Back to Journals » International Journal of Women's Health » Volume 15
Oral Tetrahydrocannabinol (THC):Cannabinoid (CBD) Cannabis Extract Adjuvant for Reducing Chemotherapy-Induced Nausea and Vomiting (CINV): A Randomized, Double-Blinded, Placebo-Controlled, Crossover Trial
Authors Sukpiriyagul A, Chartchaiyarerk R, Tabtipwon P, Smanchat B , Prommas S , Bhamarapravatana K, Suwannarurk K
Received 5 January 2023
Accepted for publication 11 July 2023
Published 16 August 2023 Volume 2023:15 Pages 1345—1352
DOI https://doi.org/10.2147/IJWH.S401938
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Apichaya Sukpiriyagul,1 Ratiporn Chartchaiyarerk,1 Paluekpon Tabtipwon,1 Buppa Smanchat,1 Sinart Prommas,1 Kornkarn Bhamarapravatana,2 Komsun Suwannarurk3
1Department of Obstetrics and Gynecology, Bhumibol Adulyadej Hospital, Royal Thai Air Force Bangkok Thailand; 2Department of Preclinical Science, Faculty of Medicine, Thammasat University Hospital, Pathum Thani, Thailand; 3Gynecologic Oncology Unit, Department of Obstetrics and Gynecology, Faculty of Medicine, Thammasat University Hospital, Pathum Thani, Thailand
Correspondence: Ratiporn Chartchaiyarerk, Department of Obstetrics and Gynecology, Bhumibol Adulyadej Hospital, Pathum Thani, Thailand, Tel +66814092569, Email [email protected]
Objective: To evaluate the effects of tetrahydrocannabinol (THC):cannabinoid (CBD) (1:1) oil in reducing chemotherapy-induced nausea and vomiting (CINV) in gynecologic cancer patients who received moderate-to-high emetogenic chemotherapy.
Material and Method: This was a randomized, double-blinded, crossover and placebo-controlled trial. The study was conducted at the Gynecologic Oncology Units, Bhumibol Adulyadej Hospital (BAH), Royal Thai Air Force, Bangkok, Thailand, between August and November 2022. Participants had gynecologic cancer and received moderate-to-high emetogenic chemotherapy. Subjects were randomized and divided into two groups (A and B) based on the block of four randomization method. In the first cycle, groups A and B received THC:CBD extract oil 1:1 (TCEO) and placebo before chemotherapy administration. In the second cycle, groups A and B received placebo and TCEO before chemotherapy administration. Both groups received per protocol antiemetic medication during chemotherapy. Nausea score and side effects were recorded.
Results: A total of 60 cases were recruited. After exclusion, 54 cases were included in the study. The mean age of participants was 54.4 years. The mean body mass index (BMI) was 26.5 kg/m2. Fifty-nine (21/54) percent cases were the advanced stages of cancer. The nausea score of TCEO and placebo groups were 2.11 and 2.99, respectively (P < 0.05). More than half of the participants (36/54) reported dizziness and sedation side effects. Dry mouth, confusion, anxiety, and palpitation of both groups were comparable.
Conclusion: The cannabinoid extract (THC:CBD) was an appropriate adjuvant agent to reduce CINV in patients with gynecologic cancer who received high-emetogenic chemotherapy. Dizziness and sedation were the major side effects.
Keywords: CINV, THC, CBD, cannabis
Introduction
Chemotherapy is an effective standard treatment for gynecologic malignancy. Despite the usefulness and efficacy of chemotherapy, it is still associated with numerous side effects, especially chemotherapy-induced nausea and vomiting (CINV). CINV is one of the most common adverse effects and leads to significant morbidity and deterioration of patients’ quality of life.1 As a consequence, noncompliance to chemotherapy treatment can be frequently observed.2,3
CINV can be divided into five different phases: The acute phase is defined as CINV occurring within 24 h post chemotherapy, delayed phase is defined as CINV occurring within 24–120 h and may last 6–7 days, anticipatory phase is when patients have CINV prior to administration of future chemotherapy, breakthrough phase is when patients have CINV within 5 days of prophylactic antiemetic agents, and refractory phase is when CINV occurs in subsequent chemotherapy cycles following prior failure of prophylactic treatment.4 Delayed phase is more common and severe than the other phases manner and is resistant to antiemetic treatment.5
According to NCCN guidelines, standard antiemetic agents for patients receiving moderate and high emetogenic chemotherapy include 5-HT3 antagonists, dexamethasone, NK1 RAs, and olanzapine. However, NK1 RAs and olanzapine were added for patients receiving high emetic risk chemotherapy. Platinum-based chemotherapy (cisplatin and carboplatin) were the backbone of chemotherapy regimen in gynecologic cancer and were classified as high emetic risk. Lorazepam and a histamine (H2) blocker or a proton pump inhibitor may also be added to all these regimens to manage anxiety and dyspepsia/reflux-related symptoms, respectively.4 Although the use of antiemetic agents have improved, CINV remains an issue with most patients.
The endocannabinoid system is associated with the control of nausea and vomiting through cannabinoid receptors 1(CB1) and cannabinoid receptors 2 (CB2). CB1 receptors are mainly found in the central venous system and CB2 receptors are located mainly in the peripheral. Both CB1 and CB2 are found in the dorsal vagal complex at the center for emetogenic stimuli.6 The activation of these receptors results in inhibition of emesis. Accordingly, the blockade of CB1 cannabinoid receptors induces vomiting. This supports CB1 and CB2 function roles within the areas of the brain related to nausea and vomiting.7–10
Cannabis sativa L. (marijuana or hemp) (Cannabinaceae) belongs to a group of herbaceous shrubs. There are now over 700 varieties of cannabis from which hundreds of compounds have been identified. The main compounds for medical use include delta-9-tetrahydrocannabinol (THC), the psychoactive compound, and cannabidiol (CBD) which is a non-psychoactive compound.10 Both THC and CBD are partial agonists at CB1 receptors. By contrast, CBD acts as a weak antagonist to both CB1 and CB2 receptors so that it can reverse the effect of the agonist.11
In Thailand, the Narcotics Act (N0.7) of 2019 allows the use of cannabis for medical treatment under the supervision of licensed physicians. There are only three types of natural cannabis oil produced by the Government Pharmaceutical Organization (GPO) in Thailand, namely THC, CBD, and THC: CBD (1:1). There are very limited studies on the efficiency, tolerability, and side effects of cannabis oil in the treatment and prevention of CINV in Thailand. Hence, the objective of this study was to evaluate the effects of THC:CBD oil in reducing CINV in gynecologic cancer patients who underwent high-emetogenic chemotherapy.
Materials and Methods
This was a randomized, double-blinded, crossover, placebo-controlled trial. And the study was approved in 2021 by the ethics committee of Bhumibol Adulyadej Hospital in Thailand (IRB: No. 96/64) (TCTR20220829003). The study was conducted in accordance with the Declaration of Helsinki. Patients were enrolled from August to November 2022 at Bhumibol Adulyadej Hospital, Royal Thai Air Force, Bangkok, Thailand.
Study Population
Patients with gynecologic malignancies treated with moderate-to-high emetogenic chemotherapy at Bhumibol Adulyadej Hospital were enrolled. All participants were ≥ 18 years old and had a performance status of Eastern Cooperative Oncology Group (ECOG) ranging from 0 to 2. All participants provided informed consent to receive standard antiemetic medication that included 20 mg dexamethasone, 8 mg ondansetron, and 50 mg ranitidine which were injected 30 min before chemotherapy administration. Thereafter, oral ondansetron (8 mg) was given twice a day. The chemotherapy session was separated between cycle at least 21 days. Home medication included one ondansetron tablet (8 mg twice a day) and two tablets (5 mg twice a day for 5 days). Therefore, the antiemetic-free duration between chemotherapy cycles was considered a washout period.
Patients with following characteristics were excluded from the study:
Procedures
THC:CBD extract oil 1:1 (CX) in this study was manufactured by Thai GPO (in a 5 mL droplet bottle container). One mL of CX contained 2.7 mg of THC and 2.5 mg of CBD. The placebo was stored in an identical CX container that contained the same oil base and had similar appearance. The bottles were labelled as 1 and 2 for consequent cycle use. After informed consent were signed, participants were randomized into two groups based on the block of four technique. Dose of chemotherapy agents were AUC 5 of carboplatin and 70 mg/m2 of cisplatin. Paclitaxel dose was 175 mg per square meter.
Group A received CX (labeled as “Cycle 1”) in the first chemotherapy cycle and received placebo 30 min before chemotherapy (labeled as “Cycle 2”) in the next chemotherapy cycle (consequent cycle). Group B received placebo 30 min before chemotherapy (“Cycle 1”) in the first chemotherapy cycle and received CX (labeled as “Cycle 2”) in the next chemotherapy cycle.
Both investigators and subjects were blinded. The subject’s name and cycle number were labelled on the container. The specific container was given to subjects before each cycle of chemotherapy. The after-use container was sent back to the investigator. The return containers were checked to evaluate the usage dose.
In prior cycles, participants were assigned to use the bottles labeled as “Cycle 1”. During day 1 to day 3, participants were advised to take one drop via sublingual route once in the morning and once in the evening before mealtime. On days 4 and 5, participants took one drop via the sublingual route in the morning, afternoon, and evening before mealtime. For the next cycle, with at least 21 days for the washout period, the second bottles labeled as “Cycle 2” were handed out and with the same instructions. All participants received the CINV prophylaxis according to National Comprehensive Cancer Network Antiemesis Version 1.2022.4
The record form comprised a self-administered questionnaire including nausea score, side effects, and drug compliance. Nausea score was measured by the participants numeric 11-point rating scale (0 = no nausea and 10 = worst possible nausea). The adverse events effect was also recorded. Participants self-filled a questionnaire for 5 consecutive days after completion of chemotherapy. (Day one = 0–24 h after chemotherapy, Days 2–5 = 24 −120 h after chemotherapy). The demographic characteristics of subjects were obtained by interviewing, with a structural questionnaire filled out by the interviewer.
The sample size was calculated by using the Minitab program version 21.2 (PSU, PA, USA). The equivalence test of 2 × 2 crossover design was used. Target power was set at a level of 90%. Alpha errors were set at the level of 0.01. The total sample size was calculated to be at least 54. Statistical analysis was performed by using the Statistical Package for the Social Science (SPSS) version 22 (IBM Corporation, Armonk, NY, USA). P ≤ 0.05 was considered statistically significant. The demographic data of all participants were analyzed and presented as percentage values. The nausea score was analyzed by independent samples t-test with 95% confidential interval (CI). Analysis of variance (ANOVA) for 2×2 crossover study was used to compare the treatment effect, sequence, and period effect. Side effects were analyzed by comparing percentages between groups using the random-effects logistic regression.
Results
During the study period, 60 patients were enrolled and divided into groups A and B. A total of 54 cases were recruited as shown in Figure 1. The mean age of participants was 54.4 years. Half (22/54) of the cases were ovarian cancer. Advanced cancer was observed in 59.3% (32/54) cases. Most cases (54/54) received platinum-based chemotherapy regimen. The demographic characteristics of subjects are presented in Table 1. There was no case who developing delayed emesis from chemotherapy that needed admission.
 |
Table 1 Baseline Characteristic (n) |
 |
Figure 1 Consort flow diagram. Notes: CONSORT figure adapted from Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010;7(3): e1000251. Copyright: © 2010 Schulz et al. Creative Commons Attribution License.12 |
The mean nausea score of subjects who received CX was significantly lower than those that received placebo (2.1 vs 3, p = 0.001) as shown in Table 2. After the first cycle, both groups were cross-over switched, as presented in Figure 2.
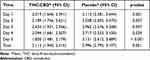 |
Table 2 Mean Nausea Score Between THC:CBD and Placebo Groups |
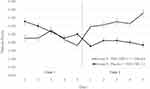 |
Figure 2 Mean nausea score between group A and B. |
Sedation and dizziness were major side effects (88.8% [48/54]). One-quarter (14/54) of subjects reported dry mouth as the side effect. The side effects of CX, namely sedation, dizziness, anxiety, dry mouth, confusion, palpitations, hallucination, rash, mood, or behavior changes are presented in Table 3. Both groups (CX and placebo) had comparable side effects.
 |
Table 3 Side-Effects Between THC:CBD 1:1 and Placebo (N = 54) |
Discussion
The current study enrolled patients with gynecologic malignancy who underwent high-emetogenic chemotherapy. Subjects who received THC:CBD reported a lower nausea score than those who received only standard antiemetic agents during the first two days. During days 3 and 4, subjects who received THC:CBD or placebo reported a similar nausea score. However, on day 5, subjects who received THC:CBD had a lower nausea score than those who received placebo. Delayed emesis after chemotherapy treatment is commonly found especially in those receiving platinum-based chemotherapy.4,13 Adjuvant of cannabinoid extract (THC:CBD) could prevent nausea and vomiting in early and delayed phases. Cross-over of cases between placebo and THC:CBD were performed reduce interpersonal variation bias. Patients who received THC:CBD still had lower CINV than those who received placebo on day 5.
A comprehensive comparison of previous literature and the current study is summarized and presented in Table 4. In a 2020 Australian study, Grimison et al reported that THC:CBD extract could reduce CINV in those who received chemotherapy.14 Patient in their study had a mix of gynecologic and non-gynecologic cancer. Half of the subjects in their study received high-emetogenic agent (platinum-based), whereas all patients in our study underwent high-emetogenic chemotherapy. Doses of THC:CBD in Grimison et al’s study were self-administered and no more than 0.5 mg. Doses of THC:CBD in our study ranged between 0.25 and 0.4 mg. Our findings seem consistent with those of Grimison’s report.
 |
Table 4 Summarized Data from Previous Literature of Cannabinoid Extract and Chemotherapy in Chemotherapy-Induced Nausea and Vomiting (CINV) Aspects |
Cannabinoid’s work in year 2010, Duran reported the efficacy of oro-mucosal spray of THC:CBD. The doses of Duran’s work were 13 mg of THC and 12 mg of CBD. Demographic characters of Duran’s cases were breast ovarian and lung cancer. The total THC:CBD doses of Duran’s work was higher than the present study. Seventy percent (5/7) of Duran’s cases reported good effect and the side effects of Duran’s reported were 86%.15
Polito et al’s 2018 study included Canadian children (<14 years old) diagnosed with solid tumors, brain tumors, leukemia, and lymphoma. It was noted that 75% (83/110) of Polito’s patients received high-emetogenic chemotherapy; moreover, nabilone (synthetic THC) was reported to reduce CINV.16 Another study from Mexico by Turcott et al in 2018 reported that advanced-stage lung cancer patients who received nabilone had better quality of life than those who did not receive the treatment.17 Nabilone’s doses in Polito’s and Turcott’s study were 0.25 and 0.5 −1 mg, respectively.16,17 Polito’s, Duran’s and Turcott’s works reported the efficacy of synthetic cannabinoids to reduce the side effect of CINV. From current study, natural extract cannabinoid supported the Polito’s and Turcott’s work with synthetic cannabinoid.
Dizziness and sedation are not serious side effects for patients with cancer. One-third of participants in the current study reported dizziness and sedation. Polito and Grimison reported the identical rates of dizziness (10% and 10%) and very similar rates of sedation (20% and 19%), respectively.14,16 The rates of sedation and dizziness in Polito’s, Grimison’s, and us were similar.
The strengths of this study include its randomized, controlled, double-blinded, and cross-over design. This could reduce the interpersonal variation bias. During the study period, the use of cannabis-related products was a major concern among the Thais, given the new Thai narcotic act. Cannabis was removed from the narcotic drug act. The placebo effect and fixed doses of cannabinoid were an unavoidable limitation of the study.
Cannabinoid extract could interact with CB1 and CB2.7–9 Hanifa et al from Indonesia recently reported that Vetiver oil (a CB2 agonist) was likely suitable for use as an anti-cancer agent in triple negative breast cancer (TNBC).18 Although Hanifa et al carried out in vitro research, this might be the light at the end of a dark tunnel. Subjects with gynecologic cancer who have undergone primary extirpation surgery followed by high-emetogenic chemotherapy should receive appropriate pharmaceutical product and psychological support. Loss of female identity from extirpation surgery, menopausal symptoms, fear of dying, and CINV could impact the quality of life in patients. Adjuvant treatment to lower detrimental side effects should be considered. However, some literatures indicated that CBD was antagonist with cisplatin in vitro study.19,20 Future studies on the potential of cannabinoids extract in improving the quality of life of patients with gynecologic cancer should be performed.
Although, all cancer cases received standard antiemetic regimen. The adjuvant of THC and CBD to those cases could reduce emetogenic score significantly. However, the baseline emetogenic score of cases were quite low (around 2/10). The further study with more subjects needed for evaluate the significance of this effect. In conclusion, cannabinoid extract (THC:CBD) was an appropriate adjuvant agent for reducing CINV in gynecologic cancer cases who underwent high emetic chemotherapy.
Conclusion
The cannabinoid extract (THC:CBD) was an appropriate adjuvant agent to reduce CINV in patients with gynecologic cancer who received high-emetogenic chemotherapy. Dizziness and sedation were the major side effects.
Data Sharing Statement
All data are available and submitted upon requests. For the additional data please contact Ratiporn Chartchaiyarerk.
Acknowledgments
This study was supported by the Bhumibol Adulyadej Hospital Research Fund granted in 2021. The authors thank Dr. Jintana Manorompatrasal and the Sawasdee Clinic for excellent consulting.
Disclosure
There is no conflict of interest in this work.
References
1. Friedlander ML, Markman M. Chemotherapy. In: Berek JS, Hecker NF, editors. Berek & Hacker’s Gynecologic Oncology.
2. Sommariva S, Pongiglione B, Tarricone R. Impact of chemotherapy-induced nausea and vomiting on health-related quality of life and resource utilization: a systematic review. Crit Rev Oncol Hematol. 2016;99:13–36. doi:10.1016/j.critrevonc.2015.12.001
3. Gupta K, Walton R, Kataria SP. Chemotherapy-induced nausea and vomiting: pathogenesis, recommendations, and new trends. Cancer Treat Res Commun. 2021;26:100278. doi:10.1016/j.ctarc.2020.100278
4. National Comprehensive Cancer Network. Antiemesis (Version 2.2022). Available from: https://www.nccn.org/professionals/physician_gls/pdf/antiemesis.pdf.
5. May MB, Glode AE. Dronabinol for chemotherapy-induced nausea and vomiting unresponsive to antiemetics. Cancer Manag Res. 2016;8:49–55. doi:10.2147/CMAR.S81425
6. Tafelski S, Häuser W, Schäfer M. Efficacy, tolerability, and safety of cannabinoids for chemotherapy-induced nausea and vomiting--a systematic review of systematic reviews. Schmerz. 2016;30(1):14–24. doi:10.1007/s00482-015-0092-3
7. Todaro B. Cannabinoids in the treatment of chemotherapy-induced nausea and vomiting. J Natl Compr Canc Netw. 2012;10(4):487–492. doi:10.6004/jnccn.2012.0048
8. Darmani NA. Mechanisms of broad-spectrum antiemetic efficacy of cannabinoids against chemotherapy-induced acute and delayed vomiting. Pharmaceuticals. 2010;3(9):2930–2955. doi:10.3390/ph3092930
9. Parker LA, Rock EM, Limebeer CL. Regulation of nausea and vomiting by cannabinoids. Br J Pharmacol. 2011;163(7):1411–1422. doi:10.1111/j.1476-5381.2010.01176.x
10. Klumpers LE, Thacker DL. A brief background on cannabis: from plant to medical indications. J AOAC Int. 2019;102(2):412–420. doi:10.5740/jaoacint.18-0208
11. Taylor BN, Mueller M, Sauls RS. Cannabinoid Antiemetic Therapy. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
12. Schulz KF, Altman DG, Moher D. CONSORT Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010;7(3):e1000251.
13. Hsieh RK, Chan A, Kim HK, et al. Baseline patient characteristics, incidence of CINV, and physician perception of CINV incidence following moderately and highly emetogenic chemotherapy in Asia Pacific countries. Support Care Cancer. 2015;23(1):263–272. doi:10.1007/s00520-014-2373-2
14. Grimison P, Mersiades A, Kirby A, et al. Oral THC: CBD cannabis extract for refractory chemotherapy-induced nausea and vomiting: a randomised, placebo-controlled, Phase II crossover trial. Ann Oncol. 2020;31(11):1553–1560. doi:10.1016/j.annonc.2020.07.020
15. Duran M, Pérez E, Abanades S, et al. Preliminary efficacy and safety of an oromucosal standardized cannabis extract in chemotherapy-induced nausea and vomiting. Br J Clin Pharmacol. 2010;70(5):656–663. doi:10.1111/j.1365-2125.2010.03743.x
16. Polito S, MacDonald T, Romanick M, et al. Safety and efficacy of nabilone for acute chemotherapy-induced vomiting prophylaxis in pediatric patients: a multicenter, retrospective review. Pediatr Blood Cancer. 2018;65(12):e27374. doi:10.1002/pbc.27374
17. Turcott JG, Del Rocío Guillen Núñez M, Flores-Estrada D, et al. The effect of nabilone on appetite, nutritional status, and quality of life in lung cancer patients: a randomized, double-blind clinical trial. Support Care Cancer. 2018;26(9):3029–3038. doi:10.1007/s00520-018-4154-9
18. Hanifa M, Wulandari R, Zulfin UM, Nugroho EP, Haryanti S, Meiyanto E. Different cytotoxic effects of vetiver oil on three types of cancer cells, mainly targeting CNR2 on TNBC. Asian Pac J Cancer Prev. 2022;23(1):241–251. doi:10.31557/APJCP.2022.23.1.241
19. Marzęda P, Wróblewska-łuczka P, Drozd M, Florek-łuszczki M, Załuska-Ogryzek K, Łuszczki JJ. Cannabidiol interacts antagonistically with cisplatin and additively with mitoxantrone in various melanoma cell lines-an isobolographic analysis. Int J Mol Sci. 2022;23(12):6752. doi:10.3390/ijms23126752
20. Alsherbiny MA, Li CG. Medicinal cannabis-potential drug interactions. Medicines. 2018;6(1):3. doi:10.3390/medicines6010003
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
