors predicting sensory and motor recovery after the repair of upper limb peripheral nerve injuries. Neural Regen Res. 2014;9:661–672. doi:10.4103/1673-5374.130094
23. Farber SJ, Hoben GM, Hunter DA, et al. Vascularization is delayed in long nerve constructs compared with nerve grafts. Muscle Nerve. 2016;54:319–321. doi:10.1002/mus.25173
24. Parikh SN, Crawford AH, Do TT, Roy DR. Popliteal pterygium syndrome: implications for orthopaedic management. J Pediatr Orthop B. 2004;13(3):197–201. doi:10.1097/00009957-200405000-00010
25. Keita B, Toure MA, Sacko ML, Barry MM, Kaba MK, Ag-bo-Panzo D. Pterygium popliteal syndrome concerning a case in the pediatric surgery department of the donka national hospital (Conakry CHU). Open J Pediatr. 2022;12:162–169. doi:10.4236/ojped.2022.121017
26. Xia W, Bai Z, Dai R, Zhang J, Lu J, Niu W. The effects of sensory re-education on hand function recovery after peripheral nerve repair: a systematic review. NeuroRehabilitation. 2021;48(3):293–304. doi:10.3233/NRE-201612
27. Sporer ME, Brugger PC, Aman M, et al. Fascicular shifting in the reconstruction of brachial plexus injuries: an anatomical and clinical evaluation. J Neurosurg. 2022:1–10. PMID: 36681968. doi:10.3171/2022.11.JNS221312
28. Bissinger RL, Koch FR. Nonlethal multiple pterygium syndrome: escobar syndrome. Adv Neonatal Care. 2014;14(1):24–29. doi:10.1097/ANC.0000000000000039
29. Bender RA, Tanriverdi EC, Yucel A, Erdem MG. A family from turkey with bartsocas-papas syndrome. Eurasian J Med. 2017;49(1):74–75. doi:10.5152/eurasianjmed.2017.16272
30. Firth GB, McMullan M, Chin T, et al. Lengthening of the gastrocnemius-soleus complex: an anatomical and biomechanical study in human cadavers. J Bone Joint Surg Am. 2013;95(16):1489–1496. PMID: 23965699. doi:10.2106/JBJS.K.01638
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




